Course
External Fixator Care and Considerations
Course Highlights
- In this External Fixator Care and Considerations
course, we will learn about the benefits and complications of external fixation. - You’ll also learn common complications of external fixators.
- You’ll leave this course with a broader understanding of the critical role of nursing care in the success of external fixation.
About
Contact Hours Awarded: 1
Course By:
R.E. Hengsterman MSN, RN
Begin Now
Read Course | Complete Survey | Claim Credit
➀ Read and Learn
The following course content
Introduction
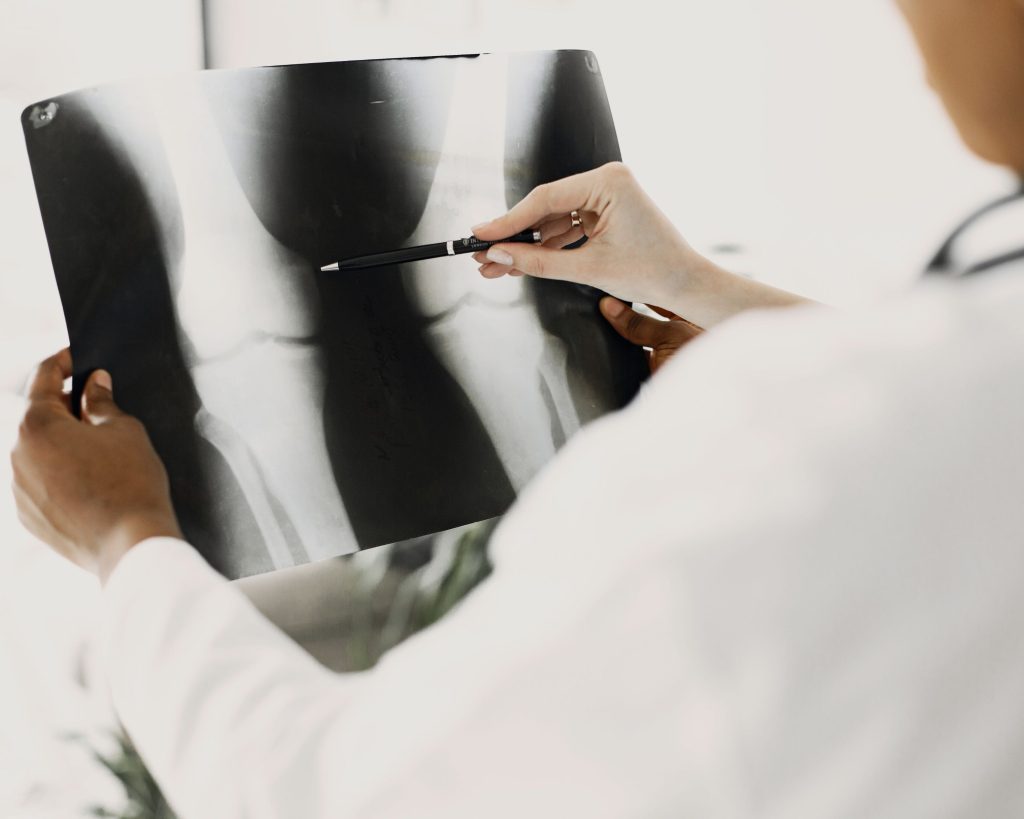
External fixators are orthopedic devices used to stabilize fractured or osteotomized bones and correct their position and orientation [1][36]. These devices consist of transosseous elements, such as pins or wires that pass through the bones, interconnected with a stabilizing structure outside the body [1][36]. Unlike open reduction and internal fixation, which aligns bone segments using attached pins and wires, external fixation methods allow realignment without surgically exposing the bones [36].
External fixation is a fundamental tool in traumatology and reconstructive orthopedic surgery. Its primary goal is to maintain the length, alignment, and rotation of the fracture [1]. For over 2000 years external fixation has treated fractures, first described by Hippocrates as a method to immobilize fractures while preserving soft tissue integrity [1]. Soviet doctor G.A. Ilizarov developed the Ilizarov System in 1951 in Kurgan, Siberia [2]. The ILIZAROV method lengthened and/or straightened bone and soft tissue, often saving limbs that might otherwise require amputation [2][3][17]. By separating the two bone halves millimeter by millimeter, the Ilizarov method leverages the body’s natural ability to regenerate bone, enabling the correction of deformities or the extension of bone length [2][3][33].
