Course
Gender Affirming Hormone Therapy
Course Highlights
- In this Gender Affirming Hormone Therapy course, we will learn about actions to reduce healthcare barriers for individuals seeking gender-affirming care.
- You’ll also learn the intended effects, risks and benefits of gender-affirming hormone therapy in the adolescent (prepuberty) patient.
- You’ll leave this course with a broader understanding of legislative bills as they currently relate to care of a transgender person seeking gender affirming care.
About
Contact Hours Awarded: 2
Course By:
Maureen Sullivan-Tevault
RN, BSN, CEN, CDCES
Begin Now
Read Course | Complete Survey | Claim Credit
➀ Read and Learn
The following course content
Introduction
The purpose of this educational offering is to increase the nurse professional’s baseline knowledge and ability to provide both comprehensive and compassionate care to transgender persons. The transgender population has been the subject of healthcare disparities due to organizational biases and legislative interference, which has often resulted in disproportionately higher medical and mental health issues.
This program will focus on various aspects of gender-affirming care, from medical and mental health services to surgical intervention and legislative issues impacting the transgender community.
Definition of Terms
There are many terms that healthcare professionals should be familiar with in providing patient-centered and compassionate care.
Gender Identity
Gender identity is a term often associated with the sex of a person. In reality, the term gender identity more so aligns with an individual’s personal and internal sense of being. Gender expression further supports the notion of gender identity, as it relates to how a person publicly expresses themselves (choice of clothing, hair, make-up). While the sex of a person is determined or assigned at the time of birth, gender may or may not align with the assigned birth sex (1).
Sex, as in the “sex” of the baby at birth, is generally defined as the characteristics of a person established at the time of birth, often characterized as either male or female. The determination of which “sex” a person is then based solely on that of a physical and visual examination at the time of birth (2).
Gender, on the other hand, is considered a social construct, meaning that gender is affected by the behaviors, norms, and roles one interacts with in society. It is not affected by biology (chromosomal makeup). There are many categories of “gender”, including the following:
- Cisgender – their gender identity is the same as their assigned sex at birth.
- Transgender male – the person’s gender identity is male; he identifies as male; he prefers male pronouns but was assigned female sex at birth.
- Transgender female – the person’s gender identity is female; she identifies as female; she prefers female pronouns but was assigned male sex at birth.
- Gender nonbinary – a person who identifies as neither male or female and prefers gender neutral pronouns (they/them/theirs).
- Gender fluid – the person’s gender identity is not fixed and may fluctuate. Their identity and pronouns may also fluctuate.
- Genderqueer – the persons gender identity may align with both/neither/or somewhere in between male and female.
- Gender nonconforming – the person does not identify with any particular gender. Their pronouns may vary but are generally neutral pronouns.

Self Quiz
Ask yourself...
A patient who identifies themselves as “gender nonconforming” presents to your clinic today for an initial visit.
- Can you name efforts on your behalf will you make this person feel comfortable and welcome?
- How could you create an awareness of this gender identity situation in your coworkers?
- Describe current policies in your work setting that may unintentionally discriminate towards a transgender person who does not have a fixed gender identity?
Gender Pronouns
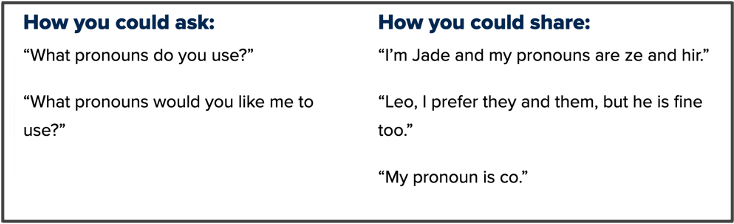
Common pronouns include she/her/hers, he/him/his, and they/them/theirs. A person’s personal choice of pronoun(s) is used to avoid being called by another pronoun, based solely on outward appearance. As a healthcare provider, self-identification on your own pronoun preference encourages others (coworkers and patients alike) to do the same and easily demonstrates the basics of a supportive, understanding environment. (3)
(3)
Sexual Orientation
Sexual orientation is defined as a person’s identity in relation to the gender or genders to which they are sexually attracted to. The term encompasses who you are attracted to and decide to have relationships with. The attraction may be for persons of the opposite sex (heterosexual) or of the same sex (homosexual), as well as persons who declare to be of both sexes or more than one gender. (4)
Sexuality includes more than just the familiar “straight, gay, lesbian and bisexual ‘identities. There are numerous types of sexuality, and healthcare providers should be familiar with these orientations so as to provide quality, patient-specific care.
