Course
Endocarditis
Course Highlights
- In this Endocarditiscourse, we will learn about the definition and epidemiology of endocarditis.
- You’ll also learn the signs, symptoms, and physical exam findings of endocarditis.
- You’ll leave this course with a broader understanding of various treatments, patient education, and complications of endocarditis.
About
Contact Hours Awarded:
Course By:
Amanda Marten MSN, FNP-C
Begin Now
Read Course | Complete Survey | Claim Credit
➀ Read and Learn
The following course content
Introduction
Endocarditis is a serious medical condition that can affect any age group, although it’s more common in children and adolescents. It’s important for nurses and healthcare providers to recognize the signs and symptoms of endocarditis, diagnostics, treatment, and potential complications. This course aims to equip learners with knowledge related to endocarditis by reviewing its definition, epidemiology, pathophysiology, and etiology. This course also describes the signs and symptoms, diagnostic tests, and treatment. Lastly, it reviews potential complications along with patient education and new research.
Definition
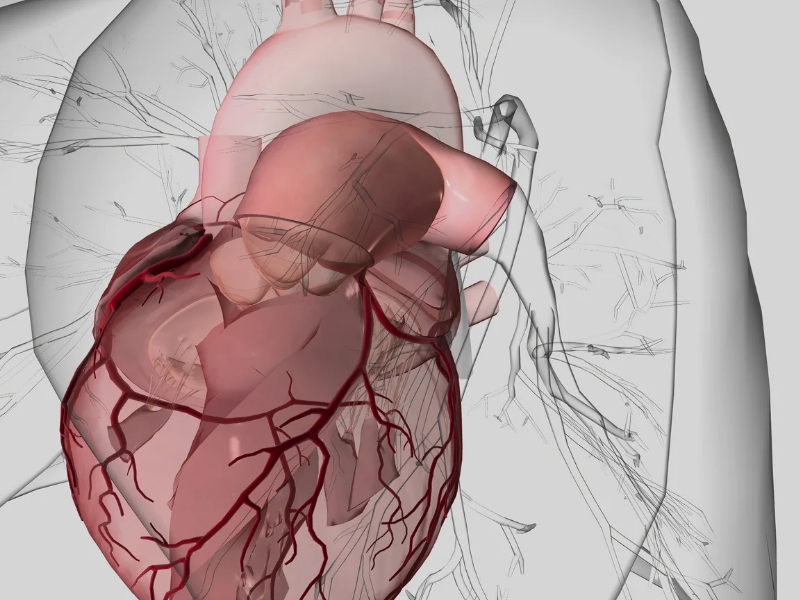
Endocarditis is a severe, life-threatening inflammation of the endocardium or heart’s inner lining (covering the atria, ventricles, and valves. There are both infective and noninfective causes, which are explained in further detail below. Noninfective endocarditis is less common than infective endocarditis [1].
Native valve endocarditis is referred to when a patient has endocarditis but has their original heart valve (so it’s not replaced) [3].
Epidemiology
In the United States, it’s estimated that there are around 12.7 cases of infective endocarditis in every 100,000 individuals annually [3]. Other sources estimate that about 5 in every 100,000 people per year develop infective endocarditis in the United States. This estimate is expected to rise due to the aging population and the presence of patients with several comorbid conditions, like type II diabetes. In addition to advanced age and comorbidities, cardiac implants are also a major risk factor. The mean age of individuals with infective endocarditis is 60.8 years old, with most cases occurring in patients above 50 years old [3, 6]. Additionally, infective endocarditis is found to be three times more common in males [3].
It’s currently estimated that healthcare-associated infective endocarditis accounts for about 50% of cases, with most cases acquired within 48 hours of hospital admission or in patients who had an invasive procedure within the six months prior. The number of healthcare-associated cases is expected to continuously rise [6].
Congenital heart disease is a common predisposing factor for endocarditis in developed countries. Patient history of a dental procedure within the 6 months prior is another risk factor for developing this condition as the bacteria can enter the bloodstream during these procedures [2, 5].

