Course
Kentucky Renewal Bundle
Course Highlights
- In this Kentucky Renewal Bundle course, we will learn about diagnosis of pediatric abusive head trauma, and why it is important for nurses to recognize the signs.
- You’ll also learn the implications and long-term outcomes of unaddressed subconscious biases in healthcare and why it is important for providers to recognize and remove any biases that could impact their ability to offer equitable care.
- You’ll leave this course with a broader understanding of the mechanism of action of invasive and noninvasive ventilation.
About
Contact Hours Awarded: 14
Course By:
Various Authors
Begin Now
Read Course | Complete Survey | Claim Credit
Kentucky Alzheimer’s and Dementia Review
Introduction
Dementia is a broad term that describes a significant decline in cognitive abilities that interferes with a person’s daily life [1]. Alzheimer's disease (AD) is the most prevalent form of dementia, accounting for at least two-thirds of dementia cases in individuals aged 65 and older [1]. AD is a neurodegenerative disorder characterized by an insidious onset and progressive impairment of cognitive and behavioral functions, including memory, comprehension, language, attention, reasoning, and judgment [1][2]. Although Alzheimer's disease (AD) itself is not fatal through direct mechanisms, it increases susceptibility to complications that can lead to premature death including aspiration pneumonia which occurs when the disease causes difficulty in swallowing, leading to the inadvertent inhalation of food particles, liquids, or gastric fluids into the lungs [1].
In 2022, Alzheimer's disease was the seventh leading cause of death in the United States, according to the Centers for Disease Control and Prevention (CDC) [3]. This is a decrease from its previous position as the sixth leading cause of death before the COVID-19 pandemic, which ranked fourth in 2022 [3]. Alzheimer's disease often appears after the age of 65, known as late-onset AD (LOAD) [3][4]. However, early-onset AD (EOAD), which occurs before age 65, is less common and affects about 5% of patients with AD [4]. EOAD often presents with atypical symptoms and with aggressive progress, leading to delayed diagnosis and a more severe disease course [5].
Over the past decade, there have been significant advancements in identifying biomarkers for the early and specific diagnosis of AD. These include neuroimaging markers from amyloid and tau PET scans, as well as cerebrospinal fluid (CSF) and plasma markers such as amyloid, tau, and phospho-tau levels [6].
While there is no cure for Alzheimer's disease, treatments are available to manage and alleviate some symptoms. Recent advancements in medication and the discovery of new biomarkers have shown promise in moderating the disease's progression.
Warning Signs and Symptoms of Alzheimer’s Disease and Other Dementias
Alzheimer's disease features gradual and progressive neurodegeneration due to neuronal cell death [1][7]. The neurodegenerative process often initiates in the entorhinal cortex, a region within the hippocampus [1][8]. Genetic factors contribute to both early and late-onset AD. Trisomy 21, for example, presents a risk factor for early-onset dementia [9]. Alzheimer's disease (AD) symptoms vary depending on the disease stage, which classifies into distinct levels of cognitive impairment and disability. These stages include the preclinical or presymptomatic stage, mild cognitive impairment, and the dementia stage, further divided into mild, moderate, and severe stages [1][10].
This staging system differs from the diagnostic criteria outlined in the Diagnostic and Statistical Manual of Mental Disorders, 5th edition (DSM-5) [1]. The initial and most common symptom of typical AD includes episodic short-term memory loss [11]. Individuals often struggle to retain added information while their long-term memories remain intact. As the disease progresses, impairments in problem-solving, judgment, executive functioning, and organizational skills become evident [11]. Early in the disease, instrumental activities of daily living, such as driving, managing finances, cooking, and planning, suffer [1].
As cognitive decline advances, individuals may experience language disorders and impaired visuospatial skills. In the moderate to late stages, neuropsychiatric symptoms like apathy, social withdrawal, disinhibition, agitation, psychosis, and wandering become more prevalent [1][12]. Late-stage symptoms can include difficulty with learned motor tasks (dyspraxia), olfactory dysfunction, sleep disturbances, and extrapyramidal motor signs such as dystonia, akathisia, and Parkinsonian symptoms [1][12]. In the final stages, primitive reflexes, incontinence, and complete dependence on caregivers are common [1][12].
AD involves multiple factors and includes many known risk factors. Age serves as the most significant factor, with advancing age as the primary contributor. The prevalence of AD doubles with every 5-year increase in age starting from age 65 [13]. Cardiovascular diseases (CVD) increase the risk of developing AD and contribute to dementia caused by strokes or vascular dementia [14]. Recognizing CVD as a modifiable risk factor for AD has become more common.
Obesity and diabetes are also important modifiable risk factors for AD [15]. Obesity can impair glucose tolerance and increase the risk of developing type II diabetes [1]. Chronic hyperglycemia can lead to cognitive impairment by promoting the accumulation of beta-amyloid (A-beta) and neuroinflammation [1][16]. Obesity further amplifies the risk by triggering the release of pro-inflammatory cytokines and promoting insulin resistance [16].
Other potential risk factors for AD include traumatic head injury, depression, cardiovascular and cerebrovascular disease, higher parental age at birth, smoking, family history of dementia, increased homocysteine levels, and the presence of the APOE e4 allele [1][17]. Having a first-degree relative with AD increases the risk of developing the disease by 10% to 30% [18]. Individuals with two or more siblings with late-onset AD face a threefold higher risk than the general population [1][19].


Self Quiz
Ask yourself...
- How does understanding the different onset ages and progression patterns of Alzheimer's Disease (AD), along with the recent advancements in biomarkers and treatments, influence the approach to diagnosing and managing AD in patients?
- What might be the implications of the progressive nature of Alzheimer's Disease on an individual's daily life in the initial stages compared to the later stages?
- Considering the various risk factors for Alzheimer's Disease, how can lifestyle modifications influence the progression or onset of the disease?
Importance of Early Detection, Diagnosis, and Communication for Memory Concerns
Early detection and diagnosis of Alzheimer's disease (AD) are critical for effective management and care planning [20]. A thorough history-taking and comprehensive physical examination are fundamental in diagnosing AD. Gathering information from family and caregivers is also vital, as patients may lack insight into their condition. Evaluating a client's functional abilities, encompassing both basic activities of daily living (ADLs) and instrumental activities of daily living (IADLs), offers import information about their cognitive and functional status. IADLs require advanced planning and cognitive skills, including tasks like shopping, managing finances, filing taxes, preparing meals, and housekeeping.
In addition to medical history, inquire about the patient's social history, including alcohol use and any history of street drug use. These factors can influence cognitive function and require consideration in the diagnostic process.
Conduct a physical exam, including a neurological exam and mental status assessment, to evaluate the AD stage and rule out other conditions. The neurological exam in AD may appear normal except for anosmia. Anosmia also occurs in patients with Parkinson's disease, dementia with Lewy bodies, and traumatic brain injury (TBI) with or without dementia, but not in individuals with vascular cognitive impairment (VCI) or depression [1][21].
Perform and document cognitive assessments such as the Mini-Mental Status Exam (MMSE) or the Montreal Cognitive Assessment Exam (MOCA). The MOCA evaluates patients with mild cognitive impairment more effectively than the MMSE [22][23]. Another cognitive screening test, the Mini-Cog exam, involves a clock drawing test and a three-item recall [24]. The results of the Mini-Cog remain consistent regardless of the individual's level of education.
In the advanced stages of AD, patients may exhibit more focal neurological signs, including apraxia, aphasia, frontal release signs, and primitive reflexes [1] [25]. As the disease progresses, patients may become mute and unresponsive to verbal requests, leading to increased dependence on caregivers and becoming confined to bed and entering a persistent vegetative state.
During a mental status examination, evaluating multiple cognitive domains is important to determine the extent of cognitive decline in Alzheimer's Disease (AD) [1]. These domains encompass concentration, attention, recent and remote memory, language abilities, visuospatial skills, praxis, and executive functions [1][26]. Regular follow-up appointments for individuals with AD should incorporate a comprehensive mental status examination to monitor disease progression and the emergence of neuropsychiatric symptoms.
Effective communication techniques are essential when discussing memory concerns with the patient and their caregiver. Clear, empathetic communication helps in building trust and ensuring that the patient and caregiver understand the diagnosis, treatment options, and care plans. This approach fosters a supportive environment, enabling better management of the disease and improving the quality of life for both the patient and the caregiver.

