Course
Caring for Pediatric Hospice Patients
Course Highlights
- In this course we will learn about pediatric hospice, and why it is important for nurses to be understand this unique population.
- You’ll also learn the difference between pallative care and hospice, as well as how adult and pediatric hospice differ.
- You’ll leave this course with a broader understanding of how to support the families of pediatric hospice patients.
About
Contact Hours Awarded: 2
Course By:
Marybeth Anderson Keppler
MSN, RN, OCN
Begin Now
Read Course | Complete Survey | Claim Credit
➀ Read and Learn
The following course content
Caring for patients with a terminal illness is challenging, but those difficulties are multiplied when the patient is a child. For starters, you will likely find that you have informal patients in addition to the child: his or her parent(s), family, caregivers, community members, and so forth. Furthermore, when the child qualifies for hospice care, this can make matters even more daunting for all parties involved. This course is designed to walk nurses through the basics of life-threatening childhood illnesses, hospice and palliative care, and the resources available for those working with the pediatric hospice population.

Self Quiz
Ask yourself...
- How familiar are you with the concepts of palliative care and pediatric hospice?
- What would you list as the top 5 terminal illnesses for children (ages birth-20 years old)?
- Have you ever had a patient in hospice care? If so, how did you deal with the situation?
- What do you think might be some common misconceptions about hospice care?
Palliative Care and Adult vs. Pediatric Hospice
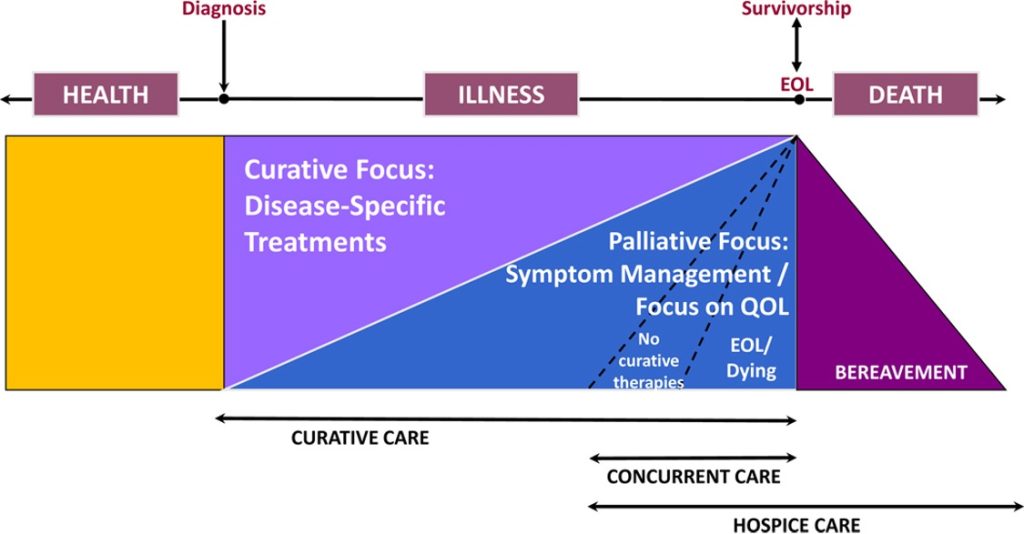
For nurses, particularly those who don’t often have pediatric hospice patients, it is good to have a working knowledge of some terminology related to this population. First, a common misconception is that hospice and palliative care are the same thing. While there is much overlap, they are two separate modalities of care (1, 2).
Sadly, far too many patients do not receive services for which they are eligible, with the median length of hospice stay just 18 days, and 75% of people using these services for less than 87 days, out of the six months available (3).
Palliative care is an umbrella concept that encompasses the management of pain and other symptoms, like nausea, vomiting, diarrhea, depression, anxiety, and more (1). This type of care may be provided for any patient and can be readily available at the time of diagnosis.
Palliative care seeks to improve the quality of life of patients and can also include the following:
- Assistance getting rides to/from medical appointments.
- Social service connections to community resources
- Assistance with medications, nutrition, and financial resources
- Relaxation techniques and counseling
- Emotional and spiritual support
- Assistance with children and/or caregivers
Hospice is special care reserved for end-of-life patients. For pediatric hospice, however, the guidelines are less rigid. There are some key differences between adult and pediatric hospice. For adults in hospice care, they need a prognosis of 6 months (or less) to live to quality for these services. If an adult is in hospice care, they must not seek curative treatment, though palliative care is certainly still provided.
For children (here, defined as prenatal through approximately 21 years old), curative treatment may still be sought, and the child may still qualify for pediatric hospice services (4). The family, not just the child, is the central area of focus for pediatric hospice services. Additionally, for those under 18 years old, parents (or legal guardians) make the medical decisions for the child, which can be very difficult for everyone involved.
Pediatric Palliative/Hospice Care (PP/HC) is its specialty, catering to the needs of the young (5). PP/HC aims to increase the quality of the child’s life, regardless of whether that includes disease-modifying treatment. A holistic approach is used in PP/HC and includes everything, from educational to psychosocial to physical needs, considering each family’s cultural, spiritual, and unique needs. Services are provided from prenatal to over the age of 21, depending on the child’s care team and diagnoses.
Diagram: Palliative & Hospice Care Continuum in Children with Cancer