Nursing care plays a fundamental role in the successful implementation of external fixation. Nurses provide essential support to patients by educating them and their families about proper pin site care, infection prevention, and the management of external fixator devices [24]. They assist in monitoring the healing process, identifying potential complications, and ensuring adherence to treatment protocols. Through comprehensive patient education and continuous support, nurses help optimize outcomes and enhance the overall patient experience with external fixation.

Self Quiz
Ask yourself...
- How does the Ilizarov method utilize the body’s natural bone regeneration process to achieve limb lengthening and deformity correction, and what implications does this have for patient outcomes?
- In what ways does nursing care contribute to the successful implementation and management of external fixation, and how might this impact the overall patient experience and treatment outcomes?
Types & Construction
Different pin morphologies, such as self-drilling pins, trocar tip pins, and hydroxyapatite-coated pins, offer variations in performance and stability [1]. Enhancing the strength of the construct involves increasing the diameter of the rods or positioning them closer to the bone. External fixators include several subtypes, such as uniplanar, multiplanar, unilateral, bilateral, and circular fixators [1]. Multiplanar constructs, created by adding pins in different planes (perpendicular to each other), provide enhanced stability compared to uniplanar devices [1][4][13]. Bilateral frames, with pins on both sides of the bone, offer additional stability [1][5]. Circular fixators, used for limb lengthening procedures, are effective in allowing patients to bear weight and maintain some joint motion during treatment [1][5].
Hybrid frames, which combine elements of various constructs, offer flexibility in achieving the desired level of stability for optimal healing [1][6]. Carbon fiber is the preferred material for bars today, as it is 15% stiffer than stainless steel bars [8]. Balancing stability with a biological environment conducive to healing is crucial for successful outcomes. Hybrid external fixators combine unilateral or bilateral fixators with circular external fixators (CEFs). These devices utilize transosseous pins and tensioned wires, which attach to both circular and unilateral frame elements, providing structural support [36]. This combination facilitates multiplanar fixation, offering greater versatility than individual frame types. Hybrid external fixators provide the ability to stabilize complex fractures typical of CEFs, while also offering better access to soft tissue, similar to unilateral fixators [36].
Various adjustments to the external fixation construct can alter the stability of the fracture. The mode of fixation and the level of stability affect the physiology of fracture healing. Bone fracture healing is a complex and dynamic regenerative process aimed at restoring the damaged bone to its pre-injury state and cellular composition [12]. A fracture disrupts the structural continuity of the bone cortex and injures the surrounding soft tissues [11]. Following a fracture, secondary healing begins, consisting of four stages: hematoma formation, granulation tissue formation, bony callus formation, and bone remodeling [11][12].
Absolute fracture stability, achieved through methods like compression plating, leads to primary intramembranous bone healing [1][11]. In contrast, relative fracture stability, such as that provided by external fixation, results in secondary endochondral bone healing [11].
While external fixation stabilizes different bones across the body, the overall application technique remains the same.

Self Quiz
Ask yourself...
- How do different pin morphologies, such as self-drilling pins and hydroxyapatite-coated pins, impact the performance and stability of external fixation constructs, and what are the factors to consider when choosing a specific pin type for a patient?
- In what ways do multiplanar and bilateral external fixator constructs provide enhanced stability compared to uniplanar devices, and how does this influence the treatment and healing process of fractures?
- Why is it important for surgeons to balance the stiffness of external fixation constructs with a biological environment conducive to healing, and what might be the consequences of using a construct that is too stiff?
- How does the mode of fixation and the level of stability in external fixation affect the physiology of fracture healing, and what are the differences between primary intramembranous bone healing and secondary endochondral bone healing in this context?
Benefits
External fixation offers numerous benefits compared to internal plates and intramedullary nails [13]. One of the primary advantages is that external fixators cause less disruption to the soft tissues, osseous blood supply, and periosteum [13][16]. This characteristic makes fixators suitable for managing soft tissue in acute trauma with skin contusions and open wounds, in chronic trauma with thin skin grafts and muscle flaps, and in patients with compromised healing potential due to conditions like rheumatoid disease, peripheral vascular disease, diabetes mellitus, and Charcot disease [14][15].
