Course
Incontinence Interventions in Complex Wound Management
Course Highlights
- In this Incontinence Interventions in Complex Wound Management course, we will learn about different types of incontinence and their prevalence.
- You’ll also learn common types of complex wounds, their underlying pathophysiology, and the phases of wound healing.
- You’ll leave this course with a broader understanding of common types of complex wounds, their underlying pathophysiology, and the phases of wound healing.
About
Contact Hours Awarded: 3
Course By:
Abbie Schmitt, MSN-ED, RN
Begin Now
Read Course | Complete Survey | Claim Credit
➀ Read and Learn
The following course content
Introduction
Welcome to our comprehensive course on Incontinence Interventions in Complex Wound Management, a crucial topic that addresses the intricate challenges faced by patients and caregivers. Imagine battling a chronic wound, such as a pressure injury. Now, add the constant battle of managing incontinence, where the skin around the wound is persistently exposed to moisture and irritation from urine or fecal material. This combination not only exacerbates the wound but also significantly impedes the healing process.
This course is designed to equip learners with an understanding of the physiological aspects of incontinence and wound management, assessment skills, strategies to protect the skin and promote healing, and collaboration within a multidisciplinary team to provide holistic care. We will also encourage the appreciation of the human side of nursing care—how to support patients with compassion, dignity, and respect.
The overall goals should be optimizing the patient’s overall condition, cleansing the wound, moisture control, infection prevention and management, debridement of any necrotic tissues, pain management, and pressure relief measures to prevent further injury.
Overview of Incontinence
As we explore incontinence, reviewing the basic anatomy and physiology of the urinary and gastrointestinal systems is important.
Renal Function and Urinary Incontinence
The urinary system, also called the renal system or urinary tract, comprises the kidneys, ureters, bladder, and urethra. The urinary system eliminates waste from the body, regulates blood volume and blood pressure, controls electrolytes and metabolites, and regulates blood pH (3). The kidneys filter blood in the nephrons and remove waste, producing urine.
Normal kidney function in a healthy adult produces 800 – 2,000 mL of urine per day, depending on fluid intake and loss; the bladder usually holds about 360 – 480 mL of urine (3). The bladder sends signals to the brain when it fills and needs to urinate. The urinary tract has a set of muscles that work together as a sphincter and has the role of closing the urethra to keep urine in the bladder until it is appropriate to urinate; the brain then sends signals to the wall of the bladder to contract and push urine out of the bladder and through the urethra (8).
An essential nursing intervention is to monitor and document urine output as part of the overall plan of care.
Terms commonly used to document conditions related to the urinary tract are as follows: |
|
| Anuria | Absence of urine output, typically found during kidney failure, defined as less than 50 mL of urine over a 24-hour period. |
| Dysuria | Pain or discomfort with urination. |
| Oliguria | Decreased urine output, defined as less than 500 mL of urine in adults in a 24-hour period. A new onset of oliguria can indicate dehydration, fluid retention, or impaired kidney function. |
| Polyuria | Urine output is more than 2.5 liters over 24 hours, also referred to as diuresis. Urine is typically colorless and clear. |
Urinary incontinence is the involuntary loss of control of urine flow. It is considered an abnormal finding; however, it is a common symptom that impacts the physical, psychological, and social well-being of affected individuals of all ages.
It has been estimated that 1 in 5 women develop urinary incontinence, but do not discuss it with their healthcare providers due to feelings of embarrassment (8). Nurses can greatly improve the quality of life for these patients by assessing for incontinence sensitively and then providing patient education about methods to prevent and/or manage incontinence.
Types of Urinary Incontinence
Continence is complex and obtained through coordination between the physiology of the bladder, urethra, sphincter, pelvic floor, and the nervous system. A disruption in any of these areas can cause several types of urinary incontinence. It is important to recognize the types of incontinence so that appropriate interventions can target the cause.
- Stress urinary incontinence is the involuntary loss of urine with intra-abdominal pressure (e.g., laughing and coughing) or physical exertion (e.g., jumping). Weak pelvic floor muscles are responsible and are often the result of pregnancy and vaginal delivery, menopause, and vaginal hysterectomy (8)
- Urge urinary incontinence is urine leakage caused by a strong sensation and desire to void. This is caused by stimulation of the bladder by the detrusor muscle or decreased inhibitory control of the central nervous system (8).
- Mixed urinary incontinence is a combination of urinary frequency, urgency, and stress incontinence.
- Overflow incontinence occurs when small amounts of urine leak from a bladder that is always full. This is common in males with enlarged prostates because it prevents the complete emptying of the bladder (3).
- Functional incontinence occurs with normal bladder control but the physical barrier of getting to the toilet due to medical conditions that impair mobility or dexterity to manipulate zippers or buttons. Patients with dementia can be at risk for functional incontinence.

Self Quiz
Ask yourself...
- How much urine is produced per day in a healthy adult with normal kidney function?
- Can you describe the various functions of the urinary system?
- Can you describe the possible psychological impact of incontinence?
- How would you define functional incontinence and possible interventions?
Gastrointestinal Function and Bowel Incontinence
The rectum, anus, pelvic muscles, and nervous system must work together to control bowel movements.
Bowel incontinence, also called fecal incontinence, is the accidental loss of bowel control causing the unexpected passage of fecal material. Incontinence can range from leaking a small amount of stool or gas to not being able to control bowel movements at all.
Bowel incontinence is caused by the disruption of one or more factors of the continence mechanism, which involves anal sphincter function, intact rectal sensation, adequate rectal capacity, compliance, colonic transit time, stool consistency, and cognitive and neurologic factors; 80% of patients have more than one compromised factor of continence (7). Also, if a patient is unable to recognize and respond to the urge to have a bowel movement, bowel incontinence can occur (8).
Causes of bowel incontinence can include the following:
- Chronic constipation, which causes the anus muscles and intestines to stretch and weaken.
- Fecal impaction and obstruction.
- Gastrointestinal, gynecological, or prostate surgery.
- Diminished sensation of the need to have a bowel movement.
- Injury to the anal muscles.
- Nerve or muscle damage from injury, cancer, or radiation
- Diarrhea that causes leakage.
- Cognitive or behavioral impairment.

Self Quiz
Ask yourself...
- Can you name examples of causative factors in bowel incontinence?
- Which is more common, bladder or bowel incontinence?
- How can chronic constipation lead to bowel incontinence episodes?
- Can you think of preventative measures for bowel incontinence?
Assessment
Assessment of Incontinence
Assessment should begin with gathering health history details and asking questions about voiding habits, frequency, and if there is difficult or painful urination. Incontinence questions can include: “Do you experience leakage or dribbling of urine? Do you ever have trouble making it to the bathroom in time?”. Hospitalized patients may have a major change in their typical bowel and bladder habits at home. For example, medical conditions and cognitive impairment during hospitalization, often caused by acute or chronic conditions or medications, may have resulted in incontinence.