Self Quiz
Ask yourself...
- What are the key differences between palliative care and hospice?
- How do hospice services differ between adults and children?
- What might be some unique needs of the pediatric hospice population (and for those involved with them)?
- What legal issues might differ between adult and pediatric hospice patients?
- Are there any ethical concerns a pediatric hospice worker may face in her line of work?
Cancer in Childhood
Of children ages 15 and younger in the United States, about 9,600 will be diagnosed with cancer in 2024 (1). While incidence has been rising in recent years, so has the survival rate; approximately 85% of pediatric oncology patients can expect to live five years or more after diagnosis (1). The disheartening statistic is that cancer remains the number two cause of death for those under age 15, after accidents, and nearly 1,040 children will die from cancer in 2024 (1).
Prevalence of Pediatric Cancer
Cancers that develop in childhood are often different from those seen in adults; in order of incidence, the most common childhood cancers are (1):
- 28%: Leukemia (in the blood and bone marrow)
- 26%: Brain, spinal, and other central nervous system cancers
- 8% Lymphoma (in the lymph nodes)
- 6%: Bone and muscle cancers (Ewing sarcoma, osteosarcoma, rhabdomyosarcoma); neuroblastoma
- 5%: Wilms tumor (in the kidney)
- 2%: Retinoblastoma (in the eye)
- 2%: retinoblastoma (in the eye)

Self Quiz
Ask yourself...
- What experience (if any) do you have with pediatric cancer?
- How would you explain cancer to a child? What about their parents or family members?
- Do you know anyone impacted by cancer?
- What types of cancer, if any, have you come across in your own life?
- What are the main types of cancer found in children?
Other Potentially Life-Threatening Illnesses in Childhood
Unfortunately, cancer is not the only cause of a shortened lifespan for some children. While cancer diagnoses account for about 36% of all pediatric hospice referrals, other illnesses can occur in childhood and may warrant palliative and/or pediatric hospice care (2).
These afflictions include (with incidences in parentheses; comorbidities occur):
- Genetic (36%)
- Neurodegenerative (27%)
- Neuromuscular (20%)
- Cardiovascular (17%)
- Pulmonary (16%)
- Perinatal (14%)
- Metabolic (13%)
- Gastrointestinal (6%)
- Renal (6%)
- Immunologic (5%)
(6)
When one or more of the above conditions exist together, the children who experience this situation are referred to as medically fragile (6). Unfortunately, according to many experts, this population may fall through the cracks of the healthcare system and miss out on many resources for which they qualify (5).
Medically fragile children are great candidates for pediatric palliative/hospice care, and you as the nurse could help start a conversation with the family about these services. In fact, over 5% of all pediatric palliative/hospice referrals come from home health workers (2).


