Course
End Tidal CO2 and Waveform Capnography
Course Highlights
- In this End Tidal CO2 and Waveform Capnography course, we will learn about capnography.
- You’ll also learn indications for capnography use.
- You’ll leave this course with a broader understanding of the segments & phases represented on the capnograph.
About
Contact Hours Awarded: 1
Course By:
Michael York, MSN, RN
Begin Now
Read Course | Complete Survey | Claim Credit
➀ Read and Learn
The following course content
Introduction
Though capnography has been available for more than fifty years, it has just recently become a staple in the different procedural suites as a way of monitoring clients under procedural sedation (moderate or conscious sedation). Typically, the main form of monitoring respiratory status during procedural sedation has been through pulse oximetry. One issue with pulse oximetry is that by the time the oximeter shows a change, the client may already be in respiratory distress. Capnography is the monitoring of the end-tidal carbon dioxide (EtCO2). It shows real time changes in the respiratory status and any intervention needed can be done immediately.
Definitions
Before getting into the meat of capnography, the scene needs to be set by giving definitions of some key terms:
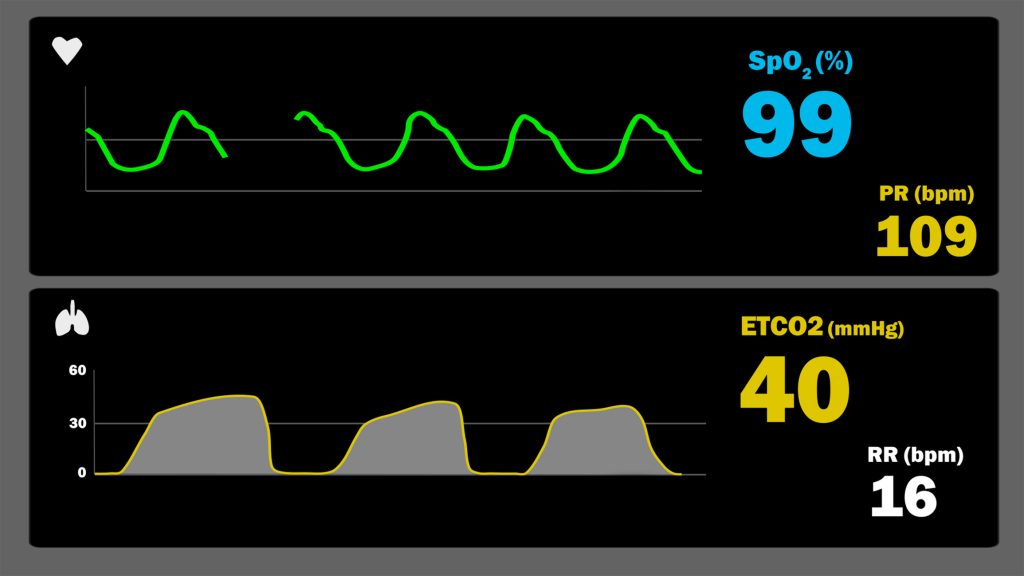
- Capnogram: Graphical illustration or waveform depicting carbon dioxide (CO2) levels when exhaled or the partial pressure, over a period of time (4, 5).
- Capnograph: This is an instrument which displays a capnogram and other digital data. In the clinical setting, a numeric value will be associated with the CO2 level as well as the waveform (4, 5).
- EtCO2: This is the concentration of CO2 at the end of expiration. This is a numeric measurement. EtCO2 levels (5):
- 35-45mmHg: normal
- Less than 35mmHg: hyperventilation/hypocapnia
- Greater than 45mmHg: hypoventilation/hypercapnia
Pulse Oximetry
Pulse oximetry has long been the standard of care for monitoring arterial oxygenation in the operating room and procedural areas. Due to its ease of operation requiring no new skills and noninvasive application, it became a main staple for anesthesia monitoring. It is able to warn the provider of early hypoxemia by providing a continuous numeric value of the arterial hemoglobin saturation of oxygen. It measures the hemoglobin saturation during the second phase of the oxygen transport process. One of the limitations of pulse oximetry is that it cannot measure the adequate oxygenation of tissues and organs (1).

Self Quiz
Ask yourself...