Self Quiz
Ask yourself...
- What is the definition of endocarditis?
- What is the epidemiology of infective endocarditis in the United States?
- Which populations are more likely to develop endocarditis?
Pathophysiology and Etiology
Noninfective endocarditis occurs when a blood clot forms on one of the heart valves. It typically develops secondary to conditions like congenital heart defects, rheumatic fever, cancers, disseminated intravascular coagulation (DIC), or autoimmune conditions, such as systemic lupus erythematosus [1].
Infective endocarditis is an infection of the endocardium typically caused by bacteria, but it can also develop from fungi, viruses, and other infectious agents. In pediatric patients, the most common bacteria contributing to this condition are Staphylococcus aureus and then Viridians-type streptococci. For intravenous (IV) drug users, Pseudomonas aeruginosa or Serratia marcescens are common bacterial agents [5].
The mitral heart valve is the most commonly affected valve and then the next most common is the aortic valve [5]. Rheumatic heart disease accounts for 30% of native valve endocarditis, while congenital heart disease accounts for 15% of cases [3].
Risk factors for developing endocarditis include diabetes, steroid use, and increased age. Prosthetic heart valves, IV drug use, prior heart valve damage (typically from rheumatic fever), and birth defects are also risk factors, especially for infective endocarditis [2, 5].

Self Quiz
Ask yourself...
- What is the pathophysiology of infective versus noninfective endocarditis?
- What is the etiology of endocarditis?
- What comorbid conditions and risk factors are associated with endocarditis?
Clinical Signs and Symptoms
The signs and symptoms of endocarditis vary per individual and will depend on the type, whether infective or noninfective. The symptoms of noninfective endocarditis usually mimic those of infective endocarditis but occur because emboli form, so most of the time, the patient lacks a fever [1]. Symptoms of infective endocarditis include [2, 3, 5]:
- Fever and chills (sometimes intermittent over several months for milder cases or persistently high for more severe cases)
- Lack of appetite
- Weight loss
- Fatigue
- Muscles and joint aches, back pain
- Headache
- Nausea and/or vomiting
- Night sweats
- Cough
- Shortness of breath
- Chest pain
Patients may also develop symptoms and physical exam findings of heart failure. Physical assessment often reveals a new heart murmur, petechiae, and subungual hemorrhages, which are dark red lesions under the nailbeds. Fever is the most common physical exam finding for patients with infective endocarditis. Osler’s nodes, which are tender, raised nodules or lumps that appear on the hands and feet, are also a common finding. Janeway lesions may also be identified, which are nontender, erythematous lesions on the palms of the hands and soles of the feet. Small retinal hemorrhages, also known as Roth spots, are indicative of endocarditis. Other neurological and cardiac findings may be present as well, like altered mental status or heart block [3, 5].

Self Quiz
Ask yourself...
- What are some typical signs and symptoms of endocarditis?
- What is a helpful differentiator of infective versus noninfective endocarditis?
- What are some physical examination findings of endocarditis?
Diagnostic Tests and Diagnosis
If endocarditis is suspected by either the nurse or healthcare provider, then diagnostic tests are ordered to confirm the diagnosis. If the patient is in an outpatient setting, then they should be immediately sent or transferred to the emergency room for immediate evaluation and a STAT workup. Initial diagnostic tests typically include a complete blood count (CBC), basic or complete metabolic panel (BMP or CMP), coagulation panel (PTT, PT, INR), blood cultures, electrocardiogram, and echocardiogram. It may be initially difficult to tell the difference between infective and noninfective endocarditis, so it’s imperative to obtain blood cultures as soon as possible to identify the underlying organism (if any). The provider may also order an erythrocyte sedimentation rate (ESR), chest x-ray, and rheumatoid factor (RF) [2, 3, 5]. An echocardiogram will often reveal one or multiple vegetations on one or more heart valves. Sometimes, a transesophageal echocardiogram (TEE) and color two-dimensional cardiac Doppler ultrasound may also be ordered to provide greater details of heart valve involvement [3].
The diagnosis of infective endocarditis is typically made using the modified Duke criteria. A definitive diagnosis can be made if the 2 major criteria are present, which are either two separate positive blood cultures or an echocardiogram revealing endocarditis. Minor criteria include a predisposing heart condition, fever, vascular phenomena (emboli, pulmonary infarcts, Janeway lesions, etc.), immunologic findings (Osler’s nodes, positive rheumatoid factor, etc.), and one positive blood culture. Diagnosis can be made using 1 major criterion plus 3 minor or with 5 minor criteria [5].