Gathering details on the gastrointestinal system includes inquiring about normal bowel patterns, the date of the last bowel movement, a description of the stool, the presence of pain, and any recent changes. Clinicians agree that “normal patterns” should be one bowel movement every one to three days with stools having a soft or formed consistency (3). Based on the patient’s answers, additional questions can be included, such as bowel routines/toileting, the amount of fiber and fluid in the daily diet, daily activity, and the use of opioid medications. Patients who have recently had abdominal surgical procedures under general anesthesia are at increased risk of paralytic ileus.
Individualized treatment should be based on any structural abnormalities and urinary/gastrointestinal function.
Performing a physical assessment of the urinary system includes palpating above the symphysis pubis for distention. If incontinence is noted, the perineal area should be inspected for skin breakdown. If urinary retention is suspected, a post-void residual amount should be measured using a bladder scanner or by straight urinary catheterization (3).
A physical assessment of the gastrointestinal system can be performed concurrently; however, it is important to auscultate the abdomen for bowel sounds before palpation. During auscultation, note if bowel sounds are present, hyperactive, or hypoactive in all four quadrants. If bowel sounds are absent and if other signs of possible obstruction or paralytic ileus are noted, the provider should be notified immediately. Light palpitation of the abdomen should be performed; assess for tenderness, abnormal masses, and firmness in the left lower quadrant, which would indicate the presence of stool (8).
For inpatient care, it is meaningful to advise the patient to report when a urination or bowel movement has occurred so the stool characteristics can be assessed.
Document:
- Urine
- Amount
- Color and Clarity
- Abnormal or strong odor
- Particles or blood present
- Bowel Movement
- Amount (small, medium, or large)
- Consistency (soft, formed, or hard)
- Color

Self Quiz
Ask yourself...
- Can you describe a focused urinary assessment?
- Can you describe a focused gastrointestinal assessment?
- Why is it important to ask about normal patterns at home concerning bladder and bowel habits?
- Why are absent bowel sounds concerning?
Nursing Interventions in Incontinence
Nurses should encourage patients to feel comfortable in expressing their fears, worries, and embarrassment about incontinence. Let them know they’re not alone and that urinary incontinence is manageable. In cases with minimal progression of diseases and cognitive impairment, provide education about pelvic floor muscle training exercises, timed voiding, lifestyle modification, and products for incontinence support. Bladder control training is an effective method of preventing and reducing incontinence in many cases.
Bladder control training includes several techniques, including:
- Pelvic muscle exercises (commonly known as Kegel exercises) are designed to strengthen the pelvic floor muscles
- Timed voiding incorporates a set schedule, for example, every hour, whether the patient feels the urge to urinate or not. The time between voiding is gradually extended with the general goal of achieving four hours between voiding. Timed voiding can help with urgency and overflow incontinence because the brain is trained to be less sensitive to the sensation of the bladder wall expansion (7).
- Lifestyle changes, such as weight loss caffeine reduction, and constipation prevention, can help with incontinence. Limiting fluid intake before bedtime and discussing taking prescribed diuretic medication in the morning or early afternoon is helpful.
- Incontinence products may be needed to protect the skin from breakdown and prevent leakage onto clothing.
These tools and strategies are meant for stress or urgency incontinence in general. We will discuss detailed incontinence care plans further in the course regarding more complex incontinence with the presence of wounds proximal to the external genitourinary (GU) system.
A recent large-scale study found incontinence of urine only is much more common than bowel incontinence or combined (5).

Self Quiz
Ask yourself...
- Have you ever taught a patient how to perform Kegel exercises?
- Are you familiar with bladder and bowel training programs?
- What are ways to explain the importance of barrier creams for incontinence?
- Can you name lifestyle modifications that could help with night-time stress or functional incontinence?
Complex Wounds
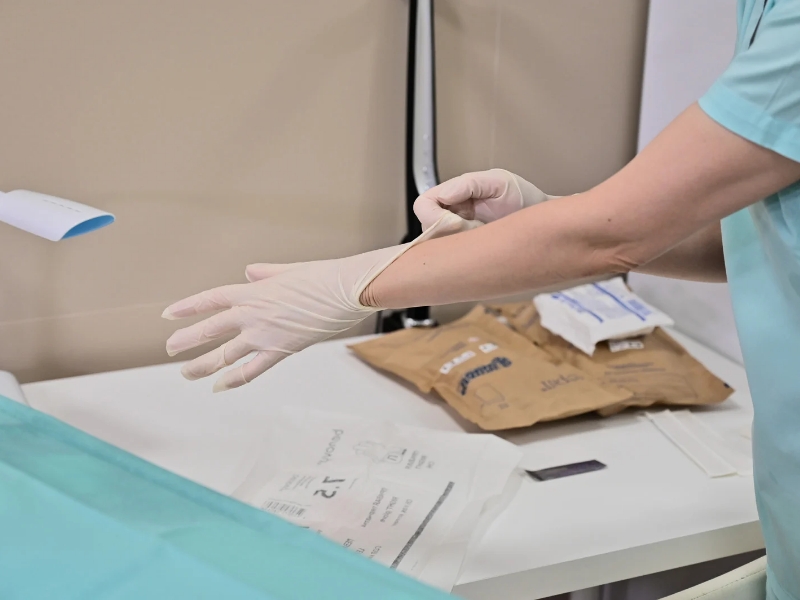
Basic Anatomy of Integumentary System
The integumentary system is considered the body’s largest organ. Skin serves as a protective barrier against heat, light, bacteria, infection, and injury; other functions include regulation of body temperature, storage of water and fat, sensory function, and a basic storage compartment for the organs (3).
The skin is made up of the following three layers:
- Epidermis
- Dermis
- Hypodermis (subcutaneous fat layer)
The epidermis is the thin outer layer of our skin, it contains squamous cells, basal cells, and melanocytes. The dermis is the middle layer of skin, it contains blood vessels, hair follicles, sweat glands, nerves, lymph vessels, fibroblasts, and sebaceous glands (3). It is important to remember that the dermis contains nerves and nerve receptors. The subcutaneous fat layer is the deepest layer of skin and is made up of a network of collagen and fat cells; this layer conserves the body’s heat and protects the body from injury by acting as a shock absorber (3).
