Course
ACL Surgery and Nursing Considerations
Course Highlights
- In this ACL Surgery and Nursing Considerations course, we will learn about and improve understanding of the anatomy and pathophysiology of the knee and ACL and knee meniscus injuries.
- You’ll also learn treatment methods for ACL and meniscus tears, especially surgical intervention.
- You’ll leave this course with a broader understanding of knowledge of knee pathophysiology and treatments to provide patient education for individuals with ACL and meniscus tears, especially for those undergoing surgery.
About
Contact Hours Awarded: 2
Course By:
Jillian Hay-Roe, BSN, CIC
Begin Now
Read Course | Complete Survey | Claim Credit
➀ Read and Learn
The following course content
Introduction
If you ever care for patients with orthopedic knee problems, you will certainly be familiar with Anterior Cruciate Ligament (ALC) tears. It is the most common knee ligament tear. This injury always presents with knee pain. Knee pain affects millions of people every year, necessitating medical care to provide relief and restore function. Surgical treatment is often required to return individuals to their original capacity.
There is a 50% likelihood that an ACL tear occurs with a knee meniscus tear. There is a high likelihood that you or someone you know personally has experienced one or both of these problems. It is bound to pop up when reviewing patients’ surgical histories. Since this is such a common problem, it is worthwhile to explore this subject in depth.
This course will primarily focus on ACL and knee meniscus tears since they are the most common cause of knee pain related to an injury. They are also likely to occur together.
Basic Anatomy Review and Definitions
Numerous muscles, nerves, and blood vessels support the knee and leg, but we will try to keep the anatomy review as brief as possible and cover structures relevant to the topic at hand.
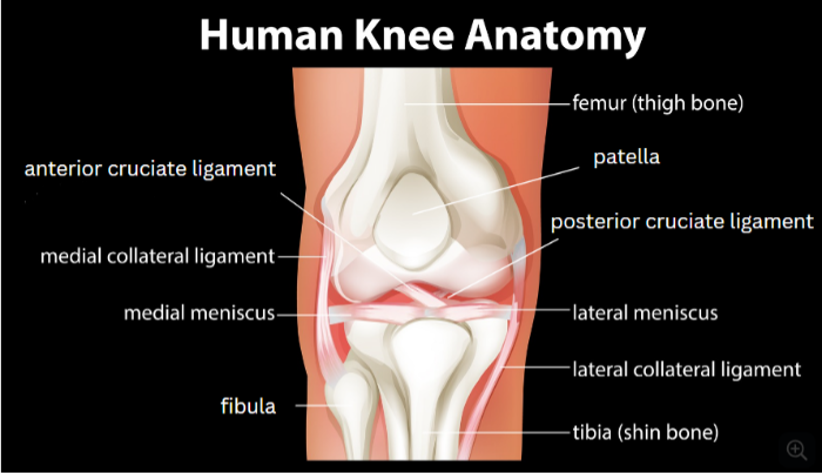
Knee Bones
The knee is the largest joint in the body. Three primary bones make up the knee joint. The ends of the bones are all covered with articular cartilage where they come together.
- Femur – the thigh bone which supports the upper leg. It is the largest bone in the body. The bottom end of this bone that forms the knee is in two spherical prominences referred to as condyles.
- Tibia – the shin bone supports the lower leg. It is shorter and thinner than the femur. The top of this bone which is a part of the knee is flat in shape. The fibula is the other smaller, shorter bone in the shin that is behind the tibia.
- Patella – the knee cap. It is a round convex triangular shape that points downward. It sits in between and in front of the condyles of the bottom of the femur.
[1] [2] [3] [4]
Ligaments
Four primary ligaments of the knee work in conjunction with leg muscles to make the knee bend. Ligaments are composed of collagen. Two are on the sides of the knee, and two are on the inside of the knee joint. When a knee injury occurs, tears can happen to one or more of these ligaments simultaneously.
- Collateral Ligaments – These two ligaments are on the sides of the knees. They function to control the side-to-side motion of your knee and brace it against swinging out too far.
- Medial Collateral Ligament (MCL) is on the inside side of the knee, and they face each other.
- Lateral Collateral Ligament (LCL) is on the side of the knee, facing outward.
- Cruciate Ligaments – These two ligaments are on the inside of the knee joint, behind the knee cap. They cross over each other to form an ‘X.’ They work to allow the knee to bend forward and back (flexion and extension – more on that below).
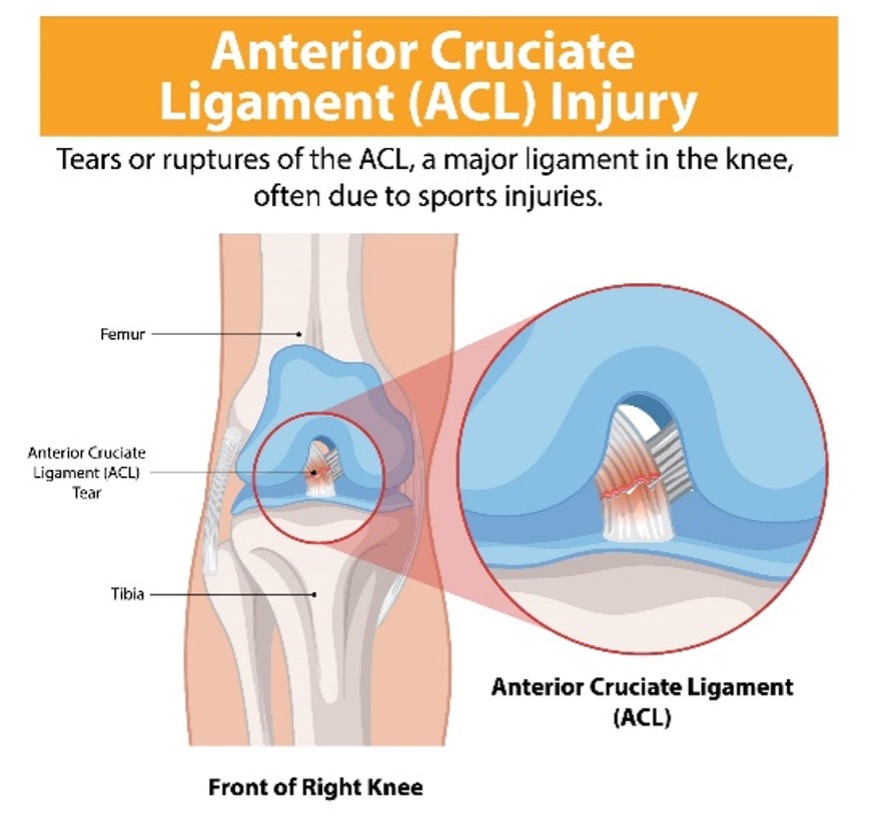
- The anterior cruciate ligament (ACL) is behind the knee cap. It runs diagonally from the kneecap toward the back of the tibia. It provides stability and prevents the tibia from sliding out in front of the femur.
- The Posterior Cruciate Ligament (PCL) – is behind the ACL and provides contrasting support to the tibia, keeping it from moving backward too far. The PCL is stronger than the ACL and is less likely to sustain an injury.
Other Knee Joint Components
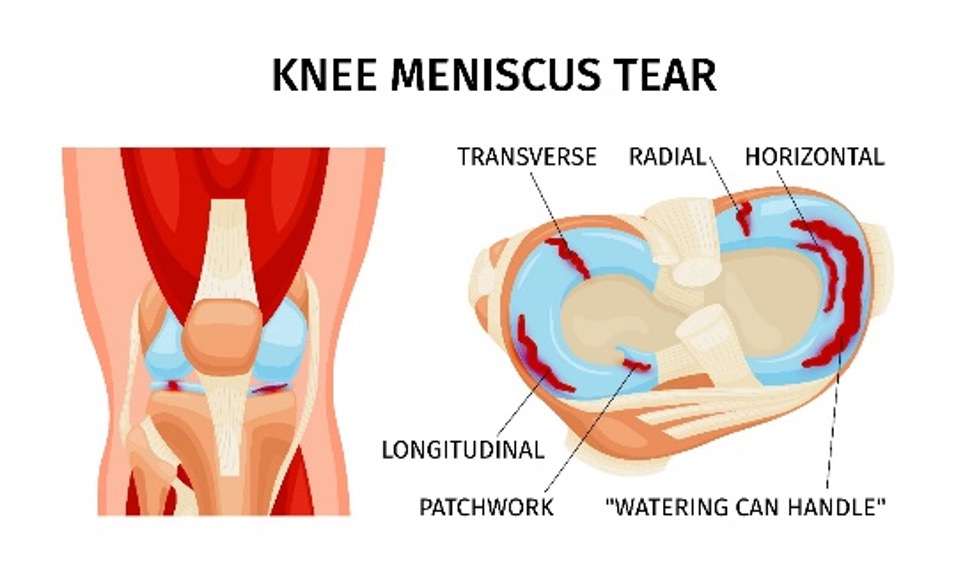
- Knee Meniscus – Two rubbery wedge-shaped pieces of fibrocartilage that sit between the femur and tibia behind the ACL and underneath the patella. They are shock absorbers and transmit weight from one bone to another. They play an essential role in knee stability. The meniscus is a separate structure from the articular cartilage at the bottom of each of the knee joint bones.
 [B]
[B]
Knee Positions
Included are some other key terms to review that arise when treating knee problems.
- Knee Extension – describes the ability to straighten your leg. A full extension would be documented as 0°.
- Knee Flexion – the ability to bend the leg (pull the calf muscle up to meet the back of the thigh). A fully flexed leg would go all the way to 150°.
The knee can also be turned inward toward the other leg by 10°, and outward by 30°.
[5]
Knee Abnormality Definitions
- Knee valgus – This is a term that refers to an abnormal posture made with the knee. This is when the knees are ‘knocking’ medially inward together. Valgus posture during jumping can lead to ligament injuries.
- Knee varus – This is the opposite when the knees are abnormally aligned outward to the side. This would appear ‘bowlegged.’
- Effusion – this is an accumulation of fluid in an abnormal location. This course applies specifically to fluid accumulation inside the joint. This is different from edema, which is the accumulation of fluid in the soft tissue of the muscles and extravascular spaces.
- Hemarthrosis – A condition of articular bleeding into the joint cavity. Patients will typically present with pain, swelling, and a decreased range of motion. [7]
[6]