Self Quiz
Ask yourself...
- Why is early detection and diagnosis of Alzheimer's Disease considered critical for effective management and care planning?
- How can effective communication techniques improve the management and quality of life for individuals with Alzheimer's Disease and their caregivers?
Tools for Assessing a Patient’s Cognition
Cognitive assessment uses various tools to evaluate various aspects of cognitive function, which diagnose and manage conditions such as Alzheimer's disease (AD) and other dementias. These tools build a clinical understanding of care needs through ongoing interactions with the patient and caregiver. Customize the choice of assessment tools to fit clinician preferences, practice composition, workflows, and clinical goals. Here are some commonly used tools
- Mini-Mental State Examination (MMSE): used for a quick assessment of cognitive function.
- Montreal Cognitive Assessment (MOCA): More sensitive than the MMSE for detecting mild cognitive impairment.
- Mini-Cog: Involves a clock drawing test and three-item recall, useful in primary care settings.
- Functional Assessment Staging Test (FAST): For staging dementia.
- Clinical Dementia Rating (CDR): For staging and evaluating dementia severity.
Use these tools alongside other diagnostic procedures such as blood tests, imaging (CT, MRI), and neuropsychological testing to evaluate
Documentation Requirements
Documentation of cognitive-relevant history should include factors contributing to cognitive impairment, such as psychoactive medications, chronic pain syndromes, infection, depression, and other brain diseases [28]. Medical decision-making documentation should cover the current and progression of the patient’s disease and the need for referrals to rehabilitative, social, legal, financial, or community services.
Patients without a firm diagnosis need documentation confirming cognitive impairment and a narrative history supporting the suspicion of potential cognitive impairment [28]. Use standardized tools for cognitive assessments and keep the full instrument raw scoring and results available for Medicare Administrative Contractor review if requested.
Required Tools and Assessments
Document the following standardized tools within the medical record:
- Cognitive assessment tools: Mini-Cog©, GPCOG, Short Montreal Cognitive Assessment (s-MoCA) [31].
- Functional assessment tools: Katz Index of Independence in Activities of Daily Living, Lawton-Brody Instrumental Activities of Daily Living Scale (IADL) [32].
- Dementia staging tools: Functional Assessment Staging Test (FAST), Clinical Dementia Rating (CDR® Dementia Staging Instrument), Dementia Severity Rating Scale (DSRS), Global Deterioration Score (GDS) [33].
- Neuropsychiatric assessment tools: Neuropsychiatric Inventory Questionnaire (NPI-Q), BEHAV5+©, Patient Health Questionnaire-2 (PHQ-2) [34].
Additional Documentation
Additional documentation of cognitive-relevant history should include:
- Medication reconciliation
- Evaluation of home and vehicle safety
- Identification of social supports and caregivers
- Advance care planning and palliative care needs

Self Quiz
Ask yourself...
- Why is comprehensive documentation essential in the management of cognitive impairment, and how does it influence the quality of care and support for patients?
- How do the use and documentation of standardized assessment tools impact management and care planning for patients with cognitive impairment?
- How does the selection and use of various cognitive assessment tools influence the diagnosis and management of Alzheimer's disease and other dementias?
Background and Introduction to CPT® Code 99483
The Alzheimer’s Association advocates for Medicare reimbursement for services to improve detection, diagnosis, and care planning for patients with Alzheimer's disease and related dementias (ADRD). This advocacy led to the approval of Medicare procedure code G0505 in January 2017, later replaced by CPT code 99483 in January 2018 [35]. CPT code 99483 reimburses physicians and eligible billing practitioners for a clinical visit that produces a written care plan [35].
Who Is Eligible for Comprehensive Care Planning Services?
Provide cognitive assessment and care plan services under CPT code 99483 when a comprehensive evaluation of a new or existing patient with signs or symptoms of cognitive impairment is necessary [35]. This evaluation aims to establish or confirm a diagnosis, etiology, and severity of the condition. If any required elements are missing or unnecessary, use the appropriate evaluation and management (E/M) code instead.
Requirements for CPT Code 99483
To bill under CPT code 99483, perform the following service elements [28]:
- Cognition-focused evaluation, including a pertinent history and examination
- Medical decision-making of moderate or high complexity
- Functional assessment (e.g., this includes basic and instrumental activities of daily living as well as decision-making capacity).
- Use of standardized instruments to stage dementia (e.g., Functional Assessment Staging Test [FAST], Clinical Dementia Rating [CDR]) [30].
- Medication reconciliation and review for high-risk medications
- Evaluation for neuropsychiatric and behavioral symptoms, including depression, using standardized instruments
- Assessment of safety, both within the home environment and in other settings, including considerations for motor vehicle operation if relevant.
- Identification of caregivers, their knowledge, needs, social supports, and willingness to take on caregiving tasks
- Development and periodic updating of an Advance Care Plan
- Develop a comprehensive written care plan that addresses neuropsychiatric and neurocognitive symptoms, outlines functional limitations, and includes referrals to community resources. Document and share this plan with the client and/or caregiver.
This service involves 50 minutes of face-to-face time with the patient and/or family or caregiver. Do not report cognitive assessment and care plan services if any essential elements are either absent or deemed unnecessary. Instead, use the appropriate evaluation and management (E/M) code [28].
Assessment Settings and Documentation
Evaluate the first nine assessment elements of CPT code 99483 during the care planning visit or across multiple visits using billing codes (often E/M codes) [36]. Include results of assessments conducted before the care plan visit if they remain valid or update them at the time of care planning. Complete assessments that require a care partner or caregiver before the clinical visit and provide them to the clinician for the care plan.
Cognitive Assessment and Care Planning Billing Codes
Use Current Procedural Terminology (CPT) code 99483 for a clinical visit that assesses cognitive impairment and establishes a care plan for patients with dementia or other cognitive impairments, including Alzheimer's disease [27][28]. This code applies to patients at any stage of impairment and once every 180 days billed to the insurance company.
Additional CPT codes related to cognitive assessment and care planning [27][28]:
- 99324–99337: Home visits for new patients
- 99341–99350: Home visits for established patients
- 99366–99368: Medical team conferences
- 99497: Advanced care planning for the first 30 minutes
- 97129, 97130: Cognitive functioning intervention services
Screening and Billing for Cognitive Assessment
Medicare Annual Wellness Visits (AWV) require screening for cognitive impairment [29]. Identify cognitive impairment during routine visits through direct observation or information from the patient, family, friends, caregivers, and others. Develop a cognitive assessment and care plan during a separate visit.
Bill CPT code 99483 apart from the annual wellness visit due to the time and medical decision-making [28]. If providing both services at the same visit, use a -25 modifier [28].

Self Quiz
Ask yourself...
- How does the use of specific CPT codes, such as 99483, facilitate the assessment and care planning for patients with cognitive impairments, including Alzheimer's Disease?
- How do the various service elements required for billing under CPT code 99483 contribute to a comprehensive approach to managing patients with cognitive impairment?
- What challenges do healthcare providers face in fulfilling the requirements for CPT code 99483, and how can they address these challenges to ensure comprehensive care for patients with cognitive impairment?
Eligible Providers and Settings
Any healthcare professional qualified to report Evaluation and Management (E/M) services can offer this service, including physicians (MD and DO), nurse practitioners (NP), clinical nurse specialists (CNS), certified nurse midwives (CNM), and physician assistants (PA) [28]. Practitioners must provide documentation substantiating a moderate-to-elevated level of complexity in their medical decision-making, following E/M guidelines [28]. Conduct care planning visits in the office, other outpatient settings, home, domiciliary, rest home settings, or via telehealth. Even when using telehealth, include all required service elements for CPT 99483 [36].
Utilizing a Care Plan Template
The required elements for this service may benefit from a standardized care plan template. This template can simplify communication and track patient care and outcomes but must allow for narrative unique to the patient. Discuss and give the written care plan to the patient and/or family or caregiver and document this face-to-face conversation in the clinical note. Share the care plan with other providers involved in the patient's care to ensure continuity and coordination.
Frequency of Service and Auditing
A single physician or other qualified health care professional reports CPT code 99483 no more than once every 180 days [28]. Revise the care plan at intervals and whenever the patient’s clinical or caregiving status changes. Ensure that revisions to reports exclude any service elements of CPT 99483 when billed through alternative E/M codes, such as those for chronic care management or non-face-to-face consultation [28][36].
The Alzheimer's Association's Cognitive Impairment Care Planning Toolkit is a valuable resource for practitioners, providing comprehensive guidance on creating effective care plans for patients with cognitive impairment.