Examples include the following:
- Asexual – there is little or no sexual attraction to others or have limited desire for sexual contact.
- Bisexual – attraction to both sexes and genders.
- Ceterosexual – attraction to transgender or nonbinary individuals.
- Fluid – sexuality changes and is not fixed.
- Libidoist asexual– asexual but experience sexual feelings and satisfy these through self-stimulation or masturbation.
- Omnisexual – attracted to “all” individuals regardless of sex or gender.
- Spectrasexual – attracted to multiple sexes and genders, but not necessarily all or any.
Explicit and Implicit Bias
Bias is defined as “prejudice in favor of or against one thing, person, or group compared with another, usually in a way considered to be unfair”. Bias is prejudice to such a degree that it is considered to be the result of a person’s closed-mindedness about a subject, whether due to innate surroundings, family upbringing, or learned behavior during the course of life. A person may develop a bias for or against another individual, a group of people, or simply a belief system.
Explicit bias refers to any conscious, easily identifiable bias (personal preferences, belief system and general attitudes) that can be openly communicated about. Implicit bias, on the other hand, is the unconscious behavior or thought process that a person chooses automatically, often without intention, insight, or personal awareness on their part. Implicit bias may be favorable or unfavorable for the parties involved and may be viewed as a pre-judgement of a person or group of people, without any evidence to substantiate the choice. (5)
The Implicit Association Test (IAT) can help you understand more about implicit bias and delve deeper into your own actions, feelings, and behaviors. Check out this link for more information:


Self Quiz
Ask yourself...
- What personal preferences/attitudes do you have, regarding healthcare, that may be perceived as biased by an outsider?
- Describe how a bias may actually be favorable to the parties involved?
- If implicit bias is an unconscious behavior or thought process that a person chooses without personal awareness, how can such choices be changed?
- What education can be done to positively affect ones “closed- mindedness” about gender affirming therapies?
Inclusion
In its most basic definition, the word inclusion means “the action or state of including or of being included within a group or structure” (6). In terms of gender affirming care and treatment, the term inclusion encourages practices and policies to provide equal access to opportunities and resources for those persons who might be otherwise excluded.
From a healthcare access standpoint, inclusion (inclusive practices) may refer to removing any barriers that prevent any/all persons from accessing the same quality of care and services (6).
Additionally, inclusive practices may involve cultural competency training for members of the healthcare team, customer service initiatives to promote equality, mutual respect, and a sense of belonging. Such practices and trainings ensure that one does not discriminate against a particular sex, or gender, and, in essence, help eradicate gender bias (7).

Self Quiz
Ask yourself...
- Describe, in your own words, what it means to be included within a group, such as with your coworkers?
- How do you create a tone of inclusion at work?
- Are there any practices or policies at your workplace that may, even inadvertently or unintentionally, exclude certain persons?
- How would you go about addressing current work practices, that exclude certain coworkers, to your senior management?
The Trans Umbrella
The “trans umbrella” refers to the term transgender, describing a person whose gender identity and behaviors do not conform to the sex that they were assigned at birth (8). As discussed previously, we are assigned a “sex” (either male or female) at birth, based primarily on physical attributes, that being our external and internal anatomy. Gender, on the other hand, refers more so to behaviors and roles considered appropriate for boys (and men) and girls (and women). These behaviors influence how people act, interact, and feel about themselves in society.
Example:
- Boys play with batman figurines; girls play with barbie dolls.
- Boys play football, girls play softball.
- Boys take shop classes at school; girls take home economics.
- Boys become doctors, firefighters, and police officers; girls become nurses or teachers.
Gender refers to the socially constructed roles, behaviors, activities, and attributes that a given society considers appropriate for boys and men or girls and women. These influence the ways that people act, interact, and feel about themselves. While aspects of biological sex are similar across different cultures, aspects of gender may differ.