Self Quiz
Ask yourself...
- What anatomical structures of the knee are most likely to be injured and why?
- When knee structures are injured, what presenting symptoms do you anticipate?
Pathophysiology – What goes wrong [1] [3]
An injury to knee structures often occurs when there has been abnormal, quick, jarring movement of the knee. ACL can be injured by changing direction rapidly, sudden stops, changes in running speed, a bad landing from a jump, or a collision that makes direct contact. This often occurs when playing sports. During these movements, the knee can pivot, and the tibia will turn anteriorly while the knee is slightly flexed and in a valgus position.
Knee ligament injuries are classified as sprains. They vary in severity:
Grade 1 |
Grade 2 |
Grade 3 |
| The ligament has mild damage. It is slightly stretched, but knee joint remains stable. | Ligament stretched to the point where it has become loose. This is referred to as a partial tear. |
Ligament has sustained a complete tear. The knee is unstable. This refers to either of the following types of injuries.
|
[C]
Meniscal tears can occur from acute trauma (e.g. a sports injury) or can result of degenerative changes (i.e. the normal aging process). Pivoting or twisting the knee are likely causes of meniscal tears. The three common types of meniscal tears are a Bucket Handle, Radial, and Flap.
[D]

Self Quiz
Ask yourself...
- Do you think a grade 3 ACL tear is more likely to be torn through the middle or be detached from the bone? What motions do you think would result in each?
- When an abnormal twist occurs, what structure or mechanisms do you think causes the meniscus to tear?
Epidemiology – How Common is this?
The most common knee injury is a meniscus tear. Most ACL injuries are Grade 3 complete or near complete tears. Approximately half of all ACL injuries occur concurrently with injuries to other knee structures, including other ligaments or the knee meniscus.
These movements often occur during sports, which is why the rate of ACL injuries is high among athletes. In particular, basketball, football, soccer players and skiers are prone to these injuries. However, it’s not just the pros who are susceptible to injury. A recreational pickleball player or a weekend warrior can also end up in a doctor’s office.
Females tend to have a higher incidence of ACL injuries compared to males. They also tend to sustain injuries at a younger age. The theory is that it could be related to differences in the pelvis, lower extremity alignment, or even looseness in ligaments, which can be influenced by estrogen. Physical conditioning, muscular strength, and neuromuscular control may be other potential factors.
[1] [2] [8]
Knee Injury and Surgery Statistics
- ACL Injury
- 1 in 3500
- Surgery- 400,000 a year
- Meniscal Tears
- 60-70 per 100,000
- Surgery – 850,000 a year

Self Quiz
Ask yourself...
- A 30-year-old physically active patient female presents with knee pain. What are some of the likely causes of knee pain?
- Besides the above-mentioned sports, what are some other sports, activities, or movements that could easily result in an ACL or meniscus tear?
- Why do you think a level 3 ACL sprain is the most common type of tear diagnosed?
Clinical Signs and Symptoms
Many of the symptoms of ACL and meniscus tear are the same. This should be no surprise since 50% of the injuries occur concurrently. The severity of symptoms is dependent on the extent of the injury. Generally speaking, an ACL tear tends to be more problematic than a meniscus tear because it leads to instability of the leg. Instability can lead to damage to the meniscus or articular cartilage.
[1] [2] [9]
| Torn ACL Symptoms | Overlapping Symptoms | Torn Meniscus Symptoms |
|
|
|
Case Study
A 42-year-old female, Ms. Smith, presents with knee pain and swelling. She has been a lifelong tennis player and still goes to play doubles every weekend with her partner. She reports that when she lunged to make a return volley, she felt her knee give way, causing her to fall to all fours.