- What is the difference between a capnogram and a capnograph?
- What is end-tidal carbon dioxide?
- What does pulse oximetry monitor?
- What can pulse oximetry warn the provider of?
Capnography
Capnography is a noninvasive way to monitor ventilation and perfusion. Its use during and post anesthesiology and procedural sedation administration has been endorsed by numerous governing bodies, including the American Society of Anesthesiologists, the Association of PeriOperative Registered Nurses and the Association for Radiologic and Imaging Nursing (11).
Capnography waveforms show the concentration of CO2 during the expiration of breath over a period of time. This will allow the provider to see any changes and intervene appropriately (2). These observed changes can be seen in both ventilation and perfusion, giving key insights into assessing both the cardiovascular and respiratory function of the client.
During capnography monitoring, CO2 levels can be represented in two different cycles. These cycles are the pressure-versus-time and the pressure-versus-volume plots. Each of these cycles have different phases. The physiologic mechanisms that are present during the phases of time capnography can be matched-up to the phases of volume capnography.
Infrared (IR) light absorption is used to measure CO2 in most of the stand-alone capnographs. Different IR wavelengths allow CO2 to absorb the IR light. 4.3µm is an IR wavelength where CO2 absorption of IR light is especially strong (4, 6).

Self Quiz
Ask yourself...
- Name two organizations that have endorsed the use of capnography.
- What does capnography monitor?
- What are the two cycles that CO2 can be represented in?
- How is CO2 measured when using capnography?
Capnography Waveform Interpretation
The analysis of CO2 can be separated into three points; numbers (represented in the capnogram), curves (represented in the capnography) and differences (represented by the EtCO2). The CO2 values can give key insights into what is going on within the body. Blood CO2 levels, pulmonary status and ventilation status are among the key assessments that can be made through interpreting CO2 values. Noting exhaled CO2 could be the most important observation when managing an airway. If there is no exhaled CO2 on the capnograph, the client is probably not ventilating their lungs (4).
The capnograph waveform can be separated into phases and angles:
- Inspiratory Segment. During inspiration, phase 0, almost no CO2 passes over the CO2 sensor. This is when the capnograph tracing indicates the inspiratory baseline. During this phase, the CO2 concentration should be zero as there should not be any rebreathing of CO2. If the CO2 level at this time is more than zero, the client is rebreathing CO2.
- Expiratory Segment. The expiratory segment is further broken into phases; phase I, II, III and, at times, IV. Once the inspiration has completed, the lungs recoil and all the gasses move quickly up and out through the trachea. These gases, approximately one third of the tidal volume, pass over the CO2 sensor. On the capnograph, this phase looks like an extension of the horizontal baseline created during phase 0. During phase II, the capnograph should demonstrate a steep upstroke. This is when the CO2 concentrated gas is exhaled and passes over the gas sensor.
If the upstroke is more slanted and not so steep, this could indicate that there may be partially obstructed gas flow, the gas being sampled too slowly or the capnograph cannot match the client’s respiratory rate. The α-angle separates phase II and phase III. α-angle changes match the sequential alveolar emptying. This mirrors the overall ventilation/perfusion of the lungs. As the variations and changes in the lung increase, the slope of the a-angle increases. This brings us into phase III. As the breath continues to flow out the lungs, the capnogram flattens out with perhaps a slight incline. Due to the lung perfusion and ventilation not being equal in all lung units, the CO2 slowly continues to increase with the late emptying of the alveoli. The ß-angle follows directly after phase III. This is usually shown on the capnograph as a 90-degree angle. It represents the initiation of a new inspiratory segment as CO2 is inhaled and passes over the gas sensor (4, 6).

Self Quiz
Ask yourself...
- In capnography, what are the 3 points of analysis of CO2?
- What assessments can be made through the interpretation of CO2 values?
- What is another name for phase 0 on the capnograph?
- In phase 0, why should the CO2 concentration be 0?
- What phases are found during the expiratory segment?
- What should be seen on the capnography during phase III?
- What separates phase II and phase III?
- How is the ß-angle represented on the capnograph?
Indications
Capnography has a variety of different applications: general anesthesia, procedural sedation, endotracheal intubation, and hemodynamic monitoring.
