Course
Hypertension (HTN) Management Updates
Course Highlights
- In this Hypertension (HTN) Management Updates course, we will learn about the prevalence, incidence, and trends of HTN within broader public health dynamics.
- You’ll also learn how to identify potential cases of hypertension and screen individuals at risk, fostering interventions and mitigating adverse outcomes through prompt diagnosis..
- You’ll leave this course with a broader understanding of management strategies for individuals with hypertension including medication management, other interventions, and emerging research.
About
Contact Hours Awarded: 1
Course By:
R.E. Hengsterman
RN, BS, MA, MSN
Begin Now
Read Course | Complete Survey | Claim Credit
➀ Read and Learn
The following course content
Introduction
This course aims to provide nurses and healthcare professionals with an up-to-date understanding of hypertension (HTN). The course covers epidemiological evidence, etiology, diagnostic tools, medication management, other interventions, and future research on HTN.
Hypertension, or high blood pressure, is a chronic condition and a significant risk factor for heart disease, stroke, kidney failure, and other serious health problems. The American College of Cardiology defines hypertension as systolic blood pressure greater than 130 mmHg or diastolic blood pressure greater than 80 mmHg [1].
Statistical Evidence/Epidemiology
According to the Centers for Disease Control and Prevention (CDC), hypertension afflicts 108 million Americans and contributes to almost 500,000 deaths per year in the United States [2]. The prevalence of hypertension varies by race and ethnicity, with non-Hispanic Black adults having the highest majority (57.1%), followed by Hispanic adults (43.7%) and non-Hispanic White adults (43.6%).
Hypertension is also more common among older adults, with (74.5%) of adults aged 60 and over having high blood pressure [3]. Despite the high prevalence of hypertension, less than a quarter of all adults with hypertension in the United States have their blood pressure under control [2].
This leaves millions at risk for serious health problems from uncontrolled hypertension, such as heart disease, stroke, kidney failure, and eye problems. In 2021, high blood pressure was a primary or contributing cause of death for more than 691,095 Americans [4].
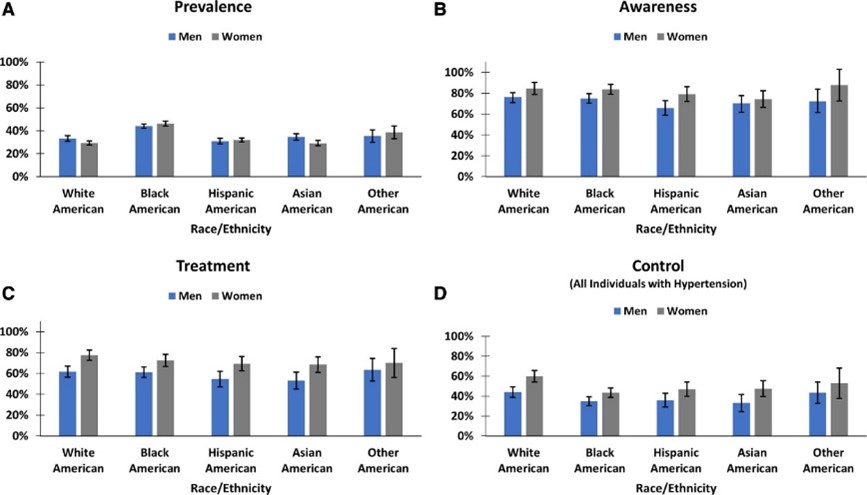
[31]

Self Quiz
Ask yourself...
- How do the current epidemiological statistics about hypertension affect healthcare planning and resource allocation?
- Given that hypertension is a significant public health problem and a major risk factor for serious health problems, what are the essential things that nurses and healthcare professionals should know about hypertension to manage their patients?
- Why do you think there exists such a pronounced disparity in the prevalence of hypertension among different racial and ethnic groups, and what societal and medical strategies might be employed to address this?
Etiology/Pathophysiology of Hypertension
Hypertension (high blood pressure) is a multifactorial disease characterized by persistent elevated blood pressure in the systemic arteries. Understanding hypertension's etiology, pathophysiology, and sequela is crucial for effective management and treatment.
