Course
Crohn’s Disease Complications and Quality of Life
Course Highlights
- In this Crohn’s Disease Complications and Quality of Life course, we will learn about Crohn’s Disease and its three degrees.
- You’ll also learn the two phases of treatment for Crohn’s disease.
- You’ll leave this course with a broader understanding of factors affecting the quality of life in Crohn’s disease patients.
About
Contact Hours Awarded: 1
Course By:
Michael York MSN, RN
Begin Now
Read Course | Complete Survey | Claim Credit
➀ Read and Learn
The following course content
Introduction
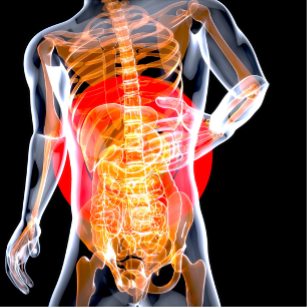
Crohn’s disease (CD) is a chronic inflammatory condition of the gastrointestinal tract that affects millions of individuals worldwide, and significantly impacts their quality of life. Characterized by periods of active symptoms and remission, Crohn’s disease can lead to a range of complications, from abdominal pain and severe diarrhea to malnutrition and fatigue.
We will explore the complexities of Crohn’s disease, reviewing its symptoms, diagnosis, treatment options, and the latest advancements in managing this challenging condition. By increasing awareness and understanding, we aim to provide valuable insights for patients, caregivers, and healthcare professionals navigating the intricacies of Crohn’s disease.
Definition
The autoimmune disease characterized by an intractable and chronic activation of the intestinal immune system is known as inflammatory bowel disease (IBD). IBD has two distinct branches which often mirror each other; ulcerative colitis (UC) and CD. CD follows a cycle of inflammatory flares and remissions (4). CD can affect the whole gastrointestinal tract and can have symptoms outside that vicinity (1).
There are three degrees of CD which will also be defined:
- Mild to moderate: Patient can ambulate and tolerate oral intake of food without any signs of dehydration, abdominal tenderness, painful mass, obstruction, or weight loss of greater than 10% from baseline.
- Moderate to severe: Did not respond to the treatment for mild to moderate disease. Also, it includes those with symptoms of fever, abdominal pain, anemia, nausea/vomiting, and/or significant weight loss.
- Severe: Incessant symptoms despite induction therapy. Symptoms include high fevers, continuous nausea/vomiting, intestinal obstruction, guarding and rebound pain, and/or abscess
(3)

Self Quiz
Ask yourself...
- Can you name three degrees of CD?
- What are the two branches of IBD?
Epidemiology
The incidence of CD in North America is 6.3-23.8 per 100,000 and rising. The incidence of CD is also rising globally. Most notably, CD is on the rise in countries that have adopted a Western diet, have increased industrialization, and increased air pollution. This further supports the evidence that environmental factors play a role in the onset of CD (2).
Certain factors in the environment have proven ties to CD. They include:
- Smoking: Evidence shows that smoking is not only a huge environmental factor in causing CD, but it also increases the risks of having an adverse outcome. Within the CD demographic of patients, smokers have been shown to have more CD flares, more intestinal tract involvement, higher need for surgery, reduced response to treatment, and an increased need for rescue therapy than non-smokers. Studies have shown that smoking regularly can cause rapid, aggressive progression of CD.
In smokers, CD can progress from a simple inflammatory condition to a penetrating stricture/fistula disease. Smoking also causes histological changes throughout the intestinal tract. It can increase lymphocytes and pro-inflammatory cytokines and change the mucosal vasculature. Smoking cessation is a great way to curb the progression of CD. It can greatly reduce the number of relapses or flares and result in an overall milder course of the disease (1, 2).
- Diet: Diet plays a big role in determining the components of the intestinal microbiome. Many dietary risk factors play a part in both the cause and progression of CD. These factors include high sugar, fat, and protein content. A lack of fruits and vegetables in the diet and fast-food intake have also proven to be CD risk factors. Studies performed in Asian countries have shown a rise in the incidence of CD as the diet becomes more Westernized. Decreasing vegetable consumption leads to less dietary fiber. Dietary fiber is essential in maintaining the gut’s intestinal flora. Eating more processed foods and foods high in fat also increases the risk of CD (1).
- Medications: The use of antibiotics can lead to an imbalance of the normal intestinal flora. This affects immune tolerance and pathogen sensitivity. Exposure to antibiotics as a child increases the risk of CD. Aspirin, NSAIDs, and oral contraceptives have also been associated with the development of CD (1, 8).

Self Quiz
Ask yourself...
- Where is the incidence of CD rising?
- Name two environmental factors that are influencing the incidence of CD.
- What can a smoker do to decrease the severity of CD?
Pathophysiology
The pathophysiology of CD is based on three components: genetics, the microbiome of the intestinal tract, and environmental factors. CD is associated with more than one hundred genetic markers. The associated genes suggest that the immune response to gut bacteria is a key factor in CD development. Studies have shown a distinct difference in the gut flora of people with CD versus those without.
An interaction between the environment and the genes associated with CD can facilitate CD pathogenesis by damaging the gut lining and/or causing an immune response within the intestinal tract. This can cause the immune system to attack the regular gut flora (2). The resulting bowel damage can lead to fibrosis. Once fibrosis sets in, it becomes very difficult to reverse the disease. This tissue destruction can lead to strictures, perforations, abscess formation, and fistulation. Approximately one-third of CD patients will progress to abscess and fistula formation (6).