Self Quiz
Ask yourself...
- Which diagnostic tests are useful to diagnose endocarditis?
- How/by what criteria is endocarditis diagnosed?
- What are the two major criteria used to diagnose endocarditis?
- What are the minor criteria used to diagnose endocarditis?
Treatment
Once the diagnosis is made, treatment should be promptly initiated, and patients are typically admitted to the intensive care unit for close monitoring. Noninfective endocarditis typically entails treating the underlying disease and starting the patient on anticoagulants for clotting, like a heparin drip or oral warfarin [1]. The patient’s coagulating factors are typically ordered every 6 hours to achieve optimal anticoagulation. However, the interval for which these labs are ordered is determined by the provider and sometimes outlined by hospital protocols.
Infective endocarditis is treated with early IV antibiotics. Initial antimicrobial selection is dependent on patient risk factors, previous antibiotic use, and other factors. Empiric antibiotics may be routinely administered pending blood cultures, such as vancomycin and gentamycin, to cover for the most common bacterial pathologies. Penicillin G and ceftriaxone may also be used. For patients with a history of IV drug use, gentamicin and nafcillin are commonly administered to cover for methicillin-resistant Staph aureus (MRSA). Rifampin is commonly used in patients with prosthetic heart valves or intravascular devices. Antivirals may be initiated if this underlying etiology is suspected or confirmed with viral testing. Once the final blood cultures have resulted, revealing the underlying organism(s), IV antibiotics or other antimicrobials will be tailored according to the antibiogram [3, 5].
Intravenous antimicrobial treatment should be ordered for at least two weeks but is often up to eight weeks [2]. Nurses should anticipate peak and trough levels to be ordered for certain antibiotics, like vancomycin. They should also monitor the patient’s kidney function since antibiotics can cause renal complications.
The need for anticoagulation therapy for individuals with infective endocarditis remains controversial. If heart failure is present, medications to manage this may also be ordered, like diuretics and blood pressure management. Depending on the extent of heart valve involvement, sometimes heart surgery to repair or replace a valve is necessary [2, 5].
Care from a multidisciplinary team is warranted for patients with endocarditis, typically involving cardiology, infectious disease, cardiothoracic surgery, and other consultations depending on the body systems affected [5]. The nurse should anticipate these consultations, as well as repeat blood cultures and echocardiograms to be completed on the patient. They should closely monitor the patient’s vital signs, especially temperature and heart rate, indicating sepsis. They should also look for any signs or symptoms of potential complications.

Self Quiz
Ask yourself...
- What is the mainstay of treatment for noninfective endocarditis?
- What is the treatment for infective endocarditis?
- How does the treatment of noninfective versus infective endocarditis differ?
Potential Complications
Assessing patients for potential complications of endocarditis is necessary. Complications like pericarditis, myocardial infarction, congestive heart failure, and valvular insufficiency exist. Emboli, aneurysms, and infarcts may also develop as complications. Acute renal failure and glomerulonephritis are potential as well [3, 5]. Clinical signs and symptoms of these complications will vary, so close monitoring is needed. For congestive heart failure, the nurse and provider should monitor for signs of fluid overload, like leg swelling, diminished breath sounds, or pleural effusion on chest X-ray. A decrease in urine output or increases in BUN and creatinine may be early signs of renal impairment, glomerulonephritis, or kidney injury.