Self Quiz
Ask yourself...
- What changes, at a society level, help reframe “traditional roles” for men and women?
- Can you think of external factors that have influenced society’s acceptance of these changes in the workforce?
- What similar external factors might influence our acceptance of transgendered roles in society?
Gender Affirming Care
The World Health Organization defines the term, “gender-affirming care” as care “designed to support and affirm an individual’s gender identity when it conflicts with the gender they were assigned at birth”. This holistic care model should include social, psychological, and medical interventions, as needed, to ensure quality care across the spectrum of services.
The goal of gender-affirming care is not necessarily actual medical treatment, but rather to create a safe environment for the patient in which concerns of emotions, medical care options, and more can be explored in a supportive, nonjudgmental way (9).
Gender affirmation care may involve numerous aspects of treatment, from hormone treatment, genital, urinary, and breast reconstruction, psychiatric services as well as ongoing primary care. “The goal is not treatment, but to listen to the child and build understanding — to create an environment of safety in which emotions, questions, and concerns can be explored,” says Dr. Jason Rafferty, lead author of a policy statement from the American Academy of Pediatrics (AAP) on gender-affirming care (9).


Self Quiz
Ask yourself...
- Have you participated, as a healthcare provider or healthcare consumer, in gender affirming care?
- How was the gender affirming care model different from “regular” medical treatment protocols?
- Do you feel comfortable making “gender affirming care” the regular and customary care model at your place of employment?
- Do you perceive any barriers that would prevent you from participating in “gender affirming care” delivery?
History and Background
German physician Magnus Hirschfield is considered by many to be the founder of transgender health care. Thought to have actually coined the term “transvestite” in 1910, Dr. Hirschfield’s work provided the early groundwork for what is now considered gender therapy and gender identity. He was the pioneer in “adaptation therapy” treatment, which enabled his patients to “live according to their nature” and was also credited with legal work establishing the support system necessary to allow name changes (10).
Magnus Hirschfield proposed that there are multiple gender expressions, theories that now support modern day concepts of gender diversity. His work was one of the first to offer patients hormone therapy, sex change operations or both. (10)
In 1919, he purchased a villa in Berlin, and opened The Institute for Sexual Research. By 1930, he and his team were performing some of the first gender-affirming surgeries. Sadly, the institute was not welcomed by all, and became a target by the Nazi party who believed in the extermination of millions of “lives unworthy of living”, including homosexuals and transgender persons. On May 6, 1933, while Magnus Hirschfield was out of the country, troops stormed the building, destroying decades of research, and engulfing an alleged 20,000 plus books in a tower high bonfire. Dr Hirschfield died in 1935 (11).
State Legislation: Current Trends
Research has shown that gender affirming care significantly improves both the medical and mental health and wellbeing of transgendered persons. Gender affirming care is patient-centered, holistic, and encompasses many elements of care often overlooked in traditional mainstream medicine.
Studies have shown that transgendered persons are at a higher risk for mental health issues and substance abuse. The proper treatment and ongoing care of these individuals is paramount to better health outcomes across the spectrum. Sadly, current legislation is lacking in these initiatives, and the result is yielding further negative outcomes in this vulnerable population (12).
In the past two years, 25 states have introduced legislative bills that would restrict access to gender affirming medical care for minors. Some of these bills have already been enacted into law. While healthcare organizations (including but not limited to, The American Medical Association, and The American Academy of Pediatrics) have spoken publicly to oppose such bills and laws, several states have passed laws stating that providing gender affirming care to minors will now be considered criminal activity for child abuse, and subject to civil liability, license revocation and/or other disciplinary sanctions.
The medical community continues to argue that these legislative bills ignore clinical guidelines for the proper treatment and benefits of gender affirming medical interventions. The state legislative representatives argue that minor children do not have the mental capacity to make such life altering decisions and are not capable of understanding the long-term effects of gender-affirming care (both medical and surgical treatment options).
Some argue that the “state” has overstepped the line by interfering with the medical decisions of a patient, their families, and their healthcare providers.

Self Quiz
Ask yourself...
- How do you feel about the effects of gender-affirming care on the mental health of transgendered persons?