Self Quiz
Ask yourself...
- CD pathophysiology is based on what three components?
- What can bowel damage lead to?
Clinical Signs and Symptoms
It is not uncommon for patients to have symptoms for years before being correctly diagnosed with CD. Misdiagnosis of irritable bowel syndrome (IBS) is often made due to fluctuations of symptoms over periods. Average delays in correct diagnosis of CD can range from nine to eighteen months from the start of symptoms. Obtaining a comprehensive medical history and performing a thorough medical examination are paramount in both correctly diagnosing CD and starting a patient-tailored treatment regimen (2).
There are cardinal signs and symptoms of CD. They include:
- Abdominal pain and cramping
- Diarrhea
- Urgent bowel movements
- Perianal ulcers or fissures
- Stricture/abscess formation
- Decreased appetite
- Weight loss
- Blood in the stool
- Mucus in the stool (2)

Self Quiz
Ask yourself...
- What is the average delay in properly diagnosing CD?
- Name two courses of action that are key to properly diagnosing CD.
- Name three cardinal symptoms of CD.
Etiology
The etiology of CD is altogether unclear. There is no single cause of CD. It is caused by genetic, immunologic, infectious, and environmental factors which work together and impact immune responses. A breakdown in the mucosal barrier of the intestine can lead to a state of constant inflammation of the gut (2, 6).

Self Quiz
Ask yourself...
- What is the cause of CD?
Management and Treatment
The medical management of CD focuses on suppressing the active intestinal immune system. Healing the mucosa is a key target in the management of CD. The medical management regimen needs to be tailored to the patient, taking into consideration factors such as disease severity and location within the intestines. Other considerations for management include the patient’s age, the extent of the CD lesions, and if there are any extra-intestinal factors in play.
There are two distinct phases of treatment: induction and maintenance.
Induction consists of high doses of steroid-sparing medications in the first weeks to months of treatment to achieve a state of remission. To attain control of CD symptoms, steroids such as budesonide and prednisone are often used in the induction phase. These drugs have a rapid onset of action that induces remission. In the maintenance phase, lower doses of steroid-sparing medications such as biologicals or immune modulators are used. Biologicals maintain remission at rates not achieved by any other drugs.
Examples of biologicals include infliximab, adalimumab, and certolizumab. The CD patient will continue with maintenance therapy for the rest of their life. This is to both maintain a state of remission and to help prevent any flares. Though steroids are used in the induction phase, they are not effective as maintenance therapy drugs. Patients are also treated with antibiotics to prevent sepsis (2, 7, 8).
Surgical intervention may also be needed when portions of the bowel become extremely damaged and demonstrate a danger to the survival of the patient. 20% of patients diagnosed with CD already present with strictures and abscesses within ninety days of diagnosis. Though surgery was the first line of treatment when CD was discovered, it has since become the last line of treatment. In CD, surgery is not a cure, and more than half of patients suffer recurrence one-year post-op. As such, bowel-sparing procedures such as bowel resection are favored over total colectomy (5).

Self Quiz
Ask yourself...
- What is the focus of the management of CD?
- Can you describe the two phases of CD treatment?
- Name two biological drugs.
- When is surgery needed for CD?
- Why would antibiotics be used in the treatment of CD?
Quality of Life
Multiple studies have shown that the patient’s quality of life is highly affected by CD. Overall, patients report that living with CD leads to a poor quality of life. CD touches nearly every aspect of the patient’s life. Due to the debilitating nature of the disease, patients can develop a sense of isolation. Symptoms such as urgent, bloody bowel movements may keep patients away from social situations. This can include work and school. Patients may have high absenteeism rates. Poor productivity at work and a high incidence of both temporary and permanent disability have been reported. Patients also have severe fatigue which may stop them from being able to perform their activities of daily living. All of these compounds and many patients with CD also develop depression and anxiety.
The fear of having an accident during a CD flare can make the patient feel alone as, again, they avoid social situations. Fecal incontinence is not uncommon with CD. Patients suffering from CD can easily become depressed as all these emotions and feelings come together.
Hopelessness is a real issue with CD patients. Living with a chronic disease can be very difficult, not just because of the disease process, but those close to the patient will often have a difficult time understanding what is happening. Friends and family find it hard to relate with the patient suffering from CD. This can further drive the feelings of isolation and hopelessness within the patient.
The disease process itself is burdensome with many complications that are both painful and, ultimately, debilitating. Extra-intestinal complications can also manifest themselves. This includes bone, liver, ophthalmic, and skin issues. Another stressor that affects quality of life is the treatment for CD. Many of the drugs used to treat CD have adverse side effects which contribute to the overall poor quality of life among CD patients (8).


