Course
Differential Diagnosis of Hypothyroidism
Course Highlights
- In this Differential Diagnosis of Hypothyroidism course, we will learn about the classic and atypical symptoms associated with hypothyroidism.
- You’ll also learn about laboratory tests and imaging studies in the diagnosis of hypothyroidism.
- You’ll leave this course with a broader understanding of the treatment for hypothyroidism.
About
Contact Hours Awarded: 2
Course By:
Abbie Schmitt
MSN-Ed, RN
Begin Now
Read Course | Complete Survey | Claim Credit
➀ Read and Learn
The following course content
Introduction
As we embark on the journey of differential diagnosis of hypothyroidism, we will examine several medical mysteries. This condition, marked by the thyroid gland's failure to produce sufficient hormones, often disguises itself with a cloak of nonspecific symptoms that could easily be mistaken for other health issues.
A patient could report feeling tired, perhaps having unexplained weight gain, or feeling unusually cold, not realizing that these could be whispers of an underactive thyroid. The challenge for clinicians lies not just in recognizing these whispers among the noise of overlapping symptoms, but in using them to trace the path back to the true culprit.
The process of differential diagnosis for hypothyroidism is a critical exploration—a blend of pathophysiology, etiology, and clinical signs and symptoms of hypothyroidism. By carefully piecing together clues from patient histories, physical exams, and targeted laboratory tests, it is possible to uncover the hidden patterns of this disorder.
Definition
"Differential diagnosis" is a term used to describe the process by which a provider determines which disease or condition most likely explains an individual’s symptoms and signs. The process involves comparing and contrasting various possibilities to arrive at the most likely diagnosis.
Hypothyroidism essentially occurs when the thyroid gland is not able to produce adequate amounts of thyroid hormone. In the context of hypothyroidism, a differential diagnosis means considering and ruling out other conditions that might cause similar symptoms to those of hypothyroidism. These symptoms can include fatigue, weight gain, cold intolerance, dry skin, hair loss, and constipation, among others.
The provider will consider medical history, physical examination, and laboratory tests to narrow down the list of possible diagnoses to the most likely one. For hypothyroidism, measuring levels of thyroid hormones and thyroid-stimulating hormone (TSH) in the blood is key to confirming the diagnosis.
Hypothyroidism can be broken down into two categories, primary and secondary (central) hypothyroidism. Secondary is less common and occurs when the thyroid gland functions normally, but the pituitary gland or hypothalamus do not, which causes thyroid dysfunction.
Epidemiology
Roughly 5% of the U.S. population has a diagnosed thyroid disorder, and the American Association of Clinical Endocrinologists suggests that an additional 5% has undiagnosed thyroid disease (8). In developing countries, where dietary iodine is lacking, thyroid disease is even more prevalent.
Impaired thyroid function is more common in females and individuals greater than 65 years old. Thyroid dysfunction is more prevalent among individuals with autoimmune diseases such as diabetes type I, celiac disease, or autoimmune endocrine disorders. Those with Downs’ or Turners’ syndrome are at higher prevalence as well.
Heredity is a significant contributor to the development of hypothyroidism in individuals who have a history of hypothyroidism in their family; the chances of TSH being transferred from parents to children are 60%, while that of free T4 is 20% to 60% (11).
Causes of Hypothyroidism
The most common cause of primary hypothyroidism across the world is iodine deficiency (6). Within the United States, the most common cause of hypothyroidism is autoimmune thyroid disease, also called Hashimoto thyroiditis. Hypothyroidism may be caused by a defect of the hypothalamic–pituitary–thyroid axis. The following are causes of hypothyroidism (4, 6).
- Autoimmune Thyroiditis (Hashimoto’s Thyroiditis)
- Inflammatory condition in which the immune system mistakenly attacks and damages the thyroid gland, which leads to a gradual decline in thyroid function.
- Iatrogenic Causes
- Examples include the surgical removal of the thyroid gland (thyroidectomy) or radioiodine therapy for hyperthyroidism.
- These interventions may inadvertently cause insufficient thyroid hormone production.
- Congenital Hypothyroidism
- This is hypothyroidism acquired from birth. This can result from genetic factors, abnormal thyroid development, or maternal thyroid dysfunction during pregnancy.
- Medication-Induced Hypothyroidism
- Certain medications can interfere with thyroid hormone production. Close monitoring is essential for patients taking such medications.
- Iodine Deficiency
- Iodine is an essential component for thyroid hormone synthesis. Living in certain regions of the world with iodine insufficiency can increase the risk of inadequate intake of iodine. Iodine deficiency is less common in areas with iodized salt supplementation.
Types of Hypothyroidism
Primary Hypothyroidism
Primary hypothyroidism is due to impaired function of the thyroid gland, resulting in increased thyroid-stimulating hormone (TSH). Primary hypothyroidism causes about 99% of cases and may be accompanied by goiter (5).