The temporary nature of the pins and wires in external fixators is ideal for providing bony stability in cases of osteomyelitis, where internal implants can complicate infection eradication [17]. The ability to avoid placing fixation in the infected area is another significant benefit. As fixed-angle devices, external fixators offer superior fixation in compromised bone, and the use of fixed-angle pins in multiple planes provides the versatility needed to optimize stability while minimizing tissue damage [13]. Many external fixators offer excellent stability, allowing for early weight-bearing and joint motion exercises [35].

Self Quiz
Ask yourself...
- How does the reduced disruption to soft tissues, osseous blood supply, and periosteum by external fixators make them particularly suitable for managing several types of trauma and patients with compromised healing potential?
- In what ways do the temporary nature of pins and wires in external fixators and the ability to avoid placing fixation in infected areas contribute to the effective management of osteomyelitis and other infection-related complications?
Complications
External fixation treatment can lead to several complications, including pin site infection, osteomyelitis, and the failure or loosening of the frame or pins/wires, placing a significant burden on both the patient and the healthcare system [22]. Patients can often differentiate between various pin site conditions by comparing the severity of inflammatory symptoms and identifying specific symptoms that are indicative of infection [30]. An irritated pin site may be due to a different pathological process, such as contact dermatitis, rather than an infection [30].
Additional complications include malunion or non-union of the fracture, soft-tissue impalement, neurovascular injury, compartment syndrome, and refracture around the pin site [18]. There is a risk of soft-tissue impalement, neurovascular injury, and compartment syndrome [18]. Each of these complications requires careful monitoring and management to ensure optimal patient outcomes.
A recent prospective study involving 39 patients with trauma, limb deformity, and bone infection treated with external fixation reported a pin site infection rate of 30%, affecting 92.5% of the patients. Although most pin site infections are superficial, this complication often causes patient pain and necessitates increased pin site care or antibiotic treatment [20]. These infections progress through four stages: Stage I involves seropurulent drainage, Stage II includes superficial cellulitis, Stage III entails deep infection, and Stage IV results in osteomyelitis [19] [21]. These infections increase the number of clinic visits required during a patient’s course of treatment, may necessitate additional interventions such as antibiotics and surgery, and can compromise patient outcomes if osteomyelitis or instability results from pin loosening or the need for pin or complete construct removal [18]. Factors influencing the development of pin site infections include patient-specific risk factors, surgical technique, pin design characteristics, use of prophylactic antibiotics, and the post-operative pin care protocol, which encompasses cleansing, dressing changes, and showering [18]. The use of antiseptics may not provide any significant benefit for routine pin site care in Ilizarov external fixation. Furthermore, daily pin site care is not superior to weekly pin site care. For early and low-grade pin site infections, empirical therapy should focus on Staphylococcus [32].
Factors associated with an increased risk of pin site infection include multiple comorbidities, poor soft tissue structure, inadequate general hygiene, and poor nutritional status. Systemic conditions such as diabetes and immunodeficiency also elevate the risk of infection [23]. Most pin site infections are treatable with improved wound care and a short course of oral antibiotics. However, deep tissue infections and osteomyelitis may occur in up to 4% of cases, which are serious complications [22]. Pin loosening can lead to increased pain, greater use of pain medications, and delayed mobilization [22].
Due to the high incidence of pin site infections in patients undergoing external fixation and the morbidity and costs associated with the sequelae, clinicians need to educate patients to recognize the signs and symptoms of pin site infections to initiate treatment.

Self Quiz
Ask yourself...
- How can patients differentiate between various pin site conditions, such as infections and other pathological processes like contact dermatitis, and why is this distinction important for their treatment and care?
- What are the potential complications associated with external fixation, such as malunion or non-union of fractures, and how can careful monitoring and management mitigate these risks?
- Considering the stages of pin site infections and the factors influencing their development, how can healthcare professionals tailor their care protocols to prevent and effectively manage these infections?
- How do systemic conditions like diabetes and immunodeficiency increase the risk of pin site infections, and what strategies can minimize these risks and ensure optimal patient outcomes?