General Anesthesia
Over the last few decades, pulse oximetry and CO2 capnography have become indispensable tools when administering general anesthesia. It was in the 1980s that the use of pulse oximetry and capnography changed the way that anesthesiologists were able to assess the way that oxygen was delivered throughout the body. This includes tissues and organs, cardiac output, respiratory function, metabolic state of the client, patency and security of the airway and how the anesthesia was affecting the body as a whole. Clearly, this technology was revolutionizing the entire way that anesthesia was administered and monitored.
By the 1990s, most professional bodies who dealt with the administration of anesthesia agreed that the use of capnography is the minimum standard of monitoring during the use of general anesthesia (7). When capnography was adopted as a standard of care in the operating room in the late 1980s, a closed-analysis study showed that the cases of adverse respiratory events took a serious decrease at the same time (12).
Procedural Sedation
Many procedures in the hospital can be discomforting and painful to clients. The majority of these procedures do not require general anesthesia, rather, analgesia or procedural sedation is all that is required to keep the client comfortable.
For this type of sedation, pulse oximetry (along with vital sign monitoring) has long been the standard of care. With procedural sedation, the client may or may not be responsive, able to answer questions and able to protect their airway. This type of sedation also has the potential for a client to lose their airway and have serious issues with ventilation and perfusion. Capnography is able to give insights into the respiratory status of the client with every breath. As such, the provider can see if the client is having any respiratory depression before it turns into an outright apneic episode.
The capnograph will show significant changes with each breath as the client is becoming hypoxic. With pulse oximetry, these changes are only seen after the client is already in distress. Capnography is much more able to predict apnea through the pre-apneic changes on the capnograph. This is especially useful when the client is undergoing procedural sedation. During a procedure, clients can very easily become oversedated. This is especially true when the client has comorbidities such as diabetes and/or chronic renal failure. The capnograph can indicate if the client is having respiratory depression (2).
Endotracheal Intubation
There are many different ways to ensure that an endotracheal tube (ETT) is properly placed. Breath sounds, vital sign monitoring and chest x-ray all help to verify proper placement. The addition of capnography is essential for quick verification and ongoing checks of ETT placement. The proper ETT placement would demonstrate a normal capnogram. If an esophageal placement was made, the capnography would show a decline in CO2 to almost a value of zero (4).
Hemodynamic Monitoring
Capnography is also useful for hemodynamic monitoring. It is a noninvasive means of obtaining valuable information about real-time gas exchange. For instance, there is a clear relationship between pulmonary perfusion and the elimination of CO2. This relationship is particularly useful in measuring pulmonary blood flow breath by breath. Clinical decisions can be made in real-time as opposed to after an episode of instability has occurred. Qualitative monitoring happens as these real-time changes in the expired CO2 are observed during an acute problem. Capnography can also be used to calculate the right cardiac output in a non-invasive way (10).


Self Quiz
Ask yourself...
- Name two indications for using capnography.
- How did capnography revolutionize respiratory and ventilatory assessment during the use of anesthesia?
- During procedural sedation, what problem can capnography help predict?
- What can capnography help verify during endotracheal intubation?
- When monitoring hemodynamics, what can the values in capnography help calculate?
Conclusion
EtCO2 monitoring through the use of waveform capnography is an essential piece of equipment to have when using any sort of general anesthesia or procedural sedation. Capnography is able to give the provider real-time information on the ventilation and perfusion of the client. When the provider can see the respiratory status of the client with each breath, they can take steps to avert any respiratory compromise with the client. Capnography can also be used to verify ETT placement. The CO2 values from the capnograph can be used to calculate pulmonary blood flow and cardiac output; this is useful when assessing the hemodynamics of the client. Overall, capnography is an extremely useful tool that the provider should be open to using in the correct environment.