Self Quiz
Ask yourself...
- What kinds of situations may patients with CD avoid?
- Name two types of psychosocial issues that patients with CD may exhibit.
Patient Education
Many patients may want to stop taking their CD medications once remission has been achieved. This may be due to their side/adverse effects and to the patient’s desire to limit the medications that they need to take daily. In some cases, a pregnant woman may not want the baby to be affected by the medication. It is of utmost importance that CD patients are educated on the need to continue their maintenance therapy. Stopping their medication can lead to increased flares, the need for surgical intervention, and other risks associated with CD (2).
Another area of opportunity for patient education is diet. Increasing dietary fiber through fruits and vegetables while limiting fast foods and foods high in sugar, fat, and animal protein (1).
The patient should also be educated in their medical management. They should be involved in their plan of care. Patients should be able to differentiate between remission and flares, understanding when they need to seek medical attention. A firm understanding of their medications is key (2).

Self Quiz
Ask yourself...
- What are two areas where CD education is needed?
- What foods should be limited to patients with CD?
Conclusion
CD is a chronic, painful, and debilitating disease. It comes with a lot of possible complications that can directly affect a patient’s quality of life. CD targets people of all genders, ages, and cultural/racial backgrounds.
Fortunately, treatments and medical management of CD has evolved, and new drugs have been developed to maintain a state of remission in the CD patient population. Education and adherence to the medical management regimen are key to maintaining a state of CD remission and a good quality of life.
References + Disclaimer
- Chen, Y., Wang, Y., & Shen, J. (2019). Role of environmental factors in the pathogenesis of Crohn’s disease: A critical review. International Journal of Colorectal Disease, 34(12), 2023–2034. https://doi.org/10.1007/s00384-019-03441-9
- Cushing, K., & Higgins, P. R. (2021). Management of Crohn’s disease. JAMA, 325(1), 69. https://doi.org/10.1001/jama.2020.18936
- Gade, A. K., Douthit, N. T., & Townsley, E. (2020). Medical management of Crohn’s disease. Cureus. https://doi.org/10.7759/cureus.8351
- Kofla-Dłubacz, A., Pytrus, T., Akutko, K., Sputa-Grzegrzółka, P., Piotrowska, A., & Dzięgiel, P. (2022). Etiology of ibd—is it still a mystery? International Journal of Molecular Sciences, 23(20), 12445. https://doi.org/10.3390/ijms232012445
- Le Berre, C., Ananthakrishnan, A. N., Danese, S., Singh, S., & Peyrin-Biroulet, L. (2020). Ulcerative colitis and crohn’s disease have similar burden and goals for treatment. Clinical Gastroenterology and Hepatology, 18(1), 14–23. https://doi.org/10.1016/j.cgh.2019.07.005
- Lightner, A. L., Ashburn, J. H., Brar, M. S., Carvello, M., Chandrasinghe, P., van Overstraeten, A., Fleshner, P. R., Gallo, G., Kotze, P., Holubar, S. D., Reza, L. M., Spinelli, A., Strong, S. A., Tozer, P. J., Truong, A., Warusavitarne, J., Yamamoto, T., & Zaghiyan, K. (2020). Fistulizing crohn’s disease. Current Problems in Surgery, 57(11), 100808. https://doi.org/10.1016/j.cpsurg.2020.100808
- Petagna, L., Antonelli, A., Ganini, C., Bellato, V., Campanelli, M., Divizia, A., Efrati, C., Franceschilli, M., Guida, A. M., Ingallinella, S., Montagnese, F., Sensi, B., Siragusa, L., & Sica, G. S. (2020). Pathophysiology of crohn’s disease inflammation and recurrence. Biology Direct, 15(1). https://doi.org/10.1186/s13062-020-00280-5
- Roda, G., Chien Ng, S., Kotze, P., Argollo, M., Panaccione, R., Spinelli, A., Kaser, A., Peyrin-Biroulet, L., & Danese, S. (2020). Crohn’s disease. Nature Reviews Disease Primers, 6(1). https://doi.org/10.1038/s41572-020-0156-2
Disclaimer:
Use of Course Content. The courses provided by NCC are based on industry knowledge and input from professional nurses, experts, practitioners, and other individuals and institutions. The information presented in this course is intended solely for the use of healthcare professionals taking this course, for credit, from NCC. The information is designed to assist healthcare professionals, including nurses, in addressing issues associated with healthcare. The information provided in this course is general in nature and is not designed to address any specific situation. This publication in no way absolves facilities of their responsibility for the appropriate orientation of healthcare professionals. Hospitals or other organizations using this publication as a part of their own orientation processes should review the contents of this publication to ensure accuracy and compliance before using this publication. Knowledge, procedures or insight gained from the Student in the course of taking classes provided by NCC may be used at the Student’s discretion during their course of work or otherwise in a professional capacity. The Student understands and agrees that NCC shall not be held liable for any acts, errors, advice or omissions provided by the Student based on knowledge or advice acquired by NCC. The Student is solely responsible for his/her own actions, even if information and/or education was acquired from a NCC course pertaining to that action or actions. By clicking “complete” you are agreeing to these terms of use.
➁ Complete Survey
Give us your thoughts and feedback
➂ Click the Green MARK COMPLETE Button Below
To receive your certificate