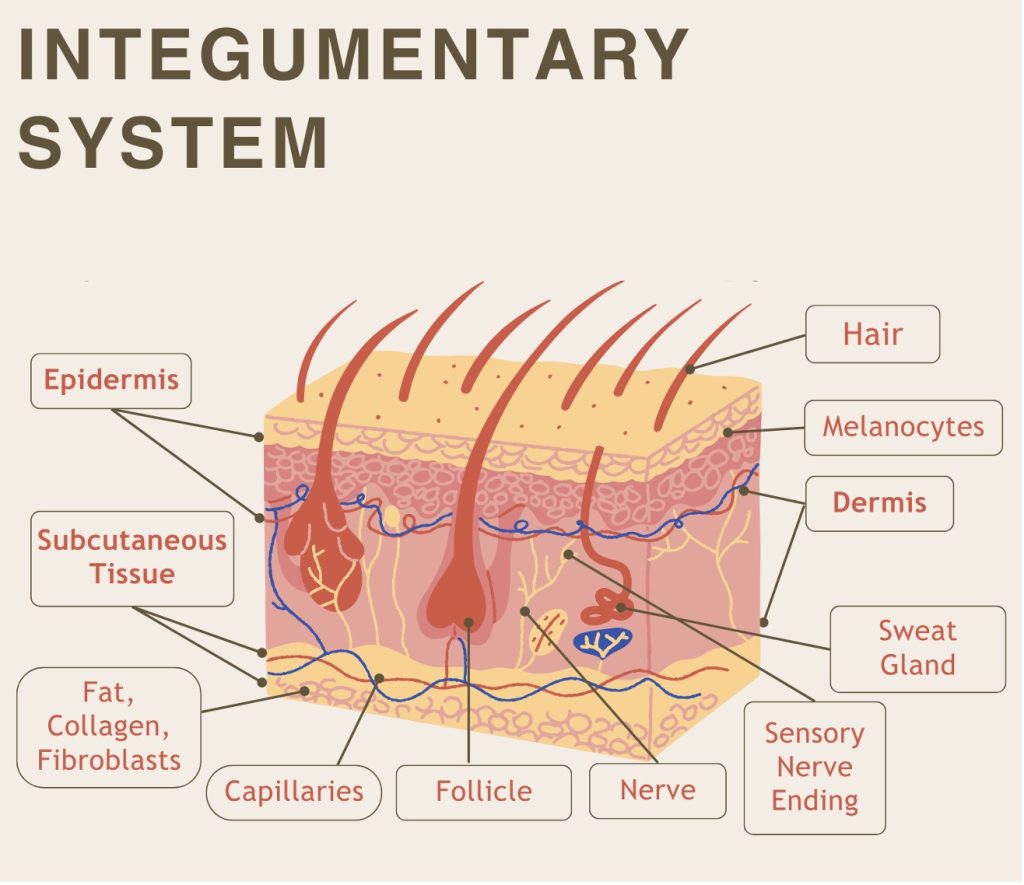 Image 1. Integumentary System (This design was created on Canva.com on September 23, 2023. It is copyrighted by Abbie Schmitt, RN, MSN, and may not be reproduced without permission from Nursing CE Central)
Image 1. Integumentary System (This design was created on Canva.com on September 23, 2023. It is copyrighted by Abbie Schmitt, RN, MSN, and may not be reproduced without permission from Nursing CE Central)
Pathophysiology of the Healing Process
Understanding the entire process of normal wound healing is critical. The body typically attempts to heal wounds immediately after the injury occurs, causing a unique cascade of processes.
There are four phases of wound healing: hemostasis, inflammatory, proliferative, and maturation (6).
Hemostasis begins immediately after an injury occurs, involving platelet aggregation and activation of clotting factors. A “plug” of platelets is formed as fibrinogen converts to fibrin and binds to itself. Vasoconstriction begins and decreases blood loss and allows clot formation.
The inflammatory phase begins after the injury as well, and the injured blood vessels leak and cause localized swelling. The swelling, warmth, pain, and redness present during this stage of wound healing are related to white blood cells being released, and the involvement of growth factors, nutrients, and enzymes to help control bleeding and prevent infection (6).
The proliferative phase of wound healing is essentially the “rebuilding” of new tissue made up of collagen and extracellular matrix. The granulation tissue is built stronger with proper oxygen and nutrients.
Ideally, the maturation phase of wound healing then occurs. In this phase, the collagen aligns along tension lines, water is reabsorbed, the collagen fibers cross-link, and the wound fully closes (1). Remember, in complex wounds, this stage takes a variable amount of time to achieve.
Abnormal and concerning factors can occur during the healing process as well. Dark granulation tissue can indicate infection, ischemia, or poor perfusion.
There are three types of wound healing (1):
- Primary intention: The wound healing is aided by sutures, staples, glue, or others to allow closure of the wound so the tissue beneath can begin regeneration.
- Secondary intention: Wound edges cannot be approximated, or “brought together”, so the wound essentially is not closed, but granulation tissue is generated from the bottom and heals upward (3). An example is pressure injuries. Secondary healed wounds are at much greater risk for infection, so contamination prevention and protection are essential.
- Tertiary intention. Tertiary intention refers to a wound that needs to remain open, often due to severe infection.
Wounds with secondary and tertiary intention have significantly longer healing times (1).

Self Quiz
Ask yourself...
- Can you describe the layers of the skin and their function?
- Which type of wound healing has a shorter healing duration on average: primary, secondary, or tertiary?
- Why is dark or black granulation tissue worrisome?
- Can you describe the phases of wound healing and why it is important to the understanding of individualized wound care?
Acute vs Chronic Wounds
It is important to recognize the difference in the healing process of acute and chronic wounds, as opposed to focusing on a specific time frame for healing.
An acute wound heals in an organized, timely, and durable way that does not require long-term follow-up; this type of wound has an identifiable mechanism of injury such as trauma or surgery (6). Acute wounds efficiently proceed through the phases of wound healing: hemostasis, inflammation, fibroplasia, epithelialization, and maturation.
Complex, or chronic wounds, are wounds that do not heal in the expected time and have complications like infection or chronicity; without treatment, the injured tissue can expand and get larger. A chronic wound does not progress through the healing process in an orderly and timely manner; tissue regeneration plateaus or “stalls” at some point due to pathologic conditions.
Common findings include a prolonged or excessive inflammatory phase (due to necrosis or bacteria colonization), infection, drug-resistant biofilms, and/or the failure of fibroblasts, endothelial cells, and keratinocytes to produce the new vessels and tissues, and delayed wound closure (6).
Biofilms refer to complex bacteria groups that create an extracellular polymeric substance that shields themselves from host immune defenses, most antiseptics, and some antibiotics (6). It may appear like a film or a thin layer of slough.
Chronic wound types include venous ulcers, arterial ulcers, pressure injuries, neuropathic (diabetic) ulcers, malignant ulcers, and hypertensive ulcers, among others. It is imperative to accurately determine the etiologic factors and to address the cause of the wound as well as the wound itself.