- How do you feel about the use of gendering-affirming medications being prescribed to adolescents?
- Do you believe that an adolescent has the mental capacity to make an informed decision to use gender-affirming medications?
- What other gender-affirming therapies (gender neutral bathrooms, legal name changes, choices in pronoun usage) are you comfortable with?
Examples of State Legislation
A glimpse into state legislative bills that became law in Alabama, Arkansas, and Arizona.
In Alabama, state laws HB1/SB10 (2021)/HB266/SB184 (2022) criminalized aspects of gender-affirming medical or surgical care to transgender youth and required school personnel to reveal the gender identity of transgender youth to their parents. Alabama Gov. Kay Ivey signed the Vulnerable Child Compassion and Protection Act into law in 2022, making it a felony punishable by fines up to $15,000 and up to 10 years in prison for doctors to treat people under the age of 19 with puberty blockers or hormones to help affirm their gender identity.
In voting this bill into effect, the state of Alabama is considered to have discriminated against transgendered youth by denying them access to certain forms of medically necessary care, while forcing medical professionals to choose between providing medically appropriate procedures and treatments and facing criminal prosecution (13).
In Arkansas, Act 626 ( 2021), known as the Save Adolescents from Experimentation (SAFE) Act, prohibited physicians from providing “gender transition” treatments like hormones, puberty blockers and surgeries to those under age 18. Additionally, the SAFE Act outlined rules stating that insurance companies would not be reimbursed for any medication or medical procedures associated with gender transition to those under the age of 18. A federal judge struck down Arkansas’ ban on gender-affirming medical care for transgender youth in June 2023, nearly two years after blocking it from going into effect.
In Arizona, State Bill 1511 (2021) added some gender-affirming medical and surgical care to the state’s definition of child abuse and criminalized physician activity of this sort. Additionally, State Bill 1138 (enacted 2022) prohibits the provision of gender-affirming surgical care to transgender minors (14).
While the medical aspects of gender-affirming care represent a large opportunity to assist the gender transition in the final stages, the truth is there are many other avenues to explore that will significantly add value to gender-affirming initiatives. From community initiatives to develop a more inclusive and supportive environment, to school policies that review gender neutral bathrooms and locker rooms, there are many areas to consider that may make a society a gender affirming safe space for all.

Self Quiz
Ask yourself...
- Why do you think approximately 50 percent of the states have introduced legislative bills restricting gender affirming medical care for minors?
- Do you feel that gender affirming therapies are comparable to a form of child abuse?
- How would you educate your state legislators on gender affirming care for transgendered youth?
- Do you feel that transgendered persons are treated differently with respect to medical and mental healthcare?
Discrimination and other Barriers to Care
Transgendered individuals tend to face a wide variety of health disparities within the healthcare system. These disparities can include outright harassment from providers, as well as from other patients and medical providers within a healthcare setting. The disparities may also be more subtle, such as mislabeling of gender (by omission or intentionally), or treatment protocols that unintentionally discriminate through a provider’s personal bias and preconceived notions.
Sadly, these disparities result in a much more global healthcare inequality for transgendered persons. The “same level of care regardless “oftentimes does not exist for those being treated for mental health issues, for those who are victims of crime, and for those individuals who are suffering from substance abuse.
Healthcare providers must intervene and positively impact all patient experiences across the board, including those involved in gender affirming care. To do so, though, means all providers must have baseline knowledge of what is meant by gender affirming care, including sensitivity and inclusiveness training.
Sometimes, the only way to know a person’s gender is by asking them. In doing so, these providers have taken the first step towards significantly impacting a patient experience and overall health outcomes. The truth is that gender-affirming care begins with the first patient encounter and continues across the care spectrum.
Positive health outcomes are directly tied to gender supportive providers and healthcare systems. That is why “we do what we do”. We choose a career in healthcare so that we can positively impact health outcomes and quality of life across the board. Laws that prevent medical professionals from providing such care prevent transgendered youth from access to safe health care that is backed by years of research and endorsed by numerous medical associations (15).
Examples of efforts to increase awareness and inclusivity:
- Education on coping strategies
- School environments and curriculum (gender neutral bathrooms and locker rooms)
- Policymaking initiatives
- Gender affirming medical care/ mental health care.