There are two main types of hypertension: primary hypertension and secondary hypertension. Primary or essential hypertension (idiopathic hypertension), which accounts for about 80-95% of all cases, has no identifiable cause and results from complex interactions between genetic, environmental, and other unknown factors [5].
The cause of secondary hypertension (15-30% of cases) is often an underlying medical condition, such as kidney disease, adrenal gland tumors, diabetes, or thyroid disease [6]. Family history plays a role, although science has identified no genetic factor as the "hypertension gene" [7].
A key mechanism in hypertension is the imbalance between the forces that constrict and dilate blood vessels. This imbalance can be caused by several factors, including increased activity of the sympathetic nervous system, which leads to vasoconstriction, increased production of vasoconstrictor hormones, such as angiotensin II and aldosterone, a decreased output of vasodilator hormones, such as nitric oxide, and structural changes in the blood vessels, such as thickening of the vessel walls [8].
The most understood mechanism of hypertension involves increased peripheral vascular resistance due to constriction of small arterioles. The Renin-Angiotensin-Aldosterone System (RAAS) is a hormonal system that regulates blood pressure. Dysfunction of the RAAS can lead to fluid retention and vasoconstriction [9]. Endothelial dysfunction involves the inner lining of the blood vessels (endothelium) and the release of nitric oxide, which promotes blood vessel relaxation. The dysfunction of nitric oxide is a primary contributor to hypertension [10].
Secondary hypertension often involves:
- The kidneys and volume overload.
- Leading to elevated blood pressure.
- Often affecting younger patients and those with resistant or refractory hypertension.
The typical secondary causes of hypertension include:
- Primary aldosteronism (PA).
- Renovascular disease.
- Chronic kidney disease (CKD).
- Obstructive sleep apnea (OSA).
- Drug-induced or alcohol-induced hypertension [11].
Overactivation within the sympathetic nervous system can result in increased heart rate (tachycardia) and vasoconstriction, both of which can cause a temporary elevation in blood pressure. Within the metabolic process, insulin resistance has been associated with endothelial dysfunction and hypertension [12].

Self Quiz
Ask yourself...
- What underlying mechanisms or factors might contribute to the development of primary hypertension when classified as having no identifiable cause, and how might this classification influence our approach to treatment and management?
- What common myths and misconceptions about hypertension have you encountered in your practice?
- How do mechanisms like vascular resistance, RAAS dysfunction, and endothelial dysfunction interact or possibly counteract each other in the pathophysiology of hypertension, and what are the implications of this interplay for targeted therapeutic interventions?
- If hypertension is a complex disease with multiple causes, how can we develop effective treatments and prevention strategies?
Diagnostic and Screening Tools
The primary current diagnostic and screening tools around hypertension include blood pressure measurement. Blood pressure consists of systolic blood pressure (SBP) and diastolic blood pressure (DBP).
SBP is the pressure when the heart is beating, and DBP is the pressure when the heart is resting. A diagnosis of hypertension can be established when the Systolic Blood Pressure (SBP) is 130 mmHg or above or when the Diastolic Blood Pressure (DBP) is at least 80 mmHg [1].
The American Heart Association (AHA) recommends that all adults have their blood pressure checked at least once a year. People with risk factors for hypertension, such as obesity, diabetes, and kidney disease, should have their blood pressure checked more often [13].
Secondary tools for evaluating hypertension include ambulatory blood pressure monitoring (ABPM). ABPM is a more accurate way to measure blood pressure, measuring blood pressure over 24 hours. ABPM is an integral part of hypertensive care [14].
Urine tests can check for protein in the urine, a sign of kidney damage. Kidney damage is a risk factor for hypertension. Blood tests can be used to check for other medical conditions that can cause hypertension, such as diabetes and kidney disease, cholesterol levels, and other risk factors for heart disease.
Hormonal Tests can measure hormones produced by the adrenal and thyroid glands, which can help diagnose secondary hypertension. Regardless of the diagnostic or screening tools, early diagnosis and management of hypertension save lives [15].