Acute wounds have higher mitogenic activity, while chronic wounds are characterized by higher levels of proinflammatory cytokines, elevated levels of MMPs, and greater numbers of senescent cells (6). MMPs are enzymes that are necessary for normal healing; they function to degrade abnormal components such as damaged collagen, and they promote the migration of immunologic cells, including neutrophils and macrophages, into the damaged tissue.
Types of Complex Wounds
Chronic wounds have been described as “complex wounds,” a term that describes the multifactorial dynamic tissue healing process.
For a wound to be classified as a complex wound, one of the following must be present:
- Persistent for more than three months
- Compromised vascularity or necrosis
- Presence of infection
- Associated comorbidities impair the healing potential
Pressure Injuries
A pressure injury is a localized injury of the skin and underlying soft tissue over a bony prominence and can often become a chronic and complex wound. Common sites include the sacrum, ischium, heels, trochanter, scapula, and occipital region of the head. Up to 15% of hospitalized patients can develop pressure injuries, and it is associated with a high mortality rate in the elderly.
The National Pressure Injury Advisory Panel (NPIAP) classifies pressure injuries into four categories according to their depth:
- Category I: non-blanching erythema
- Category II: partial thickness skin loss
- Category III: full-thickness skin loss
- Category IV: full-thickness tissue loss
[Add Course Photo 3 Here] Image 2. Stages of Pressure Injuries. (Image Reference: Stages of Ulcers Wikimedia User Sadegh Babagolzadeh, CC BY-SA 3.0)
Other Chronic Wounds
- Venous Ulcer
- Radiated Wounds
- Malignant Wounds
- Abdominal Wound Dehiscence
Wound Assessment
All wounds should be thoroughly assessed and documented. The wound assessment should include the following:
- Anatomical location
- Duration
- Measured dimensions (length, width, depth)
- Wound bed characteristics and percentage of viable/non-viable tissue
- Presence of tunnels (usually expect a higher volume of fluid)
- Characteristics of wound edges
- Type, amount, and description of exudate
- Presence of bleeding
- Signs and symptoms of infection
- Pain
- Integrity of the surrounding skin
- Skin integrity
- The general condition of skin – e.g. dry/moist, discolored
- Temperature
- Color
- Swelling
- Sensation

Self Quiz
Ask yourself...
- How would a closed, non-blanching area of skin with visible redness and erythema over a bony prominence be classified?
- Can you describe how circulation and glucose control can impact wound healing?
- Are you familiar with neurological conditions that impact sensation?
- What criteria must be met before a wound can be considered complex or chronic?
Barriers to Wound Healing
There are significant factors that impact wound healing, including age, comorbidities, and incontinence.
Age
Older adults have an increased risk of tearing and shearing due to the thinning of the epidermis and a decrease in elastin (9). Wound healing is also more complicated, and the phases of healing are prolonged in this population. Older adults are also more susceptible to bacterial growth and wound infections because the pH becomes more neutral with age (3).
Co-morbidities
Wound healing can be significantly impacted by certain medical conditions, including cardiac diseases, diabetes, neurological impairment, and conditions that result in immunosuppression (9).
- Cardiopulmonary Disease
- Oxygen is an essential element in wound healing
- Oxygen-transport pathways are impaired
- Peripheral Vascular Impairment
- Adequate perfusion is required for the regeneration of new tissue and immunological responses of the tissue.
- Arterial insufficiency leads to necrosis or lack of anti-inflammatory responses.
- Diabetes Mellitus
- Microvasculature and neuropathic components of DM increase the risk of impaired healing.
- Poor glycemic control can delay healing.
- Hyperglycemia increases the risk of infection.
- Conditions resulting in Immunosuppression
- Cancer, HIV, immunosuppressive therapy, immunosuppression syndrome
- Inflammatory phase (immunology) is impaired
- Increased risk for infection
- Conditions Resulting in Impaired Perfusion and Oxygenation
- Neurological Impairment
- Spinal cord injury, autoimmune response
- Peripheral Neuropathy
- Diminished neuronal signaling and transmission.
- Decreased sensory recognition of sensations of touch, pressure, temperature, and pain.
- Complications related to DM, alcoholism, chemotherapy
Bowel and Bladder Incontinence
Risk factors associated with wounds proximal to the genitourinary (GU) and gastrointestinal (GI) system:
- Increased Moisture and Maceration
- Incontinence results in persistent exposure of moisture, from urine or fecal material, causing excessive moisture, which impairs wound healing.
- Maceration: The skin becomes waterlogged, soft, and more prone to breakdown, which creates a favorable environment for wounds to develop and existing wounds to deteriorate.
- Irritation and breakdown from ammonia, urea, and digestive enzymes
- Urine and fecal material contain ammonia, urea, and digestive enzymes that irritate the healing factors and cause further injury.
- Exposure to these irritants leads to inflammation, redness, and skin breakdown.
- Increased Risk of Infection
- Moisture and fecal material contain bacteria, significantly increasing the risk of infection in complex wounds.
- These pathogens will enter and colonize the wound, further impeding healing.
The Overlap of Incontinence and Complex Wounds
Incontinence and open wounds are a recipe for poor outcomes. Incontinence increases the likelihood of pressure injury development, making the healing process even more challenging.
Incontinence-associated dermatitis (IAD) is a form of irritant dermatitis that develops from ongoing contact with moisture, mainly urine or liquid fecal material. IAD is one of four common types of moisture-associated skin damage (MASD) (4). MASD is defined as inflammation and erosion of the skin caused by prolonged exposure to various sources of moisture; sources of moisture include urine or stool, perspiration, wound exudate, mucus, or saliva (4). The four most common forms of MASD have been identified as incontinence-associated dermatitis (IAD), intertriginous dermatitis, peristomal moisture-associated skin damage, and peri-wound moisture-associated skin damage (6).
An intervention of providers and wound care nurses includes identifying and mitigating the source of moisture and recommending interventions to treat the skin damage. Sacral wound dressings in the presence of incontinence are challenging because the constant moisture compromises not only the skin tissue but also the dressing and topical medications. This area is already difficult to dress because of wound size, location, and shape. All these factors may prolong the healing time.
Moving forward, we will begin recognizing the interventions and management options for those impacted by incontinence and complex wounds.

Self Quiz
Ask yourself...
- Are you familiar with medications or cancer treatments that can damage tissue and prolong healing time?
- How can moisture prolong healing time?
- Can you describe how urine and fecal material can impact wounds?
- What are common conditions that impact wound healing?
Underlying Etiology Management
Wound healing is a multifaceted concept, with internal and external factors. Holistic care integrates them all into the care plan. Wound cleaning and protective barriers are essential, but evaluation of underlying factors is a key factor as well.