- Law enforcement antibullying laws

Self Quiz
Ask yourself...
- Can you describe a patient encounter when you were unsure of the person’s gender?
- What could you have done differently to make the encounter more meaningful?
- Describe policies at your place of employment could take to make “transgender education” more accessible to all employees?
- Describe actions that could be implemented in the school system to make transgendered students feel safe and respected?
Hormone Therapy
Medication Options
Gender affirming hormone therapy is the primary medical treatment sought by persons included in the trans umbrella. Such hormone therapy allows the secondary sex characteristics to be more aligned with the persons gender identity. Gender affirming hormone therapy can be used as a stand-alone treatment for persons not interested in pursuing gender affirming surgery; it may also be used prior to surgery to improve surgical outcomes.
Indications of Use
Gender affirming hormone therapy (GAHT) is an important component of care for many trans people. These hormone therapies are medical forms of gender affirmation. Studies have shown that transgender persons are at high risk for both mental and physical health issues, when denied access to gender affirming healthcare. While GAHT is welcomed by the trans community, it is not without risk. GAHT has been linked with ongoing clinical changes/challenges in lipid metabolism, insulin resistance and thus heightens the risk for chronic disease. Ongoing lifestyle, medical and psychological therapies must be a part of any GAHT treatment plan. (16)
Puberty Blockers
Transgender youths who have not completed puberty can receive a class of medication called “puberty blockers” which suppress the release of sex hormones (testosterone and estrogen). These medications would suppress the growth of facial and body hair, as well as prevent the usual voice deepening associated with male puberty. For females, puberty blockers would stop normal breast development and interrupt the normal menstruation. If the puberty blockers are stopped during any point in the puberty growth cycle, normal hormone function returns.
The goal in using puberty blockers is thought to allow a person time to further determine their true gender identity before the emergence of permanent sex characteristics. These medications are also used in the younger population prior to the start of long-term, lifetime hormone therapy, as part of the entire gender affirmation therapy cycle.
After puberty blocker therapy, adults usually go on to receive hormone therapy aimed at increasing levels of either estrogen or testosterone to aid in the development of sex characteristics more aligned with their chosen gender identity (17). According to the National Transgender Discrimination Survey, 95% of transgender people and 49% of nonbinary people were interested in hormone therapy. (18)

Self Quiz
Ask yourself...
- What concerns do you have regarding the use of puberty blockers?
- Do you believe that children should have access to puberty blockers prior to the onset of puberty?
- What information could you tell parents of a transgendered child about these types of medications (regarding the risk versus benefit for their child)?
- Have you participated in cultural sensitivity (competency) training in your work setting?
Mechanism of Action
Masculinizing hormone therapy uses various types of testosterones to promote masculinizing changes in both binary and non-binary individuals. Testosterone is most often given as an injection, but other forms are available, including pills and creams.
The use of masculinizing testosterone therapy has been shown to cause any/all of the following effects:
- Body hair/facial hair growth
- Increased muscle mass
- Increased sex drive
- Body fat and facial fat redistribution
- Hairline recession “male pattern baldness”
- Changes in emotion
- Growth of the clitoris
- Interruption/cessation of normal menstruation
Feminizing hormone therapy, conversely, uses a combination of estrogen and a testosterone blocker. The additional use of a testosterone blocker in this case is due to the fact that testosterone is actually stronger in its effects on the body more so than estrogen. Various forms of estrogen may be used for gender-affirming hormone therapy, including oral tablets, transdermal patches, or injectables.
The use of feminizing estrogen in combination with testosterone blocker therapy has been shown to cause any/all of the following effects:
- Breast growth and development
- Body fat redistribution
- Reduction of facial and body hair
- Muscle mass reduction
- Testicular size reduction
- Reduction in erectile function
Intended and Unintended Side Effects
As with the use of any medication, there are certain risks associated with the use of these hormone therapies. In general, both classes of medications heighten the risk for the following:
- High blood pressure
- Blood clot formation
- High cholesterol
- Heart disease
- Type 2 diabetes
- Weight gain
- Certain types of cancers (primarily breast and prostate cancer)
- Infertility/Interfertility
Finally, gender-affirming hormone therapy cannot reverse/halt all changes occurring in puberty. Breast tissue growth, normal height increases, facial structure and underlying vocal pitch may not respond favorably to hormone therapy. In these cases, additional therapies (including surgical intervention, speech/vocal training, and other ancillary services) may be required.