Post-therapeutic hypothyroidism is damage to the thyroid function during radioactive iodine therapy or surgical treatment of hyperthyroidism or goiter. The use of radioactive iodine to manage Graves’ disease usually results in permanent hypothyroidism in about 80-90% of those patients. Radiation treatment to the head and neck area can also result in hypothyroidism.
Hypothyroidism can also result from the use of certain medications. These include amiodarone, thalidomide, oral tyrosine kinase inhibitors (sunitinib, imatinib) stavudine, interferon, bexarotene, perchlorate, rifampin, ethionamide, phenobarbital, phenytoin, carbamazepine, interleukin-2, and lithium (5). Research shows that a newer class of cancer medications, such as anti-CTLA-4 and anti-PD-L1/PD-1 therapy, is associated with both primary and/or secondary hypothyroidism.
Postpartum thyroiditis is found in about 10% of women and commonly presents 8-20 weeks after delivery.
Secondary and Tertiary Hypothyroidism
Secondary hypothyroidism, also known as central hypothyroidism, is caused by a defect in the hypothalamic-pituitary axis.
This form of hypothyroidism is related to the following (5):
- Pituitary tumors
- Tumors compressing hypothalamus
- Sheehan syndrome
- This syndrome occurs when significant blood loss results in damage to the anterior pituitary gland.
- Thyrotropin-releasing hormone (TRH) resistance or deficiency
- Thyrotropin-releasing hormone (TRH) is a hormone produced by neurons in the hypothalamus that stimulates the release of thyroid-stimulating hormone (TSH)
- Lymphocytic hypophysis
- Radiation therapy to the brain
- Drugs such as dopamine, prednisone, or opioids

Self Quiz
Ask yourself...
- How are primary and secondary hypothyroidism different?
- What is a common cause of primary hypothyroidism in the United States?
- Can you describe post-therapeutic hypothyroidism and why this occurs?
- What are some other hormones that are impacted by an underactive thyroid?
Pathophysiology
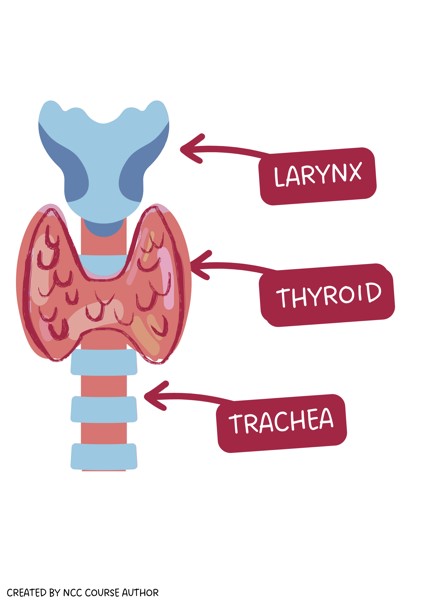
The thyroid gland is located in the neck anterior to the trachea and below the larynx and cricoid cartilage (8). It consists of right and left lobes connected by an isthmus. The thyroid weighs around 15 to 20 g (8).
The thyroid has two essential responsibilities in the endocrine system:
- Maintaining metabolic rate necessary for heat generation.
- Promotes normal growth and development from fetal life into childhood.
Thyroid follicles are the structural and functional units of a thyroid gland. They are spherical-shaped, and the wall is made up of a large number of cuboidal cells, the follicular cells, which are less than 0.5 mm in diameter. These follicular cells are the derivates of the endoderm and secrete thyroid hormone.
Follicles are filled with thyroglobulin, the glycoprotein precursor to thyroid hormone. The pool of thyroglobulin molecules is referred to collectively as a substance called colloid. The follicles are bundled into lobules by connective tissue, nerves (parasympathetic and sympathetic), blood vessels, and lymphatic tissue.

Self Quiz
Ask yourself...
- How would you describe the role of the endocrine system?
- Can you discuss how thyroid functioning impacts other systems in the body?
- If thyroid hormones maintain metabolic rates and heat generation, how would low or high levels be manifested?
- Have you ever cared for a patient with severe and untreated hypothyroidism?
Clinical Findings
Clinicians must ask why a certain sign or symptom is present. It is important to recognize the underlying physiological process.
For individuals with longer-term untreated hypothyroidism, signs and symptoms are more pervasive and involve multiple body symptoms. However, signs and symptoms of primary hypothyroidism are often subtle and less obvious.
As we mentioned, the thyroid's main job is to create the hormones T4 and T3 to control metabolism, which is the process by which food is broken down to produce energy. These hormones regulate how much energy to use. They also regulate body temperature and heart rate.
The amount of thyroid hormones in the bloodstream is controlled by the pituitary gland, which is located in the center of the skull below the brain. When the pituitary gland senses either a lack of thyroid hormone or too much, it adjusts its own hormone, called thyroid stimulating hormone, or TSH, and sends it to the thyroid to balance these levels.