Self Quiz
Ask yourself...
- What are the advantages and disadvantages of using blood pressure measurement as the primary diagnostic and screening tool for hypertension?
- What are some of the challenges of implementing ABPM as a routine screening tool for hypertension?
- How can we improve the early diagnosis and management of hypertension in all populations?
Imaging and Other Diagnostic Tests
Ultrasound of the Kidneys: To rule out kidney abnormalities.
Echocardiogram: To assess heart function and structure. Useful if hypertension has been longstanding.
Eye Exam: A fundoscopic examination can reveal changes in the retinal blood vessels, indicative of chronic hypertension.
Telemedicine: Remote monitoring can be helpful for ongoing assessment and titration of treatment.
Healthcare Apps: Smartphone apps can log and track blood pressure readings over time.

Self Quiz
Ask yourself...
- Considering the variety of diagnostic and screening tools available for hypertension—from traditional blood pressure measurements to digital devices like telemedicine and healthcare apps—how can healthcare providers ensure that they employ the most practical combination of methods for accurate diagnosis and long-term management of the condition?
- How does an early diagnosis contribute to better management and prognosis in hypertension patients?
Medication Management
The management of hypertension has evolved over the years, with numerous classes of medications available for treatment. The type of medication best suited for your patients will depend on their needs and health history.
Treatment strategies often begin with monotherapy, a single drug, usually a diuretic, beta-blocker, ACE inhibitor, or Angiotensin II receptor blocker (ARBs) [16]. Combination therapy for patients with stage 2 hypertension or those not reaching the target BP with monotherapy, which may include two or more drug classes, is also used.[16].
Step therapy involves starting with one drug and adding others to achieve the desired effect. A tailored approach is considered if comorbid conditions are present, such as diabetes or heart failure, which may influence drug choice.
Several standard classes of antihypertensive medications are used to treat hypertension, including first-line thiazides such as hydrochlorothiazide, which help rid excess salt and water and lower blood pressure [17]. Angiotensin-converting enzyme (ACE) inhibitors such as lisinopril and ramipril block the production of angiotensin II, a hormone that narrows blood vessels.
Angiotensin II Receptor Blockers (ARBs) such as losartan and valsartan which inhibit the action of angiotensin II, leading to vasodilation [17]. Beta-blockers such as atenolol or metoprolol slow the heart rate and reduce the force of the heart's contractions, which can lower blood pressure [17].
Calcium channel blockers such as amlodipine and diltiazem relax the muscles of the blood vessels by inhibiting the movement of calcium into vascular smooth muscle cells, thus lowering blood pressure [17]. Alpha-blockers such as doxazosin work by blocking alpha-adrenergic receptors, leading to vasodilation. Vasodilators such as hydralazine and minoxidil relax the muscles in blood vessel walls [17].
Central action agents such as clonidine, methyldopa, and moxonidine work on the central nervous system to lower blood pressure [17]. Moxonidine is a new-generation antihypertensive drug that works by activating imidazoline-I1 receptors in the brain, and it may be used when other antihypertensive drugs, such as thiazides, beta-blockers, ACE inhibitors, and calcium channel blockers, are not appropriate or have failed [18].
Thiazide-like diuretics such as chlorthalidone and indapamide have found increased use for their more prolonged duration of action and better cardiovascular outcomes when compared to traditional thiazides [19]. New evidence-based medications are coming into play, such as angiotensin receptor-neprilysin inhibitors (ARNIs), and a clinical trial is underway to test the effectiveness of a new drug called finerenone in preventing heart failure and kidney disease in people with hypertension and diabetes [20] [21].
Due to their safety profiles, there are special considerations with hypertensive management, including methyldopa and labetalol for pregnancy [22].
For older people, care is taken to avoid overtreatment, considering the risks of low blood pressure. For patients with chronic kidney disease (CKD), ACE inhibitors and ARBs are often favored due to their renal protective effects.
Generics are preferred when appropriate to reduce patient costs [23]. Digital adherence tools, including smartphone apps and telemedicine platforms, monitor patient compliance and adjust treatment as necessary.
