Course
Dysrhythmia Interpretation
Course Highlights
- In this Dysrhythmia Interpretation course, we will learn about various cardiac dysrhythmias.
- You’ll also learn and describe key differences between the various abnormal heart rhythms.
- You’ll leave this course with a broader understanding of signs and symptoms related to cardiac dysrhythmias.
About
Contact Hours Awarded: 3
Course By:
Amanda Marten MSN, FNP-C
Begin Now
Read Course | Complete Survey | Claim Credit
➀ Read and Learn
The following course content
Introduction
Dysrhythmias are abnormal heart rhythms identified by an electrocardiogram (EKG). Healthcare professionals, including LVN/LPNs, RNs, and APRNs, must be able to identify dysrhythmias since some are or can become life-threatening, especially if left untreated. It’s also helpful to understand their possible causes, signs, symptoms, and treatment options. This course reviews the different types of abnormal heart rhythms, including identification, causes, signs/symptoms, and treatment methods.
Sinus Bradycardia

Image 1. Sinus bradycardia (image attributed to Canva)
Sinus bradycardia occurs when a person’s heart rate is lower than the normal 60 to 100 beats per minute (bpm). EKG findings will show normal P and QRS complexes and intervals (normal sinus rhythm), but the rate will be less than 60 bpm. The condition occurs when the sinoatrial node (SA), which is the heart’s default pacemaker, produces electrical impulses that are slower than usual. Sinus bradycardia may be a normal finding in healthy adults, especially those who are athletes, or even during sleep for some individuals. Some other possible causes include myocardial infarction (MI), sick sinus syndrome, pericarditis, rheumatic fever, and hypothyroidism. Many medications can also cause sinus bradycardia, such as beta-blockers, digoxin, clonidine, lithium, and adenosine [5].
Most patients with sinus bradycardia don’t have any symptoms. However, if they do, some symptoms may include [5]:
- Dizziness
- Fatigue
- Syncope
- Chest pain
Physical assessment findings, in addition to a slow apical or peripheral pulse (less than 60 bpm), may include cyanosis, dyspnea, or abnormal lung sounds, like rales or crackles. Once identified, additional laboratory testing may be needed to identify possible underlying causes, such as thyroid tests, troponins, and electrolytes. If the patient’s vital signs are unstable, prompt treatment is necessary. Intravenous (IV) push 0.5mg of atropine is given every 3 to 5 minutes up to a maximum dosage of 3mg. If the patient still does not improve, then they may need to be placed on a temporary pacemaker. If an acute MI is initially discovered, then prompt cardiac intervention is necessary by alerting the on-call cardiologist and Cath Lab team [5].

Self Quiz
Ask yourself...
- What does the EKG for sinus bradycardia look like?
- What are some signs and symptoms of sinus bradycardia?
- What is the treatment for sinus bradycardia?
Sinus Tachycardia
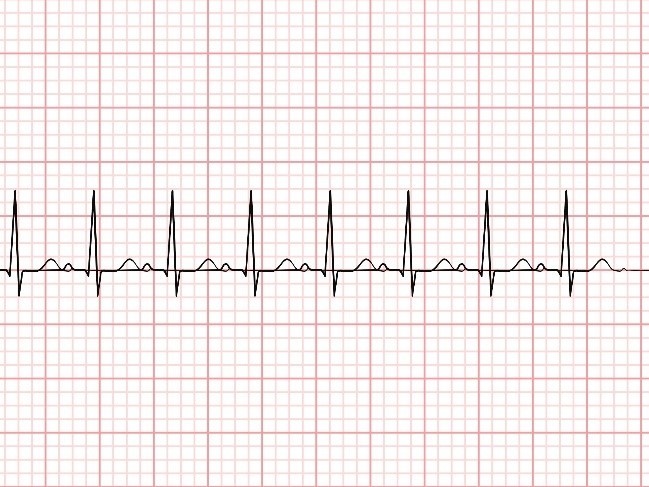
Image 2. Sinus tachycardia (image attributed to Canva)
Sinus tachycardia occurs when an individual’s heart rate is greater than 100 bpm. Electrocardiogram findings show normal P and QRS complexes and intervals (normal sinus rhythm), but the rate is greater than 100 bpm. The condition occurs when the SA node (SA) produces electrical impulses that are faster than usual. For infants and children, tachycardia is a normal physiologic finding, ranging from 100 to 150 bpm at rest. As they grow and age, a normal heart rate ranges from 60 to 100 bpm while at rest. During pregnancy, tachycardia may be present due to the body’s physiological changes. Additionally, tachycardia is the body’s normal response to exercise, pain, and stress. Abnormal underlying causes include myocarditis, cardiac tamponade, ventricular arrhythmias, and ischemic heart changes. Hyperthyroidism, hypoxia, sepsis, pulmonary embolism, dehydration, and low magnesium, calcium, and glucose are additional non-cardiac causes. Medications such as albuterol, atropine, epinephrine, levothyroxine, and scopolamine can cause tachycardia. Furthermore, withdrawal of certain medications can contribute to tachycardia, like digoxin, opioids, calcium channel blockers, magnesium, and alcohol [7].
Many patients with sinus tachycardia don’t have any symptoms. However, some may have symptoms like [7]:
- Palpitations
- Chest pain
- Lightheadedness
- Syncope or presyncope
Physical assessment findings will include a higher than normal apical or peripheral pulse. The nurse should look for signs of cardiovascular compromise, such as pulses paradoxus (blood pressure drops more than 10 mmHg when the patient takes a deep breath in), murmur, and S3 or S4 gallop. When sinus tachycardia is identified on EKG, investigating possible causes is the next step. Additional tests like a chest X-ray, cardiac enzymes, complete blood count (CBC), comprehensive metabolic panel (CMP), and others are useful. These tests are related to the possible underlying etiology. For example, if a patient is suspected of having sepsis, lactic acid and CBC may be ordered. If a pulmonary embolism is suspected, a D-dimer and chest CT may be ordered [7].
Once the underlying cause is identified, it’s treated accordingly to correct the tachycardia. For example, if the cause is sepsis, then IV antibiotics and fluids may be administered. If the cause is medication overdose, then the medication will be weaned or discontinued [7].