The signs and symptoms can point to the cause. An essential part of differential diagnosis is to evaluate the impact on each system and consider other causative factors.
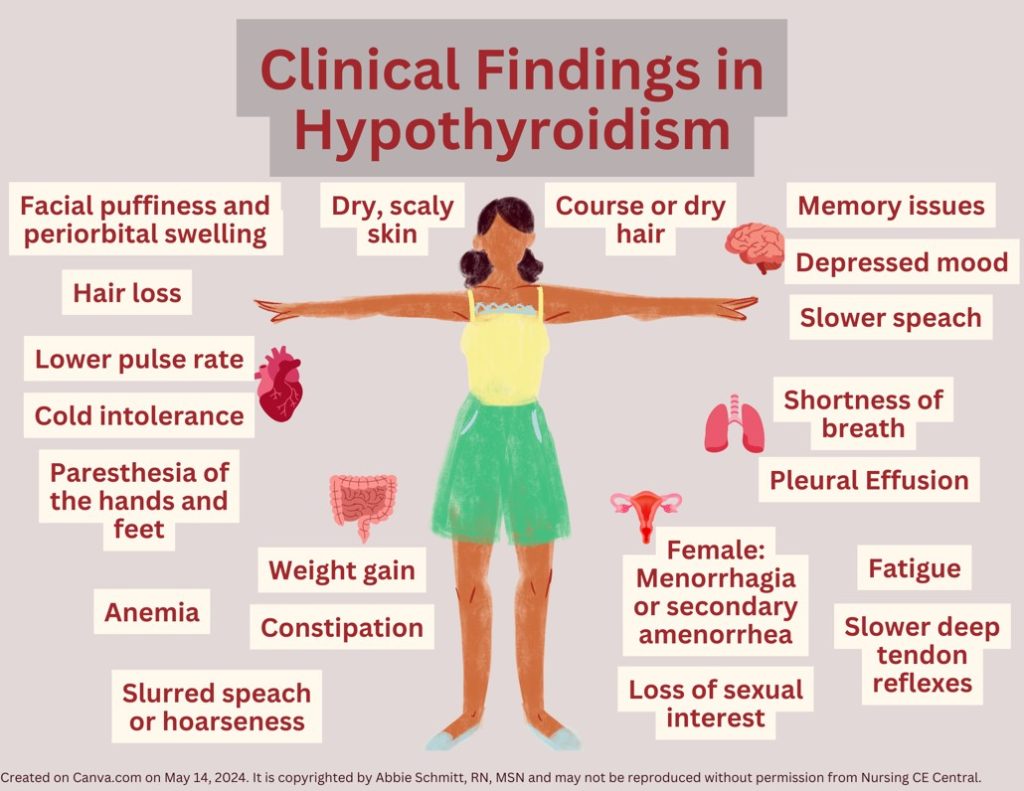
Hypothyroidism affects various organ systems in the body, including the central and peripheral nervous systems, and the cardiovascular, integumentary, gastrointestinal, muscular, reproductive, and hematopoietic systems.
Common symptoms include:
- Integumentary
-
- Myxedema (skin swelling and thickening)
-
- Dry, coarse skin and hair
-
- Hair loss
-
- Puffiness in the eyes and face
-
- Eyelid drooping
- Cardiac
-
- Bradycardia
-
- Diastolic hypertension
-
- Cold intolerance
- Neuromuscular
-
- Numbness and tingling in the hands and feet (paresthesia)
-
- Feeling depressed
-
- Feeling more forgetful or having “brain fog”
- Gastrointestinal
-
- Constipation
-
- Weight gain
- Respiratory system
-
- Shortness of breath
-
- Pleural effusion
- Muscular
-
- Muscle soreness and weakness
- Reproductive
-
- Decrease in sexual interest
-
- Frequent and heavy menstrual periods
- General
-
- Fatigue
-
- Voice may sound lower and hoarser
- Hematopoietic System
-
- Anemia
Myxedema refers to the appearance of the skin and subcutaneous tissues when severe hypothyroidism is present (5). Facial puffiness and periorbital swelling occur because of infiltration with mucopolysaccharides, known as hyaluronic acid and chondroitin sulfate. The eyelids droop due to decreased adrenergic drive (5). Hair may appear and feel coarse, dry, and sparse. The skin is also coarse, dry, scaly, and thickened. Facial expression may be dull. Myxedematous infiltration of the tongue causes thick, slurred speech; and infiltration of the larynx causes hoarseness.
Deficiency in thyroid hormones will also lead to decreased cerebral blood flow. In hypothyroidism, the decreased stroke volume and heart rate result in reduced resting cardiac output (5). These hemodynamic alterations cause pulse pressure to be narrowed, circulation time to be prolonged, and a reduction in blood flow to body tissues. Essentially, there is often a lower pulse rate. Decreased cutaneous circulation causes coolness and pallor of the skin as well as cold sensitivity.