Wounds are often manifestations of chronic disease. The care plan must include measures to manage the chronic disease in addition to the wound by improving etiologic and contributing factors.
Common conditions that impact wound development and healing include:
- Diabetes
- Cardiovascular conditions
- Chronic obstructive pulmonary disease (COPD)
Understanding the disease process, adherence to medication regimen, proper diet, and lifestyle choices are meaningful in managing these conditions. Patients may be inconsistent with medication adherence due to socioeconomic issues. A recent survey of 1,527 patients with acute coronary syndromes or acute decompensated heart failure found a correlation between financial strain, poor medication adherence, and self-rated overall health (6). Essentially, individuals who have financial burdens often discontinue taking prescribed medications.
For optimal wound healing, blood glucose level should be less than 200g/dl, albumin level more than 3 g/dl, prealbumin level of more than 15 mg/dl, and lymphocyte counts greater than 1,500.
Proper nutrition is a key element of wound healing as well. Dietary modifications may include caloric reduction, sodium and saturated fat restriction, and glycemic control, which can be challenging due to social and cultural pressures.
Additional lifestyle modifications such as increased physical activity and smoking cessation can positively impact wound healing in many ways, including circulation and oxygenation of tissues.
Non-adherence to condition management often has a delayed reaction. In most cases, the negative effects of nonadherence manifest many weeks, months, or years later which can be a major barrier to behavior change. Concerning wound care, the effects of adherence may happen quickly in terms of wound healing or deterioration. Setting short-term goals with the patient may be an effective strategy for wound healing. For example, the nurse can provide education on smoking cessation or glycemic monitoring and establish goals with the patient such as reducing cigarettes per day for one week or keeping a journal of blood glucose levels.
Each comorbidity or risk factor is unique and patient education is a key element of adherence to treatment and medication regimens.
Take a moment to review the criteria and description of complex wounds from earlier in the course:
- Persistent for more than three months
- Compromised vascularity or necrosis
- Presence of infection
- Associated comorbidities impair the healing potential
Proper wound cleansing and treatment are excellent management strategies but remember that the root of the wound should be addressed in addition to external management strategies. All of these elements can be present; for example, a patient that has incontinence, compromised vascularity and circulation, a wound infection, and uncontrolled diabetes.
“Persistent for more than three months,” which is delayed wound healing, can be significantly caused by the constant presence of moisture and harmful pathogens with incontinence. Removal of this moisture is a key element, but this can be challenging due to many factors, including wound location, mobility of the patient, environmental factors, and comorbidities that impact cognition.
This course will focus on interventions that help reduce the elements of moisture and contamination related to incontinence.

Self Quiz
Ask yourself...
- Have you witnessed cases in which financial burdens and hardships can impact adherence to treatment regimens?
- How can keeping a glucose level journal or joining a support group encourage compliance?
- Are you familiar with other reasons patients may not adhere to prescribed medications or treatment plans?
- How can impaired cognition impact adherence to treatment plans and goals?
Management of Complex Wounds in the Presence of Incontinence
Minimizing Moisture
The skin serves to not only prevent the entry of harmful pathogens but to also prevent excess fluid loss from the body. Excessive moisture from any source can cause overhydration, particularly of the outermost stratum corneum. Constant moisture and overhydration of this outermost layer will lead to inflammation and breakdown. This is classified as moisture-associated skin damage (MASD).
Imagine leaving cardboard in the rain – the hydration causes sogginess and ultimately erosion and breakdown.
Patients with MASD experience persistent symptoms such as discomfort, burning, and pruritus in the areas of partial-thickness erosion and wound development. Emerging evidence highlights the association between MASD and other skin conditions such as dermatitis, cutaneous fungal and bacterial infection, and pressure injuries (6). For example, when the skin is exposed to liquid fecal material, the enzymes and irritants in the stool may cause inflammation and skin damage. Similarly, persistent urinary and/or fecal incontinence may create an environment favorable to the overgrowth of yeast, and candidiasis is commonly developed. The combination of overhydrated skin and minor friction can lead to wounds.
Peri-wound moisture-associated skin damage (PWMASD) is linked to the production of exudate during the inflammatory phase of wound healing and the osmotic and hydrostatic forces cause fluid to leak from the blood vessels and be absorbed by the exposed stratum corneum (6). As a result, the underlying epidermal layers become overhydrated and eroded. Essentially, wound exudate contains cellular debris and enzymes, which can damage intact skin. Peri-wound skin is more vulnerable to friction damage and invasion of pathogens and irritants. Current evidence shows an increased risk of PWMASD with chronic wounds due to chronic wound exudate. Chronic wounds are also more likely to become infected, which further increases the volume of enzymatic exudate, which will cause further breakdown of the surrounding skin.
Necrotic tissue also provides a medium for bacterial growth often debrided. Wounds in which debridement is not indicated should be closely monitored for signs of infection (e.g., separation and/or drainage at wound edges, erythema, induration, or fluctuance). Debridement of non-viable tissue can be done by many methods, either autolytic, larval therapy, chemical, hydro-surgery, bedside sharp debridement, or surgical debridement (6).
The main goals of the care plan should focus on optimizing the patient’s general condition, cleaning the wound, infection prevention and management, debridement of any necrotic tissues, pain management, and pressure relief measures to prevent further injury.
Hygiene and moisture reduction are very important, and the patient should consistently be kept dry. Properly delegating and overseeing tasks of hygiene is a vital intervention. Consistent use of prescribed products including skin protectants, moisture barriers, incontinence wipes, and/or perineal skin cleansers is also recommended to prevent further breakdown.

Self Quiz
Ask yourself...
- Can you describe the physiological changes that occur when skin is constantly drenched in liquid?
- How is wound healing impacted by a shortage or excess of moisture?
- Do bacteria colonies grow better on intact skin or necrotic tissue?
- Can you explain a typical turning schedule for patients with a high risk of pressure injuries?
Indwelling and Intermittent Catheterization
Urinary catheters may be used in the management of wounds under specific circumstances to help limit the impact of urinary incontinence on wound healing (2).
Urinary incontinence with the presence of wounds in the perineal, sacral, or coccygeal areas keeps the wound area dry and minimizes the risk of infection and maceration. For patients with limited mobility or who are bedridden, managing incontinence without a catheter can be challenging.
In chronic wounds that are not healing with standard wound care practices, and incontinence is a suspected contributing factor, a catheter might be used to improve the healing environment (2).
Recommendations and considerations (2):
- Indwelling catheters should generally be considered a short-term solution because prolonged use can increase the risk of catheter-associated urinary tract infections (CAUTIs).
- Closely monitor for signs of infection or complications associated with catheter use.