Self Quiz
Ask yourself...
- What does the EKG for sinus tachycardia look like?
- What are some signs and symptoms of sinus tachycardia?
- What is the treatment for sinus tachycardia?
Atrial Fibrillation
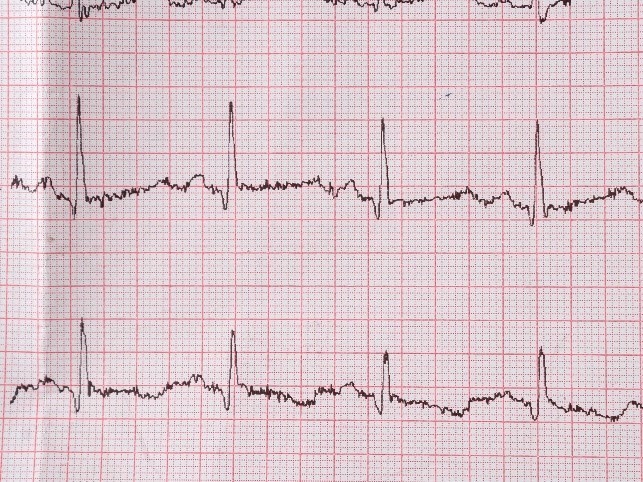
Image 3. Atrial Fibrillation (image attributed to Canva)
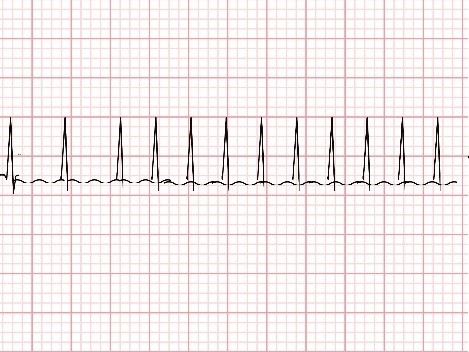
Image 4. Atrial Fibrillation with RVR (image attributed to Canva)
Atrial fibrillation (Afib or AF) is the most common heart arrhythmia; it’s an irregular heart rhythm that begins from the atria. On EKG, there are no visible P waves, and the QRS complexes are normal size but occur irregularly. Despite the irregular heart rate, the rate will be less than 100 bpm. Think of AF as the heart “quivering” without a regular beat [11]. Atrial fibrillation with a rapid ventricular response (AF with RVR) is the same irregular heart rhythm, but the heart rate is greater than 100 bpm [14].
Structural and electrical changes to the heart over time can contribute to the development of this condition. However, sometimes the underlying pathophysiology is not entirely understood, especially for those with persistent AF despite undergoing treatment. Some patient risk factors for developing AF are hypertension, alcohol use, stress, advanced age, and heart disease. Additional common causes of AF include obstructive sleep apnea, diabetes, hyperthyroidism, and pheochromocytoma [11].
Symptoms of atrial fibrillation vary greatly by patient. Some have serious symptoms, while others have no symptoms at all. If symptomatic, patients may present with [11]:
- Chest pain or palpitations
- Shortness of breath
- Dizziness
- Fatigue
- Exertional dyspnea
Since sometimes atrial fibrillation can be life-threatening, a thorough physical assessment is necessary. The nurse should look for signs of shock, heart failure, or stroke. If the patient is hemodynamically stable, then the patient’s risk stratification should be scored. They may be started on first-line rate-controlling medications, like beta-blockers or calcium channel blockers.
For those whose AF is not controlled by these medications, additional medications like amiodarone or other antiarrhythmics may be considered. A Transesophageal Echocardiogram (TEE) and/or cardioversion may ultimately be needed if the patient does not convert back to normal sinus rhythm with these medications or, in some cases, a catheter ablation. Anticoagulation is another factor to consider since patients are at increased risk of stroke and blood clots due to irregular heartbeat. The provider will review the patient’s comorbidities and contradictions to specific anticoagulants before starting. Examples of anticoagulants for AF are warfarin, apixaban, and rivaroxaban [14].
Treatment is different for patients who are hemodynamically unstable with AF or have AF with RVR. Immediate cardioversion and anticoagulant therapy are needed. Intravenous metoprolol or diltiazem may be initially administered in hopes of rate control. For individuals with new-onset AF awaiting cardioversion, they may be started on anticoagulants, like IV heparin or low-molecular-weight heparin (LMWH). Again, if cardioversion fails, then a catheter ablation, pacemaker, or percutaneous left atrial appendage occlusion procedure may be required [11, 14].

Self Quiz
Ask yourself...
- What does the EKG for atrial fibrillation look like?
- What are some signs and symptoms of atrial fibrillation?
- What is the typical treatment for atrial fibrillation?
Atrial Flutter

Image 5. Atrial Flutter (image attributed to Canva)
Atrial flutter is another common heart arrhythmia. The atrial rate is faster, and the ventricular rate will either be fixed or variable. On EKG, there will be several P waves (atrial contractions, sometimes updates of 300 bpm) followed by a QRS complex that can vary or occur after a specific amount of P waves. For example, there may be 4 atrial contractions (P waves) followed by a QRS complex (ventricular contraction), and the number of atrial contractions remains the same prior to the QRS complex (also known as fixed atrial flutter). With variable atrial flutter, the amount of P waves prior to the QRS complex varies. So, there may be 4 P waves and then a QRS followed by 3 P waves and a QRS complex. Atrial flutter looks similar to the ridges on a carpenter’s saw, kind of looking like a zig-zag pattern [18].
There are two types of atrial flutter: typical and atypical. Typical is more common, and it’s caused by abnormal electrical feedback in the heart’s atria coming from the right atrium, causing tachycardia. Atypical atrial flutter is less understood. Despite the type, conditions associated with or contributing to the development of atrial flutter include coronary artery disease, hyperthyroidism, diabetes, chronic obstructive pulmonary disease (COPD), and obesity. Alcohol use, hypoxia, digoxin toxicity, and electrolyte Imbalances are other possible causes [15, 18].
Some patients are asymptomatic, while some patients with atrial flutter will report symptoms like [15, 18]:
- Palpitations
- Fatigue
- Shortness of breath
- Feeling lightheaded or like they are going to pass out
Physical exam may reveal hypotension or signs of heart failure if severe, like jugular vein distension, lung crackles, or leg swelling. A CBC, X-ray, echocardiogram, or other diagnostic tests may be ordered to help determine the exact underlying cause [15, 18].
Treatment is aimed at attempting to control the rate, anticoagulation, and restoring the patient’s heart to normal sinus rhythm. To restore the patient with unstable vital signs to normal sinus rhythm, a cardioversion is needed. For patients who are stable, antiarrhythmic medications, like amiodarone, procainamide, or a calcium channel blocker (diltiazem) or beta-blocker (metoprolol), can be prescribed for cardioversion. Anticoagulants help reduce the likelihood of thromboembolisms forming, and the types are based on risk stratification scoring based on the patient’s history. For long-term rate control, calcium channel blockers and beta-blockers are prescribed [18].