Development of the CNS requires thyroid hormones and a deficiency in fetal life or at birth will lead to impaired neurologic development. Manifestations include hypoplasia of the cortical neurons, slowed myelination, and decreased vascularity (5). When thyroid hormone deficiency occurs in adulthood, manifestations are less severe, and symptoms usually respond easily to hormone therapy. Ongoing deficits lead to intellectual functions slowing down, including speech. Hypothyroidism may manifest with feelings of depression, a loss of initiative to perform tasks, and memory problems. There is prominent lethargy.
Modest weight gain is usually the result of decreased metabolism and fluid retention, caused by the hydrophilic glycoprotein tissue deposits, but usually does not exceed 10% of body weight (5). There is also reduced peristalsis, leading to constipation, contributing to weight gain. Symptoms that mimic mechanical ileus may occur, including gaseous abdominal distention (myxedema ileus), colicky pain, and vomiting.
Hypothyroidism affects the respiratory system and breathing due to the actions upon the central regulation of respiration, the reduced function of respiratory muscles, the upper airways, and the tongue. Generally, lung volumes are normal, but there are reductions in maximal breathing capacity and diffusing capacity. Pleural effusions may be noted. Severe hypothyroidism causes myxedematous changes in respiratory muscles and depression of the hypoxic and hypercapnic ventilatory drives. Hypothyroid patients have an increased likelihood of obstructive sleep apnea (5).
Body movements become slower and clumsier with cerebellar ataxia sometimes occurring. Numbness and tingling in the extremities are common. The relaxation phase of the deep tendon reflexes becomes slowed due to decreased rates of muscle contraction and relaxation. This is not a delay in nerve conduction, which is important when considering neurological conditions.
Females with hypothyroidism may develop menorrhagia or secondary amenorrhea. Another reproductive symptom would include decreased interest or drive for sexual activity.
The thyroid gland has a very important role in hematopoiesis. Thyroid hormones have a direct effect on blood parameters by stimulating erythrocytes precursors and indirectly by enhancing erythropoietin production. Individuals with hypothyroidism commonly have blood disorders. Patients with thyroid abnormalities may have low iron, folate, and B12 levels, which have been detected in up to 25% of patients (1). This will eventually impact the hemoglobin and the red blood cells (RBCs).
A goiter signifies an enlarged thyroid gland. It may be an overall enlargement of the thyroid, or it may be the result of irregular cell growth that forms one or more nodules in the thyroid. A goiter may or may not impact thyroid function.
Myxedema coma is a life-threatening complication of hypothyroidism and typically occurs in patients with a long history of untreated hypothyroidism. The clinical presentation can include a coma with extreme hypothermia, areflexia, seizures, and respiratory depression with carbon dioxide retention (2). Precipitating factors include illness, infection, trauma, medications (or substances that suppress the central nervous system), and exposure to cold.
Rapid diagnosis and treatment of myxedema coma are imperative because death will likely occur without rapid treatment.

Self Quiz
Ask yourself...
- How would you prioritize these symptoms from least to most worrisome?
- Can you think of any medications that have side effects that may mimic these symptoms? For example, certain antidepressants have side effects of weight gain.
- Can you discuss how insufficient thyroid hormone can impact respiration?
- How would you describe myxedema coma?
Advanced Health Assessment
An advanced health assessment for differential diagnosis of hypothyroidism involves a comprehensive evaluation that distinguishes hypothyroidism from other conditions with similar symptoms.
History and Physical
Gathering detailed information about the patient's symptoms, medical history, family history, and any medications or supplements they are taking is vital. These symptoms can be another medication condition or an effect of a medication. Remember, the common symptoms of hypothyroidism (fatigue, weight gain, cold intolerance, constipation, dry skin, hair loss, and depression) can be easily attributable to various diagnoses. Collecting information about physical and psychological symptoms; for example, ask about constipation, dry skin, muscle cramps, cold intolerance, insomnia, menstrual cycle changes, weight gain, anxiety, depression, difficulty focusing, or fatigue.
Ask if there is a family history of thyroid disease and any personal surgical, medication, psychosocial, and reproductive history (e.g., number of pregnancies and live births).
A thorough physical exam can help identify signs of hypothyroidism, such as dry skin, swelling, slowed reflexes, and goiter. Close examination of the neck and throat, palpating the thyroid gland to feel texture and firmness, and looking for skin/hair changes are important.
Vital signs provide valuable insight, including heart rate, blood pressure, temperature, respiratory rate, and pain levels.
Laboratory Tests
The most crucial tests for diagnosing hypothyroidism involve measuring levels of thyroid hormones and thyroid-stimulating hormone (TSH).
- TSH Test: High levels of TSH may indicate hypothyroidism. The pituitary gland produces more TSH to stimulate the underactive thyroid.