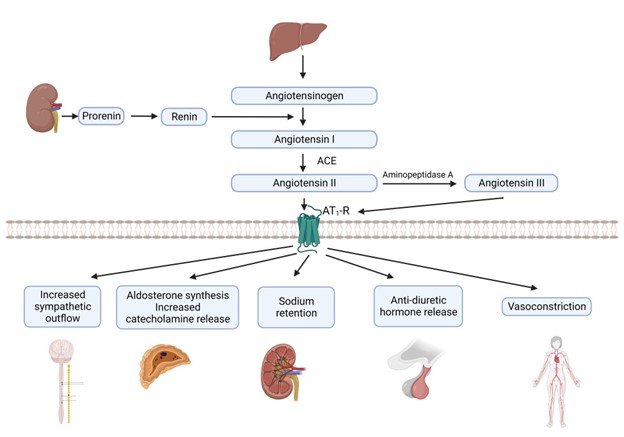
[32]

Self Quiz
Ask yourself...
- What challenges do healthcare providers face in medication compliance among hypertensive patients?
- Given the myriad antihypertensive drug classes and treatment strategies available, coupled with considerations for special populations such as pregnant women, older adults, and those with chronic kidney disease, how can healthcare providers effectively customize treatment plans while maintaining a consistent standard of care across different patient profiles?
Other Interventions
Beyond medication, lifestyle changes, including dietary interventions like the DASH diet and exercise, have proven effective in managing hypertension [24]. The DASH diet focuses on a high intake of fruits, vegetables, and low-fat dairy foods and is low in saturated and total fat.
A reduction in dietary sodium has been shown to lower blood pressure, with a general recommendation to consume less than 2,300 mg per day, with an ideal limit of 1,500 mg for most adults [24]. Regular aerobic exercise such as walking, jogging, or swimming can lower blood pressure.
Weight loss of even 5-10% can significantly impact reducing blood pressure [25]. Alcohol moderation and smoking cessation can also lead to blood pressure reduction.
Behavioral therapies, including stress management techniques such as deep breathing, meditation, and relaxation exercises, can help reduce short-term spikes in blood pressure. There is some evidence that suggests that Cognitive CBT can be effective in managing hypertension [26].
Biofeedback can help manage stress triggers and measure physiological functions like heart rate and blood pressure [26]. Although evidence is mixed, some studies suggest acupuncture can help lower blood pressure.
Renal denervation is an invasive procedure using radiofrequency energy to destroy kidney nerves contributing to hypertension. Central sleep apnea therapy can treat central sleep apnea and lower blood pressure.
Weight loss surgery can be an effective way to lower blood pressure in people who are obese or overweight. Several stress management techniques, such as yoga, meditation, and deep breathing, can be helpful.
Self-monitoring and regular medical check-ups can ensure that the treatment plan is effective and can be adjusted as needed. Remote consultations can offer more frequent touchpoints for adjustments in treatment plans.
Various mobile applications can help patients track blood pressure readings, medication schedules, and lifestyle changes. Community-based interventions to educate the public about hypertension risks, prevention, and management can be effective.
On a policy level, changes and initiatives that reduce sodium in processed foods can have a broader societal impact [27].

Self Quiz
Ask yourself...
- How do non-pharmacological interventions compare with medication management in terms of effectiveness and patient compliance?
- What roles do genetics and lifestyle factors play in the development of hypertension?
- How might the interactions among genetic factors, diet, obesity, lifestyle choices, and psychological elements contribute to the complex etiology of primary hypertension, and what does this complexity imply for diagnosing and treating secondary hypertension?
Upcoming Research
Using "Omics" genomic, proteomic, and metabolomic data to tailor antihypertensive therapies to individuals' researchers are working to identify the genes that contribute to hypertension and specific genetic markers that can help predict an individual's risk for developing hypertension and their potential response to treatments [28].
This information could be used to create new genetic tests to identify people who are at risk of developing the condition. Personalized medicine seeks to create customized approaches to managing hypertension, which would involve tailoring treatment to the individual's needs and risk factors.