Self Quiz
Ask yourself...
- What injury do you suspect?
- What factors contributed to this patient’s injury?
Assessment
Assessment consists of physical exam and imaging studies. Components of the physical exam will include: [1] [3] [4] [10]
- Subjective Assessment
- Patient reports of pain
- Sensation – burning, aching, dull, sharp, etc.
- Severity – utilization of a pain scale; changes in pain severity with movement
- Aggravating factors – which movements increase pain
- Relieving factors – medications, ice, activity modification, etc.
- Activities of daily living (ADL) limitations – Are patients having difficulty climbing stairs, or pain when they try to play their sport?
- Physical Assessment
- Obvious physical deformities – asymmetry, swelling (hemarthrosis), tenderness upon palpation
- Leg strength
- Presence of crepitus – audible when moving in addition to with palpation
- Abnormality in gait (i.e. limping)
- Range of Motion – There are several different tests that identify range of motion to help determine areas of knee injury.
- Tests for structural tears – A thorough knee exam includes several tests. Tests will be repeated on both legs for comparison. Included are just a few that test for torn ACLs and meniscus.
ACL Muscle Injury Tests
These tests are very accurate in allowing the provider to diagnose an ACL tear, even before an imaging study is done.
- Laxity Test – The patient is positioned supine. The patient will flex the knee and set the foot on the exam table.
-
- Anterior drawer sign – With the patient supine, ask the patient to flex the knee and set foot on the exam table. Immobilize the foot, grasp the head of the tibia with both hands and then pull toward the foot. Results: A movement greater than 1cm is considered a positive anterior drawer sign and is consistent with a tear.
-
- Lachman test – Flex the knee only 20-30°. Attempt to pull the tibia anterior, relative to the femur. If there is an ACL injury, there will be increased forward movement. This test is more sensitive than the anterior drawer test.
- Lever Sign Test – Performed by positioning a fulcrum (e.g., examiner’s fist) under the proximal part of the supine patient’s calf and applying a downward force to the quadriceps (distal thigh). The test is interpreted based on whether the ACL is intact or not; the patient’s heel will either rise off of the examination couch or remain down.
Meniscus Tear Tests
- McMurray Test – This test is conducted with the patient fully supine and the knee fully flexed.
-
- Lateral Meniscus tear – The provider will place their forefingers on the lateral side of the joint line, then by applying valgus stress and internal rotation of the leg, extend the knee, looking for pop, click, and pain.
-
- Medial meniscus tear – The provider will place forefingers on the medial side of the joint line, then apply varus stress and internal rotation of the leg, and extend the knee looking for pop, click, and pain.
Imaging Studies
Typically, the next step is to get an X-ray. The X-ray will not show the soft tissue, meniscus, or ligament tears, but it will be used to identify any possible causes of knee pain. X-rays will be used to find problems with the bones which can be contributing to knee problems.
Particularly, an X-ray can identify problems with the articular cartilage at the end of the bones, leading to a diagnosis of arthritis.
To look at the soft tissues, an MRI will be ordered. These allow the provider to visualize the location, and degree of tears in ligaments and meniscus and any other soft tissue abnormalities. The MRI is particularly helpful in identifying meniscus tears. Alternatively, a CT scan and ultrasound may be sufficient to visualize injuries.
[3]

Self Quiz
Ask yourself...
- A patient presents with knee pain. In what order should the provider move through their exam?
- Based on pathophysiology, do you think it is easier to diagnose an ACL injury or a meniscus injury?
- A provider obtains an X-ray of a patient’s knee, but everything appears to be within normal limits. How would the provider proceed to diagnose the cause of knee pain?
- What additional tests would the provider perform?
Treatment
During the diagnostic appointment, the provider will recommend treatments for the patient. The provider can make some general recommendations that don’t require a prescription or order. [2] [9]
The RICE(D) Treatment [2]
- Rest – Limit movements, activities or sports that aggravate the ligament tears. The tear can worsen over time if it continues to be strained. A patient may be unable to work, depending on their job duties. Crutches or a brace may be recommended.
- Ice – May also help reduce swelling and decrease pain. Providers need to make sure to tell patients to take a break from the ice every twenty minutes and to protect the skin with a thin towel.
- Compression – Wearing a compression sleeve, wrap or brace can help the patient to maintain stability.
- Elevation – Elevation helps to reduce swelling which accumulates with gravity. Swelling creates additional pressure in the knee which increases pain. The patient should keep the leg up and extended when possible.
- Drugs – This is a recommended treatment, but not a part of the traditional RICE acronym (this author thinks it would be a helpful addition). Over-the-counter non-steroidal anti-inflammatory drugs (NSAIDs) can be taken as needed for pain. If non-opioid pain medications are not sufficient to keep pain tolerable, other therapies should be considered before a long-term opioid prescription regimen should be considered.
These treatments are common sense, and most people try them before even seeking advice from a provider. The next treatments do require a provider’s order.
- Physical therapy is a very important part of recovery from these injuries. Strengthening other supportive muscles, while preventing further injury to the tear, can help to improve function. Physical therapy may be enough to help the patient restore adequate function without needing surgery.
- Cortisone Steroid Injections – Steroids that have an anti-inflammatory effect are injected directly into the knee area. Evidence identifies that it does not change a patient’s pain levels, but it can have a positive effect on ACL healing. [11]
- Platelet-rich plasma – (PRP) Is a relatively new treatment that is increasing in popularity as research continues to determine its efficacy. For PRP, a blood sample of approximately 30-60mL is drawn from the patient. The sample is then centrifuged to separate blood components. The patient’s plasma, which has a high level of concentrated platelets, is then injected back into the injured joint area. It is hypothesized that the platelets release growth factors that aid in tissue repair. A word of caution: this therapy may not be covered by health insurance. [12]
Case Study
Case Example: The orthopedic surgeon reviews Ms. Smith’s imaging results and performs a focused physical exam. The surgeon, Dr. Brone, explains that she has a
Grade 3 ACL complete tear and a lateral meniscus tear.
Dr. Brone has discussed treatment options with Ms. Smith. She already had to stop playing tennis about three weeks ago due to the pain and has been taking NSAIDS PRN. She will start using ice. She is interested in learning more about PRP treatment since she had a friend report good results when she had tennis elbow.