- Free T4 and Free T3 Test: Low levels of the thyroid hormone thyroxine (T4) and (T3) can confirm hypothyroidism.
Reference Ranges for Thyroid Function Tests:
The majority of TSH and free T4 assays used in industry are immunoassays, and their reference ranges are based on statistics to be between the 2.5th and 97.5th percentiles in a population with positive health indicators (11). The reference ranges vary according to age, sex, and ethnicity.
Additional Tests: Depending on the suspected cause of hypothyroidism, additional tests may be necessary:
- Thyroid Antibodies Test: This test can detect autoimmune thyroiditis (like Hashimoto's disease), which is a common cause of hypothyroidism.
- Ultrasound of the Thyroid: The structure of the thyroid gland is visualized, which can help identify nodules or abnormalities.
Diagnosis
Primary hypothyroidism is distinguished by (11):
- TSH values higher than the standard reference range (0.5-5 mIU/L)
- Free T4 levels below the patient-specific reference range
- The reference ranges for pregnant women are 0.1-2.5 mIU/L (first trimester), 0.2-3.0 mIU/L (second trimester), and 0.3-3.5 mIU/L (third trimester)
Fluctuation of Hormone Levels
The levels of TSH fluctuate throughout the day, with the peak value being in the late afternoon and evening. Individuals with severe hypothyroidism have very high TSH secretion, which may become erratic (11). Seasonal fluctuation has been noted and concentrations of TSH are higher in winter and spring, while they are lower in autumn and summer.

Self Quiz
Ask yourself...
- Can you explain why TSH would be higher in hypothyroidism?
- What vital sign abnormalities may be present in a patient with hypothyroidism?
- At what time of day do TSH levels peak?
- Are you familiar with performing an assessment and palpation of the thyroid gland?
Differential Diagnosis
The presence of hypothyroidism can be overlooked if the diagnosis is not considered adequately. Severe primary hypothyroidism is often not recognized. It is meaningful to consider other conditions that might mimic the symptoms of hypothyroidism.
Differential diagnosing hypothyroidism involves a systematic approach to rule out other conditions that share similar symptoms. We are going to break down each sign and symptom to expose other conditions with similar presentations.
These conditions may be considered in the differential diagnosis of hypothyroidism:
- Pernicious anemia
- Chronic renal insufficiency
- Depression
- Other hormonal disorders
- Nutritional deficiencies
- Autoimmune disorders
- Heart disease
- Euthyroid sick syndrome
- Goiter
- Myxedema coma
- Riedel thyroiditis
- Subacute thyroiditis
- Thyroid lymphoma
- Iodine deficiency
- Addison disease
- Chronic fatigue syndrome
- Dysmenorrhea
- Erectile dysfunction
- Infertility
Pernicious Anemia
There are several overlapping signs and symptoms of pernicious anemia and hypothyroidism. These symptoms include pallor, fatigue, weakness, and intolerance to cold. Blood tests showing low hemoglobin and hematocrit levels help differentiate anemia from hypothyroidism.
Chronic Renal Insufficiency
Chronic renal insufficiency and hypothyroidism may be suggested by anorexia, periorbital puffiness, torpor, anemia, and a sallow (yellow or grayish) complexion. It may be more difficult to distinguish hypothyroidism from nephrotic states by clinical examination alone.
Edema, pallor (or “waxy” pallor), hypometabolism, and hypercholesterolemia may suggest hypothyroidism. Also, total serum thyroxine concentrations may be decreased when large amounts of thyroid-binding globulin are excreted in the urine, yet the fT4 and TSH would be normal.
Depression
Depression is a mental health disorder that can mimic several symptoms of hypothyroidism, such as fatigue, feelings of sadness or despair, and weight changes. Depression typically lacks specific thyroid-related symptoms like cold intolerance and hair loss.
Adrenal Insufficiency
Fatigue, weight loss (or less commonly, gain), and low blood pressure can overlap in these conditions. Adrenal insufficiency may have symptoms like hyperpigmentation and electrolyte imbalances that are not typically present in hypothyroidism.
Pituitary Disorders
- Overlapping symptoms: May present with symptoms of multiple hormonal imbalances, including hypothyroidism.
- Distinguishing factors: Other hormonal deficiencies, such as in growth hormone or adrenal hormones, alongside imaging tests showing pituitary abnormalities.
Other Hormonal Imbalances
Conditions like Cushing's syndrome or hyperprolactinemia can cause symptoms that overlap with those of hypothyroidism. Low testosterone or adrenal insufficiency could also be considered. Similarly, conditions like hypoparathyroidism can have similar presentations. The distinguishing factors would include specific symptoms and hormonal test results.
Nutritional Deficiencies
Deficiencies in iron or vitamin B12, for example, can cause fatigue and other symptoms similar to hypothyroidism.
Autoimmune Disorders
Other autoimmune conditions like lupus or rheumatoid arthritis might initially present with symptoms that can be confused with hypothyroidism.