Non-invasive treatments, such as devices worn on the body to deliver medication or stimulate the nerves, may also be effective. Researchers are developing a new type of blood pressure monitor that can be worn on the wrist and measure blood pressure throughout the day.
A study is underway to investigate the use of artificial intelligence to develop personalized treatment plans for people with hypertension. With predictive analytics, AI models are trained to predict hypertension risk and disease progression using large-scale electronic health records [29].
In the area of new therapeutic targets, researchers are looking into novel ways to improve endothelial function and vascular health. Studies into how the gut microbiome may influence blood pressure regulation offer potential for new treatment modalities [30]. Research on how diet interacts with genes within the gut microbiome may affect blood pressure.

Self Quiz
Ask yourself...
- How might advancements in technology and research change the landscape of hypertension management in the next decade?
- How can we balance the potential benefits of personalized medicine for hypertension with the challenges of ensuring that everyone has access to these new treatments?
Awareness and Patient Education
What your patients should know:
- Early diagnosis and treatment of hypertension are essential for preventing complications.
- There are several different types of medications available to treat hypertension.
- Lifestyle changes, such as eating a healthy diet, exercising regularly, and maintaining a healthy weight, can also help to lower blood pressure.
Nurses and healthcare professionals should be aware of the following:
- Nurses and healthcare professionals play a vital role in educating patients about hypertension and helping them manage their condition.
- The latest epidemiological statistics on hypertension, including its prevalence, risk factors, and impact on public health.
- The etiology and pathophysiology of hypertension, including the different types of hypertension and their underlying causes.
- The diagnostic tools used to diagnose hypertension include blood pressure measurement, ambulatory blood pressure monitoring, urine tests, blood tests, and imaging tests.
- The different types of medications available to treat hypertension, as well as their side effects and interactions.
Nurses and healthcare professionals can help patients to manage their hypertension by:
- Educating patients about hypertension and its risks.
- Helping patients develop a treatment plan that includes lifestyle changes and medications.
- Monitoring their blood pressure and adjusting their treatment plan as needed.
- Providing support and encouragement.
By working together, nurses and healthcare professionals can help patients manage their hypertension and reduce their risk of complications.

Self Quiz
Ask yourself...
- What are your key takeaways from this course, and how do you plan to implement these learnings in your clinical practice?
Conclusion
Hypertension is a significant public health problem in the United States and worldwide [1]. It is a chronic condition that can lead to serious health problems like heart disease, stroke, kidney failure, and eye problems. However, despite its complexity, hypertension is manageable with lifestyle changes, medications, and the potential information from future genomic discoveries [25] [17].
References + Disclaimer
- New ACC/AHA High Blood Pressure Guidelines Lower Definition of Hypertension – American College of Cardiology. (2017, November 8). American College of Cardiology. https://www.acc.org/latest-in-cardiology/articles/2017/11/08/11/47/mon-5pm-bp-guideline-aha-2017
- 2. Facts about hypertension | CDgov. (2023, July 6). Centers for Disease Control and Prevention. https://www.cdc.gov/bloodpressure/facts.htm
- 3. Ostchega, Y., Fryar, C. D., Nwankwo, T., & Nguyen, D. T. (2020). Hypertension Prevalence Among Adults Aged 18 and Over: United States, 2017-2018. NCHS data brief, (364), 1–8.
- 4. Multiple cause of death data on CDC WONDER. (2023, September 8). Retrieved September 18, 2023, from https://wonder.cdc.gov/mcd.html.