Self Quiz
Ask yourself...
- What does the EKG for atrial flutter look like?
- What are some signs and symptoms of atrial flutter?
- What is the typical treatment for atrial flutter?
Premature Ventricular Contractions (PVCs)
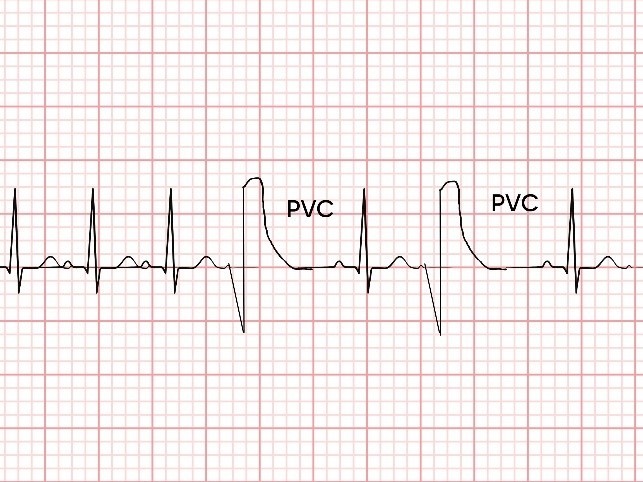
Image 6. Premature Ventricular Contractions (image attributed to Canva)
As its name implies, premature ventricular contractions (PVCs) are ventricular contractions or beats that occur before they are supposed to be in a normal sinus rhythm electrocardiogram. On EKG, there will be a premature and abnormally shaped, wide QRS complex (greater than 0.12 sec). So, this means the large QRS complex does not follow a P wave, as it would with normal sinus rhythm. Usually, it’s one single PVC on the EKG strip, but in some instances, there are two or three simultaneous PVCs, which are known as couplets or triplets, respectively [3].
Most PVCs are spontaneous and benign, and their exact cause is unknown. However, some known possible causes of PVCs are anxiety, electrolyte imbalances, alcohol use, and increased caffeine intake. Other possible causes are cardiomyopathy, MI, anemia, and hypertension. Individuals who are male or African American are also more likely to have PVCs [3].
Most people with PVCs don’t feel anything, and they are incidentally found on EKG. However, some may report symptoms like [3]:
- Heart fluttering or skipping a beat
- Palpitations
- Chest pain
- Anxiety
- Difficulty breathing
If PVCs are frequent, the nurse may note a single or few irregular beats during their physical assessment. However, for the majority of patients, the physical exam findings are unremarkable. Oftentimes, patients have to wear a Holter monitor for several days to detect the frequency of PVCs. Bloodwork may also be ordered to look for electrolyte disturbances or other possible causes. Most patients with infrequent PVCs don’t require treatment. If abnormal lab results or other etiologies are discovered, correcting these abnormalities is the treatment and usually reverses the PVCs. If patients have frequent PVCs or have symptoms, they may be prescribed a beta-blocker or calcium channel blocker. If medications do not control their frequency, then a radiofrequency catheter ablation may be necessary [3].

Self Quiz
Ask yourself...
- What does the EKG for PVCs look like?
- What are some signs and symptoms of PVCs?
- What is the treatment for PVCs?
Supraventricular Tachycardia (SVT)
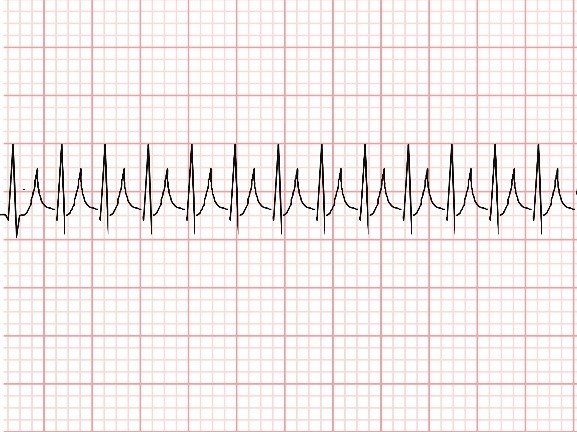 Image 7. Supraventricular tachycardia (image attributed to Canva)
Image 7. Supraventricular tachycardia (image attributed to Canva)
Supraventricular tachycardia (SVT) occurs when the body’s heart rate originates from the atrioventricular (AV) instead of the SA node and is greater than 100 bpm. Most people who have SVT have a heart rate of 150 to 220 bpm but it can increase upwards of 300 bpm. SVT is a sustained high heart rhythm and rate, whereas paroxysmal supraventricular tachycardia (PSVT) occurs occasionally and intermittently without any provoking factors. The EKG will show tall, narrow QRS complexes (less than 0.12 seconds), and oftentimes, P waves will be indistinguishable. Again, the heart rate will be 100 bpm or faster [13].
Some possible causes of SVT are alcohol and caffeine intake, stress, and certain medications. Symptoms often include [13]:
- Anxiety
- Palpitations and chest pain
- Syncope
- Dyspnea
Nurses should look for signs of poor perfusion, hemodynamic instability, or heart failure during their physical exam. A synchronized cardioversion is warranted for unstable patients. For stable patients, attempting the Valsalva maneuver is first recommended, followed by possibly carotid massage. If this does not resolve SVT, 6mg of IV adenosine may be administered up to a maximum of 12 mg. Diltiazem or metoprolol may be given after adenosine if the patient’s heart fails to respond to initial methods. Patients with SVT are often prescribed long-term medications like beta-blockers [13].