Nursing Considerations
The role of the orthopedic nurse encompasses identifying patients’ concerns and addressing their expectations about care. The nurse provides expert support to patients during periods of change and adjustment, helping to reduce the risk of non-acceptance of the frame and non-adherence to treatment. When planning discharge from the hospital, it is important for nurses to address factors such as depression and destructive behavior [24].
External fixation comes with several complications impacting patients’ lives and relationships. Nurses are responsible for developing educational plans that teach patients and their relatives about pin-site care, thereby enabling effective self-care of external fixation systems [24]. Maladaptive coping leads to depression, anxiety, and poorer psychological and social well-being [34]. Patients who struggle post-discharge may benefit from additional community support and more frequent follow-up. Self-management programs can aid in developing effective coping strategies [25].
Nurses play a crucial role in supporting patients with external fixator devices and in caring for pin sites. Clear and consistent assessment and documentation enable nurses to monitor the condition of pin sites and distinguish between new and recurrent pin site infections. Patients often notice subtle changes in symptoms first, making their perceptions of potential infections a key part of the assessment.
By providing both verbal and written information, nurses help patients understand the importance of proper pin site care and early infection detection. Patients with external fixator devices should undergo regular review by the orthopedic team to assess healing progress and check the position and stability of the frame [19]. Depending on the device, adjustments such as tightening elements or changing struts may be necessary. The orthopedic team and nurse can provide patient-specific advice on managing the device throughout the treatment period. Regular reviews of pin sites are essential to check for signs of inflammation, irritation, infection, or pin loosening. Assessment of pin sites and surrounding tissue can be subjective and vary between clinicians [19].
By involving patients in care planning and evaluation, the nurse can foster a holistic, patient-centered approach, ensuring individualized care. Involving the multidisciplinary team in both acute and community settings equips patients with the skills and resources for effective self-care.

Self Quiz
Ask yourself...
- How can orthopedic nurses identify and address patients’ concerns and expectations about external fixation care, and what impact does this have on treatment adherence and patient outcomes?
- In what ways can developing comprehensive educational plans for patients and their relatives about pin-site care and infection prevention enhance self-care and improve overall patient well-being during and after treatment with external fixators?
- How does the involvement of a multidisciplinary team in both acute and community settings contribute to a holistic, patient-centered approach in managing external fixation, and what are the benefits of regular reviews and assessments by healthcare professionals?
Patient and Family Education
Pin site care is essential for reducing infection rates, though techniques vary, and no universal protocol exists to completely eliminate the risk of pin site infections. In recovery, pins may use xeroform or iodine-impregnated gauze [26]. The use of compressive garments under the external fixator bars can help reduce motion around the skin-pin junction [26]. If skin drainage or erythema occurs, perform pin care three times a day until the infection clears [1]. To clean pin sites, recommend using chlorhexidine in an alcohol solution, except for patients with a known sensitivity to chlorhexidine or pre-existing skin conditions like eczema [27]. Use caution with chlorhexidine due to its potential to cause hypersensitivity, generalized allergic reactions, and anaphylaxis [28]. If irritation or allergy occurs, suggest using sterile saline [28].
Pin Site Care
Comprehensive guide to cleaning and caring for pin sites [29]:
- Wash Your Hands: Use soap and water.
- Prepare Cleaning Supplies: Gather your supplies
- A cleaning solution prescribed by your doctor
- Cups to hold the cleaning solution
- Cotton swabs
- Cotton gauze
- Wash Your Hands Again: Ensure cleanliness by washing your hands a second time before touching the pin sites.
- Massage the Pin Area: Massage the skin around the pin to detach any adhered skin and bring any fluid to the surface for easier cleaning.
- Clean Each Pin Site:
- Use a new cotton swab for each pin site.
- Dip the swab in the cleaning solution.
- Clean around the pin site in a circular motion, moving away from the pin. Use fresh swabs until the site is thoroughly clean.
- Dry the area with a new, clean swab.
- Clean the Pins:
- Dip a swab or piece of gauze in the cleaning solution.
- Clean the pin itself, paying special attention to any threaded areas. For each pin, ensure to use a fresh swab or a new piece of gauze
- Wrap the Pin Sites: Loosely wrap gauze around each pin site for the first few days.