Self Quiz
Ask yourself...
- What impact does the approval of CPT code 99483 have on the detection, diagnosis, and care planning for patients with Alzheimer's disease and related dementias?
- How does meeting the specific requirements of CPT code 99483 enhance the quality of care and outcomes for patients with cognitive impairment?
- How does the assessment setting and thorough documentation of the first nine assessment elements required by CPT code 99483 influence the effectiveness of care planning for patients with cognitive impairment?
- How does the flexibility in eligible providers and settings for CPT code 99483 enhance access to comprehensive care planning for patients with cognitive impairment?
- How does the use of a standardized care plan template enhance the effectiveness and coordination of care for patients with cognitive impairment?
Current Treatments Available to the Patient
The primary approach to treatment manages symptoms of Alzheimer's disease (AD). Two categories of drugs treat AD: cholinesterase inhibitors and partial N-methyl D-aspartate (NMDA) antagonists [1].
Cholinesterase Inhibitors
Cholinesterase inhibitors work by increasing the levels of acetylcholine, a neurotransmitter involved in learning, memory, and cognitive functions [1][37]. Three drugs in this category have received FDA approval for treating AD [1][37][38]:
- Donepezil:
- Preferred medication
- Used in AD with mild dementia
- Rapid and reversible inhibitor of acetylcholinesterase
- Administered once daily in the evening
- Rivastigmine:
- Used in mild cognitive impairment (MCI) and mild dementia stages
- Slow, reversible inhibitor of acetylcholinesterase and butyrylcholinesterase
- Available in oral and transdermal formulations
- Galantamine:
- Approved for MCI and mild dementia stages
- Rapid, reversible inhibitor of acetylcholinesterase
- Available as a twice-daily tablet or once-daily extended-release capsule
- Not suitable for individuals with end-stage renal disease or severe liver dysfunction
Common side effects of cholinesterase inhibitors include gastrointestinal symptoms such as nausea, vomiting, and diarrhea [37]. They may also cause bradycardia, cardiac conduction defects, and syncope due to increased vagal tone [37]. These medications are contraindicated in patients with severe cardiac conduction abnormalities [37].
Partial N-Methyl D-Aspartate (NMDA) Antagonist: Memantine
Memantine acts as a partial NMDA antagonist that blocks NMDA receptors and slows intracellular calcium accumulation [39]. The FDA has approved it for the treatment of moderate to severe Alzheimer's disease. Side effects may include dizziness, body aches, headaches, and constipation [39]. Combine memantine with cholinesterase inhibitors like donepezil, rivastigmine, or galantamine in individuals with moderate to severe AD [39].
Disease-Modifying Therapies for Alzheimer’s Disease
AD treatment managed symptoms. However, understanding AD's pathophysiology and improving diagnostic testing led to new disease-modifying therapies. These therapies target the disease's mechanisms, even in preclinical and presymptomatic stages.
Recent Therapy Approvals
- Aducanumab [40]:
- FDA accelerated approval in June 2020
- Shown to reduce amyloid-beta plaque in the brain
- Did not meet the primary phase III trial endpoint of clinical improvement
- Lecanemab [41]:
- FDA accelerated approval in January 2023
- Reduced amyloid-beta burden in the brain
- Phase III trial showed a 27% slowing of disease progression
- Donanemab [42]:
- Expected FDA approval in 2023
- Reduced amyloid-beta burden in the brain
- Slowed cognitive decline by 35%
Amyloid-Related Imaging Abnormalities (ARIA)
ARIA results from an immune response to amyloid-targeting therapies, causing capillary leakage and hemorrhages in cerebral vascular walls [43]. Two types exist: ARIA edema (ARIA-E) and ARIA hemorrhage (ARIA-H). Key risk factors for developing ARIA include the apolipoprotein E4 allele and cerebral amyloid angiopathy findings in brain MRI [43].

Self Quiz
Ask yourself...
- How do cholinesterase inhibitors function in the management of Alzheimer's disease, and what factors should clinicians consider when prescribing these medications?
- How do partial NMDA antagonists like memantine and recent disease-modifying therapies impact the treatment and progression of Alzheimer's disease?
Other Management Strategies in Alzheimer’s Disease
Manage symptoms such as anxiety, depression, and psychosis in the mid to late stages of the disease. Avoid tricyclic antidepressants due to their anticholinergic effects, which worsen cognitive impairment [44]. Use antipsychotic medications with caution for acute agitation when other interventions have failed, and the patient's or caregiver's safety is at risk. Try SSRIs like citalopram and anticholinesterases like donepezil before considering antipsychotics.
Prefer second-generation antipsychotics over first-generation antipsychotics due to their safer profile and fewer extrapyramidal side effects [45]. Brexpiprazole, approved by the FDA in May 2023 for treating agitation associated with dementia due to AD, serves as an example. Use the lowest effective dose when prescribing antipsychotics [46]. Avoid benzodiazepines as they worsen delirium and agitation [47].
Non-Pharmacological Interventions
- Behavioral Strategies: Establishing a familiar and secure environment is essential. This includes addressing personal comfort needs, offering security objects, redirecting attention when necessary, removing hazardous items, and avoiding confrontational situations.
- Sleep Disturbances: Addressing mild sleep disturbances through non-pharmacological strategies such as exposure to sunlight, daytime exercise, and establishing a bedtime routine.
- Exercise: Regular aerobic exercise slows the progression of AD.


Self Quiz
Ask yourself...
- What are the implications of amyloid-related imaging abnormalities (ARIA) in the treatment of Alzheimer's disease, and how should healthcare providers manage symptoms like anxiety, depression, and psychosis in patients with AD?
- How do non-pharmacological interventions contribute to the management and quality of life of patients with Alzheimer's disease?
Conclusion
Alzheimer's disease (AD) is the prevalent form of dementia, impacting cognitive and behavioral functions, and is a leading cause of death among the elderly [1]. AD presents with symptoms that progress from mild memory loss to severe cognitive and functional decline [1]. Early detection and diagnosis are critical for effective management, involving a thorough assessment of cognitive and functional abilities [48]. While there is no cure for AD, symptomatic treatments such as cholinesterase inhibitors and NMDA antagonists can help manage symptoms, and recent advancements in disease-modifying therapies offer new hope for slowing disease progression [49].
Comprehensive care planning, including regular cognitive assessments and tailored interventions, is essential for optimizing patient outcomes and supporting caregivers. Regular follow-ups and a multidisciplinary approach to treatment, incorporating both pharmacological and non-pharmacological strategies, can improve the quality of life for individuals with AD and their families.
Pediatric Abusive Head Trauma
Introduction and Objectives
Pediatric Abusive Head Trauma (AHT), also known as Shaken Baby Syndrome, includes an array of symptoms and complications resulting from injury to a child or infant’s head and brain after violent or intentional shaking or impact. There are approximately 1,300 reported cases of AHT each year and it is the leading cause of child abuse deaths nationally. For those children who survive, most suffer lifelong complications and disabilities (7).
This serious and tragic injury may be a challenge to diagnose because obvious signs of injury may not be easily detectable right away, and those responsible for the injuries may avoid taking the child for treatment (4). Therefore, it is incredibly important for healthcare professionals who work in pediatrics or emergency medicine to be able to identify at-risk individuals and recognize signs and symptoms of potential victims of AHT. It is also 100% preventable, and proper training on how to mitigate the risks and situations that lead to AHT can help healthcare professionals reduce the incidence of this horrific injury. Upon completion of this course, the learner will be able to:
- Identify risk factors and common mechanisms of injury for pediatric abusive head trauma.
- Describe signs and symptoms and diagnostic tools used to identify pediatric abusive head trauma.
- List potential outcomes of pediatric abusive head trauma and their prevalence.
- Understand the legal considerations of mandated reporters, process of reporting, and penalties for pediatric abusive head trauma perpetrators in the state of Kentucky
- Identify ways that societal and healthcare interventions can help reduce the prevalence of pediatric abusive head trauma
Epidemiology/Risk Factors
Though pediatric abusive head trauma most often occurs in children under age 5, the majority of these injuries are in children under the age of 1 year. There is a slight difference in incidence between genders, with 57.9% of victims being male and 41.9% being female. There is a peak occurrence of AHT between 3 and 8 months (4). Babies of this age are particularly vulnerable for a multitude of reasons, including large head size, weak neck muscles, fragile and developing brains, and the discrepancy in strength between infant and abuser. Sleep deprivation paired with longer and louder crying spells of very young infants sets the stage for high levels of caregiver frustration, which often precedes AHT injuries. The perpetrator is almost always a parent or caregiver (7).
Besides infant age, there are many social factors that increase the risk of AHT, including a lack of childcare experience, young or poorly supported parents, single-parent homes, low socioeconomic status, low education level, and a history of violence. These factors paired with a lack of prenatal care or parenting classes often leads to poorly prepared parents who have not been taught to anticipate crying spells or how to deal with the frustration in a safe manner (7).
Unfortunately, Kentucky has one of the highest rates of child abuse in the country. In 2019, there were more than 130,000 reports of suspected abuse or neglect, and 15,000 of those had substantial evidence to support abuse had occurred. Of those, nearly 76 were nearly fatal or fatal, and 32 of those were due to pediatric abusive head trauma(1).
Case Study
A Nursery nurse on a Labor, Delivery, and Postpartum unit is providing discharge information to the parents of a 2 day old baby girl, Violet, who is going home today. This is the first child for both parents. They are 19 years old, living in an apartment together while the mother works part time as a waitress and the father works full time for a lawn mowing company. The child’s maternal grandmother lives nearby and will be helping the mother care for the baby the first few weeks and then watching the baby a few days per week when the mother returns to work.

Self Quiz
Ask yourself...
- Which factors put this child at an increased risk of being abused?
- Which factors are protective against abuse?
- What resources might the nurse connect these parents with in order to maximize their support network once they are discharged?
Pathophysiology of Pediatric Abusive Head Trauma
While anyone can sustain a head injury, the relatively large size of young children’s heads paired with their weak and underdeveloped neck muscles is what makes them particularly susceptible to AHT. When a child’s head moves around forcefully, the brain moves around within the skull, which can tear blood vessels and nerves, causing permanent damage. Bruising and bleeding may occur when the brain collides with the inside of the skull or fractured pieces of skull. Finally, swelling of the brain may occur, which builds up pressure inside the skull and makes it difficult for the body to properly circulate oxygen to the brain (6).
It should be noted that bouncing or tossing a child in play, sudden stops or bumps in the car, and falls from furniture (or less than 4 feet) do not involve the force required to mimic the injuries of AHT (7).
Also important to understand is that AHT is a broad term used to describe the injury, but there are a collection of various mechanisms of injury within AHT. Among these different causes are Shaken Baby Syndrome (SBS), blunt impact, suffocation, intentional dropping or throwing, and strangulation. It is recommended to classify all of these injuries as AHT so as to avoid any confusion or challenges in court if multiple mechanisms of injury were involved (4).