Heart Disease
Overlapping symptoms for various heart conditions include fatigue, abnormal pulse rate, and exercise intolerance. Distinguishing factors would include symptoms primarily related to cardiac function, such as chest pain and palpitations are key.
Euthyroid Sick Syndrome
Euthyroid sick syndrome is a condition in which serum levels of thyroid hormones are low in patients who have non-thyroidal systemic illness. Possible underlying system illnesses include starvation, protein-energy undernutrition, severe trauma, myocardial infarction, chronic kidney disease, diabetic ketoacidosis, cirrhosis, thermal injury, drug overdose, and sepsis (3).
Symptoms overlap with severe hypothyroidism, such as hypothermia, hypoventilation, hypotension, lethargy, or coma.
Decreased triiodothyronine (T3) levels are most common, but more severe or prolonged illnesses will result in decreased thyroxine (T4) levels (3). Thyroid-stimulating hormone (TSH) levels may be normal or even low (3).
Pathogenesis is unknown, but suspected to be a result of the following:
- Decreased peripheral conversion of T4 to T3
- Decreased clearance of rT3 generated from T4
- Decreased binding of thyroid hormones to thyroxine-binding globulin (TBG)
Treatment is directed toward the underlying illness and thyroid hormone replacement is not indicated.
Medication Effects
Certain medications can lead to symptoms mimicking hypothyroidism. A thorough review of the patient's medication history may reveal drugs known to affect thyroid function, such as lithium or amiodarone.
Sleep Apnea
Individuals with sleep apnea may have significant fatigue and cognitive impairment. Sleep apnea is characterized by episodes of breathing cessation during sleep, which can also impact heart rate and blood pressure.
Fibromyalgia
Fibromyalgia has classic symptoms of muscle and joint pain, fatigue, and sleep disturbances. Fibromyalgia usually involves widespread pain and tender points throughout the body, which are not specific to hypothyroidism.

Medical History and Demographic Considerations
Clinical diagnosis overlap often happens in older patients. Sometimes, slowed mental and physical activity, dry skin, and hair loss can mimic similar hypothyroidism findings. Older individuals often become hypothermic from cold exposure.
Hypothyroidism can develop from an extrinsic factor, an acquired condition, or due to a congenital defect that impairs TH biosynthesis (5).
About 20% of patients who have a surgical lobectomy develop hypothyroidism (5). There is also increased risk in locations of insufficient iodine or in patients who have anti-TPO (thyroid peroxidase) antibodies.
Hypothyroidism should be considered in the differential diagnosis of ovarian cysts and multi-cystic adnexal masses to avoid inadvertent surgery (9).

Self Quiz
Ask yourself...
- Can you name overlapping symptoms of hypothyroidism and heart disease?
- What are some underlying illnesses that cause euthyroid sick syndrome?
- Can you describe how differential diagnosis for hypothyroidism should be modified for older adults?
- Can you think of conditions that cause muscle soreness and malaise?
Case Study: Gertrude
Gertrude is a 40-year-old female who presented to her general physician for a regular check-up. Past medical history includes fibromyalgia and depression. Gertrude reported a family history of hypertension, Alzheimer’s disease, hypercholesterolemia, and Hashimoto's disease.
Gertrude is currently working as a schoolteacher and lives with her husband and teenage child. She has a sedentary lifestyle and reports occasional non-adherence to her medications due to forgetfulness.
Gertrude’s vital signs are as follows: Blood pressure (BP) 130/80 mmHg, heart rate (HR) 60 beats per minute (BPM), respiratory rate (RR) 18 breaths per minute, and temperature 98.6°F.
She is alert and fully oriented but complains of an intermittent headache. Her skin is warm and dry, and there is no visible edema. Lungs are clear on auscultation and heart sounds are normal rhythm with no murmurs. The abdominal assessment reveals no tenderness or masses. Body mass index (BMI) of 30, which indicates obesity.
Gertrude reports new symptoms that have slowly worsened over the previous 3 months. She reports worsening depression symptoms, changes in her menstrual cycle, hair loss, and intermittent tingling in her toes throughout the day.
- Are there any new symptoms that Gertrude is experiencing that could be attributed to more than one possible condition?
- Should the provider order any lab work or just refer this patient to a mental health provider, neurologist, and gynecologist?
- What are appropriate assessment questions to ask Gertrude?
- What would you focus on during a head-to-toe physical assessment?
Statistical Evidence
Let's incorporate current statistical evidence on the prevalence and risk factors for these conditions in the differential diagnosis of hypothyroidism.
These statistics are from recent studies (5, 9, 10):
- Hypothyroidism
-
- Prevalence: Varies by region but generally around 0.3-0.4% for overt hypothyroidism and 4-5% for subclinical hypothyroidism in the general population.
-
- Risk Factors: Female gender, older age, family history of thyroid disease, history of autoimmune conditions or specific surgeries or radiation therapy.