Self Quiz
Ask yourself...
- What exercises and activity parameters should the provider recommend to Ms. Smith?
- What information should the provider include with discussing PRP treatment with Ms. Smith?
Surgical Treatment
It is always best to avoid surgery unless necessary. However, it is often necessary because an untreated tear can result in other knee problems down the road.
|
ACL Surgery is Recommended |
Non-surgical Treatment |
|
|
|
|
|
Meniscus Surgery is Recommended |
Non-surgical treatment |
|
A tear in the ‘white zone.’ The white zone makes up two thirds of the meniscus that does not have a significant blood supply. Blood flow is necessary to bring in healing factors. Tears in this area are less likely to heal on their own. |
A tear in the ‘red zone.’ This is the outer one third of the meniscus that does have a significant blood supply where the tissue has a greater likelihood of healing naturally. |
Consideration – An ACL injury is not uncommon in pediatric athletes. For young children or adolescents with ACL tears, early ACL reconstruction creates a possible risk of growth plate injury, leading to bone growth problems. The growth plates can be avoided by using certain surgical techniques. Despite the increased risks this population has with surgical repair, recent evidence has shown that delaying treatment can lead to a higher rate of future meniscus or cartilage injuries. [9]

Self Quiz
Ask yourself...
- A patient states they are miserable with knee pain and wishes to proceed directly to surgery. How should the healthcare provider respond?
- A patient states their sibling had a similar knee problem 20 years ago, and nothing helped much. How should the healthcare provider respond?
- A 13-year-old has a level 3 ACL sprain during volleyball practice. What does the provider need to consider when developing a treatment plan? How should the provider discuss the treatment plan with the parents?
Knee Arthroscopic Repair Surgery
ACL reconstruction and knee meniscus surgeries are usually elective surgeries and are relatively safe. They are typically done arthroscopically, where only two to three small incisions (approx. 1cm long) are made. The small incisions are referred to as portals and allow for surgical implements to be inserted into the patient. The implements that go into the portals include:
- Arthroscopic camera – This small camera is used to visualize the area. The picture is displayed on a large monitor inside the OR.
- Irrigation fluid – Several large bags of sterile normal saline are hung on poles and run through the patient’s operative area. The fluid enlarges the area for the repair to be made, and also prevents bleeding in the open space.
- Surgical Instruments – Surgical tools are designed to be very small to fit through the portals. These include forceps, graspers, drills and shavers.
Multiple portals are needed to place the necessary arthroscopic camera to visualize the area on a large monitor, the irrigation fluid, and instruments that allow the surgeon to make the repair. These incisions are placed a few inches apart around the knee cap.
Arthroscopic surgeries result in less pain and joint stiffness and often have shorter recoveries than previous surgical techniques. The surgery usually can be done in an outpatient surgery center (more about that below). The patient can go home after spending an hour or two in the recovery room.
[4] [9]

[E]

[F]
During ACL surgery, often other procedures are also completed, especially fixing torn meniscus. However, a patient with intact ligaments may have surgery just to address a meniscus tear. Meniscus surgery is a simpler, quicker surgery than an ACL reconstruction and is usually completed in under an hour. Patients can be fully weight-bearing without crutches immediately post-op.
There are two main types of surgery done for a meniscus tear:
- Partial meniscectomy – The damaged meniscus tissue is trimmed away.
- Meniscus repair – Depending on the type of tear and condition of the injured meniscus, it may be better to repair the meniscus rather than remove it. The recovery time for the patient will be longer as the tissue needs to heal back together.
ACL reconstruction surgeries also have varying types. The ACL is surgically repaired by using graft tissue. There are two primary types, each with their own pros and cons.
| Graft Type | Pros | Risks | |
|
Autograft (from the patient)
|
Patellar Tendon |
|
|
| Hamstring Tendon |
|
|
|
| Quadriceps Tendon |
|
|
|
|
Allograft (Cadaver donor tissue)
|
Patellar tendon, Achilles tendon, semitendinosus, gracilis, or posterior tibialis |
|
|
Both autograft and allograft reconstruction are highly effective. Recent studies show little difference in failure rates between autografts and allografts (about 6% and 7%, respectively). Allografts cost more, since they need to be carefully harvested, tested, treated, sterilized and transported. The cost-effectiveness of autografts and high efficacy make it a first choice. [13]
The surgeon will of course discuss with the patient what would be the best graft for their specific injury. Together they will decide what graft they plan to use. Patients who will use an autograft may have additional incisions made for the tissue to be harvested. For patients who either elect or who wouldn’t be good candidates for autograft reconstruction, the nurse will be integral in ensuring the facility has received the donor graft that is stored appropriately and that the right documentation is present. The one who receives the tissue delivery needs to inspect it and complete the documentation record.
The information that should be recorded includes:
- A description of the package integrity upon receipt
- Transport and storage temperatures are controlled and within acceptable parameters
- Tissue identification numbers
- Date and time of arrival
- Name of the person who accepted the delivery
[14]
Case Study
It has been determined that Ms. Smith should proceed with ACL surgery which will include a meniscectomy. She asks the nurse the following questions, please consider your response:
- What kind of scar will I have after this surgery?
- If I have an autograft, will I lose strength in my leg by cutting up another tendon?
Surgery Location – Hospital VS. Ambulatory Facility
These elective surgeries are increasingly performed at ambulatory surgery centers. A patient has multiple comorbidities that put them at high risk of a complication would need to have this surgery performed at a hospital. A hospital has additional resources that can be provided in the event of an emergency. Patients who may require a blood transfusion, or an overnight stay in an inpatient unit would be candidates for surgery at a hospital. However, most patients can safely have surgery at an outpatient center. It is much more cost effective and patient satisfaction tends to be higher.
[15] [16]