Self Quiz
Ask yourself...
- Consider why it is important to know that falls from less than 4 feet do not typically cause much injury to babies and young children. What would you think if an infant presents with a serious brain injury and the parents state he fell off the couch?
- What sort of problems could occur in the litigation process if a child is diagnosed with Shaken Baby Syndrome but it is then revealed the child was thrown to the ground?
- Young children fall all the time while running, riding bikes, and climbing on playground equipment. What makes this less dangerous than an infant being shaken or thrown?
Diagnosis of Pediatric Abusive Head Trauma
Parents or caregivers who have inflicted injury onto a child may delay seeking treatment for fear of consequences. It is important to gather a thorough history and be on the lookout for inconsistent stories, changing details, or mechanism of injury that does not match the severity of symptoms (7).
Symptoms that typically lead caregivers to seek treatment for their child include:
- Decrease in responsiveness or change in level of consciousness
- Poor feeding
- Vomiting
- Seizures
- Apnea
- Irritability
Upon exam, these children may exhibit:
- Bradycardia
- Bulging fontanel
- Irritability or lethargy
- Apnea
- Bruising
A lack of any external injuries or obvious illnesses when presenting with these symptoms should alert the healthcare professional to the possibility of AHT, particularly in young children or infants. Additionally, unexplained fractures, particularly of the skull or long bones, bruising around the head or neck, or any bruising in a child less than 4 months are red flags (4).
An ophthalmology consult to assess for retinal hemorrhage should be obtained. The force used with AHT can cause a shearing effect with the retina and is visible with a simple fundal exam of the eye. This type of injury does not typically occur with accidental or blunt head trauma and is typically considered highly indicative of abuse. That same shearing force often causes bleeding within the brain, and subdural hematomas are often revealed on CT or MRI (4).
Any of the above criteria, or other suspicious story or injuries, should be reported for further investigation. Mild injuries are harder to detect but only occur around 15% of the time. Severe injury from AHT accounts for 70% of cases (4).
Case Study Cont.
Baby Violet is now 5 weeks old and is brought to the ED by her parents. Her mother reports that she has been eating poorly and acting strange since this morning. Her father reports he thinks she has been sleeping excessively for 2 days now. On exam, the baby is found to have a bulging fontanel, slow heart rate, and a bruise on the side of her head. Her mother states she sustained that bruise when she rolled off of her changing table yesterday.

Self Quiz
Ask yourself...
- What additional exam information would be necessary/helpful at this time? Specialty consult? Imaging?
- What assessment finding or diagnostic data might alleviate some suspicion that this is an abuse case? What would contribute to the suspicion?
Outcomes and Sequelae
For children diagnosed with even mild to moderate AHT, the prognosis is fairly grim. Up to 25% of children with AHT end up dying from their injuries, and for those who survive, 80% will have lifelong disabilities of varying severity (7).
The most common complications and disabilities include: blindness, hearing loss, developmental delays, seizures, muscle weakness or spasticity, hydrocephalus, learning disabilities, and speech problems. Lifelong skilled care and therapies are often needed for these children, accruing over $70 million in healthcare costs in the United States annually (4).

Self Quiz
Ask yourself...
- What characteristics of AHT would lead to long term disabilities like blindness, muscle spasticity, and speech problems?
- How do you think the cost of social programs and parental support programs within a community might compare to the costs of abuse investigation and healthcare costs for abused children?
Legal Considerations in the State of Kentucky
In the state of Kentucky, anyone with a reasonable suspicion that abuse or neglect is occurring is mandated by law to report the incident, and there are legal consequences (from misdemeanor all the way to felony) for willfully failing to make a report. For healthcare professionals, this is particularly important to note, as you will come in contact with many different types of families, injuries, and stories, and must remain vigilant in assessing for abuse (5).
A report of suspected abuse should be made at the first available opportunity and can be made by contacting the child abuse hotline (1-877-KYSAFE1), local law enforcement, Kentucky State Police, or the Cabinet for Health and Family Services. The child’s name, approximate age and address, as well as the nature and description of injuries, and the name and relationship of the alleged abuser should all be included in the report (9).
Once a report has been made, the Department for Community Based Services will determine if an investigation is warranted. If the home is deemed to be unsafe or there is a threat of immediate danger to a child, the child will be removed from the home, but in all other cases, every effort will be made to maintain the family (5).
Case Study
It is later determined that Baby Violet was violently shaken by her mother during a crying spell one evening. During legal proceedings for the incident, it is revealed that the grandmother witnessed this abuse.

Self Quiz
Ask yourself...
- Did the grandmother break any laws in this scenario?
- Is it likely that the child would stay in the home in this scenario, or do you think her safety is at a continued risk and removal would be necessary?
Prevention
While accurate detection of AHT is incredibly important, another key consideration for this injury and its poor outcomes, is that these incidents are 100% preventable. Much of the time, AHT is preceded by extreme frustration by a parent or caregiver when an infant is crying for long periods or is inconsolable. Proper education and preparedness about when and why this occurs, and what to do when it does, can help prevent AHT from occurring. For healthcare professionals who regularly care for infants, children, and expecting or new parents, there is a huge potential for positive impact (2).
Identifying those most at risk is a great starting place and new parenting courses, educational discussion and pamphlets, as well as regular check-ins are extremely beneficial for at-risk families. Young or inexperienced families, families without a lot of external support, or those with low socioeconomic status or poor education should be looked at first.
Once the most at risk families have been identified, provide them with information and services that may help reduce risks. These interventions are useful for anyone with an infant or small child, but special attention and close follow up should be given to those with more risk factors (8).
- Educate about infant crying: The PURPLE Crying program is particularly useful for this and includes facts and common symptoms of excessive or colicky infant crying. PURPLE stands for:
- Peak of Crying, with crying increasing weekly after birth and peaking around 8 weeks
- Unexpected, where crying may come and go with no apparent cause
- Resists soothing, where your baby won’t settle no matter what you try
- Pain like face, where your baby looks like they are in pain even if nothing is wrong
- Long-lasting, with crying lasting as long as 5 hours
- Evening, with excessive crying being more common in the evening or at night (8)
2. Enhance parenting skills: Let parents know it is okay to feel frustrated. Take a deep breath, count to 10, place your infant in a safe place and walk away for a few minutes to collect yourself. Many parents don’t know that this is okay to do (3).
3. Strengthen socioeconomic support: Make sure families are aware of and utilizing access to supportive services like WIC to help ease financial strain.
4. Emphasize social support and positive parenting: Ask about nearby help in the form of relatives or friends. Encourage them to reach out for emotional support, or even a break from caring for the infant. Connect families with community resources like motherhood support groups or playdates. Schedule for early childhood home visits (2).

Self Quiz
Ask yourself...
- Think about the populations you work with. How can you check in to make sure families have adequate support and decrease their risk of child abuse?
- What areas are the easiest to address at your current job? The most difficult?
Conclusion
Though the goal is for there to be no scenarios where children suffer head trauma at the hands of an abuser, there is a long way to go before that objective can be reached. In the meantime, healthcare professionals must be vigilant in maintaining a high level of suspicion for pediatric abusive head trauma whenever they are caring for children. Understanding contributing risk factors, as well as signs and symptoms, and how to properly assess for and diagnose pediatric abusive head trauma will lead to more accurate detection, appropriate treatment, and hopefully better outcomes. On the other end of things, those in a position to influence parenting education and community health standards should consider the ways in which caregiver frustration might be better handled to prevent the abuse from even occurring. There is much work to be done when it comes to AHT, but well informed medical professionals is an essential step in the right direction.
Health Equity is a rising area of focus in the healthcare field as renewed attention is being given to ongoing data regarding discrepancies and gaps in the accessibility, expanse, and quality of healthcare delivered across racial, gender, cultural, and other groups. Yes, there are some differences in healthcare outcomes purely based on biological differences between people of different genders or races, but more and more evidence points to the vast majority of healthcare gaps stemming from individual and systemic biases.
Policy change and restructuring is happening at an institutional level across the country, but this will only get us so far. In order for real change to occur and the gaps in healthcare to be closed, there must also be awareness and change on an individual level. Implicit, or subconscious, bias has the potential to change the way healthcare professionals deliver care in subtle but meaningful ways and must be addressed to modernize healthcare and reach true equity.
This Kentucky Implicit Bias training meets the “Implicit Bias” requirement needed for Kentucky nursing license renewal.
What is Implicit Bias?
So what is implicit bias and how is it affecting the way healthcare is delivered? Simply put, implicit bias is a subconscious attitude or opinion about a person or group of people that has the potential to influence the actions and decisions taken when providing care. This differs from explicit bias which is a conscious and controllable attitude (using racial slurs, making sexist comments, etc). Implicit bias is something that everyone has and may be largely unaware of how it is influencing their understanding of and actions towards others. The way we are raised, our unique life experiences, and an individual’s efforts to understand their own biases all affect the opinions and attitudes we have towards other people or groups (7). This Kentucky Implicit Bias training course will increase your awareness of implicit bias in your nursing practice.
This can be both a positive or a negative thing. For example if a patient’s loved ones tells you they are a nurse, you may immediately feel more connected to them and go above and beyond the expected care as a “professional courtesy.” This doesn’t mean you dislike your other patients and their loved ones, just that you feel more at ease with a fellow healthcare professional which shapes your thoughts and behaviors in a positive manner.
More often though, implicit biases have a negative connotation and can lead to care that is not as empathetic, holistic, or high quality as it should be. Common examples of implicit bias in healthcare include:
- Thinking elderly patients have lower cognitive or physical abilities
- Thinking women exaggerate their pain or have too many complaints
- Assuming patients who state they are sexually active are heterosexual
- Thinking Black patients delay seeking preventative or acute care because they are passive about their health
- Assuming a chatty college student is asking for ADHD evaluation because she is lazy and wants medication to make things easier
On a larger, more institutional and societal level, the effects of bias create barriers such as:
- Underrepresentation of minority races as providers: in 2018 56.2% of physicians were white, while only 5% were Black and 5.8% Hispanic (2)
- Crowded living conditions and food deserts for minority patients due to outdated zoning laws created during times of segregation (17).
- Difficulty obtaining health insurance for minority or even LGBTQ clients, decreasing access to healthcare (3).
- Lack of support and acceptance for LGBTQ people in the home, workplace, or school as well as lack of community resources leads to negative social and mental health outcomes.
- Due to variations in the way disabilities are assessed, the reported prevalence of disabilities ranges from 12% to 30% of the population (15).