Self Quiz
Ask yourself...
- How would you explain the risks of hormone therapies?
- What patient education would you provide to your GAHT patient on the risk of cancer, heart disease, and blood clot formation?
Gender Affirming Hormone Therapy and Drug Interactions
Feminizing hormone therapy usually focuses on estrogen-based medications, available in the following forms: oral tablets, injectables, patches and topical creams.
Therapeutic drug levels of these medications are known to be increased in the presence of the following medications:
- Antibiotics such as Clarithromycin, Erythromycin
- Antihypertensives such as Diltiazem, Verapamil
- Selective Serotonin Reuptake Inhibitor (SSRI)such as Sertraline, Paroxetine
- Antifungal medications such as Ketoconazole, Miconazole, and Fluconazole
- Antacid medication such as Cimetidine
Estrogen therapeutic drug levels are known to be decreased in the presence of the following medications:
- Anticonvulsant medication such as Carbamazepine, Phenobarbital, and Phenytoin
- Corticosteroid medications such as Dexamethasone
- Protease inhibitor/ antiretroviral medications including Nelfinavir, Ritonavir and Lopinavir
Masculinizing Hormone Therapy and Drug Interactions
Masculinizing hormone therapy usually focuses on testosterone-based medications, available in the following forms: injectables, patches of topical gel, oral tablets and testosterone pellets injected under the skin (20).
There are many medications that may interfere with testosterone hormone therapy, including the following:
- Anticoagulant blood thinners, such as Warfarin and Coumadin
- NSAIDS (non-steroidal anti-inflammatory medication) such as Toradol, Naproxen and Aleve
- Over the counter medications such as certain vitamins and herbal supplements
(20)
This is a very brief overview of potential drug interactions. Patients are always advised to speak with their healthcare provider and pharmacist for the most up to date information on possible drug interactions.
Contraindications
As with any use of long-term hormonal therapy and associated treatments, there is a screening process in place to ascertain if the patient is appropriate for GAHT. Some areas of consideration/concern have led to the following use of contraindications for GAHT usage (21). As always, the final determination is patient specific and taken on a case-by-case examination.
Listed among absolute contraindications were the following (in no specific order):
- History of hormone sensitive cancer (to include endometrial, breast, cervical and prostate cancer).
- Current alcohol or drug use/abuse.
- Liver insufficiency or cirrhosis.
- Uncontrolled preexisting chronic medical conditions (including diabetes and hypertension).
- Preexisting history of ischemic cardiovascular or cerebrovascular conditions.
- Severe psychiatric disorders influencing decision making capacity.
- Known noncompliance with previous medical treatment therapy.
(21)

Self Quiz
Ask yourself...
- Consider that you are the nurse for a transgender patient that has a known history of noncompliance with previous medical therapies, what patient education and counseling will you provide to this patient during your encounter?
- Consider a patient who has a history of type 2 diabetes, currently under control, would this be a contraindication?
- What additional patient education would this patient need regarding (pre-existing) chronic medical conditions?
Common Misconceptions
Across the country, efforts continue to block and eliminate gender affirming care and treatment options. Despite years of research finding favorable results with GAHT, inaccurate information and discriminatory laws continue to negatively impact access to this care. While a percentage of people still believe that gender affirming care is unsafe, medical research has shown that such care is not only medically necessary, but often lifesaving for transgendered persons of all ages. All persons, regardless of their gender identity, should have available to them affordable, holistic care in a supportive, nurturing environment.
Many people believe that children are being forced into life altering therapies, including surgical intervention, at a young age (before the age of lawful consent). The reality is that, prior to puberty, gender affirming care may include simple changes in clothing preference, hairstyles, and choice of pronouns. These plans of care are noninvasive and fully reversible. In the event of medical treatments prior to the age of puberty, the treatments can only occur after extensive consultations with the youth, the parents, and all members of a multidisciplinary team.