- Clean the Fixator and Wires: For those with an external fixator, clean both the fixator and any connecting wires with gauze or cotton swabs dipped in the cleaning solution.
Recognizing Signs of Pin Site Infection
- Tenderness: Increased tenderness around the pin site that was not tender prior to the current assessment is often the first sign of infection.
- Redness: Redness in the area compared to other areas; be careful not to confuse infection redness with the red or purple color from scar formation.
- Warmth: Increased warmth in the affected area compared to other areas.
- Swelling: Swelling that may feel hard or fluid-like.
- Drainage: Varying characteristics such as consistency, color, and smell. Note that amber or tea-colored drainage in lesser amounts is normal.
- Odor: A noticeable odor indicates that the infection has progressed.
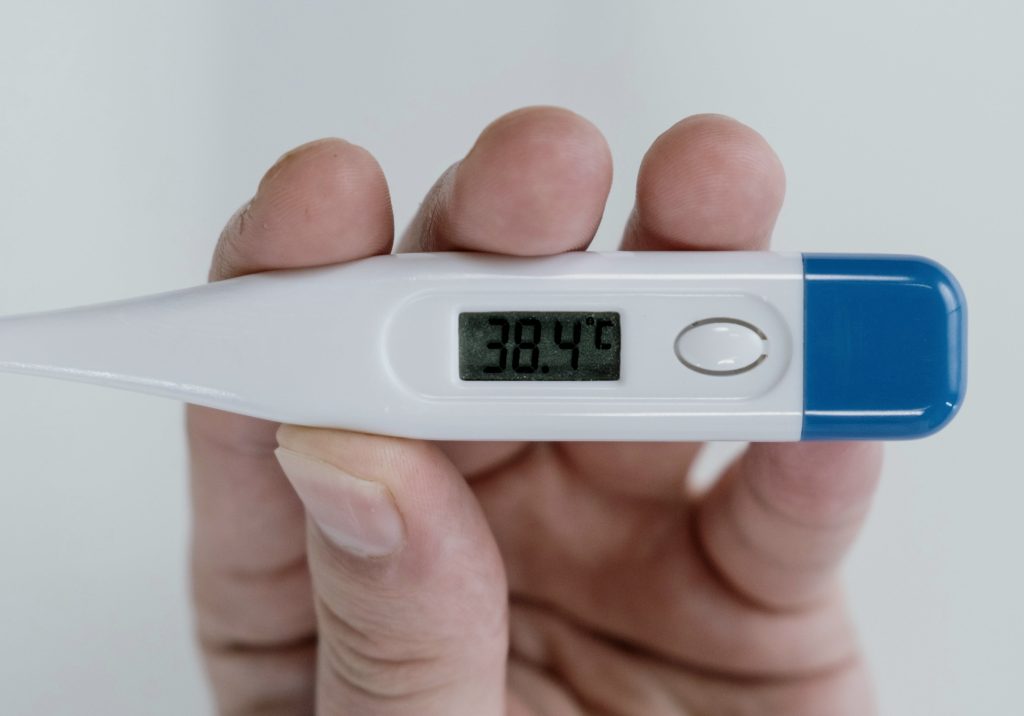
- Temperature: A fever of 101 degrees or greater taken by mouth or under the arm. Avoid taking your temperature within two hours of physical therapy. It is possible to have a pin site infection without an accompanying fever.

Self Quiz
Ask yourself...
- How can educating patients and their families about proper pin site care and infection prevention techniques, despite the lack of a universal protocol, help reduce the risk of complications and improve recovery outcomes?
- In what ways might the use of different cleaning solutions, such as chlorhexidine or sterile saline, impact the effectiveness of pin site care and the incidence of allergic reactions or sensitivities in patients with external fixators?
- How does recognizing early signs of pin site infection, such as increased tenderness or changes in drainage, contribute to timely intervention and better patient outcomes, and what role does patient education play in this process?
- What are the primary benefits and potential complications of using external fixation in orthopedic surgery, and how can comprehensive patient education and multidisciplinary care approaches help mitigate these risks and enhance patient outcomes?
