Course
Factitious Disorder Imposed on Another (FDIA)
Course Highlights
- In this Factitious Disorder Imposed on Another (FDIA) course, we will learn about the defining components of Factitious Disorder Imposed on Another.
- You’ll also learn etiology and behavioral signs and symptoms of both the abuser and victim of Factitious Disorder Imposed on Another.
- You’ll leave this course with a broader understanding of treatment plans and resources available to clinicians to apply in cases of Factitious Disorder Imposed on Another.
About
Contact Hours Awarded: 1
Course By:
Abbie Schmitt, MSN, RN
Begin Now
Read Course | Complete Survey | Claim Credit
➀ Read and Learn
The following course content
Introduction
As nurses strive to become advocates for their patients, we must collect data in unique, puzzling situations. Diagnosing Factitious Disorder Imposed on Another (FDIA) is not a simple task and not within the scope of nursing practice. However, nurses have a unique responsibility to gather data, critically question inconsistent results, apply knowledge on this mental disorder, and advocate for their patients. We will apply these concepts in an unfolding, progressive case study where puzzle pieces are placed together to explain the larger concept. The puzzle pieces that lead to understanding FDIA include the definition of this disorder, statistical evidence, demographics, etiology, and signs and symptoms. Nurses should beware of warning signs and feel confident in reporting and safety measures. Treatments and resources are available for these patients and those impacted by FDIA.
Definition
As we define FDIA, we need to break it down and define: (1) factitious disorder and (2) when it is imposed on someone else.
Factitious Disorder (FD)
Factitious disorder describes a behavior that occurs when a person falsifies physical or psychological signs or symptoms or takes a step further to induce injury or disease (1). Essentially, these patients either pretend to have signs or symptoms or they can actually cause injury to produce these symptoms. FD is when the deceptive behavior typically does not have an obvious reward and cannot be explained by another mental disorder, such as delusional psychosis (1). If an obvious financial or other incentive is present, FD is not an appropriate diagnosis. FD may happen in one or more brief episodes, but it is typically a chronic, lifelong pattern (1).
Factitious Disorder (FD) has historically been known as Munchausen syndrome and Factitious Disorder Inflicted on Another (FDIA) often called Munchausen syndrome by proxy (MSbP). The new title and definition were created because it describes a behavioral pattern rather than an underlying psychiatric syndrome (4). The clinical description of FD is found in the Diagnostic and Statistical Manual of Mental Disorders, Fifth Edition (DSM-5), and is listed as a recognized mental illness (1).
Defining Factitious Disorder Imposed on Another (FDIA)
FDIA is defined as deception created by falsification of medical or psychological signs and symptoms in others; including dishonest reporting of illness or actually inducing injury or disease in another and presenting the person to others as if they are actually ill or impaired (1). This deceptive behavior is missing an obvious external reward.
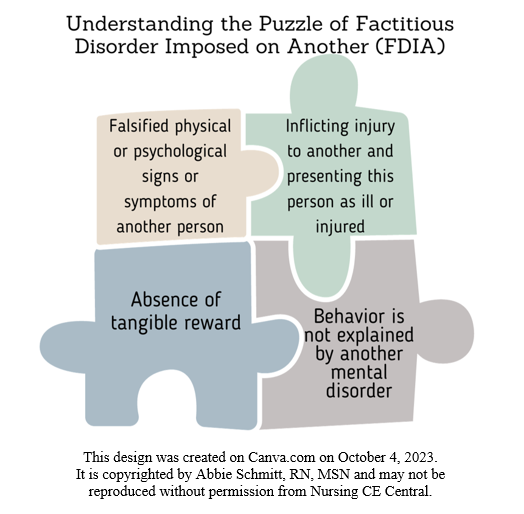
FDIA is listed in the DSM-V beneath the umbrella of somatic symptom and related disorders. Concepts to consider in diagnosing FDIA (1):
- Falsified physical or psychological signs or symptoms in another person.
- Inflicting injury or disease in another, and misrepresenting this as ill, impaired, or injured.
- Deceptive behavior is present even in the absence of external rewards.
- The behavior is not explained by another mental disorder.