The use of puberty blocker medications is another area of concern for those that oppose GAHT. They falsely believe that these treatments are permanent, harmful, and nonreversible. The truth is that puberty blockers are temporary in nature and, once stopped, puberty and its related hormonal changes resume. These medications are prescribed to stop the physical and developmental changes associated with puberty, which allows the youth to further explore their gender identity issues before making permanent changes.
The American Academy of Pediatrics, American Medical Association, and the American Psychiatric Association support gender affirming care for transgender and nonbinary people (22).

Self Quiz
Ask yourself...
- Why do you feel that many people believe any and all gender affirming therapies are unsafe?
Patient Education
In addition to information already discussed on drug interaction, side effects, and treatment options, it is important that all patients undergoing GAHT be educated on the long-term plans of care. The use of GAHT is a lifetime process, not a short-term treatment, and persons undergoing such therapy should be educated on therapy expectations.
- Lifetime medication monitoring and management: As some of these hormone therapies have nonreversible effects, it is important to be diligent in routine monitoring and medical management, not only regarding the GAHT, but with routine/ preventive care with your primary care provider. Regular screenings reduce the risk of long-term side effects and complications.
- Ongoing mental health/ psychology therapy: Mental and physical changes will occur during the use of hormone therapy. Ongoing therapy and counseling sessions will ensure support and guidance as a person meets with such challenges. Such therapies are highly encouraged for the transgender person, but often include family members and, sometimes, the work environment.
Conclusion
In conclusion, many barriers and biases still exist towards the transgender community and their personal access to gender-affirming care. As healthcare professionals, we have a duty to provide patient-centered, quality care. In order to do so, we must first put aside our own biases towards transgendered persons and gender-affirming therapy. We must advocate for our patients and their loved ones in encouraging knowledge of and access to medically supported research and treatment options for gender-affirming care.
References + Disclaimer
- Chiniara, L. (n.d.). Gender Identity: Definitions, Development of Gender Identity – Usual Patterns, Development of Gender Identity – Differences in sex development (DSD). https://emedicine.medscape.com/article/917990-overview
- Bhatt, M. D., MPH, Cannella, M., & Gentile, M. D., MPH. (n.d.). Gender-affirming Care for Transgender Patients. Innovations in Clinical Neuroscience, 2022 Apr-Jun; 19(4-6), 23–32. https://www.ncbi.nlm.nih.gov/pmc/articles/PMC9341318/
- Pronouns and inclusive language. (2022, December 20). LGBTQIA Resource Center. https://lgbtqia.ucdavis.edu/educated/pronouns-inclusive-language
- Choosing Therapy. (2023). A guide to 25 different types of sexualities. Choosing Therapy. https://www.choosingtherapy.com/types-of-sexuality/
- Vela, M., Erondu, A., Smith, N., Peek, M., Woodruff, J., & Chin, M. (2022). Eliminating Explicit and Implicit Biases in Health Care: Evidence and Research Needs. Annual Reviews of Public Health, 2022 Apr 5; 43, 477–501. https://www.ncbi.nlm.nih.gov/pmc/articles/PMC9172268/
- CSHA. (2021, February 2). Gender Equality and Inclusivity – CSHA. https://www.csha.org/gender-equality-and-inclusivity/
- United Nations. (n.d.). UNITED NATIONS Gender-inclusive language. https://www.un.org/en/gender-inclusive-language/
- Understanding transgender people, gender identity and gender expression. (2023, June 6). https://www.apa.org. https://www.apa.org/topics/lgbtq/transgender-people-gender-identity-gender-expression
- Boyle, P. (2022, October 13). What is gender-affirming care? Your questions answered. AAMC. https://www.aamc.org/news/what-gender-affirming-care-your-questions-answered
- A history of transgender and gender diverse health care: From medical mistreatment to Gender-Affirmative Health Care. (n.d.). McGraw Hill Medical. https://accessmedicine.mhmedical.com/content.aspx?bookid=3104§ionid=259324704
- Schillace, B. (2021, May 10). The forgotten history of the world’s first trans clinic. Scientific American. https://www.scientificamerican.com/article/the-forgotten-history-of-the-worlds-first-trans-clinic/