- Anemia
-
- Prevalence: Depends on the type; for example, iron deficiency anemia is very common worldwide, especially in women of childbearing age.
-
- Risk Factors: Poor diet, chronic bleeding (e.g., from ulcers), genetic conditions.
-
- Depression
-
- Prevalence: Approximately 5% globally in adults.
-
- Risk Factors: Family history of depression, major life changes, trauma, certain medications.
- Adrenal Insufficiency
-
- Prevalence: Primary adrenal insufficiency is rare, about 40-60 cases per million in developed countries.
-
- Risk Factors: Autoimmune disorders, infections, genetic predisposition.
- Sleep Apnea
-
- Prevalence: Estimated to affect about 3-7% of men and 2-5% of women in the general population.
-
- Risk Factors: Obesity, male gender, older age, family history.
- Fibromyalgia
-
- Prevalence: About 2-4% of the population, predominantly in women.
-
- Risk Factors: Female gender, middle age, family history.
- Pituitary Disorders
-
- Prevalence: Rare; specific prevalence depends on the type of pituitary disorder.
-
- Risk Factors: Genetic mutations, brain tumors, radiation treatment.
- Other Hormonal Imbalances
-
- Prevalence and Risk Factors: Vary widely depending on the specific hormonal disorder, such as diabetes, hypoparathyroidism, etc.
- Heart Disease
-
- Prevalence: One of the leading causes of morbidity and mortality worldwide; the prevalence varies by type of heart disease.
-
- Risk Factors: Family history, smoking, high blood pressure, high cholesterol, diabetes, obesity, sedentary lifestyle.

Self Quiz
Ask yourself...
- Can you discuss the prevalence of the above conditions?
- How do overlapping risk factors contribute to the likelihood of comorbidities?
Pharmacological Treatment of Hypothyroidism
The goal of treatment is to return blood levels of thyroid-stimulating hormone (TSH) and thyroxine (T4) to the normal range and to relieve symptoms.
Hypothyroidism is mainly treated with thyroid hormone replacement therapy, which is an oral T4 replacement called "levothyroxine." In most cases, symptoms of hypothyroidism begin to improve within two weeks of starting thyroid replacement therapy. However, people with more severe symptoms, especially muscle pain and weakness, may require several months of treatment before they fully recover.
The majority of individuals with hypothyroidism need to take levothyroxine for the rest of their lives.
The levothyroxine dose is 1.6 mcg/kg per day; however, in patients who are elderly and those who have atrial fibrillation, it is important to reduce the dose (6). Elemental supplements such as calcium and magnesium, to name a few, do affect the absorption of levothyroxine. Proton pump inhibitors also interfere with levothyroxine absorption.
Switching to the intravenous (IV) form in the hospitals is indicated when thyroid replacement orally is not possible or if myxedema coma is suspected; the dose of levothyroxine is reduced to generally 50% of the oral dose (6).

Self Quiz
Ask yourself...
- How would you describe the goal of treatment for hypothyroidism?
- How should levothyroxine dosing be adjusted for older adults or individuals with atrial fibrillation?
Follow Up and Monitoring
Effective treatment helps to achieve a clinical improvement of signs and symptoms and normal TSH (or free T4 levels as applicable). If symptoms persist despite normalization of TSH/free T4 levels, then non-endocrine etiologies should be considered.
Thyroid replacement treatment can exacerbate co-existing adrenal insufficiency. Patients with known or suspected adrenal insufficiency should be tested and treated. Adrenal insufficiency can also be associated with subclinical hypothyroidism that is reversible with treatment of the adrenal insufficiency. It is important to rule out or treat adrenal insufficiency when a patient has severe hypothyroidism, as with myxedema coma.
Patient Education
Patient education should be focused on hypothyroidism and properly taking medication.
Tips include:
- Levothyroxine should be taken once daily on an empty stomach (ideally one hour before eating or 2 to 4 hours after).
- It may be helpful to take the medication upon waking in the morning.
- Foods that are high in fiber, calcium or aluminum-containing antacids, and iron tablets can interfere with the absorption of levothyroxine and should be taken at a different time of day.
- It is preferable to stay on the same manufacturer of levothyroxine, rather than switching between brand name or generic formulations.
- Duration and dose: An initial dose of levothyroxine will be determined by the provider and then the blood level of TSH will be checked in six weeks. The dose can be adjusted at that time if needed. This process may need to be repeated several times before the hormone levels become normal and a therapeutic dose is found.
- Color-coded tablets can help with dose adjustments.
- Never increase or decrease the levothyroxine dose without talking with your healthcare provider.
The dose may need to be decreased with aging, after childbirth, or with weight changes. Most healthcare providers prescribe a lower initial dose of levothyroxine in older adults and those with coronary artery disease.
Over-replacement of T4 can cause mild hyperthyroidism, with the associated risks of atrial fibrillation and osteoporosis.