Self Quiz
Ask yourself...
Before introducing the implications and long-term outcomes of unaddressed implicit biases in healthcare, reflect on your practice and the clients you work with. This will help as we progress through this Kentucky implicit bias training course.
- Think about the facility where you work and the different types of clients you come into contact with each day. Are there certain types of people you assume things about just based on the way they look, their gender, or their skin color?
- In what ways do you think these assumptions might affect the way you care for your clients, even if you keep these opinions internal?
- How do you think you could try and re-frame some of these assumptions?
- Do you think being more aware of your internal opinions will change your actions the next time you work?
- Before the Kentucky Implicit Bias Training course requirement, how often did you consider implict bias?
- Reflecting on your personal nursing practice, why do you think Kentucky has added a requirement on Kentucky Implict Bias training?
Implications
Once you have an understanding of what implicit bias is, you may be wondering what it looks like on a larger scale and what it means in terms of healthcare discrepancies. More and more data stacks up each year with examples that span all types of diversity, from race to gender, age, disabilities, religion, sexual identification and orientation, and even Veteran status. Examples of what subconscious biases in healthcare may look like include:
- Medical training and textbooks are mostly commonly centered around white patients, even though many rashes and conditions may look very different in patients with darker skin or different hair textures. This can lead to missed or delayed diagnoses and treatment for patients of color (9).
- A 2018 survey of LGBTQ youth revealed 80% reporting their provider assumed they were straight or did not ask (12). And in 2014, over half of gay men (56%) surveyed who had been to a doctor said they had never been recommended for HIV screening, despite increased risk for the disease (10).
- A 2010 study found that women were more verbose in their encounters with physicians and may not be able to fit all of their complaints into the designated appointment time, leading to a less accurate understanding of their symptoms by their doctor (4). For centuries, any symptoms or behaviors that women displayed (largely related to mental health) that male doctors could not diagnose fell under the umbrella of “hysteria”, a condition that was not removed from the DSM until 1980 (20).
- When treating elderly patients, providers may dismiss a treatable condition as part of aging, skip preventative screenings due to old age, or overtreat natural parts of aging as though they are a disease. Providers may be less patient, responsive, and empathetic to a patient’s concerns or even talk down to them or not explain things because they believe them to be cognitively impaired (18).
- Minority, particularly Black or Hispanic patients, are often thought to be less concerned or more neglectful of their health, but minority patients are also most often those living in poverty, which goes hand in hand with crowded living conditions and food deserts due to outdated zoning laws created during times of segregation. This means less access to nutritious foods, fresh air, or clean water which has overall negative effects on health (mude). Minority patients are also still disproportionately uninsured, which leads to delayed or no care when necessary (3).
Although these are only a few examples, there are obvious and substantial consequences of these biases; which is why it is vital that we address them in this Kentucky Implicit Bias training course.
This has obvious negative connotations or repercussions at the time of care and can lead to client dissatisfaction or suboptimal treatment and missed preventative care, but over time the effects of implicit bias can add up and lead to even larger consequences. Examples include:
- A 2020 study found that Black individuals over age 56 experience decline in memory, executive function, and global cognition at a rate much faster than their white peers, often as much as 4 years ahead in terms of cognitive decline. Data in this study attribute the difference to the cumulative effects of chronically high blood pressure more likely to be experienced and undertreated for Black Americans (16).
- Lack of health insurance keeps many minority patients from seeking care at all. 25% of Hispanic people are uninsured and 14% of Black people, compared to just 8.5% of white people. This leads to lack of preventative care and screenings, lack of management of chronic conditions, delayed or no treatment for acute conditions, and later diagnosis and poorer outcomes of life threatening conditions (3).
- A 2010 study showed men and women over age 65 were about equally likely to have visits with a primary care provider, but women were less likely to receive preventative care such as flu vaccines (75.4%) and cholesterol screening (87.3%) compared to men (77.3% and 88.8% respectively) (4).
- About 12.9% of school aged boys are diagnosed and treated for ADHD, compared to 5.6% of girls, though the actual rate of girls with the disorder is believed to be much higher (5).
- Teenagers and young adults who are part of the LGBTQ community are 4.5 times more likely to attempt suicide than straight, cis-gender peers (11).

Self Quiz
Ask yourself...
For the purpose of this Kentucky Implicit Bias training, put yourself in a patient’s perspective and reflect on the following:
- Have you ever been a patient and had a healthcare professional assume something about you without asking or getting the whole story? How did that make you feel?
- How do you think it might affect you over time if every healthcare encounter you had went the same way?
Impact of Historic Racism
In addition to discrepancies in insurance status, representation in medical textbooks, and representation among medical professionals, there is a long history of systemic racism that has created generational trauma for minority families, leading to mistrust in the healthcare system and poorer outcomes for those marginalized communities.
Possibly one of the most infamous examples is the Tuskegee Syphilis Study. This 1932 experiment included 600 Black men, about two thirds of which had syphilis, and involved collecting blood and monitoring the progression of symptoms for research purposes in exchange for free medical exams and meals. Informed consent was not collected and participants were given no information about the study other than that they were being “treated for bad blood”, even though no treatment was actually administered. By 1943, syphilis was routinely and effectively treated with penicillin, however the men involved in the study were not offered treatment and their progressively worsening symptoms continued to be monitored and studied until 1972 when it was deemed unethical. Once the study was stopped, participants were given reparations in the form of free medical benefits for the participants and their families. The last participant of the study lived until 2004 (6).
The “father of modern gynecology,” Dr. J. Marion Sims, is another example steeped in a complicated and racially unethical past. Though he did groundbreaking work on curing many gynecological complications of childbirth, most notably vesicovaginal fistulas, he did so by practicing on unconsenting, unanesthetized, Black enslaved women. The majority of his work was done between 1845 and 1849 when slavery was legal and these women were likely unable to refuse treatment, sometimes undergoing 20-30 surgeries while positioned on all fours and not given anything for pain. Historically his work has been criticized because he achieved so much recognition and fame through an uneven power dynamic with women who have largely remained unknown and unrecognized for their contributions to medical advancement (23).
Another example is the story of Henrietta Lacks, a young Black mother who died of cervical cancer in 1951. During the course of her treatment, a sample of cells was collected from her cervix by Dr. Gey, a prominent cancer researcher at the time. Up until this point, cells being utilized in Dr. Gey’s lab died after just a few weeks and new cells needed to be collected from other patients. Henrietta Lacks’ cells were unique and groundbreaking in that they were thriving and multiplying in the lab, growing new cells (nearly double) every 24 hours. These highly prolific cells were nicknamed HeLa Cells and have been used for decades in the development of many medical breakthroughs, including studies involving viruses, toxins, hormones, and other treatments on cancer cells and even playing a prominent role in vaccine development. All of this may sound wonderful, but it is important to understand that Henrietta Lacks never gave permission for these cells to be collected or studied and her family did not even know they existed or were the foundation for so much medical research until 20 years after her death. There have since been lawsuits to give family members control over what the cells are used for, as well as requiring recognition of Henrietta in published studies and financial payments from companies who profited off of the use of her cells (15).
When considering all of the above scenarios, the common theme is a lack of informed consent for Black patients and the lack of recognition for their invaluable role in society’s advancement to modern medicine. It only makes sense that these stories, and the many others that exist, have left many Black patients mistrustful of modern medicine, medical professionals, or treatments offered to them, particularly if the provider caring for them doesn’t look like them or seems dismissive or unknowledgeable about their unique concerns. Awareness that these types of events occurred and left a lasting impact on many generations of Black families is incredibly important in order for medical professionals to provide empathetic and racially sensitive care.