Self Quiz
Ask yourself...
- What chronic conditions or comorbidities would require a patient to have surgery at a hospital?
- What factors do you think increase patient satisfaction at an ambulatory surgery center?
Pre-operative Care
Standard pre-operative care will apply to a knee surgery patient. Nurses often prepare the patient for surgery, which includes providing education about what to expect on the day of surgery. They will review the patient’s medical history and medications and alert the surgeon and anesthesiologist if there are any red flags to be further assessed. For example, a patient with multiple comorbidities including diabetes, renal failure, and COPD should be scheduled for surgery at a hospital, rather than at an outpatient surgery center.
Once the patient has arrived at the surgery center, a pre-operative nurse will review medical history, inform the surgeon that he has completed it, and perform a brief physical assessment. The pre-op nurse will get the patient into a gown, make sure there is IV access, and apply a cardiac ECG monitor, blood pressure cuff, and pulse oximetry. Hair on the extremity that may interfere with the incisions or dressing may need to be clipped. They may also prepare prophylactic IV antibiotics that should be administered no more than one hour prior to surgery start time. Throughout the perioperative process, along with the OR nurse, they make sure safety time-out checks are performed.
[4]
A Note about Informed Consent
It is the physician’s responsibility to conduct informed consent with the patient before the surgery. Informed consent means that the surgeon has explained what will happen during the surgery and the benefits and risks of the procedure in a way that the patient understands. The patient must have the opportunity to have any questions answered.
It is the duty of the nurse to ensure that all aspects of the conversation have occurred between the doctor and patient or their guardian/power of attorney. The patient and doctor will then sign an informed consent document that contains all this information. The nurse may need to also sign the document that they witnessed the informed consent process. On the day of surgery, the informed consent document will be verified to ensure that it was properly completed and that the correct procedure is being done for the correct patient.
Knee Surgery Benefits and Risks Discussed
The benefits of the surgery are straightforward. The procedure is being done because it will help restore knee function, reduce pain, reduce the chance of further tissue damage, and overall improve the patient’s quality of life. The surgery is necessary due to the nature of the tear, natural healing and other conservative treatments have proven to be ineffective at allowing the patient to return to baseline status. Risks of anesthesia need to be included. This includes the risk of pneumonia, aspiration, and respiratory failure. [9]
The following risks of knee surgery should be discussed with the patient by the surgeon:
- Infection
- Bleeding
- Nerve Damage
- Chronic Instability
- Stiffness Blood Clots
- Rupture or Fracture
- Growth Plate Injury
While some risks can happen during the surgery, there are chances problems will arise after the patient has been discharged. Patients should be educated that they need to adhere to discharge instructions, so they don’t cause a problem leading to a negative outcome. For example, the procedure was conducted with perfect sterile technique, but the patient didn’t follow instructions regarding wound care, which can lead to an infection.

Self Quiz
Ask yourself...
- The surgeon discusses informed consent, and the patient becomes very concerned about the risks involved. How can the healthcare provider respond?
- A 16-year-old patient requires knee surgery. Who should be involved in the informed consent process?
A Note about Nerve Blocks [17]
A nerve block is a procedure done before ACL surgery to provide analgesia for the patient. It is usually not needed for just meniscus surgery. This procedure is done by administering an injection of a numbing medication around a major nerve in the leg, which will cause a decrease in sensation, pain, and control of the extremity by approximately 70%. The effects of the nerve block can last anywhere from 6-72 hours. This helps reduce the amount of anesthetic medication given to the patient during surgery and reduce the amount of pain and subsequent opioid medication the patient will need post-operatively. Typically, a nerve block procedure will then be performed by an anesthesiologist in pre-op, and nurses may need to assist with this procedure.
Initially, femoral and sciatic nerve blocks were commonly used but were associated with motor blockade, an increased risk of falls, delayed ambulation, and delayed discharge. These motor blocks have been replaced by adductor canal block (ACB) and Infiltration between the Popliteal Artery and Capsule of the Knee (IPACK) block.
These blocks provide analgesia without affecting the motor strength of the leg. A combination of both these blocks has demonstrated positive outcomes in knee arthroscopy surgery. The latest advancement is with the blockade of the genicular nerves, the articular branches of the knee. This is because the knee joint has a complex neural innervation, formed by several nerves that neither ACB nor IPACK blocks can fully cover.
Nerve Block Procedure
The anesthesiologist uses a point-of-care ultrasound machine to locate the nerve bundles at various locations along the leg. They then will use a long needle to inject between 15-30mL of bupivacaine, or other similar numbing medication just around the nerve. Depending on the nerve pathways the anesthesiologist intends to numb, they may inject at a few different points in the leg.
Prior to this, the patient will either be given moderate sedation or will already be put under surgical anesthesia. Pre-op sedation is done with a benzodiazepine, like Midazolam (Versed©), and possibly an opioid like Fentanyl. Of course, each process will vary between each surgery center, and each anesthesiologist, who develops a custom plan for each patient.
nerve block is usually done with sedation for a few reasons. Moderate sedation allows the patient to feel relaxed. Most people already feel some degree of anxiety before surgery. Allowing the patient to relax helps decrease the chances the patient will flinch or move during this procedure. The procedure involves a large needle injecting a large amount of fluid, which can be a scary experience for people, even though it only causes minor discomfort. Besides, the patient is already NPO and will be receiving general anesthesia for the surgery anyway. However, it is helpful to keep the patient somewhat awake because they can let the anesthesiologist know if they feel nerve contact, which is a zing or electrical sensation down the nerve if the needle has made contact.

Self Quiz
Ask yourself...
- What is important for the patient to know about the nerve block post-operatively?
- The patient asks why the surgeon doesn’t inject numbing into their knee during the surgery. How can the nurse or anesthesiologist respond?
Inside the Operating Room
OR Table Positioning [18] [19]
Positioning is very important so that the surgeon can access the structures at the precise necessary angles. The nurse will position the patient based on surgeon preference. The surgeon may opt to sit during the procedure. Options for positioning include positioning with the patient supine flat on the table or positioning the patient supine with the knee in a leg holder. For the supine position, it requires a valgus post, a bump placed under hip, and a bump placed on at the foot of the table to assist with knee flexion. Lithotomy leg holders in low position may be used. In low lithotomy, the hips should be flexed no more than 60° from the table’s surface. Too much flexion or abduction can injure the sciatic nerve. Sometimes a padded Mayo stand is used.
While the surgeon directs all of their focus on the surgical area, the nurse’s focus spans the entire patient. They must consider protecting muscles, nerves, bony prominences, and the skin. Nurses need to give extra care to high-risk patients such as the elderly and those with comorbidities, especially diabetes or vascular disease. A skin assessment needs to be done (and documented) pre-operatively to see if there are any lesions that are already present.
The circulator nurse must ensure that there is adequate padding underneath the body. Bony prominences, in particular, should be checked. Even specialty booties or padding are placed on the feet to protect the heels.
For ACL surgeries, a pneumatic tourniquet (which can be inflated/deflated to apply/release tourniquet pressure) will be placed on the patient’s thigh. The nurse needs to be familiar with the equipment components (e.g. are the cuffs single use, will the patient need to have a stockinette or padding placed on the leg under the tourniquet). [20]
Sequential compression devices (SCDs) are typically included in facility protocol to prevent development of VTE (venous thromboembolism) and are applied to the calves of any patient undergoing a procedure that is anticipated to be 30 minutes or longer.
The patient will have safety straps applied at different points to keep them in place on the operating room table. Orthopedic procedures can require substantial manipulation, and the patient may shift around on the narrow OR table.
Sterilely Prepping the Patient [21]
Once the patient is safely positioned on the operating room table the skin anti-septic preparation can begin. One member of the surgical team will hold the patient’s operative limb up and away from the body. Another member will cleanse the patient’s skin extensively, far exceeding the boundaries where surgery will be performed. Cleaning starts with the incision areas first, the top of the knee, and will extend outward to the other areas of the leg. If an autograft surgery is planned, the area of extraction will also require sterile preparation. A brightly colorful chlorhexidine solution will be used, either by itself or in combination with an alcohol solution. The bright color of the solution helps indicate the areas that have been prepped.
Drapes with adhesive edges will be placed, covering the entire patient except for the surgical area. The incision sites will be marked. The knee may be covered with a transparent surgical adhesive drape (IO-ban, which is similar to a Tegaderm except bigger and thicker and has an antimicrobial solution embedded in it) that the surgeon cuts directly through.