Self Quiz
Ask yourself...
- What are some other potentially life-threatening conditions that may occur in children besides cancer?
- Would you be comfortable discussing palliative/hospice care with a pediatric patient or his/her family? Why or why not?
- If you encounter a child who might be considered medically fragile, what information would you want to offer to their family?
- Why might people be hesitant to sign up for this type of assistance?
Caring for a Pediatric Hospice Patient: A Case Study
Jessica is an 8-year-old girl with acute myeloid leukemia (AML) and is being admitted to the pediatric oncology unit for the first time. This is a new diagnosis, and her parents are devastated. They tell you that they aren’t prepared to cope with something like this. Jessica’s parents are in their early 30s and have another child, 6-year-old Jason. They are not sure how (or even if) they should tell Jason about Jessica’s AML, nor how much they should discuss with Jessica herself. The parents cry together often, though when Jessica is around, they smile and act as if nothing is wrong.
When you are assessing Jessica during her admission, she says to you, “My parents are acting weird. What’s going on? Is it like I’m dying or something?”
- What can you say to Jessica at this time? To her parents?
- Do you think it is a good idea to meet privately with Jessica’s parents first before talking to Jessica at length? Why or why not? What would you do in this situation?
- Who else can and should be involved with this discussion?
Who Is Involved in Palliative and Pediatric Hospice Care?
Like any other area of healthcare, hospice and palliative care does not happen in a vacuum; it employs members from many disciplines, and typically includes at least the following people (3):
- Nurses
- Doctors and advanced practice nurses
- Nutritionists
- Child life specialists
- Counselors
- Pharmacists
- Chaplains
- Social workers
- Integrative therapists
- Certified nursing assistants
- Volunteers
In general, health insurance covers most palliative care costs, and Medicare and/or Medicaid are utilized for hospice services (2). However, each patient’s situation is different, and social workers are great resources for helping parents plan for the inevitable cost of care. When discussing end-of-life options, a chaplain, counselor, therapist, and/or child life specialist may be sources of comfort and information for parents and children alike.
For managing pain and other symptoms, the medical team (pharmacists, nurses, and doctors) works together to care for the patient. If parents/caregivers need a break (called respite in hospice care), volunteers and other caregivers can be recruited to help.

Self Quiz
Ask yourself...
- Who are the main members of a palliative care or pediatric hospice team?
- Would you include any other members in this group (or omit any)? If so, who, and for what reasons?
- What would you say to a patient who states, “Hospice? I can’t afford all that care!”
Case Study cont.
In Jessica’s case, she and her family will soon receive this array of professional support while in the hospital. Anyone can bring up the idea of palliative (or pediatric hospice) care at any time: the nurse, doctor, chaplain, social worker, etc. The main goal is to maintain the best quality of life for Jessica, as well as to support her family in the meantime.
While end-of-life discussions are incredibly difficult, it would be helpful to her and her family to make some decisions, even if only about supportive care, and to be prepared for several different outcomes. It might help to tell the family that the preparations are only in the event of the worst-case scenario and that they may never need these plans at all.

Self Quiz
Ask yourself...
- Do you know of any community resources for hospice patients of any age? If so, what are they?
- How would you go about referring Jessica and her family to local resources when she is discharged from the hospital?
- What other discharge teaching might you want to give this family?
Factors of Pediatric Hospice
Oftentimes, the pediatric hospice journey begins with a diagnosis. As discussed above, the most common diagnoses leading to hospice are cancer, congenital anomalies, and other childhood illnesses.
Many factors present after this (5,6, 7), and may include any or all of the following:
- Grieving Process: Denial and any of the other stages of grief outlined by the Kübler-Ross model: anger, bargaining, depression, and acceptance.
- Disease Process: Many patients, particularly children, may experience periods of remission followed by relapse/recurrence. Unfortunately, this can lead to a proverbial rollercoaster of emotions for the child and their family.
- Location: Many pediatric hospice patients begin their journey in the hospital, but then may oscillate between various doctors’ offices, home, school, hospice facilities, and back to the hospital. This can present emotional and logistical challenges for families. At present, only about 75% of hospitals in the US have a pediatric palliative care team, so referrals can be challenging in certain geographic areas.
- Adequately Trained Staff: While there are many hospices in the US, only about 20% have formal pediatric services with staff trained specifically for this population.
- Underserved Communities: As with many other areas in healthcare, people of color, the LGBTQ+ community, and those in certain geographic locations have significantly less access to pediatric hospice services.
- Family Concerns: Every family dynamic is different and helping an entire family cope with a pediatric hospice case can prove challenging. The parents may need to coordinate the care of siblings and other family members while keeping their other child in mind. Fortunately, as discussed above, respite care is a hospice service designed to give families a brief period of rest from daily duties and activities related to the end-of-life care of their child. Other community resources available to families are listed at the end of this course.
- Preparing for Death: While unimaginable to many, childhood death is a sad reality at times. The family and the child may find it helpful to discuss wishes as early as they can manage. While a child’s and parent’s wishes may conflict, hopefully, a consensus may be reached that is agreeable to all parties.