Self Quiz
Ask yourself...
- What does the EKG for supraventricular tachycardia look like?
- What does the EKG for paroxysmal supraventricular tachycardia look like?
- What are some signs and symptoms of supraventricular tachycardia?
- What is the treatment for supraventricular tachycardia?
Ventricular Tachycardia
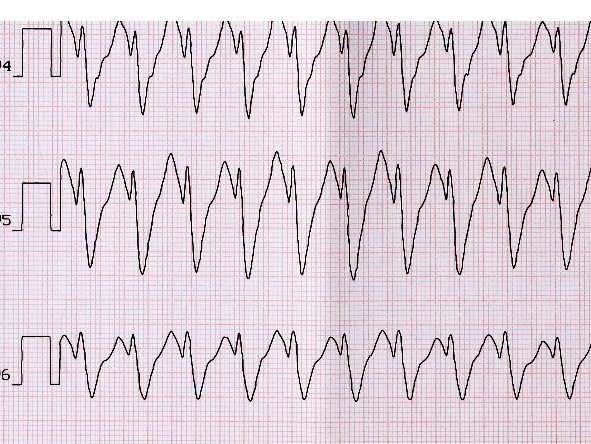 Image 8. Monomorphic ventricular tachycardia (image attributed to Canva)
Image 8. Monomorphic ventricular tachycardia (image attributed to Canva)
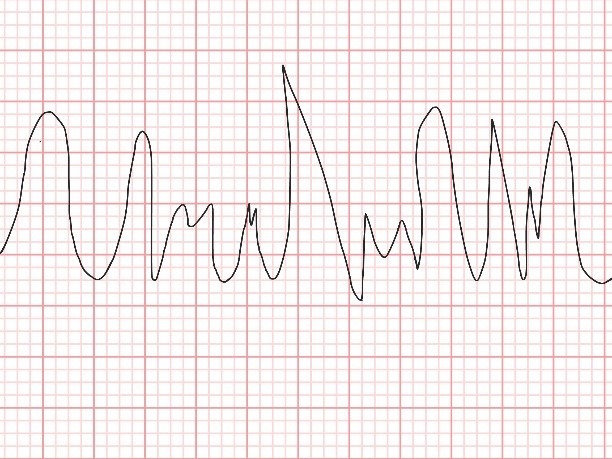 Image 9. Polymorphic ventricular tachycardia (image attributed to Canva)
Image 9. Polymorphic ventricular tachycardia (image attributed to Canva)
Ventricular tachycardia is considered a potentially life-threatening heart dysrhythmia, especially if left untreated. It occurs when the heart’s ventricles contract for three or more beats in a row and at a rate greater than 100 bpm. In monomorphic ventricular tachycardia, the EKG will show a rapid (greater than 100 bpm) and regular rhythm with wide QRS complexes (greater than 0.12 secs) that have the same amplitude (height). P waves are not distinguishable in this type of rhythm. Ventricular tachycardia can also be polymorphic, where the amplitude of the QRS complexes varies. Possible causes of ventricular tachycardia include myocardial ischemia, cardiomyopathy, and coronary artery disease. Electrolyte abnormalities, sepsis, and structural heart disease may also contribute to the development of this condition [4].
Patients can present cardiac arrest or sudden cardiac death or with varying symptoms like [4]:
- Chest pain
- Palpitations
- Shortness of breath
- Syncope
Upon physical exam, the nurse should assess for signs of instability, like hypotension, reduced perfusion, and heart failure. If a patient in an inpatient facility is in ventricular tachycardia, the nurse should check for a pulse and alert the provider and rapid response/code blue healthcare team and begin the advanced cardiac life support (ACLS) protocol, which typically involves defibrillation and administering epinephrine. If the patient is in outpatient care, the nurse should call 911, alert other team members to obtain an automated external defibrillator (AED) to connect the patient to and attempt to obtain IV access while possibly starting the ACLS protocol. However, actions are dependent on the facility’s policies. These patients are followed by a cardiologist and require long-term follow-up. They may require frequent cardioversion or a permanent implantable cardiac defibrillator [1, 4].