- What role do nurses play in mitigating the complications associated with external fixation, such as pin site infections and neurovascular injury, through patient education and regular monitoring, and how does this contribute to better recovery outcomes and reduced healthcare system burdens?
Conclusion
External fixation is a pivotal tool in orthopedic surgery, used for over 2000 years to treat fractures while preserving soft tissue integrity [1]. The ILIZAROV method, introduced to the West in 1981, has advanced the field by enabling bone lengthening and deformity correction through the body’s natural bone regeneration process [1]. Despite its numerous benefits, such as minimal soft tissue disruption and suitability for patients with compromised healing potential, external fixation presents several complications. These include pin site infections, osteomyelitis, frame, or pin loosening, malunion, and non-union of fractures, as well as risks of soft-tissue impalement, neurovascular injury, compartment syndrome, and refracture around pin sites [18] [22][30]. Effective pin site care and patient education are key in mitigating these risks and ensuring optimal outcomes.
Nurses play a critical role in supporting patients with external fixator devices and in managing pin sites. They provide essential education to patients and their families about proper pin site care, recognizing infection signs, and promoting self-care [31]. Regular reviews by the orthopedic team and nurses are necessary to assess healing progress and adjust the fixation devices as needed. By involving patients in care planning and utilizing a multidisciplinary approach, nurses ensure individualized, holistic care. Understanding the importance of proper pin site care and early infection detection helps patients achieve better recovery outcomes and reduces the overall burden on the healthcare system.
References + Disclaimer
- Hadeed, A., Werntz, R. L., & Varacallo, M. (2023, August 4). External Fixation Principles and Overview. StatPearls – NCBI Bookshelf. https://www.ncbi.nlm.nih.gov/books/NBK547694/
- Gubin, A. V., Borzunov, D. Y., Marchenkova, L. O., Malkova, T. A., & Smirnova, I. L. (2016). Contribution of G.A. Ilizarov to bone reconstruction: historical achievements and state of the art. Strategies in Trauma and Limb Reconstruction/Strategies in Trauma and Limb Reconstruction, 11(3), 145–152. https://doi.org/10.1007/s11751-016-0261-7
- Jiang, Q., Huang, K., Liu, Y., & Chi, G. (2020). Using the Ilizarov technique to treat limb shortening after replantation of a severed lower limb: a case report. Annals of Translational Medicine, 8(16), 1025. https://doi.org/10.21037/atm-20-5316
- Handbook of Orthopaedic Trauma Implantology. (2020). SpringerLink. https://link.springer.com/referencework/10.1007/978-981-15-6278-5
- Bafor, A., & Iobst, C. A. (2022). What’s new in limb lengthening and deformity correction. Journal of Bone and Joint Surgery. American Volume The Journal of Bone and Joint Surgery. American Volume, 104(16), 1419–1425. https://doi.org/10.2106/jbjs.22.00398
- Antezana, P. E., Municoy, S., Álvarez-Echazú, M. I., Santo-Orihuela, P. L., Catalano, P. N., Al-Tel, T. H., Kadumudi, F. B., Dolatshahi-Pirouz, A., Orive, G., & Desimone, M. F. (2022). The 3D bioprinted scaffolds for wound healing. Pharmaceutics, 14(2), 464. https://doi.org/10.3390/pharmaceutics14020464
- View of a review and comparison of hexapod external fixators | Journal of the Pediatric Orthopaedic Society of North America. (2023). https://jposna.org/index.php/jposna/article/view/627/704
- Fernando, P., Abeygunawardane, A., Wijesinghe, P., Dharmaratne, P., & Silva, P. (2021). An engineering review of external fixators. Medical Engineering & Physics, 98, 91–103. https://doi.org/10.1016/j.medengphy.2021.11.002
- Wahab, A. H. A., Wui, N. B., Kadir, M. R. A., & Ramlee, M. H. (2020). Biomechanical evaluation of three different configurations of external fixators for treating distal third tibia fracture: Finite element analysis in axial, bending and torsion load. Computers in Biology and Medicine, 127, 104062. https://doi.org/10.1016/j.compbiomed.2020.104062