- Decisions about catheter use should involve a multidisciplinary team, including wound care specialists, providers, nurses, and infection specialists to ensure the benefits outweigh the risks and to develop a comprehensive care plan
- Consider alternatives if possible, including frequent incontinence care, use of absorbent products, barrier creams, continence training, and external urinary collection devices.
External Collection Devices
Complications linked to indwelling catheter use have caused a decrease in their usage and an increase in the use of female external urinary containment devices which can be safely used for urine diversion in males as well (6). External collection devices (ECDs) include latex and non-latex sheath devices (i.e., “condom” catheters). These devices are intended for bed and chair-bound patients who have incontinence.
Sheath devices are available in a range of sizes, and nurses and healthcare assistants should be trained in techniques of application and removal to prevent medical adhesive–related skin injury (MARSI).
Other ECD options for urine include a retracted penile pouch and a glans-adherent device (6).
Fecal management systems are sometimes used for the diversion of liquid stool in non-ambulatory patients. A silicone catheter with a soft inflatable cuff is retained in the rectum and connected to a drainage pouch or container. These devices offer the advantage of stool diversion and containment providing benefits for both skin health and infection control.
Evidence-based practice research has reported positive findings with the use of these systems. For example, a study conducted on ICU patients with bowel incontinence and/or diarrhea found that fecal collection devices connected to continuous low-negative-pressure suction devices yielded positive outcomes in proximal wound healing (10).
There are benefits to this non-invasive approach, but there are still negative outcomes associated with the use of the external device. Complications include the application being difficult due to anatomic contours and the pouch can be easily disrupted with patient movement or repositioning, causing leakage and frustration for the patient and caregiver.

Self Quiz
Ask yourself...
- Can you name a complication of indwelling urinary catheters?
- Why is sterile technique a critical aspect of catheter insertion?
Cleansing and Topical Agents
Terminology related to cleansing and topical agents is often misunderstood and misused (6). The overall evidence and recommendations on the efficacy of topical antimicrobials in the management of wounds are based on laboratory studies rather than clinical research.
Common definitions of topical agents include (6):
- Antibacterial: An agent that inhibits the growth of bacteria.
- Antibiotic: A natural or synthetic agent that can destroy or inhibit bacterial growth.
- Antimicrobial: An agent that either directly or indirectly kills microbial organisms or hinders the development of new colonies.
- Antiseptic: A nonselective, topical agent that may kill microorganisms or inhibit the multiplication of microorganisms.
A key intervention is to institute and follow a structured skin care regimen or algorithm using quality products. All wounds should be managed with an aseptic, non-touch technique using personal protective equipment (PPE) to prevent contamination and subsequent infection.
Prompt cleansing of urine and feces is imperative, using a product that does not raise skin pH and is gentle, followed by thorough drying of the skin. The use of warmed saline is generally recommended for cleansing the wound. The use of an antiseptic solution is recommended if there are excessive exudates or signs of infection but is highly subjective to provider orders and individual patient factors.
There are a variety of approaches aimed at protecting the surrounding skin from direct contact with leaked urine or feces to promote the healing, including:
The topical application of a skin protectant (also called a skin barrier) is also recommended. Skin protectants come in a variety of formulations and applications including creams, pastes, films, sprays, skin cleansers and wipes, etc. Periwound healing may involve replenishing moisture or lipids using topical products such as a moisturizer, humectant, or emollient.
Dressings
Once the wound is cleansed, the dressing may be applied. Common dressings include:
- Gauze
- Hydrogel dressings
- Hydrocolloid dressings
- Dressings containing silver or alginates
- Foam dressings
Dressings should be changed its visibly soaked with secretion, if they slip out of place, if fluid leaks out of the bandage, or if contamination occurs from incontinence. Wounds heal quicker in a clean environment as this facilitates the migration of numerous growth factors and epithelial cells to the wound bed.
There are four main principles involved in dressing choice, including:
- For wounds that have excessive discharge, this exudate needs to be absorbed.
- Dry wounds typically require hydration.
- Infected wounds require appropriate antimicrobial treatment.
- Wounds with necrotic tissue require debridement.
Essentially, dressing choice must be based on a holistic assessment of the wound bed and the patient’s overall condition.
Regarding the frequency of dressing change, infected wounds and wounds with high exudate should be monitored and changed more frequently, while non-infected wounds should be changed less frequently. Continuous wound assessment with each dressing change is essential.
There are three broad dressing category actions:
- Autolytic debridement in the wound bed by activation of the host’s proteolytic enzymes
- Moisture-preserving and enhancing
- Bacterial growth suppression
Gauze: One of the simplest and most commonly available products in healthcare environments. It is highly permeable, non-occlusive, and can be used as a primary or secondary dressing. A drawback is that it can adhere to the bed and lead to wound injury and removal of new tissue when removed. This removal is sometimes useful as a form of debridement, but only in cases when this is appropriate. When iodine, petroleum, bismuth, or zinc is applied to gauze, it becomes non-adherent and semi-occlusive. It is important to understand that bismuth or iodine is cytotoxic and inhibits inflammatory cells, so they should be changed regularly and time-limited (usually less than 5 days).
Iodine dressings: This type of dressing was first used in 1882; the mechanism of action of iodine is unclear but researchers suggested that low-dose, slow-release iodine can kill floating bacteria by rapidly penetrating their cells, hence its efficacy as an antiseptic solution
Transparent film dressing: These dressings are thin, flexible sheets composed of polyurethane; They provide moisture and do not provide absorption. This type of dressing is commonly used for dressing surgical wounds or the donor site of skin grafts.
Foam dressing: This is a polyurethane-based dressing that is typically used in wounds with moderate to high exudate. It is contraindicated for dry eschar or arterial ulcers, as it can impair the healing process.
Hydrogel: This type of dressing is a hydrophilic polymer consisting of about 90% water base; The high-water content is helpful to soften necrotic wound beds like pressure sores and vascular ulcers and dress low-exudate wounds, as it has minimal absorption properties. The surrounding skin should be protected from injury from the moisture.
Hydrocolloid: This dressing has a self-adhesive gel-forming hydrophilic inner layer of colloid particles that can absorb exudate, allow for a moisture-healing environment, and provide thermal insulation. The outer protective layer acts as a mechanical barrier for bacteria and foreign bodies. It is available in a paste, granules, and powder. Hydrocolloids should be avoided in infected wounds (6).
Alginate: This dressing is a highly absorbent, non-adherent, and biodegradable dressing; it is made from seaweed and covered with calcium/sodium salts. Calcium and sodium salts interact with an individual’s skin to form a hydrophilic gel once applied. It is considered highly effective for exudating wounds, abdominal dehiscence, pressure injuries, and infected wounds.