Self Quiz
Ask yourself...
- What does the EKG for ventricular tachycardia look like?
- What does the EKG for monomorphic versus polymorphic ventricular tachycardia look like?
- What are some signs and symptoms of ventricular tachycardia?
- What is the treatment for ventricular tachycardia?
Torsade de Pointes
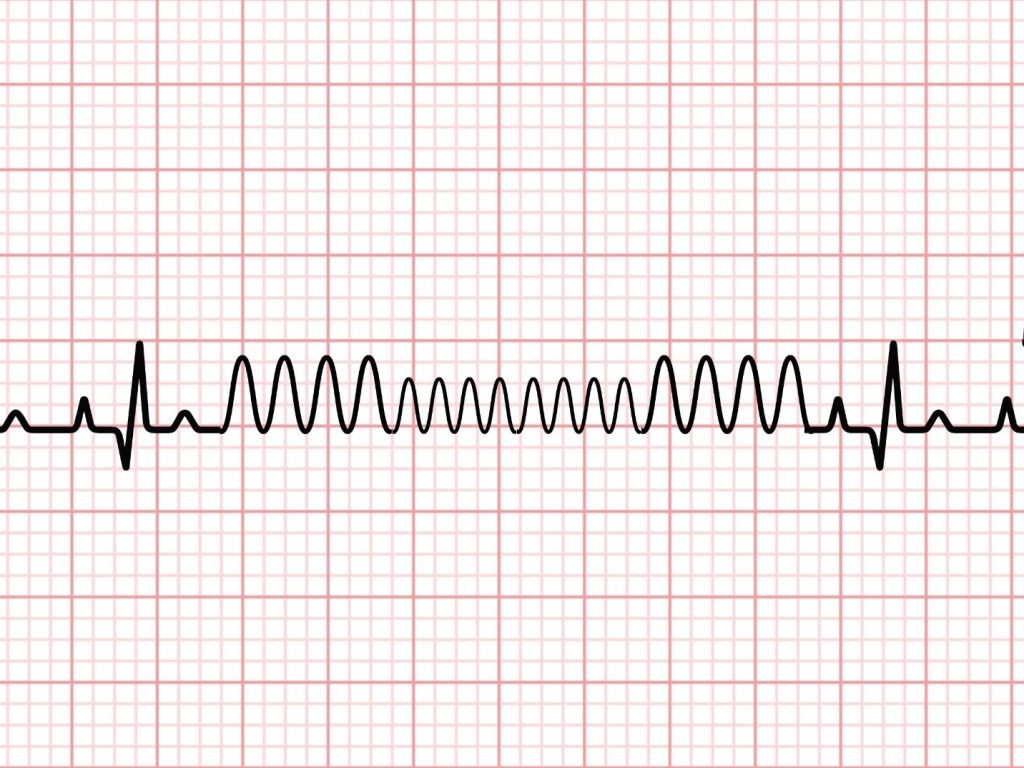 Image 10. Torsade de Pointes (image attributed to Canva)
Image 10. Torsade de Pointes (image attributed to Canva)
Torsade de Pointes is considered a type of ventricular tachycardia, which can sometimes resolve on its own, or patients can go into ventricular fibrillation. However, the EKG will have rapid (greater than 100 bpm) and wide QRS complexes (greater than 0.12 secs) that have alternating amplitude. Again, there is the absence of P waves. The key feature to tell this rhythm apart from polymorphic ventricular tachycardia is that the QRS complexes will appear to “twist” around the center line (isoelectric line) in Torsade de Pointes. This heart dysrhythmia typically originates from QT prolongation and delay, which is often drug-induced or congenital. Some classes of medications that can cause this condition are antiemetics, antifungals, antimicrobials, and some antiarrhythmics as well [2].
Many patients with Torsade de Pointes don’t have any symptoms, but if they do, some common symptoms include [2]:
- Palpitations
- Dizziness
- Syncope
Patients may become hypotensive and lose consciousness with Torsade de Pointes. Treatment aims to identify the underlying cause, such as medications or electrolyte disturbances. If it’s medication-induced, the treatment is to discontinue the medication immediately. Patients usually have “runs” of torsades that intermittently spontaneously resolve. Intravenous magnesium may be given to help or isoproterenol. Synchronized cardioversion is needed for unstable patients with a pulse. Those who are unstable and without a pulse require defibrillation. Again, IV magnesium may be administered if it is low. Some patients require pacing. Regardless of treatment, patients with torsades must be closely monitored. Individuals with congenital torsades are typically advised not to exercise and require frequent follow-up with a cardiologist [2].

Self Quiz
Ask yourself...
- What does the EKG for Torsade de Pointes look like?
- What are some signs and symptoms of Torsade de Pointes?
- What is the treatment for Torsade de Pointes?
Ventricular Fibrillation
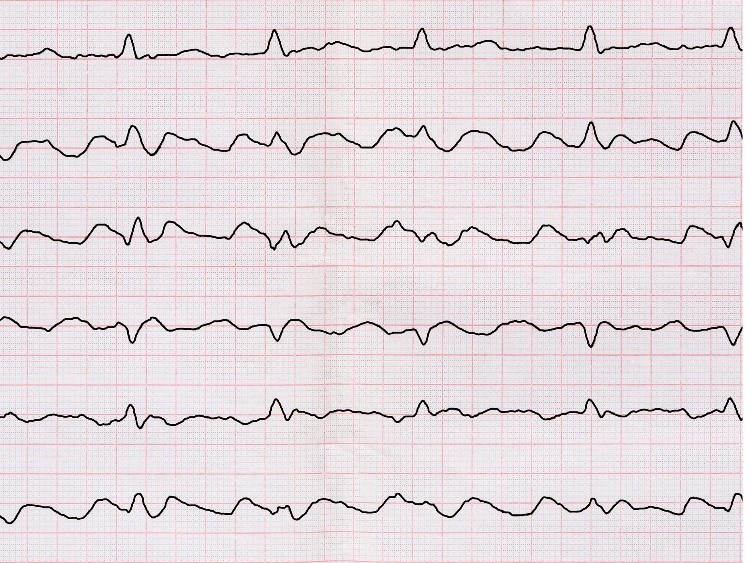
Image 11. Ventricular fibrillation (image attributed to Canva)
Ventricular fibrillation is another life-threatening dysrhythmia that occurs when the ventricles contract erratically. It arises from increased automaticity, triggered activity, or pulse conduction issues. On EKG, there are no recognizable P waves, QRS complexes, or T waves. Causes of this dysrhythmia are myocardial infarction, electrolyte imbalances, hypoxia, cardiomyopathy, and alcohol use. Sudden cardiac arrest is the most common sign of ventricular fibrillation [9]. However, other symptoms may include [9]:
- Chest pain
- Shortness of breath
- Nausea and Vomiting
During physical assessment, patients will be unconscious and have no palpable pulse. Once identified, the nurse should begin cardiopulmonary resuscitation (CPR) and call for help (either via 911 or Code Blue). If inpatient, the healthcare team usually follows ACLS protocol for treatment, which involves administering 1mg IV push epinephrine every 3-5 minutes, 2 minutes of CPR, and defibrillation by delivering a shock to the heart. During this time, the provider may look for and treat reversible causes, like electrolyte imbalances, toxins, or hypoxia. Intravenous amiodarone or lidocaine may also be administered, and an endotracheal airway may be inserted if the patient doesn’t already have one in place [1, 9]. This process of CPR, defibrillation, and administering medications may go on for several minutes until there is a return of spontaneous circulation, including a palpable pulse, and the EKG rhythm is non-life-threatening [9].