Statistical Evidence
The prevalence of FDIA in the US is largely unknown. Researchers contribute this difficulty in detection to the deceptive nature of FDIA and the hesitancy of medical providers to report (6). The American Academy of Pediatrics estimate that 0.5 to 2.0 per 100,000 children younger than 16 will become a victim of FDIA (4). This is not a condition unique to the United States. This behavior has been reported in over 50 countries (4). There are very common trends found among researcher studies. FDIA is more common in women and more than 95% of perpetrators are the mother of the victim (8). Researchers estimate the mortality rate of victims of FDIA is 6-10% (6). Personality disorders are commonly seen in the perpetrators, and up to 70% of women who engage in illness falsification of their children also report unsubstantiated somatic symptoms themselves (4). Literature review reveals that poisoning and suffocation are the most common forms of harm (8). There is an estimated 600 cases of suffocation and non-accidental poisoning linked to FDIA in the US every year (6).

Self Quiz
Ask yourself...
- Have you ever cared for a patient that falsely reported symptoms?
- Can you think of mental disorders that may impact a patient’s perception of their health status? (ex: hallucinations, etc.)
- Can you think of reasons why it would be difficult for one single provider, without prior history of treating the patient or medical records, to detect falsification of an illness in someone else?
Demographics
Demographic information can vary, but several literature reviews have been conducted over the past few decades and reveal important trends. One of the most meaningful research studies on FDIA was conducted by Gregory Yates and Christopher Bass in 2017, when they did a systematic review of 796 cases and translated this into demographic and clinical characteristics (8).
Demographic trends for those labeled with FDIA: (8)
- Majority is female
- They are typically the victim’s mother
- Married
- Mean caretaker age at the child’s presentation was 27.6 years
- Healthcare-related professionals
- Reported to have pregnancy or post-term complications
- History of childhood abuse or neglect
- Personality disorder (especially histrionic and borderline types) is common
Victim Demographics:
- Commonly in younger children (range of 1 month – 21 years) (3)
- Elderly or disabled individuals
- Males and females are seen at comparable rates

Self Quiz
Ask yourself...
- Can you name the common demographics of FDIA abusers?
- Have you ever cared for a patient with a diagnosed personality disorder?
Etiology
The etiology of FDIA is not clearly known, but we will review some of the biological and psychological factors that researchers suggest play a role in the development of this disorder. Even when seen in long-term treatment, patients diagnosed with FDIA are resistant to discussing or comprehending their motivations (2). Possible motivations, both conscious and unconscious, include a desire for attention or heroic deeds, dependency needs, maladaptive reactions to loss or separation, or the pleasure of deceiving others (3).
There is a correlation between the onset of the behavior of FDIA and an initial hospitalization of the individual’s child or other dependent for legitimate reasons. (8). Essentially, this individual may have enjoyed the experience of the first legitimate illness and felt a need to recreate it.
Learned Coping Mechanism. Interviews with patients who willingly seek treatment for FDIA often report a childhood history of parental illness, death, or abandonment, or personal illness or institutionalization (6). As a result of these childhood experiences, dishonest reporting of illness may be viewed as a learned coping mechanism. For example, if this mother remembers the only affection received from her own mother or father was during an illness, the state of being ill can be positive in their own experience.
Cerebral Dysfunction. The possible role of cerebral dysfunction for at least some patients has been proposed. Research found these patients commonly had deficits in conceptual organization. Essentially, there may be abnormalities within the nervous system physiology. Abnormal findings on brain imaging have also been reported (6). Brain dysfunction has been reported in approximately 20%–25% of persons with pseudologia fantastica and/or FDIA (6).

Self Quiz
Ask yourself...
- Can you think of examples of unhealthy coping mechanisms, such as alcohol abuse or aggressive behavior?
- Can you think of positive, healthy coping mechanisms, such as exercise or deep breathing?
Signs and Symptoms
Unlike conditions like hypertension or diabetes, this disorder does not have a specific lab or single abnormal clinical finding. The healthcare team must rely on behavior and reporting that is not consistent with the diagnostic testing. As the nurse, you are looking for bizarre and unexpected findings. For example, the caregiver of a patient reports a rash, but it appears like a scrape or wound inflicted with a sharp surface. The presentation can be characterized by disease imitation, pathological lying, and frequent wanderings (2).
Research found the following trends among those with FDIA: (3)
- Demonstrate a remarkable knowledge of medical information (disease process, etiology, diagnostic testing)
- Reports extensive travelling or relocations, explaining multiple hospitals
- Description of illness in chronic, ongoing terms
- Present to locations “outside of typical hours” or during weekends when less experienced doctors are on duty
- Demands for medication
- Insists on absence of visitors
- Difficult to establish rapport
- Presentation: restless, evasive, histrionic, and attention seeking
- Intelligence ranges from learning disability range to superior
- Physical signs such as scars and fever; males often antisocial, females histrionic
- Possible associated factors: criminal records; pseudologia fantastica
- Typically lacks referral letters from physicians
- Reluctant to give consent to obtain previous medical records
Common signs and symptoms of victims: (3)
- Hypoglycemia
- Chest pain
- Skin lesions
The following disorders were reported or imposed on the victims in a review of FDIA case studies: epilepsy, otitis, bacteremia, fever, poisoning, suffocation, apnea, sudden infant death, developmental disability, impaired hearing, cystic fibrosis, airway obstruction, hemophilia, psychiatric disorder, cardiac disease, menorrhagia, hematuria, and esophageal perforation (3).