Hydrofiber: It is made of 100% CMC fiber. They have similar properties and usage of alginates, so they are also suitable for use in highly exudative wounds. They can be used in partial-thickness burn and graft donor sites. Hydrofiber has also been combined with silver which helps to maintain the antimicrobial properties for a longer period and a broader spectrum.
Silicone dressing: These dressings are used in cases of abnormal wound healing such as hypertrophic and keloid scars. Several studies showed that they soften the scar and prevent progression to hypertrophic scars. The exact mechanism of action is unknown. The most popular theory is an improvement of scar hydration by decreasing vapor loss. Unfortunately, most studies have been done with a small sample size, short-term follow-up, and without a control group.
Silver dressing: Silver is a broad-spectrum antimicrobial agent that is protective against bacteria, viruses, fungi, and yeast; it has also been reported to be effective against methicillin-resistant Staphylococcus aureus (MRSA) and vancomycin-resistant enterococci (VRE).
Triad hydrophilic dressing: Triad is a product that addresses the challenges that arise when applying wound foam dressings in the presence of incontinence.
Triad is an example of a product that has evidence-based practice supporting increased efficiency. Most foam dressings are considered contaminated if an incontinence episode occurs and contact is made, and foam dressings may not adhere if the skin is moist. Triad is different because it adheres to wet skin, thus allowing the dressing to stay in place. When a patient has an incontinent episode, this specific dressing does not require a full change, as a foam dressing does. Instead, the top layer is removed by cleansing, and additional product is reapplied as needed.
The overarching goals for the use of foam dressings in the presence of incontinence are to help manage pressure, maintain wound coverage, and provide protection from urine and feces. Ensuring that a dressing adheres to the skin is essential.

Self Quiz
Ask yourself...
- Can you discuss the principles to consider when choosing a dressing type?
- Why do you think the presence of infection or necrotic tissue would require a different type of tissue?
- Are you familiar with wound debridement?
- Does your place of employment have a wound care nurse?
Negative Pressure Wound Therapy
Negative pressure wound therapy (NPWT), also known as a wound vac, helps manage acute and chronic wounds. Negative pressure wound therapy (NPWT) is the application of sub-atmospheric pressure to help reduce inflammatory exudate and promote granulation tissue to enhance wound healing (9). Once the pressure is lower around the wound, the gentle vacuum suction can lift fluid and wound debris away and encourage the wound to heal.
Research supports that NPWT is more effective and promotes more rapid healing of chronic wounds compared with conventional dressing.
The mechanism of action is dependent on applying negative pressure, which is below atmospheric pressure, to the wound. The mechanism of action is not only in removing fluid and debris from the tissue, but the pressure causes stimulation of the growth of granulation tissue at a macroscopic and microscopic level.
An NPWT system consists of a sterile foam sponge, a semi-occlusive adhesive cover, a fluid collection system or canister, and a suction pump (9). The foam sponge is applied to the wound and covered. A fenestrated tube is embedded in the foam and the wound is sealed with adhesive tape to make it airtight, and the machine delivers continuous or intermittent suction, ranging from 50 to 125 mmHg (9).
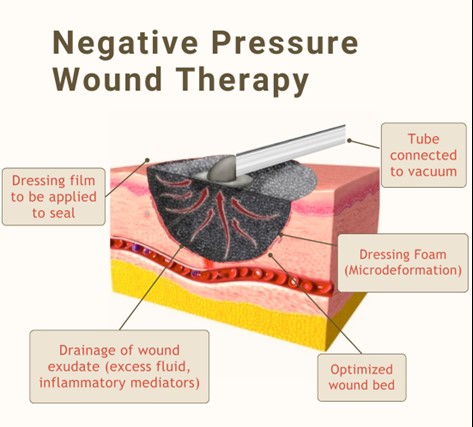 Image 3. Negative Pressure Wound Therapy (This design was created on Canva.com on October 1, 2023. It is copyrighted by Abbie Schmitt, RN, MSN and may not be reproduced without permission from Nursing CE Central)
Image 3. Negative Pressure Wound Therapy (This design was created on Canva.com on October 1, 2023. It is copyrighted by Abbie Schmitt, RN, MSN and may not be reproduced without permission from Nursing CE Central)
NPWT is contraindicated for the following (9):
- Malignant wounds
- Wounds involving untreated osteomyelitis.
- Wounds with exposed blood vessels
- Wounds with exposed nerves, anastomotic sites, or organs
- Wounds including open joint capsules
- Presence of necrotic tissue
The actions and sealed nature of NPWT make it suitable for patients without continence of bowel and bladder. A proper seal around the wound is essential, as well as cleanliness and assessment of the surrounding skin.

Self Quiz
Ask yourself...
- Can you describe the mechanism of action of NPWT devices?
- Why would a necrotic or malignant wound be contraindicated for NPWT?
- Have you worked with wound vacs in your professional practice?
- Can you discuss the benefits of NPWT for enhancing wound healing?
Case Study: Mrs. Lilly
Mrs. Lilly is a 72-year-old female who was admitted to the general medical unit due to sudden onset of confusion, fever, and elevated blood pressure. She resides in a long-term skilled nursing facility. The emergency department team found a Stage 3 pressure injury on her sacral area. She was not aware of the wound and the personnel with her was also not aware according to the healthcare records, this has not been treated.
History of Present Illness
Mrs. Lilly has a previous medical history of DM Type II, hypertension, and diabetic neuropathy (DPN).
Physical Examination
Examination in the ED reveals an alert 72-year-old female, who appeared anxious and confused, she is disoriented to place and situation. Vital signs are as follows. Blood Pressure 204/120 mmHg, Heart Rate 70/min – HR Thready – Respiratory Rate – 20 /minute; Temperature 102.0
- ENT/SKIN: Facial pallor and cool, moist skin are noted. No telangiectasia of the lips or oral cavity is noted.
- CHEST: Lungs are clear to auscultation and percussion. The cardiac exam reveals a regular rhythm with an S4. No murmur is appreciated. Peripheral pulses are present but are rapid and weak. A positive Stemmer sign was noted and palpable pedal pulses with mild symptoms of venous insufficiency were noted.
- ABDOMEN/RECTUM: The abdomen reveals a rounded abdomen. Bowel sounds are present.
Wound Assessment
- STAGE: Stage 3 (full-thickness skin loss involving damage to subcutaneous tissue) pressure wound to the midline sacral area. Size: 5 cm x 6 cm with a depth of approximately 1 cm.
- APPEARANCE: The wound bed shows granulation tissue, some slough, and minimal exudate.
- SURROUNDING SKIN: The peri-wound skin is erythematous and macerated.
Continence Assessment
Urinary incontinence is possibly temporary and related to probable infection. The type is likely a combination of stress and functional incontinence. Persistent moisture and contact with urine contribute to skin maceration and irritation around the wound.