Self Quiz
Ask yourself...
- What does the EKG for ventricular fibrillation look like?
- What are some signs and symptoms of ventricular fibrillation?
- What is the treatment for ventricular fibrillation?
Left Bundle Branch Block
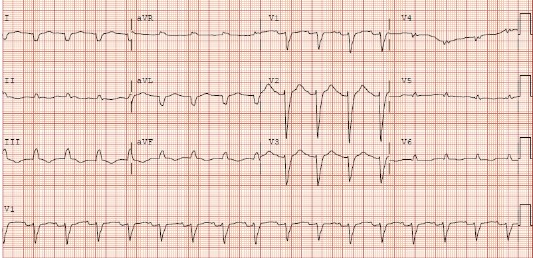
Image 12. Left bundle branch block (20)
A left bundle branch block (LBBB) occurs when there is abnormal conduction through the Bundle of His and Purkinje fibers of the heart. On electrocardiogram, the QRS complexes will be wide (greater than 0.12 seconds), lead V1 will have QS, or a small r wave followed by a large S wave, and lead V6 will have a notched R wave and no Q wave. These parameters are defined by the American College of Cardiology and the American Heart Association [17]. LBBBs are often caused by stretching of the heart’s tissue. Myocardial infarction, coronary artery disease, heart failure, and cardiomyopathy often cause this dysrhythmia [16].
Most patients with an LBBB are asymptomatic, and it’s found incidentally on electrocardiogram. However, the presence of an LBBB is a large indicator of coronary heart disease. If new onset, then other underlying conditions must be assessed and investigated, like the possibility of acute MI, heart failure, or cardiomyopathy. For patients without symptoms and no underlying heart conditions present, then treatment is not necessary. If symptoms develop or a syncopal episode, they may need a pacemaker implanted. Patients should be followed by a cardiologist closely [16].

Self Quiz
Ask yourself...
- What does the EKG for an LBBB look like?
- What are some signs and symptoms of an LBBB?
- What is the treatment for an LBBB?
Right Bundle Branch Block
 Image 13. Right bundle branch block (19)
Image 13. Right bundle branch block (19)
Similar to a left bundle branch block, a right bundle branch block (RBBB) is an abnormal conduction through the heart’s Bundle of His and Purkinje fibers [6]. There are several EKG findings that correlate with an RBBB, which include [6]:
- Widened QRS complexes
- Lead V1 and V2 RSR’ (also called “rabbit ears”)
- Leads 1 and V6, large S wave (greater than 40 milliseconds) OR S wave is longer than R wave
- Leads V5 and V6 have a normal R wave peak
- Lead V1, the R wave peak is greater than 0.5 milliseconds
Structural changes in the heart, trauma, myocarditis, infections, fibrosis, and myocardial ischemia can cause this dysrhythmia. Most patients do not have symptoms, and again, an RBBB is discovered on a routine EKG. Physical exam may reveal a split-second heart sound. If a new RBBB is discovered and the patient has symptoms, then an emergency evaluation is warranted. Treatment involves identifying the underlying cause [6].

Self Quiz
Ask yourself...
- What does the EKG for an RBBB look like?
- What are some signs and symptoms of an RBBB?
- What is the treatment for an RBBB?
Atrioventricular Blocks (AV Blocks)
Atrioventricular (AV) blocks occur when this is a conduction delay or blockage between the heart’s atria and ventricles. There are four types of AV blocks: first degree, second degree type I, second degree type II, and third degree, which are discussed below.
First Degree AV Block

Image 14. First degree AV block (image attributed to Canva)
A first degree AV block occurs when conduction is slowed through the heart’s AV node. The conduction delay may occur anywhere along the AV node, right atrium, or Purkinje fibers and Bundle of His. This is evidenced on EKG by a consistently prolonged PR interval of more than 0.20 seconds (remember, the normal PR interval is 0.12 to 0.20 seconds). QRS complexes will be of normal size and width and still follow the P waves, but there’s just a delay. Increased vagal tone, cardiac fibrosis, myocardial infarction, electrolyte imbalances, and infections can cause this condition. Some neuromuscular disorders and degenerative diseases can contribute to this dysrhythmia as well [12].
Patients will often be asymptomatic with a first degree AV block, and the physical exam is often unremarkable. However, patients with a PR interval of 0.30 seconds or more are more likely to have symptoms like [12]:
- Difficulty breathing
- Chest pain
- Presyncope or syncope
- Fatigue
Treatment involves obtaining a thorough patient history of possible contributing factors and personal and familial medical history. Treatment is often not required for most patients. For patients with an MI causing the first degree AV block, initial emergency treatment, like cardiac catheterization, is needed. Sometimes, patients may need a permanent pacemaker implanted if the block or delay becomes more severe [12].

Self Quiz
Ask yourself...
- What does the EKG for a first degree AV block look like?
- What are some signs and symptoms of a first degree AV block?
- What is the treatment for a first degree AV block?
Second Degree AV Block, Type I (Wenckebach)
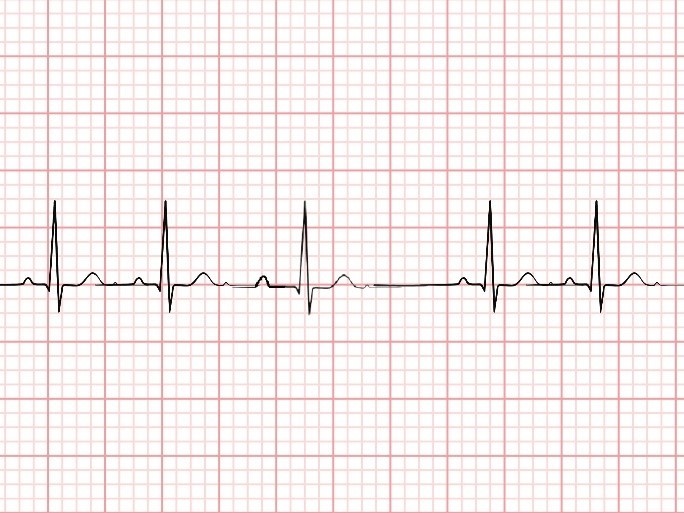 Image 15. Second degree AV block, type I (image attributed to Canva)
Image 15. Second degree AV block, type I (image attributed to Canva)
A second degree type I AV block, also known as Wenckebach, occurs when conduction is slowed through the AV node. The EKG will have a PR interval that progressively gets longer and longer until a QRS complex is completely missed or “dropped.” So, each P wave will be followed by a QRS complex until one P wave is not followed by a QRS complex, indicating a missed beat. Conditions like myocardial ischemia, hyperkalemia, rheumatic fever, heart tumors, and cardiomyopathy can cause this dysrhythmia. Additionally, medications like digoxin, calcium channel blockers, and some immunosuppressants can cause a second degree type I AV block [10].
Patients with a second degree type I AV block are most likely not to experience symptoms. However, some individuals may have symptoms like fatigue, syncope, chest pain, and shortness of breath. Upon assessment, they may be bradycardic, diaphoretic, or hypotensive. If these are present, IV atropine is administered, and sometimes pacing is needed. If not already in the hospital, patients should be sent to the emergency department via ambulance for monitoring and hospital admission. If this type of block is caused by medications, then they should be discontinued [10].