Self Quiz
Ask yourself...
- If the sterile technique is broken during the prepping phase, how should the surgical team proceed?
- A patient asks why their surgical leg is a bright orange after surgery. They are concerned it might be infected. How should the nurse respond?
Arthroscopic Surgery Specifics [9]
Once the arthroscope and instruments are in place, the surgeon will examine the condition of the knee, trim or repair any meniscus and cartilage injuries, and then remove the torn ACL stump. In the most common ACL reconstruction technique, the surgeon drills bone tunnels into the tibia and the femur so they can place the ACL graft in a way that is as anatomically correct as possible.
During this time, a surgical assistant, usually a physician’s assistant or nurse practitioner prepares the graft. They ensure it is the correct length and there is no muscle tissue attached. Once the graft is placed into the knee, it is held under tension and fixed in place with permanent sutures and anchors, which will remain in the patient.

Self Quiz
Ask yourself...
- A patient who had a right ACL repair with an autograft asks why there aren’t any bandages on their left leg. The patient states they thought the surgeon was going to use the graft from their own leg tissue. How should the nurse respond?
- The patient asks the nurse if the stitches will dissolve or if they need them removed. How can the nurse respond? What should the nurse include about implanted sutures?
Implants
Suture anchors are broadly used for attaching soft tissue (e.g., tendons, ligaments, and meniscus) to the bone. Suture anchors are continually changing to become safer and more efficient. The primary function of the suture anchor is to attach tissue at the proper site and maintain its position without loosening or excessive tension until physiologic healing is accomplished. An ideal suture anchor is easy to handle, maintains enough pull-out strength, prevents suture abrasion, and is absorbable without resulting in any reactions as the material dissolves.
The surgeon should consider the status of bone quality, predictable complications, material-related adverse reactions, and the need for potential future revision surgery when determining the most appropriate suture anchor. The following are a few different types of materials that can be used:
- Metal Anchors – Although metallic suture anchors provide rigid fixation and have been used successfully for a long time, multiple disadvantages are associated with their use. The complications include migration, loosening, or irreversible imbedding and interference with diagnostic imaging including CT and MRI scans. Therefore, other anchor materials are preferred.
- Biostable Anchors (e.g. PEEK (Polyether ether ketone) – Are a non-degradable plastic. PEEK materials showed high strength, strong mechanical properties, good wear- and heat resistance, and excellent chemical and biological resistance. The patient can safely undergo airport metal detector screenings and MRIs without any concerns.
- Biocomposite Suture Anchors – are metal-free and composed of both a biodegradable polymer material and a bone formation-promoting bioceramic material. Some completely absorb into bone tissue within a few years.
- All-soft suture anchors (ASAs) – Were developed to minimize complications and invasiveness related to the use of solid-type anchors. The sutures are passed through a fabric anchor sleeve or tape made of an ultrahigh molecular weight polyethylene (non-metallic).
[22]

Self Quiz
Ask yourself...
- What instructions should the nurse give to a post-op ACL patient regarding going through metal detectors or having an MRI?
OR Circulator Nursing Duties [4]
In addition to the standard tasks performed by an OR circulator nurse in any surgery, the following are specific for knee arthroscopic procedures:
- Arthroscopic Fluid – Large, 3-liter bags of sterile normal saline are continually irrigated through the joint space. An important role of circulator nurses is to monitor fluid bags and change them out as needed during the procedure.
- Arthroscopy Tower – During the surgery, the nurse may also need to assist in adjusting arthroscopic screen images and monitors.
- Implants – To attach the graft to the bone, the surgeon will implant permanent sutures and anchors into the patient. Nurses often work with implant manufacturer sales representatives who are present in the operating room during the surgery. Nurses must make sure that the correct sizes and materials are available and have not expired.
After the surgery has been completed, the portals will be closed with sutures and possibly surgical glue and then covered with sterile strips (small white stickers). An outer bandage will then be applied. The OR nurse along with the scrub technician will complete an instrument count to make sure that no unintentional items, like suture needles, were left inside the patient. Drapes are removed, the anesthesiologist begins to arouse the patient, and they are placed back onto a gurney to be brought into the Post-Anesthesia Care Unit (PACU).