Based on the findings:
- What risk factors for skin breakdown does Mrs. Lilly have?
- What labs or diagnostic studies could indicate her long-term glucose control?
- What would the initial priority be for this patient upon admission?
- Are there any nursing interventions you would implement for Mrs. Lilly?
The provider, nurse, and wound care nurse assessed Mrs. Lilly and determined the following treatments and orders:
- Etiology and diagnostic studies for causative factors for elevated blood pressure and temperature. Sudden confusion without a history of dementia is also being evaluated with lab work and cognitive studies.
- Bedside debridement of necrotic tissue to promote healing.
- Order for hydrocolloid dressing to maintain a moist wound environment while protecting the wound from further contamination.
- Order antimicrobial ointments to prevent infection and promote granulation.
- Skin Protection: Regular application of barrier creams around the wound and peri-wound area to protect the skin from urine.
- Application of high-absorbency incontinence pads to keep the skin dry, delegating to aids that changing them frequently to minimize moisture exposure is critical.
- Temporary indwelling urinary catheterization to keep the wound area dry.
- A dietitian consult was ordered to ensure adequate protein intake and balanced nutrition, which are essential for wound healing.
Goals:
- Reduction in wound size: An achievable goal would be for the wound size to be reduced to 3 cm x 4 cm within four weeks, with increased granulation tissue and decreased slough.
- Reduced maceration and erythema in the Periwound area.
- Protection of surrounding skin and bony prominences that are at higher risk for breakdown.
- Improved management of incontinence episodes, reduced frequency of skin exposure to urine, and education given to Mrs. Lilly and the staff at her skilled nursing facility.
- Appropriate utilization of dressings like hydrocolloids, foam dressings, or silver-impregnated dressings to manage exudate, protect the wound, and reduce bacterial load.
- Appropriate application of topical antimicrobial agents to control bioburden and prevent infection.
- Implementation of pressure-relieving devices such as specialized mattresses or cushions, ongoing turning schedule, ambulation support, and other measures to reduce pressure on the sacral area upon return to the skilled nursing facility.
- Order for a physical and occupational therapist to assist with mobility and exercises to reduce the risk of further pressure injuries.

Self Quiz
Ask yourself...
- Why is proper physical movement and nutrition essential in incontinence interventions and wound management?
- What are ways that nurses can provide advocacy for patients who are being discharged to home or a long-term facility?
- Are you familiar with various dressing orders and topical medications used in wound care?
- Why is a multidisciplinary approach critical to incontinence interventions and complex wound management
Conclusion
Hopefully, upon completing this course, you feel empowered in caring for patients with incontinence and a proximal complex wound. The course has navigated through the disruptive role of incontinence and the pathophysiology of wound healing. We have discussed various options for cleansing wounds, moisture control, infection prevention, and dressings. Interventions should be based on evidence-based practices, advanced wound care technologies, and a multifaceted, individualized approach to patient care. Remember, there are no wounds that are the exact same, each unique situation will require a specialized plan.
References + Disclaimer
- Baranoski, & Ayello, E. A. (2020). Wound care essentials: practice principles (5th ed.). Wolters Kluwer.
- Doughty, D. B., & Moore, K. N. (2016). Wound, Ostomy, and Continence Nurses Society core curriculum. Continence management (1st ed.). Wolters Kluwer.
- Ernstmeyer, K., & Christman, E. (Eds.). (2020). Nursing Fundamentals. WI Technical Colleges Open Press.
- Gray, Mikel; Bliss, Donna Z.; McNichol, Laurie. (2022). Moisture-associated skin damage: expanding and updating practice Based on the Newest ICD-10-CM Codes. Journal of Wound, Ostomy and Continence Nursing 49(2):p 143-151, March/April 2022. | DOI: 10.1097/WON.0000000000000865
- Kayser, S. A., Koloms, K., Murray, A., Khawar, W., & Gray, M. (2021). Incontinence and Incontinence-Associated Dermatitis in Acute Care: A Retrospective Analysis of Total Cost of Care and Patient Outcomes From the Premier Healthcare Database. Journal of wound, ostomy, and continence nursing: official publication of The Wound, Ostomy and Continence Nurses Society, 48(6), 545–552. https://doi.org/10.1097/WON.0000000000000818
- McNichol, Laurie, et al. Wound, Ostomy, and Continence Nurses Society Core Curriculum: Wound Management, Wolters Kluwer Health, 2021. ProQuest Ebook Central, http://ebookcentral.proquest.com/lib/liberty/detail.action?docID=7026348.
- Meyer, I., & Richter, H. E. (2021). Accidental Bowel Leakage/Fecal Incontinence. Obstetrics and Gynecology Clinics, 48(3), 467–485. https://doi.org/10.1016/j.ogc.2021.05.003
- Open Resources for Nursing (Open RN); Ernstmeyer K, Christman E, editors. Nursing Fundamentals [Internet]. Eau Claire (WI): Chippewa Valley Technical College; 2021. Chapter 16 Elimination. Available from: https://www.ncbi.nlm.nih.gov/books/NBK591831/
- Schmitt, A. (2023). Negative pressure wound therapy. Nursing CE Central Courses Page. https://www.nursingcecentral.com
- Zhou X, Wang Q, He Z, Xiao S, Ruan W. (2024). Application of fecal collection device in Intensive Care Unit Patients with fecal incontinence Receiving Extracorporeal Membrane Oxygenation: A Comparison Cohort Study. Altern Ther Health Med. 2024 Jan 31:AT9914. Epub ahead of print. PMID: 38330575.
Disclaimer:
Use of Course Content. The courses provided by NCC are based on industry knowledge and input from professional nurses, experts, practitioners, and other individuals and institutions. The information presented in this course is intended solely for the use of healthcare professionals taking this course, for credit, from NCC. The information is designed to assist healthcare professionals, including nurses, in addressing issues associated with healthcare. The information provided in this course is general in nature and is not designed to address any specific situation. This publication in no way absolves facilities of their responsibility for the appropriate orientation of healthcare professionals. Hospitals or other organizations using this publication as a part of their own orientation processes should review the contents of this publication to ensure accuracy and compliance before using this publication. Knowledge, procedures or insight gained from the Student in the course of taking classes provided by NCC may be used at the Student’s discretion during their course of work or otherwise in a professional capacity. The Student understands and agrees that NCC shall not be held liable for any acts, errors, advice or omissions provided by the Student based on knowledge or advice acquired by NCC. The Student is solely responsible for his/her own actions, even if information and/or education was acquired from a NCC course pertaining to that action or actions. By clicking “complete” you are agreeing to these terms of use.
➁ Complete Survey
Give us your thoughts and feedback
➂ Click Complete
To receive your certificate