Self Quiz
Ask yourself...
Consider the above-mentioned historic events and reflect on the following:
- Have you ever had a negative experience at a healthcare facility? How has that experience impacted your view of that facility or your opinion when others talk about that facility?
- How would you feel if you learned that a sample of your cells or a bodily fluid was taken without your consent and had been used for medical experimentation? What about if companies had made huge profits from something taken from your body?
- Even without monetary compensation, why do you think recognition for a person’s role in healthcare advancement through the use of their own body is important?
Exploring Areas of Bias
Culture
Cultural competence is a common buzzword used in healthcare training programs and information about various religions, ethnicities, beliefs, or practices is often integrated into medical training. Students and staff members are often reminded that the highest quality of care anticipates the unique cultural needs a client may have and aims to provide care that is holistic and respectful of cultural differences. An awareness of the potential variances in care, such as dietary needs, desire for prayer or clergy members, rituals around birth or death, beliefs surrounding and even refusal for certain types of treatments, are all certainly very important for the culturally sensitive healthcare professional to have (and the distinctions far too many for the scope of this course); however, there is also a fine line between being aware of cultural similarities and stereotyping. Since this course is a required California Implicit Bias training, it is essential that this topic is covered.
Clinicians should make sure to understand that people hold different identities, beliefs, and practices across racial, ethnic, and religious groups. Remember that just because someone looks a certain way or identifies with a certain group does not mean all people within that group are the same. Holding assumptions about clients of a particular race or religion, without getting to know the individual needs of your client, is a form of implicit bias and may cause your client to become uncomfortable or offended.
Simply asking clients if they have any cultural, dietary, or spiritual needs throughout the course of their care is often the best way to learn their needs without making assumptions or stereotyping. Overall, it should be thought of as extending care beyond cultural competence and working on partnership and advocacy for your client’s unique needs.

Self Quiz
Ask yourself...
- Have you ever cared for a client that you made an assumption about based on appearances and it turned out not to be true?
- Did your behavior or attitude towards that client change at all once you gained new information about them?
- Think about ways you could incorporate cultural questions into your plan of care and how it could improve your understanding of client needs.
Maternal Health
One of the most strikingly obvious places that implicit bias has tainted the healthcare industry is in maternal health. Repeatedly, statistics show that Black women experience twice the infant mortality rate and nearly four times the maternal mortality rate of non-Hispanic white women during childbirth.
Let those numbers sink in and realize that this is a crisis. Pregnancy and childbirth are natural processes, but do come with inherent risks for mother and baby; but in a modern society, women should feel comfortable and confident in their care, not scared they won’t be treated properly or even survive. Home births among Black women are on the rise as they seek to avoid the biases of the hospital setting and maintain control over their own experiences (21).
The reasons for this disparity and Black women fearing for their lives when birthing in hospitals are many. This disparity exists regardless of socioeconomic class or education, indicating that a more insidious culprit, implicit bias, is hugely responsible (21). In order for true change to come, this topic must be addressed in this California Implicit Bias training. A few notes that indicate the prevalence of implicit bias in healthcare throughout history are listed below:
- False beliefs about biological differences between white and black women date back to slavery, including the belief that Black women have fewer nerve endings, thicker skin, and thicker bones and therefore do not feel pain as intensely.
- These beliefs are obviously untrue, but subconscious bias towards those beliefs still exists as Black and Hispanic women statistically have their perceived pain rated lower by health care professionals and are offered appropriate pain management interventions less often than white peers.
- Complaints from minority patients that may indicate red flags for conditions such as preeclampsia or hypertension are often downplayed or ignored by healthcare professionals.
- Studies show healthcare professionals may believe minority patients are less capable of adhering to or understanding treatment plans and may explain their care in a condescending tone of voice not used with other patients.
- One in five Black and Hispanic women report poor treatment during pregnancy and childbirth by healthcare staff.
- These patients are less likely to feel respected or like a partner in their care and may be non-compliant with treatment recommendations due to feeling this way, however this just perpetuates the attitudes held by the healthcare providers (21).

Self Quiz
Ask yourself...
- Think about how a provider’s perception of a maternity client’s pain could snowball throughout the labor and delivery process. How do you think it might affect the rate of c-sections or other birth interventions if clients have not had their pain properly managed throughout labor?
- Pregnancy is a very vulnerable time. Think about how you would feel if you were experiencing a pregnancy and had fears or concerns and your provider did not seem to validate or respect you. Would you feel comfortable going into birth? How might added fears or stress impact the experience?
Reproductive Rights
Branching off of maternal health is reproductive justice. Biases surrounding the reproductive decisions of women may negatively impact the care they receive when seeking care for contraception or during pregnancy. While some of these inequities may be more profound for women of color, women of all races can be and are affected by biases surrounding reproduction, which is why it is being covered in this California Implicit Bias training course. Examples of ways implicit bias may affect care include:
- Some healthcare professionals may believe there is a “right” time or way to become pregnant and feel pregnancy outside of those qualifiers is undesirable; this can stem from personal or religious beliefs. While healthcare staff are certainly entitled to hold these beliefs in their personal lives, if the resulting implicit biases are left unchecked, they can lead to attitudes and actions that are less compassionate when caring for their clients. Clients may feel shamed or judged during their experiences instead of having their needs addressed (8). Variables that may be perceived as unacceptable or less desirable include:
- Age during pregnancy. Clinicians may feel differently about pregnant clients who are very young (teenagers) or even those who are in their 40s or 50s (8).
- Marital status during pregnancy. Healthcare professionals may have beliefs that clients should be married when having children and may have a bias against unmarried or single clients (8).
- Number or spacing of pregnancies. Professionals may hold beliefs about how many pregnancies are acceptable or how far apart they should be and may hold judgment against clients with a large number of children or pregnancies occurring soon after childbirth.
- Low-income and minority women are more likely to report being counseled to limit the number of children they have, as opposed to their white peers (15).
- Method of conception. Some healthcare professionals may have personal beliefs about how children should be conceived and may have negative opinions about pregnancies resulting from fertility treatments such as IVF or surrogacy (8).
- Personal or religious beliefs about contraception may also cause healthcare professionals to provide less than optimal care to clients seeking methods of birth control.
- Providers may believe young or unmarried clients should not be given access to contraception because they do not believe they should be engaging in sexual activity (8).
- Providers, or even some institutions such as Catholic hospitals, may withhold contraception from clients as they believe it to be immoral to prevent pregnancy.
- Providers may push certain types or usage of contraception onto clients that they feel should limit the number of children they have, even if this does not align with the desires of the client. This includes the use of permanent contraception such as tubal ligation (15).
- Providers may provide biased information about the types of contraception available, minimizing side effects or pushing for easier, more effective types of contraception (such as IUDs), despite a client’s questions, concerns, or contraindications (15).
- One study showed Black and Hispanic women felt pressured to accept a certain type of contraception based on effectiveness alone, with little concern for their individual needs or reproductive goals (15).
- Personal or religious beliefs about pregnancy termination may impact the care provided and counsel given to pregnant clients who may wish to consider termination. Providers who disagree with abortion on a personal level may find it difficult to provide clear and unbiased information about all options available to pregnant clients or may have a judgmental or uncompassionate attitude when caring for clients who desire or have had an abortion (8).
Case Study
Alexandria is a 22-year-old Hispanic woman who has always wanted a big family with 3-5 children. She met her current boyfriend in college when she was 19 and became pregnant shortly afterward. It was an uneventful pregnancy, and Alexandria had a vaginal delivery to a healthy baby girl at 39 weeks. When that child turned 2, Alexandria and her partner decided they would like to have another baby.
At 38 weeks gestation, Alexandria was at a prenatal appointment when her provider brought up her plans for contraception after the birth. The provider suggested an IUD and stated it could be placed immediately after birth, could be left in for 5 years, and would be 99% effective at preventing pregnancy. Alexandria stated she had an IUD when she was 17 and did not like some of the side effects, mostly abdominal cramping, and that she also might like to have another baby before the 5-year mark.
Her doctor stated “All birth control has side effects, and this one is the most effective. You are so young, do you really want 3 children by age 25 anyway?”

Self Quiz
Ask yourself...
- What implicit biases does this healthcare professional hold about reproductive rights?
- How do you think those opinions are likely to affect Alexandria? Do you think she will change her mind or her future plans? Or do you think she will be more likely to disregard this provider’s advice and opinions moving forward?
- What are some potential negative consequences for Alexandria’s pregnancy prevention plans after this exchange with her doctor?
- Prior taking this Kentucky Implicit Bias course, were you aware of any implict biases regarding reproductive health?
How to Measure and Reduce Implicit Biases in Healthcare
Assessing for Bias
In order for change to occur, there is a broad spectrum of transitions in individual thought and policy that must occur. Evaluating for the presence, and the extent, of implicit bias is one of the first steps. This Kentucky Implicit Bias training will cover both individual and institutional level focuses.
On the individual level, possible action include:
- Identifying and exploring one’s own implicit biases. Everyone has them and we all need to reflect upon them. This goes beyond basic cultural competence and includes a deeper understanding of how your own experiences or environment may differ from someone else and may have caused you to feel or believe a certain way.
- Attending training or workshops provided by your job and completing exercises in self reflection will help you better understand where your biases are and the extent to which they may be impacting your behavior or actions at work and in your personal life.
- Reflecting on how one’s biases affect actions. Once you have recognized the internal opinions you hold, you can examine ways that those opinions may have been affecting your actions, behaviors, or attitudes towards others. Reflect on your care of patients at the end of each shift. Consider if you made assumptions about certain clients early on in their care. Think about ways those assumptions may have affected your interactions with the client. Think about if you cared for your clients in a way that you would want your own loved ones cared for.
- If you have the time, volunteer at events or in places that will expose you to people who are different from you. Use the opportunity to learn more about others, their lived experiences, and identify how often your implicit biases may be affecting your view of others before you even get to know them.
On an institutional level, the measurement of biases can be more streamlined and may utilize tools like surveys.
- Monitoring patient data and assessing for any broad gaps in diagnoses, preventative care and treatment rates, as well as health outcomes across racial, ethnic, gender, and other spectrums. Recognizing gaps or problem areas and assigning task forces to evaluate further and address the underlying issues.
- Regularly poll clients and employees of healthcare facilities to determine who might be experiencing effects of bias and when.
- Require employee participation in implicit bias presentations or courses, allowing employees to self identify areas where they may be biased.