Self Quiz
Ask yourself...
- Have you ever experienced extremely unexpected laboratory results while caring for a patient?
- Can you describe common behavior patterns of FDIA?
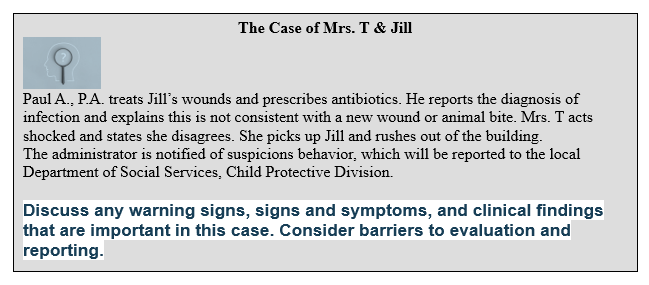
Warning Signs
Providers should be aware of warning signs that are common to FD. Each warning sign cannot be used alone, but similar to a puzzle, the warning signs together should ring a loud alarm. The warning signs generally include the involvement of multiple medical providers, recurrent hospitalizations, inconsistencies between reported condition and clinical findings, and symptoms that dramatically worsen or shift when the caregiver is present (6). According to the American Professional Society on the Abuse of Children (APSAC), here are some other common signs FDIA to watch out for: (1)
- Discrepancy between the caregiver’s reports of individual’s medical history and the physical medical record.
- Extensive medical assessments do not identify a medical explanation for the child’s reported problems.
- Laboratory findings that are clinically impossible or implausible or identify chemicals, medications, or contaminants that should not be present.
- Child’s symptoms resolve or improve when separated from the caregiver.
- Other individuals in the home report unusual or unexplained illnesses or conditions.
- Sometimes one child has resolved symptoms and shortly later another child becomes ill.
- Caregiver is reluctant to provide medical records, claims that past records are not available, or refuses to allow medical providers to discuss care with previous medical providers.
- Caregiver isolates patient from other parent or family.
- Family members, neighbors, and teachers express concern about ongoing illnesses, rare conditions, or overuse of medical providers.

Self Quiz
Ask yourself...
- Are you familiar with lab results that reveal various medications?
- Would it be a warning sign if a caregiver refuses to provide consent to obtain medical records?
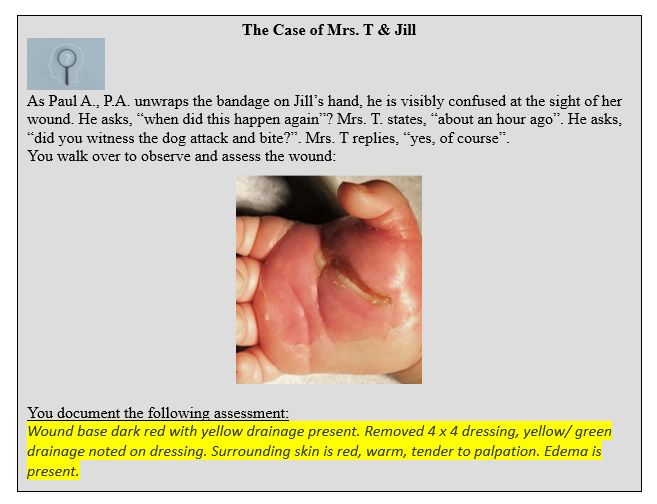
- For the case study: are there assessment findings for the wound that are inconsistent with a new wound?
Pediatric Considerations
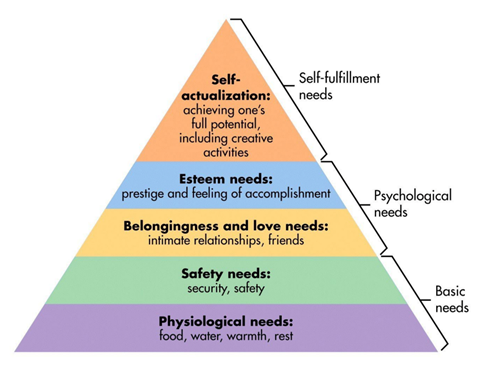
The pediatric population has a unique dependency on others to meet their needs. Prioritization of their needs is essential. Children rely on adults in their lives to provide for their physiological needs and to ensure their safety. Maslow’s hierarchy of needs is a motivational theory used in psychology that applies a five-tier model of human needs (7). Healthcare professionals can use this when prioritizing care.