Self Quiz
Ask yourself...
- What does the EKG for a second degree AV block type I, look like?
- What are some signs and symptoms of a second degree AV block, type I?
- What is the treatment for a second degree AV block, type I?
Second Degree AV Block, Type II (Mobitz II)
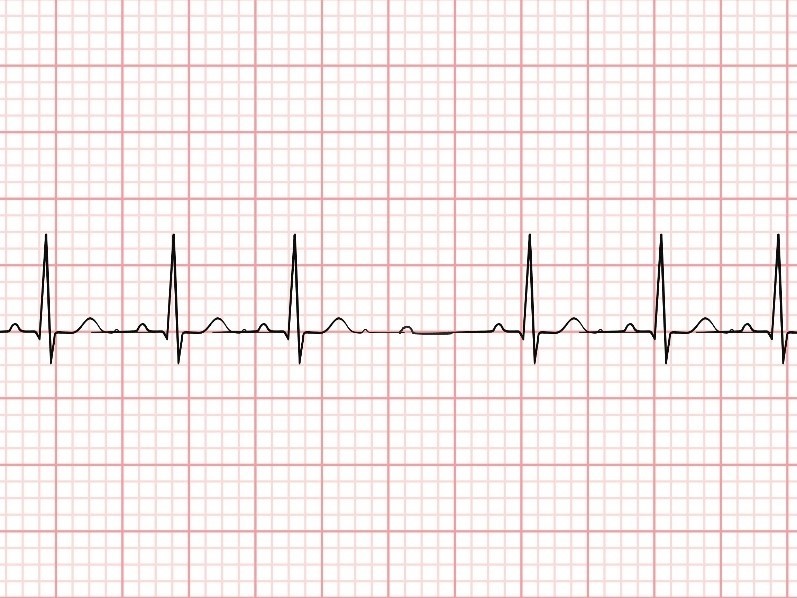
Image 16. Second degree AV block, type II (image attributed to Canva)
A second degree type II AV block, also known as Mobitz II, occurs when conduction is slowed through the AV node. The EKG will have a constant PR interval and QRS complexes, until there is one PR interval not followed by a QRS complex. The key difference between a second degree type I and type II is that in a type II, the PR interval always remains the same. Oftentimes, too, the QRS complexes will be wider than normal. Causes of a second degree type II AV block are similar to a type I and include myocardial ischemia, hyperthyroidism, rheumatic fever, and others. Again, the medications as listed above for a second degree type I also may cause a second degree type II block [10].
Patients with a second degree type II AV block will have symptoms of chest pain, syncope, and dyspnea. Sudden cardiac arrest is another presentation, along with diaphoresis, hypotension, and bradycardia. This dysrhythmia has a high likelihood of advancing to a third-degree AV block, so it is treated emergently. Immediate transcutaneous or transvenous pacing is required, and eventually, patients will need a permanent pacemaker [10].

Self Quiz
Ask yourself...
- What does the EKG for a second degree AV block, type II, look like?
- What are some signs and symptoms of a second degree AV block, type II?
- What is the treatment for a second degree AV block, type II?
Third Degree AV Block
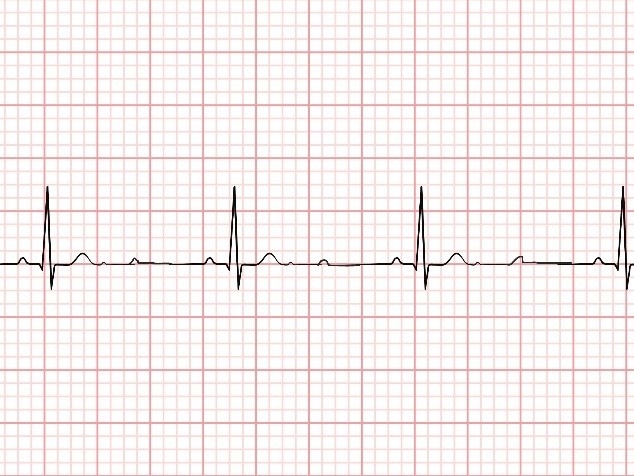
Image 17. Third degree AV block (image attributed to Canva)
A third-degree AV block occurs when the conduction between the SA and AV nodes is completely blocked, causing the SA and AV nodes to transmit signals independently. This condition is life-threatening. This is evidenced on the EKG by there being no correlation between the P waves and QRS complexes. Digoxin, sarcoidosis, amyloidosis, acute MI, and other conditions can cause this dysrhythmia [8].
Patients will have symptoms such as fatigue, chest pain, shortness of breath, and syncope. Bradycardia, diaphoresis, altered mental status, and hypotension are evident on physical exam. Emergency evaluation and treatment are necessary for patient survival. Pacing and other medications to stabilize the patient are needed, and patients require close monitoring in the hospital until the underlying cause is identified and treated [8].