Self Quiz
Ask yourself...
- What roles (if any) do you see yourself in when it comes to the pediatric hospice/palliative care population?
- In what ways might you help support a pediatric hospice/palliative care patient or their family?
- How can you help close the gap of care experienced by marginalized communities (e.g., those with lower income, people of color, and non-English speaking patients)?
The Non-Hospice Nurse’s Role
Since most pediatric nurses are not serving in a hospice role, here are some things that the non-hospice pediatric nurse might wish to keep in mind when working with this population:
Pain and Symptom Management
Many childhood illnesses are accompanied by pain and other uncomfortable symptoms. Palliative care is typically given for other problems, like fatigue, fever, fluid overload, incontinence, infections, skin breakdown, and more (5). Thus, the pediatric nurse’s role is to help assess and alleviate these problems whenever possible. Understanding the Child’s and Parents’ Wishes
Sometimes the child may not understand the full extent of their disease due to what the parents are willing to discuss. The nurse must tread carefully and respect the wishes of the family. It might be best to talk to parents away from the child, to see the expectations for the interactions at hand.
Communication
The nurse needs to communicate between family and physician even more than those working with the adult population. Many doctors may be hesitant to address death and dying with children and their families, so it falls to the nurse to facilitate whatever discussion the family deems necessary. If needed, the child life specialist, chaplain, and/or social worker may help in these situations.
Maintaining Medical Treatment
The pediatric nurse will also need to perform her basic duties with this child as well: central line maintenance (if applicable), medication administrations (including PEG/J tubes, total parenteral nutrition, and more), oxygen delivery, infection/wound management, and physical positioning of the child.

Self Quiz
Ask yourself...
- What other nursing roles might you anticipate for the pediatric hospice patient who is seen in an inpatient setting? In a doctor’s office or other outpatient setting?
- What might the role of a school nurse be for the pediatric hospice patient?
- What would you do if you were caring for a child in hospice care whose parents didn’t want him to know about his diagnosis?
Comfort Measures and In-Depth Support for the Pediatric Hospice Population
Unlike adult patients, the parents of the pediatric patient are typically the primary decision-makers, particularly for younger children. A family assessment, not just the child’s, is crucial for pediatric hospice patients, and treatment courses will usually be decided by the parents, not the child (especially for those under the age of 10). However, symptom-directed treatment (e.g., pain or nausea control) is always something to be addressed with this for the children themselves. This care may include the application of oxygen, positioning the patient, administering various pain or antiemetic medications, and more. As with all other patients, the child’s disease process and coping abilities will determine the comfort measures needed.
Psychosocial needs must be assessed as well. If the family is having a particularly challenging time coping, the child life specialist and chaplain are the best resources to ask for assistance. Other disciplines, such as art or music therapy, may be utilized, as well as physical and occupational therapy. Perhaps the family prefers that the child primarily be treated at home, so a referral to home health services might be appropriate. Social workers can help with this process, as can the pediatric hospice team that is assigned to the child.
Cultural needs are also of the utmost importance. Depending on the family’s cultural and religious backgrounds, preferences for end-of-life care may vary greatly. Each family you encounter will have different concepts of death and dying. This may vary from wanting every single intervention possible until the patient’s last breath to withdrawing all care at a certain point. The nurse should be mindful of these preferences, noting that the family’s decisions may change one or many times during the child’s illness.

Self Quiz
Ask yourself...
- How might comfort measures for children differ from those given to adults?
- What other needs might a family have with an extremely ill child? What resources might you share with these families?
- What is your view on death and dying? How would you work with a child and/or family with different ideas than yours?
Community Resources and Support for Pediatric Palliative/Hospice Care Patients
In the United States, many organizations deal with cancer, palliative care, and hospice. A simple internet search can yield myriad results for those needing services. Some good starting points are:
- National Hospice and Palliative Care Organization, Pediatric Palliative and Hospice Care: http://www.nhpco.org/pediatrics
- Palliative Care for Children: https://www.ninr.nih.gov/newsandinformation/conversationsmatter/palliative-care-for-children
- Thinking about Hospice: A Discussion Guide for Families: https://www.vitas.com/-/media/files/pdfs/hospice-and-palliative-care-basics/when-is-it-time-for-hospice/family-discussion-guide-english.ashx
- Finding Social Support and Information: https://www.cancer.net/coping-with-cancer/finding-social-support-and-information
- Cancer Information and Helplines: https://www.cancer.net/coping-with-cancer/finding-social-support-and-information/telephone-and-e-mail-cancer-helplines
- Caring for a Terminally Ill Child: https://www.cancer.net/navigating-cancer-care/advanced-cancer/caring-terminally-ill-child
- Accessing Palliative Care Services: https://getpalliativecare.org/
- ELNEC: End-of-Life Nursing Education Consortium project from the American Association of Colleges of Nursing: https://www.aacnnursing.org/ELNEC