- O’Connor, H. A., Adams, L. W., MacFadden, L. N., & Skelley, N. W. (2023). 3D Printed Orthopaedic External Fixation Devices: A Systematic review. 3D Printing in Medicine, 9(1). https://doi.org/10.1186/s41205-023-00180-0
- Sheen, J. R., Mabrouk, A., & Garla, V. V. (2023, April 8). Fracture Healing Overview. StatPearls – NCBI Bookshelf. https://www.ncbi.nlm.nih.gov/books/NBK551678/
- Duan, Z., & Lu, H. (2021). Effect of mechanical strain on cells involved in fracture healing. Orthopaedic Surgery, 13(2), 369–375. https://doi.org/10.1111/os.12885
- Kwan, Y. H., Decruz, J., Premchand, A. X., & Khan, S. A. (2022). Complex distal tibia fractures treated with multi-planar external fixation – a single center experience. PubMed Central (PMC). https://www.ncbi.nlm.nih.gov/pmc/articles/PMC9301155/
- Fragomen, A. T., & Rozbruch, S. R. (2006). The mechanics of external fixation. HSS Journal, 3(1), 13–29. https://doi.org/10.1007/s11420-006-9025-0
- Yammine, K., & Assi, C. (2019). Intramedullary nail versus external fixator for ankle arthrodesis in Charcot neuroarthropathy: A meta-analysis of comparative studies. Journal of Orthopaedic Surgery, 27(2), 230949901983601. https://doi.org/10.1177/2309499019836012
- Fernando, P., Abeygunawardane, A., Wijesinghe, P., Dharmaratne, P., & Silva, P. (2021). An engineering review of external fixators. Medical Engineering & Physics, 98, 91–103. https://doi.org/10.1016/j.medengphy.2021.11.002
- Bliven, E. K., Greinwald, M., Hackl, S., & Augat, P. (2019). External fixation of the lower extremities: Biomechanical perspective and recent innovations. Injury, 50, S10–S17. https://doi.org/10.1016/j.injury.2019.03.041
- Kold, S., Fridberg, M., Bue, M., & Rölfing, J. (2022). Host factors and risk of pin site infection in external fixation: A systematic review examining age, body mass index, smoking, and comorbidities including diabetes. Journal of Limb Lengthening & Reconstruction, 8(3), 3. https://doi.org/10.4103/jllr.jllr_32_21
- Bue, M., Bjarnason, A. Ó., Rölfing, J. D., Larsen, K., & Petruskevicius, J. (2021). Prospective evaluation of pin site infections in 39 patients treated with external ring fixation. Journal of Bone and Joint Infection, 6(5), 135–140. https://doi.org/10.5194/jbji-6-135-2021
- Momodu, I. I., & Savaliya, V. (2023, May 31). Osteomyelitis. StatPearls – NCBI Bookshelf. https://www.ncbi.nlm.nih.gov/books/NBK532250/
- Rozbruch, S. R., Kazmers, N. H., & Fragomen, A. T. (2016). Prevention of pin site infection in external fixation: a review of the literature. Strategies in Trauma and Limb Reconstruction/Strategies in Trauma and Limb Reconstruction, 11(2), 75–85. https://doi.org/10.1007/s11751-016-0256-4
- Liu, K., Abulaiti, A., Liu, Y., Cai, F., Ren, P., & Yusufu, A. (2021). Risk factors of pin tract infection during bone transport using unilateral external fixator in the treatment of bone defects. BMC Surgery, 21(1). https://doi.org/10.1186/s12893-021-01384-z
- Xing, J., Sun, N., Li, L., Lv, D., Geng, S., & Li, Y. (2020). Factors influencing self-care in outpatients with external fixation in China. Journal of International Medical Research, 48(2), 030006052090260. https://doi.org/10.1177/0300060520902603
- Faculty of Medical Sciences, Tetova. (2). (2023) NURSING CARE IN PATIENTS WITH EXTERNAL FIXATION – Universiteti i Tetoves. http://eprints.unite.edu.mk/id/eprint/1204
- Heidari, N., Shields, D. W., Iliadis, A., Kelly, E., & Jamal, B. (2022). Pin-site infection: A Systematic Review of Prevention Strategies. Strategies in Trauma and Limb Reconstruction/Strategies in Trauma and Limb Reconstruction, 17(2), 93–104. https://doi.org/10.5005/jp-journals-10080-1562
- Hasegawa, T., Tashiro, S., Mihara, T., Kon, J., Sakurai, K., Tanaka, Y., Morita, T., Enoki, Y., Taguchi, K., Matsumoto, K., Nakajima, K., & Takesue, Y. (2022). Efficacy of surgical skin preparation with chlorhexidine in alcohol according to the concentration required to prevent surgical site infection: meta-analysis. BJS Open, 6(5). https://doi.org/10.1093/bjsopen/zrac111