[G]
Post-Operative Care
Post-operative care for an ACL surgery patient is usually straightforward and routine, especially when the patient has received an effective nerve block. Routine postoperative care applies, which includes monitoring vital signs, assessment of the level of consciousness, surgical site dressing and distal extremity appearance and circulation, pain, nausea, and PO tolerance.
Most patients are discharged directly home, usually within an hour or two of leaving the OR. The PACU nurse needs to review education again, preferably with the support person who will be taking the patient home.
When patients have received a nerve block, they will need crutches. If the patient has not been fitted for crutches before surgery, the nurse will need to adjust them to an appropriate height and educate the patient how to ambulate with them. This will be an extra challenge for a patient who is still discombobulated from anesthesia and has limited sensation in their operative leg. Depending on the repair made, the surgeon will specify the level of weight bearing (non, partial, full) appropriate for the patient.
The patient may also receive a specialized brace to keep the knee stabilized. This can also require proper fitting and education for the patient. Some can be locked or unlocked at certain angles. The surgeon must provide clear orders on locking the brace, and if the patient can remove it at rest.
[9]
Post-Operative Education [9]
Post-Operative Education should be reviewed at many different points throughout the patient care experience. It should start with physician consultation appointments and continue on the day of surgery, both pre- and post-operatively. Anxiety and the effects of anesthesia can greatly impact the patient’s ability to recall instructions, so repetition is important. Including the patient’s supportive caregivers is very helpful.
- General Recovery – Review the expected side effects of anesthesia, which include tiredness, and limited mental abilities.
Patients should be given information on what symptoms may constitute an emergency, and when they should follow up with their doctor. For example, if a patient is very difficult to arouse, or is having difficulty breathing.
- Dressing and Wound Care – Surgeons have varying preferences about when it is okay to remove the bandage and resume showering. The surgeon may allow the patient to shower the day after surgery, and some prefer the patient to wait until their follow up appointment. All recommend waiting for incisions to heal for a few weeks before the patient is able to submerge the area in water through swimming or bathing. Signs and symptoms of infection or complications such as bleeding should also be reviewed.
- Activities and Movement – Again, depending on the type of repair made and surgeon preference, there will be limitations on when the patient can resume different activities. It may be 1-3 weeks before a patient can resume driving.
Generally speaking, the patient should be encouraged to encourage light circulation in the extremity by wiggling toes, doing ankle circles. Lifting weights should be avoided, and even simple activities such as squatting or bending down to pick something up may need to be cautioned against.
- Physical therapy may be recommended to begin immediately after surgery or may not start for a few weeks. The patient should also be provided with a home exercise plan.
- Patients should be encouraged to take short walks frequently. When they are sitting, they should keep their legs elevated. This will help reduce swelling in the knee, and an overall decrease in pain. If propping up the leg on pillows, they should be placed behind the calf or ankle. Putting a pillow directly behind the knee can impede circulation of the popliteal vessels. This can decrease healing and increase risk of deep vein thrombosis (DVT formation).
- Rehabilitation time for a meniscus repair is about 3 to 6 months. A meniscectomy requires less time for healing — approximately 3 to 6 weeks.
- An ACL recovery can be longer, usually several months. A patient may need to stay away from intense sports for 6-12 months.
- Pain management – A big category of education is on pain management. Patients experience great pain relief following the nerve block. However, once this wears off 6-72 hours later, pain can be very unpleasant. For most patients, the first three days are the worst. Things should then continue to improve each day. There are three main analgesic interventions:
-
- Non-pharmacologic – The most common is applying ice to the affected knee. This helps reduce swelling and thereby pain. Patients must be reminded to protect the skin with a towel and to keep the incisions dry. They want to remove the ice at regular intervals so that blood can recirculate to the area which promotes tissue healing. Repositioning and small movements can also help. Elevation is also important to decrease swelling. Swelling increases pressure in the area which can add to the pain sensation.
-
- Non-opioid Medications – Non-steroidal anti-inflammatory medications (NSAIDS). These are appropriate for mild to moderate pain (approximately 2-6/10 of a numeric pain scale).
-
- Opioid Medications – Opioids (e.g. Oxycodone, Percocet, Tramadol) are being prescribed with increasingly strict parameters. These drugs are very effective in treating pain, but they must be taken with caution.
-
-
- Surgeons should prescribe only a small quantity of medications, initially just enough to get the patient through the first three days.
-
-
-
- Patients requiring pain relief for severe pain (> or = 7/10) should be evaluated by the provider for a prescription renewal.
-
-
-
- Nurses should highlight safety concerns about not driving while on opioids, and not mixing with alcohol or cannabinoids.
-
-
-
- Patients may be advised not to return to work or school while they are taking these medications.
-
-
-
- They should also be informed about common side effects of nausea and constipation, and how to reduce these.
-
If patients try to stoically recover without using any medications, they may avoid using the leg at all. This will decrease circulation and the healing process, overall leading to a suboptimal outcome. They may not achieve full recovery of range of motion or strength.
Patients can use all three pain relief strategies simultaneously. They should also wean off opioid medications as soon as it is tolerable and just take NSAIDS until they are no longer needed.
Case Study
Ms. Smith is given prescriptions for the following:
- Naproxen 800mg PO Q8 hrs PRN mild-moderate pain
- Oxycodone 5mg PO Q6-8 hrs PRN moderate-severe pain
Ms. Smith tells the post-op nurse she plans to attend a boat party in one week and asks the nurse if she will be able to have alcohol at the party.
What can the nurse tell the patient?