Self Quiz
Ask yourself...
- In what ways will your approach be different the next time you care for a client unlike yourself?
- Can you think of a policy or practice that your facility could change in order to provide more equitable care to the clients you serve?
- Do you have a better understanding of implicit bias in healthcare after taking this Kentucky Implicit Bias course?
Acting to Reduce Bias
Once the presence and extent of bias has been identified, individuals can make small, consistent changes to recognize and address those biases in order to become more self aware and intentional in their actions. Some possible ways to address and reduce implicit bias on an individual level include:
- Educating oneself and reframing biases. In order to change patterns of thinking and subsequent behaviors that may negatively impact others, you can work on broadening your views on various topics. This can be done through reading about the experiences of others, watching informational videos or documentaries, attending speaking engagements, and just listening to the experiences of others and gaining an understanding of how their lives might be different than yours.
- Understanding and celebrating differences. Once you can learn to see others for their differences and consider how you can adapt your care to help them achieve the best outcomes for their wellbeing, you are able to provide truly equitable care to your clients. This includes understanding differences in experiences, perceptions, cultures, languages, and realities for people different from yourself, recognizing when disparities are occurring, and advocating for change and equity.
When enough people have recognized and addressed their own implicit biases, advocacy can extend beyond individual care of clients and reach the institutional level where change is more easily seen (though no more important than the small individual changes). One of the most effective ways to make institutional level changes is through representation of minority groups in positions of power and decision making. Simply keeping structures as they are and dictating change without any evolution from leadership is not likely to be effective in the long term. Including minority professionals in positions of leadership or on decision making panels has the most potential to make true and meaningful change for hospitals and healthcare facilities.
Examples of institutional level changes include:
- Medical schools will need to take a broader, more inclusive approach when admitting future doctors, incentivise minority students to choose careers in healthcare, and invest in their retention and success (9).
- Properly training and integrating professionals like midwives and doulas into routine antenatal care and investing in practices like group visits and home births will give power back to minority women while still giving them safe choices during pregnancy (1).
- Universal health insurance, basic housing regulations, access to grocery stores, and many other socio-political changes can also work towards closing the gaps in accessibility to quality healthcare and may vary by geographic location (3).
- Community programs should be available to create safe spaces for connection and acceptance for LGBTQ people. Laws and school policy need to focus on how to prevent and react to bullying and violence against LGBTQ individuals (12).
- Cultural competence training in medical professions needs to include LGBTQ issues and data collection regarding this population needs to increase and be recognized as a medical necessity (12).
- Medical professionals must be trained in the history of inequality among women, particularly in regards to mental health, and proper, modern diagnostics must be used. The differences in communication styles of men and women should be taught as well (20).
- Medical facilities should emphasize respect of a client’s views on controversial topics such as pregnancy/birth, death, and acceptance or declining of treatments even if it conflicts with a staff members’ own beliefs (14).
- Healthcare facilities can adopt practices that are standardized regardless of age and include anti-ageism and geriatric focused training, including training about elder abuse (18).
Obviously each geographic area will have differing demographics depending on the populations they serve. What works at one facility may not work at another. Hearing from the community is beneficial for keeping things individualized and allows facilities to gain perspective from the local groups they serve.
- Town Hall style meetings, keeping hospital board members and employees local rather than outsourcing from travel companies (when possible), and encouraging community involvement from staff members are all great ways to keep a community centered facility and keep the lines of communication open for clients who may be having a different experience than their neighbor.
There are many things that will need to be done in order for equitable, bias-free healthcare to become a norm nationwide. However, taking the time to learn from this Kentucky Implicit Bias training, apply it to current practices, and continue to learn about others and their respective beliefs and cultures is just the beginning.
Suicide risks among nurses is a public health concern. The first and most profound way to address the troubling rates of suicide among nurses is to employ suicide prevention. For that matter, mandatory training, resources, and the establishment of policies and procedures are crucial within the operation of organizations. All healthcare providers are responsible for identifying and addressing situations which warrant intervention.
This Kentucky Suicide Prevention course meets the “Suicide Prevention” requirement needed for Kentucky nursing license renewal.
Introduction
According to the Centers for Disease Control and Prevention, suicide is a leading cause of death in the United States, which is subsequently a public health concern (6). As underscored by the CDC (6), “In 2018, suicide took more than 48,000 lives and was the 10th leading cause of death in the United States”. Yet, it has been noted that suicidal ideations and attempts occur more often than suicidal deaths (17). However, suicide is preventable and from a collaborative approach, preventive strategies can help reduce an individual’s risk for a detrimental outcome (6). Some of the warning signs of suicide include, but are not limited to, the following: feeling hopeless or helpless; feeling like a burden to others or unable to find a reason for living; unbearable pain; expressing thoughts of suicide; exhibiting signs of depression or loss of interest in normal activities; aggression, impulsivity, or humiliation; or displaying a sudden sense of peace (4). From a public health standpoint, all ages are affected by suicide (6). Nevertheless, there are higher suicide rates in some groups (e.g., non-Hispanic American/Alaska Native; non-Hispanic White populations; veterans; persons residing in rural areas; individuals who identify as lesbian, gay, or bisexual; and individuals holding certain occupations often considered high stress such as healthcare providers) in comparison to others (6). As stated, individuals requiring intervention are often those with high stressors and/or have a history of other acts of violence (6). One of the most demanding professions is nursing, and nurses are deemed at a higher risk for suicide than the general population. Taking that into account, suicide awareness and prevention programs are fundamental. This Kentucky Suicide Prevention course will increase your awareness among nurses at risk for suicide and provide tools for screening and preventative measures.
The Significance of Suicide Prevention
As emphasized, suicide is a public health concern due to the nature of its adverse impact on not only the individual, but their loved ones and communities correspondingly (6). Factors such as socioeconomical issues, interpersonal problems, mental or physical health problems, substance abuse, previous suicidal attempts, occupational demands/workplace stressors, and being able to access deadly means may contribute to individuals being at a higher risk for suicide (6). Anxiety, stress disorders, and depression are all increased by the demands of the responsibilities related to the nursing profession, and sadly, those factors are interrelated to higher suicide rates among nurses (7). In saying that, nurses who work on the frontlines are heavily burdened, which is why it is so critical that support is rendered with the goal of yielding a reduction in the risks of suicide. There are many strategies that can be implemented to protect individuals from suicidal thoughts and behavior. Some of those protective factors include the following: coping and problem-solving skills; cultural and religious believes that dissuade suicide; support from friends, family, and communities; supportive affiliations with care providers; access to physical and mental health care; and restricted access to fatal means among persons at risk for suicide (6).

Self Quiz
Ask yourself...
Reflect on your prior knowledge of what you knew about suicide prior to taking this Kentucky Suicide Prevention course.
- What are contributing factors that may increase an individual’s risk for suicide?
- What are protective factors to consider regarding suicide prevention?
- How would you rate your current knowledge for identifying suicide risk factors?
- What resources are available at your workplace for those experiencing burnout of feelings of suicide?
- Why do you think Kentucky has added a CE requirement on Kentucky Suicide Prevention ?
Suicide Risk Factors Amongst the Nursing Population
With suicide prevention being a public health concern, it is important to identify groups of persons considered at substantial risk for suicide. Nurses are often faced with high demands of responsibilities as well as easy access to fatal means. Primarily, workplace stressors and lack of personal care can lead to burnout which consequently can lead to an increased risk for suicide incidences in the nursing population. Burnout has been noted as one of the most common reasons nurses contemplate suicide, and circumstances such as short-staffing and the most recent pandemic (COVID-19) have brought about a wave of burnout among nurses who work on the front line (11). Nurses are often responsible for the care of all others (professionally and personally) while unintentionally neglecting their own needs; therefore, providing support for nurses is imperative. For example, there have been fifty-eight suicides amongst the nursing population in the state of Kentucky since 2016; however, nurses in the state of Kentucky are required to obtain recurring suicide prevention education and training (15). Hence why the Kentucky Board of Nursing has added a continuing education requirement to address suicide prevention in nursing. Furthermore, Kentucky nurses can obtain additional education on identifying signs of burnout and ways to reduce stress by viewing a suicide prevention video and engaging in a program developed by the Kentucky Nurses Action Coalition in collaboration via the support of the Kentucky Nurses Association (15).
As previously emphasized in this Kentucky Suicide Prevention course, in comparison to the general population, there is notably a higher risk of suicide amongst nurses (both females and males) (8). There are many suicide risk factors among nurses, but the following are some of the most evident: exposure to frequent trauma and death; working long, consecutive shifts; workplace bullying; neglecting self- care; social isolation or seclusion; and access to as well as knowledge of, lethal substances, such as opioids (5). Case in point, it has been proven that female nurses often opt for pharmacological poisoning (e.g., opioids and benzodiazepines) as a method to complete suicide, whereas their male counterparts utilize firearms in the same nature as the general population (8). Nurses are unlikely to seek mental health assistance in comparison to the general population due to some of the following reasons: concerns with how their careers could potentially be impacted; uncertainties regarding confidentiality; conflicts with taking time off to attend appointments as well as inability to obtain appointments; and fear of potential consequences associated with their professional licenses in the form of reprisals (11). For optimal outcomes, strategies to address suicide risks must aim to properly identify and address those exhibiting signs of burnout and depression as well as to reduce stigma and other barriers to seeking treatment (11). Next we will explore strategies to address suicide risk factors as required by the Kentucky Board of Nursing in this Kentucky Suicide Prevention course.