Patient Education
Patient education and monitoring are also key to the future prevention of endocarditis. Patients with a history of endocarditis should take preventative antibiotics prior to any dental, respiratory, genitourinary, or gastrointestinal procedures due to their increased risk for recurrence. Prevention guidelines vary and depend on which association or organization the provider is following. Prophylactic antibiotics are also prescribed to individuals with a prosthetic heart valve, cardiac valvopathy, or congenital heart disease. Additionally, if IV drug use was the initial cause of endocarditis, then patients should be instructed to stop using IV drugs [3, 5]. A referral for drug rehabilitation and counseling is useful for these patients. For patients with congenital heart defects, they should be closely followed by a pediatric cardiologist.
After the patient is discharged from the hospital, close monitoring and follow-up will be required. Some patients may require several weeks of continued IV antibiotics after discharge, during which they receive outpatient infusions. Other patients may be converted to oral antibiotics. Serial echocardiograms are also completed to monitor the patient’s heart function and valves. Sometimes, valve replacement is necessary several months after discharge. Close follow-up and collaboration between cardiology and infectious diseases are necessary [3, 5]. For patients with noninfective endocarditis or heart valve replacement, long-term anticoagulation may be necessary. They may be started on warfarin, where they will frequently need to have their INR checked to ensure therapeutic levels are reached [1].
Emerging Research
Endocarditis still remains a somewhat difficult diagnosis to make, especially for patients who meet minor criteria. A new antibiotic, dalbavancin, is being used to treat infectious endocarditis in some individuals. In 2023, the original Duke criteria for diagnosis of endocarditis was altered to now what’s called the modified Duke criteria, which is used for diagnosis and patient risk stratification. A definitive diagnosis of infectious endocarditis is made with 2 major OR either 1 major and 3 minor criteria. Possible endocarditis with 1 major OR 3 minor criteria. Additionally, studies have found value in ordering CT or PET imaging and TEE for diagnosis. There’s also been an increased prevalence of Enterococcus as a bacterial cause. PCR or other nucleic-based testing strategies, as well as IgM and IgG testing, are useful in aiding diagnosis when blood cultures are negative [4].

Self Quiz
Ask yourself...
- What are some potential complications of endocarditis?
- What elements of patient education are important?
- When are preventative antibiotics usually prescribed?
- What is some new, emerging research relevant to endocarditis?
Conclusion
The incidence of endocarditis is increasing due to various factors. Therefore, nurses and healthcare providers must be diligent and able to recognize the signs and symptoms of this condition, along with the importance of prompt intervention. A thorough history, including symptoms, medications, and physical exam, must be completed to help guide the possible diagnosis. Oftentimes, a congenital heart defect is the patient’s only predisposing factor, so close monitoring and follow-up are key. Patient education should be provided regarding this condition, as well as prevention strategies to avoid potential complications and future recurrence.
References + Disclaimer
- Armstrong, G.P. (2022, September). Noninfective Endocarditis. Merck Manual. https://www.merckmanuals.com/home/heart-and-blood-vessel-disorders/endocarditis/noninfective-endocarditis
- Armstrong, G.P. (2023, January). Infective Endocarditis. Merck Manual. https://www.merckmanuals.com/home/heart-and-blood-vessel-disorders/endocarditis/infective-endocarditis
- Brusch, J.L. (Updated 2024, April 18). Infective Endocarditis. Medscape. https://emedicine.medscape.com/article/216650-overview#a4
- Dale, S., Tayyem, Z. & Maceyko, S. Endocarditis: A Review of Recent Literature. Current Emergency Hospital Medicine Reports 12, 67–73 (2024). https://doi.org/10.1007/s40138-024-00292-9
- Gupta, A., & Mendez, M.D. (Updated 2023, July 17). Endocarditis. In StatPearls. StatPearls Publishing. https://www.ncbi.nlm.nih.gov/books/NBK499844/
- Martínez-Sellés, M., & Muñoz, P. (2023). Epidemiology, Diagnosis, Treatment, and Prognosis of Infective Endocarditis. Journal of clinical medicine, 12(17), 5705. https://doi.org/10.3390/jcm12175705
Disclaimer:
Use of Course Content. The courses provided by NCC are based on industry knowledge and input from professional nurses, experts, practitioners, and other individuals and institutions. The information presented in this course is intended solely for the use of healthcare professionals taking this course, for credit, from NCC. The information is designed to assist healthcare professionals, including nurses, in addressing issues associated with healthcare. The information provided in this course is general in nature and is not designed to address any specific situation. This publication in no way absolves facilities of their responsibility for the appropriate orientation of healthcare professionals. Hospitals or other organizations using this publication as a part of their own orientation processes should review the contents of this publication to ensure accuracy and compliance before using this publication. Knowledge, procedures or insight gained from the Student in the course of taking classes provided by NCC may be used at the Student’s discretion during their course of work or otherwise in a professional capacity. The Student understands and agrees that NCC shall not be held liable for any acts, errors, advice or omissions provided by the Student based on knowledge or advice acquired by NCC. The Student is solely responsible for his/her own actions, even if information and/or education was acquired from a NCC course pertaining to that action or actions. By clicking “complete” you are agreeing to these terms of use.
➁ Complete Survey
Give us your thoughts and feedback
➂ Click Complete
To receive your certificate