Self Quiz
Ask yourself...
- You are taking care of a patient who has a history of substance misuse and states they cannot take opioids during their recovery. How would the nurse develop a pain control plan of care for this patient?
- A patient states they were scared to take their opioid medications because they were afraid of addiction. What problems would the nurse anticipate? What should the nurse assess for?
- A patient’s family member asks the nurse when they should give the patient the next dose of pain medication when they get home. How can the nurse respond?
Conclusion
At this point, you hopefully know more about a single ligament than you ever wanted to know. Or perhaps it piqued your curiosity to learn more about other types of knee injuries and surgeries. There certainly is no shortage. If the problem is not addressed, it can create more problems in the long run. The silver lining with the widespread problem of knee pain is that the medical community has gotten lots of practice in diagnosing and treating it. Nurses play an important role in providing treatment for these patients, especially in the perioperative setting. As always, they are counted on to educate patients on how to complete their healing journey.
References + Disclaimer
- M. K. Mulcahey MD, “Anterior Cruciate Ligament (ACL) Injuries,” OrthoInfo, October 2022. [Online]. Available: https://orthoinfo.aaos.org/en/diseases–conditions/anterior-cruciate-ligament-acl-injuries/.
- M. J. Alaia MD and R. Wilkerson DO, “Meniscus Tears,” OrthoInfo, March 2021. [Online]. Available: https://orthoinfo.aaos.org/en/diseases–conditions/meniscus-tears/.
- J. Evans, A. Mabrouk and J. I. Nielson, “Anterior Cruciate Ligament Knee Injury,” 17 November 2023. [Online]. Available: https://www.ncbi.nlm.nih.gov/books/NBK499848/.
- M. J. Alaia MD and R. Wilkerson DO, “Knee Arthroscopy,” OrthoInfo, January 2022. [Online]. Available: https://orthoinfo.aaos.org/en/treatment/knee-arthroscopy/.
- InformedHealth.org [Internet], “In brief: How does the knee work?,” 24 August 2021. [Online]. Available: https://www.ncbi.nlm.nih.gov/books/NBK561512/.
- K. A. Krackow MD, “The Measurement and Analysis of Axial Deformity at the Knee,” 2008. [Online]. Available: https://www.medschool.lsuhsc.edu/ortho/docs/How%20to%20Measure%20Knee%20Alignment.pdf.
- M. Lombardi and A. C. Cardenas, “Hemarthrosis,” 31 July 2023. [Online]. Available: https://www.ncbi.nlm.nih.gov/books/NBK525999/.
- F. Mizuno RPT, S. Koganemaru MD PhD, H. Irisawa MD PhD, A. Saito PhD and T. Mizushima MD PhD, “Knee Valgus during Jump Landing Is Related to the Inaccuracy of Knee Position Recognition in Healthy Young Women,” 23 October 2021. [Online]. Available: https://www.ncbi.nlm.nih.gov/pmc/articles/PMC8530781/.
- M. J. Alaia MD, “ACL Injury: Does It Require Surgery?,” October 2022. [Online]. Available: https://orthoinfo.aaos.org/en/treatment/acl-injury-does-it-require-surgery/.
- M. Genovese MD, “Knee Exam,” Stanford Medicine 25, [Online]. Available: https://stanfordmedicine25.stanford.edu/the25/knee.html.
- C. Lattermann, C. A. Jacobs, M. P. Bunnell, L. J. Huston, L. G. Gammon, D. L. Johnson, E. K. Reinke, J. L. Huebner, V. B. Kraus and K. P. Spindler, “A Multicenter Study of Early Anti-inflammatory Treatment in Patients With Acute Anterior Cruciate Ligament Tear,” February 2017. [Online]. Available: https://pubmed.ncbi.nlm.nih.gov/28146402/.
- M. J. Alaia MD and F. B. Kelly MD, “Platelet-Rich Plasma (PRP),” OrthoInfo, January 2022. [Online]. Available: https://orthoinfo.aaos.org/en/treatment/platelet-rich-plasma-prp/.
- H. Mistry, A. Metcalfe, J. Colquitt, E. Loveman, N. A. Smith, P. Royle and N. Waugh, “Autograft or allograft for reconstruction of anterior cruciate ligament: a health economics perspective,” Springer, 14 March 2019. [Online]. Available: https://www.ncbi.nlm.nih.gov/pmc/articles/PMC6541574/.
- V. Steelman, “Banking on Allograft Safety,” AORN, 10 October 2007. [Online]. Available: https://www.aorn.org/outpatient-surgery/article/2006-November-banking-on-allograft-safety.
- J. Tiao, K. Wang, A. D. Carbone, M. Herrera, N. Zubizarreta, J. N. Gladstone, A. C. Colvin and S. G. Anthony, “Ambulatory Surgery Centers Significantly Decrease Total Health Care Expenditures in Primary Anterior Cruciate Ligament Reconstruction,” January 2023. [Online]. Available: https://pubmed.ncbi.nlm.nih.gov/36453721/.
- S. A. Krywulak, N. G. Mohtadi, M. L. Russell and T. M. Sasyniuk, “Patient satisfaction with inpatient versus outpatient reconstruction of the anterior cruciate ligament: a randomized clinical trial,” June 2005. [Online]. Available: https://www.ncbi.nlm.nih.gov/pmc/articles/PMC3211553/.
- V. Ramanujam, S. DiMaria and V. Varma, “Ultrasound-Guided Genicular Nerve Blocks for Anterior Cruciate Ligament Reconstruction Surgery in an Outpatient Setting: A Case Series,” 1 September 2023. [Online]. Available: https://www.ncbi.nlm.nih.gov/pmc/articles/PMC10544945.
- C. Wheeless MD, “Positioning and Setup of ACL Reconstruction,” Wheeless’ Textbook of Orthopaedics, [Online]. Available: https://www.wheelessonline.com/joints/positioning-and-setup-of-acl-reconstruction/.
- ”Positioning Is Paramount in Orthopedics,” AORN, 14 July 2020. [Online]. Available: https://www.aorn.org/outpatient-surgery/article/2020-July-positioning-is-paramount-in-orthopedics.
- j. McEwen, Outpatient Surgery, 25 July 2013. [Online]. Available: https://www.aorn.org/outpatient-surgery/article/2013-August-4-keys-to-safe-tourniquet-use.
- World Health Organization, “Surgical Site Infection Prevention,” 2016. [Online]. Available: https://cdn.who.int/media/docs/default-source/integrated-health-services-(ihs)/ssi/fact-sheet-skin-web.pdf?sfvrsn=ead06f37_2#:~:text=Surgical%20site%20skin%20preparation%20is,skin%20around%20the%20incision%20site..
- C.-H. Cho MD, K.-C. Bae MD and H.-H. Kim MD, “Biomaterials Used for Suture Anchors in Orthopedic Surgery,” September 2021. [Online]. Available: https://pubmed.ncbi.nlm.nih.gov/34484619/.

Image References
- [B] brgfx on Freepik.com. Human Knee Anatomy diagram. https://www.freepik.com/free-vector/human-knee-anatomy-diagram_9741711.htm#fromView=search&page=1&position=24&uuid=bae55ff4-6bd6-4c67-b9a0-efeeae6ce70c
- [C] brgfx on Freepik.com ACL Injury ACL <a href=”https://www.freepik.com/free-vector/anterior-cruciate-ligament-acl-injury_222523509.htm#fromView=search&page=1&position=19&uuid=bae55ff4-6bd6-4c67-b9a0-efeeae6ce70c”>Image by brgfx on Freepik</a>
- [D] Macrovector on Freepik.com Knee Meniscus Tear https://www.freepik.com/free-vector/knee-meniscus-tear-anatomy-diagram-realistic-infographics-white-background-vector-illustration_33771055.htm#fromView=search&page=1&position=18&uuid=bae55ff4-6bd6-4c67-b9a0-efeeae6ce70c
- [E] Ligamentaxis on Commons.Wikimedia.org July 12, 2017 https://commons.wikimedia.org/wiki/File:Arthroskopie.jpg
- [F] Hillcrestpvtltd Surgical Arthroscopic Forceps on Commons.Wikimedia.org December 18, 2013. https://commons.wikimedia.org/wiki/File:Surgical_Arthroscopic_Forceps.jpg
- [G] Tim1965 on Typical arthroscopic surgery incisions – knee on Commons.Wikimedia.org March 27, 2010. https://commons.wikimedia.org/wiki/File:Typical_arthroscopic_surgery_incisions_-_knee.JPG
- [H] BruceBlaus Walking with Crutches on Commons.Wikimedia.org May 31, 2017 https://commons.wikimedia.org/wiki/File:Home_Care_Crutches_Walking.png
Disclaimer:
Use of Course Content. The courses provided by NCC are based on industry knowledge and input from professional nurses, experts, practitioners, and other individuals and institutions. The information presented in this course is intended solely for the use of healthcare professionals taking this course, for credit, from NCC. The information is designed to assist healthcare professionals, including nurses, in addressing issues associated with healthcare. The information provided in this course is general in nature and is not designed to address any specific situation. This publication in no way absolves facilities of their responsibility for the appropriate orientation of healthcare professionals. Hospitals or other organizations using this publication as a part of their own orientation processes should review the contents of this publication to ensure accuracy and compliance before using this publication. Knowledge, procedures or insight gained from the Student in the course of taking classes provided by NCC may be used at the Student’s discretion during their course of work or otherwise in a professional capacity. The Student understands and agrees that NCC shall not be held liable for any acts, errors, advice or omissions provided by the Student based on knowledge or advice acquired by NCC. The Student is solely responsible for his/her own actions, even if information and/or education was acquired from a NCC course pertaining to that action or actions. By clicking “complete” you are agreeing to these terms of use.
➁ Complete Survey
Give us your thoughts and feedback
➂ Click the Green MARK COMPLETE Button Below
To receive your certificate