An Insider’s Perspective
I have experienced this subject matter on an extremely personal level, as my family member was a parent faced with the terminal illness diagnosis of their child. The role of the palliative care and pediatric hospice team was constant throughout their son’s diagnosis before his birth. They walked my family through every aspect of care including options, diagnosis, the pathophysiology behind the diagnosis, consults with pastoral care, social work, and more.
For parents, receiving a terminal diagnosis of an unborn child is unimaginably difficult. Without the pediatric hospice and palliative care teams, my family would have completely crumbled. When their son was born, it was unknown how long he would live. Because of the care teams, the parents were educated on what to expect, and what was happening hour by hour, and were assisted with how to cope.
As nurses, we are the bridge. We are the communicators and the advocates, no matter how hard or how easy the circumstance is.
When their son surpassed their expectations of life expectancy, he was discharged home with pediatric hospice services. The parents were prepped with end-of-life care, how to handle the situation, what to look for, and what measures to take. Without this guidance, they would have been lost. When it came time for them to put their education into practice, they were prepared. No matter how gut-wrenching that moment was, the team was a phone call away. Measures were in place to make their son as comfortable as possible during his last moments.
It is the team’s responsibility to make a difference in patients’ lives, to show compassion, and empathy, and to advocate for everyone involved. It is imperative that the entire healthcare team is on board and available as an educational and support resource to these parents, patients, and families as they deal with this difficult time.
Conclusion
Palliative care and hospice services are available to anyone, from the time before they are born until the time they die (and a year after to support family members). However, when such care is needed for children, it can be even more difficult for everyone involved. There are resources to help, and it is beneficial for all nurses to be aware of some information to share with these patient populations and their loved ones. As with every type of nursing, it is one of our duties to focus on the quality of life of our patients, and to ensure our own well-being in the process.
References + Disclaimer
- American Cancer Society (2021). Types of cancer that develop in children. Retrieved from https://www.cancer.org/cancer/cancer-in-children/key-statistics.html
- National Hospice and Palliative Care Organization (NHPCO) (2023). NHPCO Pediatric Facts and Figures: 2023 Edition. Retrieved from https://www.nhpco.org/wp-content/uploads/NHPCO_Pediatric_Facts_Figures_2023.pdf
- NHPCO (2024). Pediatric Concurrent Care. Retrieved from https://www.nhpco.org/palliativecare/pediatrics/pediatric-concurrent-care/
- Pyke-Grimm, K. A., Fisher, B., Haskamp, A., Bell, C. J., & Newman, A. R. (2021). Providing Palliative and Hospice Care to Children, Adolescents, and Young Adults with Cancer. Seminars in Oncology Nursing, 37(3), 151166. https://doi.org/10.1016/j.soncn.2021.151166
- Vossel, H. (2023). The Forces Driving, Impeding Access to Pediatric Palliative Care. Hospice News. Retrieved from https://hospicenews.com/2023/10/13/the-forces-driving-impeding-access-to-pediatric-palliative-care/
- Abt Associates (2022). 2022 Hospice Information Gathering Report: Health Equity in the Hospice Setting. Retrieved from https://www.cms.gov/files/document/hospice-quality-reporting-program-information-gathering-report2022508.pdf
Disclaimer:
Use of Course Content. The courses provided by NCC are based on industry knowledge and input from professional nurses, experts, practitioners, and other individuals and institutions. The information presented in this course is intended solely for the use of healthcare professionals taking this course, for credit, from NCC. The information is designed to assist healthcare professionals, including nurses, in addressing issues associated with healthcare. The information provided in this course is general in nature and is not designed to address any specific situation. This publication in no way absolves facilities of their responsibility for the appropriate orientation of healthcare professionals. Hospitals or other organizations using this publication as a part of their own orientation processes should review the contents of this publication to ensure accuracy and compliance before using this publication. Knowledge, procedures or insight gained from the Student in the course of taking classes provided by NCC may be used at the Student’s discretion during their course of work or otherwise in a professional capacity. The Student understands and agrees that NCC shall not be held liable for any acts, errors, advice or omissions provided by the Student based on knowledge or advice acquired by NCC. The Student is solely responsible for his/her own actions, even if information and/or education was acquired from a NCC course pertaining to that action or actions. By clicking “complete” you are agreeing to these terms of use.
➁ Complete Survey
Give us your thoughts and feedback
➂ Click the Green MARK COMPLETE Button Below
To receive your certificate