- Carretero, O. A., & Oparil, S. (2000). Essential Hypertension. Circulation, 101(3), 329–335. https://doi.org/10.1161/01.cir.101.3.329
- 6. Koch, C. (2020, February 4). Overview of Endocrine Hypertension. Endotext – NCBI Bookshelf. https://www.ncbi.nlm.nih.gov/books/NBK278980/
- 7. Manosroi, W., & Williams, G. H. (2018). Genetics of Human Primary Hypertension: Focus on Hormonal Mechanisms. Endocrine Reviews, 40(3), 825–856. https://doi.org/10.1210/er.2018-00071
- Ayada, C. (2015, June 1). The relationship of stress and blood pressure effectors. PubMed Central (PMC). https://www.ncbi.nlm.nih.gov/pmc/articles/PMC4938117/
- Terry, K. W., Kam, K. K., Yan, B. P., & Lam, Y. (2010). Renin-angiotensin-aldosterone system blockade for cardiovascular diseases: current status. British Journal of Pharmacology, 160(6), 1273–1292. https://doi.org/10.1111/j.1476-5381.2010.00750.x
- Bryan, N. S. (2022). Nitric oxide deficiency is a primary driver of hypertension. Biochemical Pharmacology, 206, 115325. https://doi.org/10.1016/j.bcp.2022.115325
- Sarathy, H., Salman, L. A., Lee, C., & Cohen, J. B. (2022). Evaluation and Management of Secondary Hypertension. Medical Clinics of North America, 106(2), 269–283. https://doi.org/10.1016/j.mcna.2021.11.004
- Muniyappa, R., Iantorno, M., & Quon, M. J. (2008). An Integrated View of Insulin Resistance and Endothelial Dysfunction. Endocrinology and Metabolism Clinics of North America, 37(3), 685–711. https://doi.org/10.1016/j.ecl.2008.06.001
- Heart-Health Screenings. (2022, August 23). www.heart.org. https://www.heart.org/en/health-topics/consumer-healthcare/what-is-cardiovascular-disease/heart-health-screenings
- Pena-Hernandez, C., Nugent, K., & Tuncel, M. (2019). Twenty-Four-Hour Ambulatory Blood Pressure Monitoring. Journal of Primary Care & Community Health, 11, 215013272094051. https://doi.org/10.1177/2150132720940519
- Gulec, S. (2013). Early diagnosis saves lives: focus on patients with hypertension. Kidney International Supplements, 3(4), 332–334. https://doi.org/10.1038/kisup.2013.69
- UpToDate. (2023, June 22). UpToDate. Retrieved September 18, 2023, from https://www.uptodate.com/contents/choice-of-drug-therapy-in-primary-essential-hypertension/print
- Types of Blood Pressure Medications. (2023, June 6). www.heart.org. https://www.heart.org/en/health-topics/high-blood-pressure/changes-you-can-make-to-manage-high-blood-pressure/types-of-blood-pressure-medications
- Moxonidine: a new antiadrenergic antihypertensive agent. (1999, August 1). PubMed. https://pubmed.ncbi.nlm.nih.gov/10489098/
- Liang, W., Ma, H., Cao, L., Yan, W., & Yang, J. (2017). Comparison of thiazide-like diuretics versus thiazide-type diuretics: a meta-analysis. Journal of Cellular and Molecular Medicine, 21(11), 2634–2642. https://doi.org/10.1111/jcmm.13205
- Greenberg, B. (2019). Angiotensin Receptor-Neprilysin Inhibition (ARNI) in Heart Failure. International Journal of Heart Failure, 2(2), 73. https://doi.org/10.36628/ijhf.2020.0002
- Filippatos, G., Anker, S. D., Agarwal, R., Ruilope, L., Rossing, P., Bakris, G. L., Tasto, C., Joseph, A., Kolkhof, P., Lage, A., & Pitt, B. (2022). Finerenone Reduces Risk of Incident Heart Failure in Patients With Chronic Kidney Disease and Type 2 Diabetes: Analyses From the FIGARO-DKD Trial. Circulation, 145(6), 437–447. https://doi.org/10.1161/circulationaha.121.057983
- Brown, C., & Garovic, V. D. (2014). Drug Treatment of Hypertension in Pregnancy. Drugs, 74(3), 283–296. https://doi.org/10.1007/s40265-014-0187-7
- Zhang, Y., He, D., Zhang, W., Xing, Y., Guo, Y., Wang, F., Jia, J., Yan, T., Liu, Y., & Lin, S. (2020). ACE Inhibitor Benefit to Kidney and Cardiovascular Outcomes for Patients with Non-Dialysis Chronic Kidney Disease Stages 3–5: A Network Meta-Analysis of Randomised Clinical Trials. Drugs, 80(8), 797–811. https://doi.org/10.1007/s40265-020-01290-3