References + Disclaimer
- Barker, S. J. (2021). Pulse oximetry. In Anesthesia equipment (pp. 253–270). Elsevier. https://doi.org/10.1016/b978-0-323-67279-5.00011-x
- Conway, A., Collins, P., Chang, K., Mafeld, S., Sutherland, J., Fingleton, J., & Parotto, M. (2019). Pre-apneic capnography waveform abnormalities during procedural sedation and analgesia. Journal of Clinical Monitoring and Computing, 34(5), 1061–1068. Retrieved September 7, 2024, from https://doi.org/10.1007/s10877-019-00391-z
- Fujimoto, S., Suzuki, M., Sakamoto, K., Ibusuki, R., Tamura, K., Shiozawa, A., Ishii, S., Iikura, M., Izumi, S., & Sugiyama, H. (2019). Comparison of end-tidal, arterial, venous, and transcutaneous pco2. Respiratory Care, 64(10), 1208–1214. Retrieved September 7, 2024, from https://doi.org/10.4187/respcare.06094
- Gravenstein, N., & Jaffe, M. B. (2021). Capnography. In Anesthesia equipment (pp. 239–252). Elsevier. https://doi.org/10.1016/b978-0-323-67279-5.00010-8
- Huff, M. E. (2019). End tidal carbon dioxide monitoring (capnography) in the cardiac intensive care unit. ScholarWorks @ UTRGV. Retrieved September 7, 2024, from https://scholarworks.utrgv.edu/som_pub/378
- Kreit, J. W. (2019). Volume capnography in the intensive care unit: Potential clinical applications. Annals of the American Thoracic Society, 16(4), 409–420. https://doi.org/10.1513/annalsats.201807-502cme
- McDougall, R. J., Morriss, W. W., Desai, P. K., & Batgombo, N. (2023). Getting capnography to the front lines. Anesthesia & Analgesia, 137(5), 929–933. Retrieved September 7, 2024, from https://doi.org/10.1213/ane.0000000000006690
- Minami, D., Murakami, E., Shibata, Y., Nakamura, K., Kishino, T., Takigawa, N., Onishi, K., Takigawa, Y., Shimonishi, A., Kudo, K., Sato, A., Sato, K., Fujiwara, K., & Shibayama, T. (2021). End-tidal capnographic monitoring during flexible bronchoscopy under fentanyl and midazolam sedation. Annals of Palliative Medicine, 10(8), 8665–8671. Retrieved September 7, 2024, from https://doi.org/10.21037/apm-21-1009
- Owens, B., & Hall, C. (2024). Application of end-tidal co2 monitoring to icu management. Critical Care Nursing Quarterly, 47(2), 157–162. Retrieved September 7, 2024, from https://doi.org/10.1097/cnq.0000000000000506
- Tusman, G., & Bohm, S. H. (2021). Clinical monitoring by volumetric capnography. In Cardiopulmonary monitoring (pp. 601–617). Springer International Publishing. https://doi.org/10.1007/978-3-030-73387-2_38
- Williams, K. (2022). Guidelines in practice: Moderate sedation and analgesia. AORN Journal, 115(6), 553–564. https://doi.org/10.1002/aorn.13690
- Wollner, E. A., Nourian, M. M., Bertille, K. K., Wake, P. B., Lipnick, M. S., & Whitaker, D. K. (2023). Capnography—an essential monitor, everywhere: A narrative review. Anesthesia & Analgesia, 137(5), 934–942. Retrieved September 7, 2024, from https://doi.org/10.1213/ane.0000000000006689
Disclaimer:
Use of Course Content. The courses provided by NCC are based on industry knowledge and input from professional nurses, experts, practitioners, and other individuals and institutions. The information presented in this course is intended solely for the use of healthcare professionals taking this course, for credit, from NCC. The information is designed to assist healthcare professionals, including nurses, in addressing issues associated with healthcare. The information provided in this course is general in nature and is not designed to address any specific situation. This publication in no way absolves facilities of their responsibility for the appropriate orientation of healthcare professionals. Hospitals or other organizations using this publication as a part of their own orientation processes should review the contents of this publication to ensure accuracy and compliance before using this publication. Knowledge, procedures or insight gained from the Student in the course of taking classes provided by NCC may be used at the Student’s discretion during their course of work or otherwise in a professional capacity. The Student understands and agrees that NCC shall not be held liable for any acts, errors, advice or omissions provided by the Student based on knowledge or advice acquired by NCC. The Student is solely responsible for his/her own actions, even if information and/or education was acquired from a NCC course pertaining to that action or actions. By clicking “complete” you are agreeing to these terms of use.
➁ Complete Survey
Give us your thoughts and feedback
➂ Click Complete
To receive your certificate