Self Quiz
Ask yourself...
- What does the EKG for a third degree AV block look like?
- What are some signs and symptoms of a third degree AV block?
- What is the treatment for a third degree AV block?
Conclusion
It’s important for nurses to recognize signs and symptoms related to dysrhythmias. If patients present with any cardiac symptoms, an EKG is needed. Identifying the underlying EKG rhythm is necessary to begin prompt treatment, and in some cases, nurses can start CPR and administer life-saving medications before the provider or emergency team arrives. Understanding typical treatment for patients with any type of dysrhythmia helps improve patient education and outcomes.
References + Disclaimer
- American Heart Association. (2024). Algorithms. American Heart Association. Retrieved from https://cpr.heart.org/en/resuscitation-science/cpr-and-ecc-guidelines/algorithms
- Cohagan, B., & Brandis, D. (Updated 2023, August 8). Torsade de Pointes. In StatPearls. StatPearls Publishing. Retrieved from https://www.ncbi.nlm.nih.gov/books/NBK459388/
- Farzam, K., & Richards, J.R. (Updated 2023, August). Premature Ventricular Contraction. In StatPearls. StatPearls Publishing. Retrieved from https://www.ncbi.nlm.nih.gov/books/NBK532991
- Foth, C., Gangwani, M.K., Ahmed, I., & Alvey, H. (Updated 2023, July 30). Ventricular Tachycardia. In StatPearls. StatPearls Publishing. Retrieved from https://www.ncbi.nlm.nih.gov/books/NBK532954/
- Hafeez, Y., & Grossman, S.A. (Updated 2023, August 7). Sinus Bradycardia. In StatPearls. StatPearls Publishing. Retrieved from https://www.ncbi.nlm.nih.gov/books/NBK493201/
- Harkness. W.T., & Hicks, M. (Updated 2023, August 8). Right Bundle Branch Block. In StatPearls. StatPearls Publishing. Retrieved from https://www.ncbi.nlm.nih.gov/books/NBK507872/
- Henning, A., & Krawiec, C. (Updated 2023, March 5). Sinus Tachycardia. In StatPearls. StatPearls Publishing. Retrieved from https://www.ncbi.nlm.nih.gov/books/NBK553128
- Knabben, V., Chhabra, L., & Slane, M. (Updated 2023, July 31). Third Degree Atrioventricular Block. In StatPearls. StatPearls Publishing. Retrieved from https://www.ncbi.nlm.nih.gov/books/NBK545199/
- Ludhwani, D., Goyal, A., & Jagtap, M. (Updated 2023, August 8). Ventricular Fibrillation. In StatPearls. StatPearls Publishing. Retrieved from https://www.ncbi.nlm.nih.gov/books/NBK537120/
- Mangi, M.A., Jones, W.M., Mansour, M.K., & Napier, L. (Updated 2023, August 14). Second-Degree Atrioventricular Block. In StatPearls. StatPearls Publishing. Retrieved from https://www.ncbi.nlm.nih.gov/books/NBK482359/
- Nesheiwat, Z., Goyal, A., & Jagtap, M. (Updated 2023, April 26). Atrial Fibrillation. In StatPearls. StatPearls Publishing. Retrieved from https://www.ncbi.nlm.nih.gov/books/NBK526072/
- Oldroyd, S.H., Rodriguez, B.S., Makaryus, A.N. (Updated 2023, January 19). First Degree Heart Block. In StatPearls. StatPearls Publishing. Retrieved from https://www.ncbi.nlm.nih.gov/books/NBK448164/
- Patti, L., & Ashurst, J.V. (Updated 2023, August 7). Supraventricular Tachycardia. In StatPearls. StatPearls Publishing. Retrieved from https://www.ncbi.nlm.nih.gov/books/NBK441972/
- Rosenthal, L. (Updated 2019, November 18). Atrial Fibrillation Treatment & Management. Medscape. Retrieved from https://emedicine.medscape.com/article/151066-treatment#d11
- Rosenthal, L. (Updated 2019, November 18). Atrial Flutter. Medscape. Retrieved from https://emedicine.medscape.com/article/151210-overview#a4
- Sauer, W.H. (Updated 2024, March 28). Left Bundle Branch Block. UpToDate. Retrieved from https://www.uptodate.com/contents/left-bundle-branch-block#H6
- Scherbak, D., & Hicks, G.J. (Updated 2023, July 25). Left Bundle Branch Block. In StatPearls. StatPearls Publishing. Retrieved from https://www.ncbi.nlm.nih.gov/books/NBK482167/
- Ziccardi, M.R., Goyal, A., & Maani, C.V. (Updated 2022, December 8). Atrial Flutter. In StatPearls. StatPearls Publishing. Retrieved from https://www.ncbi.nlm.nih.gov/books/NBK540985/
- American College of Cardiology. (2017). ECG of the Month: Right Bundle Branch Block and Myocardial Infarction. Retrieved from https://www.acc.org/education-and-meetings/patient-case-quizzes/dec2017-ecg-of-the-month
- Emory School of Medicine. (2020). Left Bundle Branch Block. Retrieved from https://med.emory.edu/departments/emergency-medicine/sections/ultrasound/case-of-the-month/cardiac/left-bundle-branch-block.html
Disclaimer:
Use of Course Content. The courses provided by NCC are based on industry knowledge and input from professional nurses, experts, practitioners, and other individuals and institutions. The information presented in this course is intended solely for the use of healthcare professionals taking this course, for credit, from NCC. The information is designed to assist healthcare professionals, including nurses, in addressing issues associated with healthcare. The information provided in this course is general in nature and is not designed to address any specific situation. This publication in no way absolves facilities of their responsibility for the appropriate orientation of healthcare professionals. Hospitals or other organizations using this publication as a part of their own orientation processes should review the contents of this publication to ensure accuracy and compliance before using this publication. Knowledge, procedures or insight gained from the Student in the course of taking classes provided by NCC may be used at the Student’s discretion during their course of work or otherwise in a professional capacity. The Student understands and agrees that NCC shall not be held liable for any acts, errors, advice or omissions provided by the Student based on knowledge or advice acquired by NCC. The Student is solely responsible for his/her own actions, even if information and/or education was acquired from a NCC course pertaining to that action or actions. By clicking “complete” you are agreeing to these terms of use.
➁ Complete Survey
Give us your thoughts and feedback
➂ Click Complete
To receive your certificate