Reporting
Once the medical team has gathered evidence that supports the claim of FDIA, including medical records and statements, and a mental health professional determines all four criteria are met, the administrators should report it to the state child protective services agency and law enforcement (3). If the suspected abuser removes the child from care before adequate evaluation can be done and the caregiver refuses to communicate or cooperate, the suspicions should still be reported so it can be evaluated. Medical child abuse should be reported in the same way as physical and sexual child abuse.
How does HIPAA impact reporting of FDIA? Nurses should be very knowledgeable on HIPAA guidelines, especially when providing medical information of their patients to others. The safety of the pediatric patient is priority. The federal Health Insurance Portability and Accountability Act (HIPAA), Title II addresses the release of information about children and minors who are suspected victims of child abuse; essentially, HIPAA rules do not apply where the information “provides for the reporting of disease or injury, child abuse, birth, or death, or for the conduct of public health surveillance, investigation or intervention” (Section 160.203[c]) However, HIPAA laws cannot be completely disregarded. The appropriate entity should be notified. For example, the healthcare facility must notify child protective services agency and/or law enforcement; the nurse cannot call their best friend and gossip about the details. HIPAA laws still apply when medical information is provided to those who are not involved or needed in the intervention of abuse.
Safety
It is important to remember that although bizarre behavior may be exhibited by a parent or caregiver, the safety of the pediatric patient is a priority. Care for pediatric patients must be holistic. Maslow’s Hierarchy of Needs model can be helpful in caring for the pediatric patient who is a suspected victim of FDIA, recognition of physiological needs is the only priority above safety. Safety is a broad term, but essentially if there are warning signs of FDIA, healthcare providers have the responsibility to ensure safety for the patient in the medical facility and at home. Evaluation needs to precede quickly, such as psychiatric evaluations, specialist testing, pediatric case workers, etc. If the deception is corroborated with evidence that the pediatric patient is in a dangerous situation, the team will initiate reporting to law enforcement and legal proceedings to control the mother’s access to the child (3).
Support
A team should be created if FDIA is suspected, recruiting mental health providers, legal personnel, administration, and social workers. The medical disciples must act as a team to uncover the needed “mountain” of evidence that is required for this diagnosis. Multiple medical specialties are involved in officially reporting this condition, due to the critical need to rule out the reported diseases and establish the cause. The following specialists are often involved: allergy and immunology, dermatology, gastroenterology, oncology, orthopedics, and rheumatology. The illnesses and disabilities must be ruled out with a high level of certainty. Evaluations from third party investigators or psychologists that specialize in FDIA should be conducted.
There are ethical and legal challenges to diagnosing and reporting FDIA. The diagnosis must be supported by abundant documentation, and this could pose legal risks for providers. Allegations that are unsupported can increase the risk of liability for slanderous or defamatory statements (6). A pragmatic approach is key as false allegations can have a severely negative impact on patients and suspected perpetrators.
Treatment
Remember, FDIA is considered a pattern of behavior. Although patients found to have this condition may stop for a period of time, research shows this behavior will probably be long-term and chronic. The immediate approach is to remove the victim from harm and remove the opportunity to continue the deception. This is compared to a substance abuser, in which the illicit substance must be removed from their possession. Research supports the following trends on the majority of FDIA cases: (3)
- Poor response to pharmacotherapy
- Reluctance to engage with psychiatrists
- Tendency to relocate from area to area and thus lose contact with healthcare professionals
Treatment approaches:
- Early recognition and accurate assessment
- Many authors have advocated this since 1967 (3)
- Informing the perpetrator of the diagnosis
- Psychotherapy
- Cognitive and behavior therapy may help develop coping skills
- Medication
- Medications may be used to treat additional mental health disorders, such as depression or anxiety
- Inpatient therapy/ hospitalization
- In severe cases, psychiatric hospitalization may be necessary for safety and treatment.
- Legislation for detainment is controversial; this is determined by the mental health provider.

Self Quiz
Ask yourself...
- Do you have experience working with the pediatric, handicap, or elderly population?
- How do you think advocacy is different for this population?