- McGuire, H. L., Svetkey, L. P., Harsha, D. W., Elmer, P. J., Appel, L. J., & Ard, J. D. (2004). Comprehensive Lifestyle Modification and Blood Pressure Control: A Review of the PREMIER Trial. Journal of Clinical Hypertension, 6(7), 383–390. https://doi.org/10.1111/j.1524-6175.2004.03147.x
- Vasheghani-Farahani, A., Mansournia, M. A., Asheri, H., Fotouhi, A., Yunesian, M., Jamali, M., & Ziaee, V. (2010). The Effects of a 10-Week Water Aerobic Exercise on the Resting Blood Pressure in Patients with Essential Hypertension. Asian Journal of Sports Medicine, 1(3). https://doi.org/10.5812/asjsm.34854
- Li, Y., Buys, N., Li, Z., Li, L., Song, Q., & Sun, J. (2021). The efficacy of cognitive behavioral therapy-based interventions on patients with hypertension: A systematic review and meta-analysis. Preventive Medicine Reports, 23, 101477. https://doi.org/10.1016/j.pmedr.2021.101477
- Jachimowicz, K., & Winiarska-Mieczan, A. (2023). Initiatives to Reduce the Content of Sodium in Food Products and Meals and Improve the Population’s Health. Nutrients, 15(10), 2393. https://doi.org/10.3390/nu15102393
- Currie, G., & Delles, C. (2017). The Future of “Omics” in Hypertension. Canadian Journal of Cardiology, 33(5), 601–610. https://doi.org/10.1016/j.cjca.2016.11.023
- Chaikijurajai, T., Laffin, L. J., & Tang, W. W. (2020). Artificial Intelligence and Hypertension: Recent Advances and Future Outlook. American Journal of Hypertension, 33(11), 967–974. https://doi.org/10.1093/ajh/hpaa102
- Palmu, J., Lahti, L., & Niiranen, T. J. (2021). Targeting Gut Microbiota to Treat Hypertension: A Systematic Review. International Journal of Environmental Research and Public Health, 18(3), 1248. https://doi.org/10.3390/ijerph18031248
- Aggarwal, R. (2021, December 1). Racial/Ethnic Disparities in Hypertension Prevalence, Awareness, Treatment, and Control in the United States, 2013 to 2018. Hypertension. https://www.ahajournals.org/doi/full/10.1161/HYPERTENSIONAHA.121.17570
- Fountain, J. H. (2023, March 12). Physiology, Renin Angiotensin System. StatPearls – NCBI Bookshelf. https://www.ncbi.nlm.nih.gov/books/NBK470410/
Disclaimer:
Use of Course Content. The courses provided by NCC are based on industry knowledge and input from professional nurses, experts, practitioners, and other individuals and institutions. The information presented in this course is intended solely for the use of healthcare professionals taking this course, for credit, from NCC. The information is designed to assist healthcare professionals, including nurses, in addressing issues associated with healthcare. The information provided in this course is general in nature and is not designed to address any specific situation. This publication in no way absolves facilities of their responsibility for the appropriate orientation of healthcare professionals. Hospitals or other organizations using this publication as a part of their own orientation processes should review the contents of this publication to ensure accuracy and compliance before using this publication. Knowledge, procedures or insight gained from the Student in the course of taking classes provided by NCC may be used at the Student’s discretion during their course of work or otherwise in a professional capacity. The Student understands and agrees that NCC shall not be held liable for any acts, errors, advice or omissions provided by the Student based on knowledge or advice acquired by NCC. The Student is solely responsible for his/her own actions, even if information and/or education was acquired from a NCC course pertaining to that action or actions. By clicking “complete” you are agreeing to these terms of use.
➁ Complete Survey
Give us your thoughts and feedback
➂ Click the Green MARK COMPLETE Button Below
To receive your certificate