Case Study: Gertrude
Laboratory results show CBC and differential WBC are normal, serum TSH is 8.0 uIU/ml (reference range: 0.450 to 4.500 uIU/mL)
- Are there any follow-up labs that would be appropriate to collect?
- What education would be appropriate for Gertrude?
- Collaboration with which interdisciplinary team would be appropriate?
- Do you anticipate further studies and evaluation?
Conclusion
The differential diagnosis of hypothyroidism is a critical aspect of clinical practice, requiring meticulous attention to detail. The commonality of its symptoms—such as fatigue, weight gain, and cold intolerance—may overlap with other medical conditions. Differentiating these conditions requires a systematic approach. This process includes a thorough patient history, detailed physical examination, specific laboratory tests, and sometimes, advanced imaging techniques. Each of these components plays a vital role in accurately diagnosing hypothyroidism and ruling out other potential causes of the symptoms, ensuring that the patient receives appropriate treatment. The implications of correctly diagnosing hypothyroidism extend beyond immediate symptom management to long-term health outcomes and quality of life.
References + Disclaimer
- Ahmed, S. S., & Mohammed, A. A. (2020). Effects of thyroid dysfunction on hematological parameters: Case-controlled study. Annals of medicine and surgery, 57, 52–55. https://doi.org/10.1016/j.amsu.2020.07.008
- Boucai, L. (2024). Hypothyroidism. Merck Manual Professional Version. https://www.merckmanuals.com/professional/endocrine-and-metabolic-disorders/thyroid-disorders/hypothyroidism
- Boucai, L. (2024). Euthyroid sick syndrome. Merck Manual Professional Version. https://www.merckmanuals.com/professional/endocrine-and-metabolic-disorders/thyroid-disorders/euthyroid-sick-syndrome
- Kasper, D. L., Fauci, A. S., Hauser, S. L., Longo, D. L., Jameson, J. L., & Loscalzo, J. (2018). Harrison’s principles of internal medicine (20th ed.). McGraw-Hill Education.
- Moini, J., Pereira, K., & Samsam, M. (2020). Epidemiology of thyroid disorders. Elsevier.
- Patil N, Rehman A, Jialal I. Hypothyroidism. [Updated 2023 Aug 8]. In: StatPearls [Internet]. Treasure Island (FL): StatPearls Publishing; 2024 Jan-. Available from: https://www.ncbi.nlm.nih.gov/books/NBK519536/
- Pirahanchi Y, Toro F, Jialal I. Physiology, Thyroid Stimulating Hormone. [Updated 2023 May 1]. In: StatPearls [Internet]. Treasure Island (FL): Stat Pearls Publishing; 2024 Jan-. Available from: https://www.ncbi.nlm.nih.gov/books/NBK499850/
- Seifter, J., Sloane, D., & Walsh, E. C. (2022). Integrated physiology and pathophysiology. Elsevier.
- Tresa A, Rema P, Suchetha S, Dinesh D, Sivaranjith J, Nath AG. Hypothyroidism Presenting as Ovarian Cysts-a Case Series. Indian J Surg Oncol. 2021 Dec;12(Suppl 2):343-347. doi: 10.1007/s13193-020-01263-8. Epub 2021 Jan 2. PMID: 35035167; PMCID: PMC8716654.
- World Health Organization. (2021). Global health estimates: Leading causes of DALYs. https://www.who.int/data/global-health-estimates
- Zamwar, U. M., & Muneshwar, K. N. (2023). Epidemiology, Types, Causes, Clinical Presentation, Diagnosis, and Treatment of Hypothyroidism. Cureus, 15(9), e46241. https://doi.org/10.7759/cureus.46241
Disclaimer:
Use of Course Content. The courses provided by NCC are based on industry knowledge and input from professional nurses, experts, practitioners, and other individuals and institutions. The information presented in this course is intended solely for the use of healthcare professionals taking this course, for credit, from NCC. The information is designed to assist healthcare professionals, including nurses, in addressing issues associated with healthcare. The information provided in this course is general in nature and is not designed to address any specific situation. This publication in no way absolves facilities of their responsibility for the appropriate orientation of healthcare professionals. Hospitals or other organizations using this publication as a part of their own orientation processes should review the contents of this publication to ensure accuracy and compliance before using this publication. Knowledge, procedures or insight gained from the Student in the course of taking classes provided by NCC may be used at the Student’s discretion during their course of work or otherwise in a professional capacity. The Student understands and agrees that NCC shall not be held liable for any acts, errors, advice or omissions provided by the Student based on knowledge or advice acquired by NCC. The Student is solely responsible for his/her own actions, even if information and/or education was acquired from a NCC course pertaining to that action or actions. By clicking “complete” you are agreeing to these terms of use.
➁ Complete Survey
Give us your thoughts and feedback
➂ Click the Green MARK COMPLETE Button Below
To receive your certificate