- Can you describe how the allegations of “lying” about a child’s illness would differ from allegations of “inflicting” the child’s illness or injury?
- Do you have experience in inpatient or outpatient mental health facilities?
Resources
The American Professional Society on the Abuse of Children (APSAC) is an excellent resource for frontline professionals. The APSAC’s Munchausen by Proxy Committee is an interdisciplinary group of experts in this field (1). The Committee has developed professional guidelines for resources and information about law enforcement, epidemiology, intervention, treatment, and more (1). Mental health professionals who specialize in FDIA can also be found through this group.
There are terrific practicing tools on the following topics: (1)
- Forensic Interviewing of Children
- Forensic Mental Health Evaluations When Child Maltreatment Is at Issue
- Clinical & Case Management Guidance for FDIA
- The Investigation and Determination of Suspected Psychological Maltreatment in Children and Adolescents

Self Quiz
Ask yourself...
- Can you name an organization that provides resources for medical professionals in identifying and reporting abuse?
- Do you recognize any resources mentioned above in your previous/ current workplace?
- Can you think of ways you can make a difference in your workplace or community in the battle against child and elder abuse?
Conclusion
FDIA is a heavy and complicated disorder in which a person falsifies or induces physical or psychological illness or injury in another individual. The condition occurs without an obvious reward to the perpetrator and is not explained by another mental disorder. Statistical evidence, demographics, etiology, and signs and symptoms are meaningful in understanding FDIA. Nurses should beware of warning signs and feel confident in reporting and safety measures. Early detection and intervention are important for achieving better outcomes.
References + Disclaimer
- American Professional Society on the Abuse of Children (APSAC). (2023). Munchausen by proxy issue briefs, new clinical guidance from the APSAC taskforce, and more. Retrieved from https://www.munchausensupport.com/resources/
- Abdurrachid, N. & Gama Marques, J. (2022). Munchausen syndrome by proxy (MSBP): a review regarding perpetrators of factitious disorder imposed on another (FDIA). CNS spectrums, 27(1), 16–26. https://doi.org/10.1017/S1092852920001741
- Artingstall, K. (2017). Munchausen by proxy and other factitious abuse: practical and forensic investigative techniques. CRC Press/Taylor & Francis Group.
- Bursch, B., Emerson, N.D. & Sanders, M.J. (2021). Evaluation and management of factitious disorder imposed on another. J Clin Psychol Med Settings 28, 67–77. https://doi.org/10.1007/s10880-019-09668-6
- Enoch, D., Puri, B. K., & Ball, H. N. (2021). Uncommon psychiatric syndromes (Fifth edition). Routledge. https://doi.org/10.4324/9781315381145
- Fatade, O. & Ajibade, O. K. (2022). Medicolegal and ethical challenges in diagnosing and managing factitious disorder imposed on another (FDIA): A Case Report. Cureus, 14(11), e31513. https://doi.org/10.7759/cureus.31513
- McLeod, S. A. (2018, May 21). Maslow’s hierarchy of needs. Retrieved from https://www.simplypsychology.org/maslow.html
- Yates, G., & Bass, C. (2017). The perpetrators of medical child abuse (Munchausen Syndrome by Proxy) – A systematic review of 796 cases. Child abuse & neglect, 72, 45–53. https://doi.org/10.1016/j.chiabu.2017.07.008
Disclaimer:
Use of Course Content. The courses provided by NCC are based on industry knowledge and input from professional nurses, experts, practitioners, and other individuals and institutions. The information presented in this course is intended solely for the use of healthcare professionals taking this course, for credit, from NCC. The information is designed to assist healthcare professionals, including nurses, in addressing issues associated with healthcare. The information provided in this course is general in nature and is not designed to address any specific situation. This publication in no way absolves facilities of their responsibility for the appropriate orientation of healthcare professionals. Hospitals or other organizations using this publication as a part of their own orientation processes should review the contents of this publication to ensure accuracy and compliance before using this publication. Knowledge, procedures or insight gained from the Student in the course of taking classes provided by NCC may be used at the Student’s discretion during their course of work or otherwise in a professional capacity. The Student understands and agrees that NCC shall not be held liable for any acts, errors, advice or omissions provided by the Student based on knowledge or advice acquired by NCC. The Student is solely responsible for his/her own actions, even if information and/or education was acquired from a NCC course pertaining to that action or actions. By clicking “complete” you are agreeing to these terms of use.
➁ Complete Survey
Give us your thoughts and feedback
➂ Click Complete
To receive your certificate