- Kraschel, K. L., Chen, A., Turban, J. L., & Cohen, I. G. (2022). Legislation restricting gender-affirming care for transgender youth: Politics eclipse healthcare. Cell Reports Medicine, 3(8), 100719. https://doi.org/10.1016/j.xcrm.2022.100719
- Justice Department Challenges Alabama Law that Criminalizes Medically Necessary Care for Transgender Youth. (2022, April 29). https://www.justice.gov/opa/pr/justice-department-challenges-alabama-law-criminalizes-medically-necessary-care-transgender
- Kraschel, K. L., Chen, A., Turban, J. L., & Cohen, I. G. (2022b). Legislation restricting gender-affirming care for transgender youth: Politics eclipse healthcare. Cell Reports Medicine, 3(8), 100719. https://doi.org/10.1016/j.xcrm.2022.100719
- Attacks on gender affirming care by State Map. (n.d.). Human Rights Campaign. https://www.hrc.org/resources/attacks-on-gender-affirming-care-by-state-map
- Jones, P., Voison, S., Nolan, B., & Landen, S. (2022). Uncovering the effects of gender affirming hormone therapy on skeletal muscle and epigenetics: protocol for a prospective matched cohort study in transgender individuals (the GAME study). BMJ, 2022; 12(5): e060869. https://www.ncbi.nlm.nih.gov/pmc/articles/PMC9096568/
- Boyle, P. (2022b, October 13). What is gender-affirming care? Your questions answered. AAMC. https://www.aamc.org/news/what-gender-affirming-care-your-questions-answered
- Boskey, E., PhD. (2023). What is Gender-Affirming hormone therapy? Verywell Health. https://www.verywellhealth.com/gender-affirming-hormone-therapy-5083919#:~:text=It%20allows%20their%20secondary%20sex,develop%20typically%20female%20sex%20characteristics
- Vetters, R. (2021, June 23). Estrogen Therapy and Anti-Androgens as Gender Affirming Hormone Therapy. The National LGBTQIA+ Health Education Center. Retrieved October 4, 2023, from https://lgbtqiahealtheducation.org/wp-content/uploads/2021/06/TransECHO-Estrogen-and-Anti-androgen-Therapy-for-Gender-Affirmation-June-2021.pdf
- Testosterone Interactions Checker. (n.d.). Drugs.com. https://www.drugs.com/drug-interactions/testosterone.html
- Meyer, G., Boczek, U., & Bojunga, J. (2020). Hormonal Gender reassignment Treatment for gender dysphoria. Deutsches Arzteblatt International. https://doi.org/10.3238/arztebl.2020.0725
- National Association of Social Workers. (n.d.). Debunking the Myths About Gender-Affirming Care. https://www.socialworkers.org/. Retrieved October 3, 2023, from https://www.socialworkers.org/LinkClick.aspx?fileticket=SfQYdWPJAoY%3D&portalid=0
- Gender-Affirming hormone therapy. (n.d.). CooperHealth.org. https://www.cooperhealth.org/services/cooper-proud-lgbtq-health/gender-affirming-hormone-therapy
Disclaimer:
Use of Course Content. The courses provided by NCC are based on industry knowledge and input from professional nurses, experts, practitioners, and other individuals and institutions. The information presented in this course is intended solely for the use of healthcare professionals taking this course, for credit, from NCC. The information is designed to assist healthcare professionals, including nurses, in addressing issues associated with healthcare. The information provided in this course is general in nature and is not designed to address any specific situation. This publication in no way absolves facilities of their responsibility for the appropriate orientation of healthcare professionals. Hospitals or other organizations using this publication as a part of their own orientation processes should review the contents of this publication to ensure accuracy and compliance before using this publication. Knowledge, procedures or insight gained from the Student in the course of taking classes provided by NCC may be used at the Student’s discretion during their course of work or otherwise in a professional capacity. The Student understands and agrees that NCC shall not be held liable for any acts, errors, advice or omissions provided by the Student based on knowledge or advice acquired by NCC. The Student is solely responsible for his/her own actions, even if information and/or education was acquired from a NCC course pertaining to that action or actions. By clicking “complete” you are agreeing to these terms of use.
➁ Complete Survey
Give us your thoughts and feedback
➂ Click the Green MARK COMPLETE Button Below
To receive your certificate