- Opstrup, M. S., & Garvey, L. H. (2019). Chlorhexidine allergy: Mild allergic reactions can precede anaphylaxis in the healthcare setting. Turkish Journal of Anaesthesiology and Reanimation, 47(4), 342–344. https://doi.org/10.5152/tjar.2019.22058
- Pin care: MedlinePlus Medical Encyclopedia. (2022). https://medlineplus.gov/ency/patientinstructions/000481.htm
- Santy-Tomlinson, J., Jomeen, J., & Ersser, S. J. (2019). Patient-reported symptoms of ‘calm’ ‘irritated’ and ‘infected’ skeletal external fixator pin site wound states; a cross-sectional study. International Journal of Orthopaedic and Trauma Nursing, 33, 44–51. https://doi.org/10.1016/j.ijotn.2019.01.002
- Campbell, F., & Watt, E. (2020). An exploration of nursing practices related to care of orthopaedic external fixators (pin/wire sites) in the Australian context. International Journal of Orthopaedic and Trauma Nursing, 36, 100711. https://doi.org/10.1016/j.ijotn.2019.100711
- Subramanyam, K. N., Mundargi, A. V., Potarlanka, R., & Khanchandani, P. (2019). No role for antiseptics in routine pin site care in Ilizarov fixators: A randomised prospective single blinded control study. Injury, 50(3), 770–776. https://doi.org/10.1016/j.injury.2019.01.031
- Malkova, T. A., & Borzunov, D. Y. (2021). International recognition of the Ilizarov bone reconstruction techniques: Current practice and research (dedicated to 100thbirthday of G. A. Ilizarov). World Journal of Orthopedics, 12(8), 515–533. https://doi.org/10.5312/wjo.v12.i8.515
- Balikji, J., Hoogbergen, M. M., Garssen, J., & Verster, J. C. (2022). Mental Resilience, Mood, and Quality of Life in Young Adults with Self-Reported Impaired Wound Healing. International Journal of Environmental Research and Public Health/International Journal of Environmental Research and Public Health, 19(5), 2542. https://doi.org/10.3390/ijerph19052542
- The Mechanics of External Fixation | HSS Journal – Springer, https://link.springer.com/article/10.1007/s11420-006-9025-0.
- Widanage, K. N., De Silva, M. J., Lalitharatne, T. D., Bull, A. M., & Gopura, R. (2023). Developments in circular external fixators: A review. Injury, 54(12), 111157. https://doi.org/10.1016/j.injury.2023.111157
Disclaimer:
Use of Course Content. The courses provided by NCC are based on industry knowledge and input from professional nurses, experts, practitioners, and other individuals and institutions. The information presented in this course is intended solely for the use of healthcare professionals taking this course, for credit, from NCC. The information is designed to assist healthcare professionals, including nurses, in addressing issues associated with healthcare. The information provided in this course is general in nature and is not designed to address any specific situation. This publication in no way absolves facilities of their responsibility for the appropriate orientation of healthcare professionals. Hospitals or other organizations using this publication as a part of their own orientation processes should review the contents of this publication to ensure accuracy and compliance before using this publication. Knowledge, procedures or insight gained from the Student in the course of taking classes provided by NCC may be used at the Student’s discretion during their course of work or otherwise in a professional capacity. The Student understands and agrees that NCC shall not be held liable for any acts, errors, advice or omissions provided by the Student based on knowledge or advice acquired by NCC. The Student is solely responsible for his/her own actions, even if information and/or education was acquired from a NCC course pertaining to that action or actions. By clicking “complete” you are agreeing to these terms of use.
➁ Complete Survey
Give us your thoughts and feedback
➂ Click the Green MARK COMPLETE Button Below
To receive your certificate