Self Quiz
Ask yourself...
- What are workplace concerns that you have witnessed or encountered which are associated with burnout?
- What are ways to assess for suicide risk factors in nurses?
- Have you known a nurse or heard of a nurse that committed suicide?
- Are there any specific suicide risk screening tools utilized by your organization?
- Are you aware of the resources available for suicide awareness?
Strategies to Address Suicide Risks
Mental health promotion is one of the most critical strategies to help decrease incidences of suicide in the nursing population (2). Upon identifying individuals and/or groups at risk for suicide, it is important to derive pathways for proper intervention. The negative stigma associated with the treatment of mental illnesses is a well-known barrier for those in need of help, especially professionals such as nurses who are obliged to taking care of others, and this stigma prevents individuals from seeking treatment when they lack any type of support system. Organizations can better support individuals who are at risk for suicide by assuring that suicide training and screening tools for suicide risk are available to all employees, making every other member in one’s organization part of their support network. In fact, there are three primary initiative-taking strategies recommended by the Suicide Prevention Resource Center (SPRC) for organizations to implement and those strategies include establishing a respectful, inclusive work environment; identifying employees at risk for suicide; and formulating a responsive plan to enforce (12). Vitally, there should be identifying and reporting methods available for nurses to be screened anonymously (2). For example, individuals enduring a crisis can text “HOME” to 741741 to communicate with a crisis counselor (15). Another example of an anonymous suicide prevention resource is the HEAR (Healer Education Assessment and Referral) screening program (2). The HEAR program is purposed for screening, assessing, and referring nurses at risk for suicide as well as providing education pertaining to mental health, and likewise, it is aimed at removing the stigma associated with the reluctancy in seeking mental health assistance (16). In addition, managers and leaders are equipped with the knowledge necessary for providing support to their staff which, in turn, leads to healthier ways for alleviating stress and avoiding burnout (16). Essentially, organizations must convey the message to their employees that it is okay to seek assistance for mental health concerns as their well-being is priority. This can also be achieved by offering resources such as Employee Assistance Programs or displaying information for crisis hotlines (e.g., National Suicide Prevention Lifeline, Safe Call Now, Disaster Distress Helpline, or the Crisis Text Line) for individuals who are experiencing depression and/or those afflicted by suicidal thoughts/ideations (2). Trainings and in-services are also necessities.
Oftentimes, an individual may require the assistance of a peer (whether a colleague or a friend) when faced with a crisis (2). Nurses should be educated and aware of suicide prevention strategies which include assessing for risk factors, inquiring about plans (ask direct questions) as well as means, monitoring behavior, and collaboratively creating a safety plan (13). Specifically, some of the strategies recommended to prevent suicide include the following: reinforce economic supports; strengthen access and delivery of suicide care; generate protective environments; encourage connectedness; teach coping and critical thinking skills; identify and support people at risk; and reduce harms and prevent future risk (6). Though suicide prevention strategies may not be 100 percent effective in stopping an individual from executing a plan, peers need to know how to identify signs of suicide risk to properly support their colleagues in obtaining appropriate mental health assistance (2). Besides, the American Foundation for Suicide provides an abundance of suicide prevention resources (3). In essence, suicide awareness and prevention are vital.

Self Quiz
Ask yourself...
- What do you feel would be a vital strategy for assessing for signs of burnout and suicide risks in a colleague?
- Do you believe that suicide awareness education is impactful for suicide prevention?
- Does your organization utilize any specific tools to assess for suicide risk?
- Would you feel comfortable addressing a suicidal colleague?
- Does your employer take mental health concerns seriously?
- Have you had to connect patients or others with suicide programs?
- Were you previously aware of resources such as the HEAR program?
Additional Interventions and Protective Factors to Reduce Suicide Rates
Though assessing and safety planning are crucial in caring for nurses at risk for suicide, it is also important that appropriate referrals and follow-up interventions are implemented. As previously indicated in this Kentucky Suicide Prevention course, the HEAR program is an anonymous program that was designed to assess and refer individuals at risk for suicide. The program interactively screens the individual, categorizes the responses into tiers, then proactively provides options for counseling either online, via telephone, or in-person, and/or referrals are submitted to community providers for continuity in treatment (1). This method is remarkable for nurses who are reluctant to seek help because of the fear of having one’s career and reputation jeopardized, as their organizational safety net does what is supposed to do – recognize and report. What is also more noteworthy is that the HEAR team can be contacted for assistance by employees who have identified colleagues who are at risk (1). Correspondingly, organizations can replicate the HEAR program at their facilities by either modifying their Employee Assistance Programs to incorporate the HEAR service, establishing contracts with local or virtual mental health agencies, or by imitating the program by means of staffing provisions (1). Still, organizations can elicit protection to employees at risk by promoting safety and wellness as well as encouraging teamwork and providing support (18). Similarly, it is important that other preventive and/or protective factors are explored to achieve a reduction in suicide rates. For that matter, Hutton (2015) listed the following as preventive or protective factors for individuals at risk for suicide: “Reasons for living, perceived meaning in life, adaptive beliefs; Social support and feeling connected that may include religious affiliation; Being married, and for women, being pregnant, having children; Restricted access to firearms; Moral objection to suicide; Engaged in treatment or having access to mental or physical health care; Resilience, coping skills; Fear of social disapproval; and Cognitive flexibility”. In the same aspect, following up with an individual at risk is another intervention that can assist in prevention and protection. In this regard, one major advantage of the HEAR program is its unique outreach approach which entails counselors following up with the individual to assist him/her in seeking emergent care or to help the affected individual obtain an appointment for mental health treatment/counseling in a timely manner (10).

Self Quiz
Ask yourself...
Think about your current practice.
- Are there guidelines in place for dealing with patients or colleagues who are suicidal?
- Are debriefings held after stressful incidents?
- What type of resources does your organization have in place to address burnout and suicide prevention?
- Can you think of someone right now who may be exhibiting signs of suicidal thoughts or actions?
Ethical and Legal Considerations Regarding Care for Suicidal Individuals
As formerly stated, no intervention is 100% certain to prevent an individual from executing a suicidal plan, but with training and resources to help recognize and support, the resulting interventions have proven to be positively impactful in many cases. However, when providing care for suicidal individuals, ethical and legal considerations should be prioritized.
For one’s protection as well as the protection of the individual and the organization, the following legal considerations are notable when caring for persons who are at risk for suicide: become familiar with suicide policies and procedures for your organization; gain awareness regarding state laws associated with advanced directives, involuntary commitment, seclusion and restraint; familiarize yourself with HIPAA regulations and exceptions regarding confidentiality; and if dealing with a patient, document all action in his/her health record (13).
Also, if one is assisting a colleague, organizational protocol should be followed. As a nurse professional, it is crucial that one follows policies, procedures, and protocol to avoid breaching patient confidentiality as well as potentially being sued for negligence or malpractice. It is equally important to consider ethical responsibilities when dealing with individuals at risk or suicide. A nurse can reference the professional Code of Ethics as a guide for dealing with ethical concerns or he/she can consult with an ethics committee. Regarding ethical responsibilities, one should display these key attributes: be respectful and compassionate, serve as an advocate, promote health and safety, encourage autonomy, maintain confidentiality, refrain from conflict of interests, participate in collaborative care, engage in research to remain cognizant of evidence-based practices, and address ethical issues (9).

Self Quiz
Ask yourself...
- Are you competent in assessing and intervening when dealing with an individual who is at risk for suicide?
- What do you believe is the best approach for making sure individuals at risk for suicide receive appropriate care and follow-up?
- What are ethical considerations to be mindful of when dealing with patients or colleagues at risk for suicide?
- What are legal considerations to reflect on when dealing with individuals who are at risk for suicide?
- Do you feel more aware and confident in identifying suicide risk factors and resources for fellow nurse colleagues and patients?
Case Study
A 24-year-old novice nurse has been noted to have discrepancies in the narcotic counts of her medication cart on a few occasions. Moreover, it has also been observed by other colleagues that the nurse is often truant, and her mood is very unpredictable. She has episodes of extreme euphoria, and she has become overly generous (i.e., offering a necklace that she inherited from her late mother to a colleague). Even more so, an incident report was recently completed regarding her miscalculation of a critical medication dosage. Although the nurse’s error reflected in the incident report was a “Near Miss,” the nurse’s recent behavioral changes warrant the need for immediate intervention. Regrettably, this error has caused the nurse to feel even more overwhelmed and emotionally detached. All the above occurrences have resulted in her feeling emotionally unstable to the point of her expressing suicidal thoughts and ideations. A colleague who has established rapport with the nurse makes herself available to listen, she asks the nurse direct questions, and she provides encouragement to the nurse as well as supportive resources (i.e., phone numbers for the Employee Assistance Program, the National Suicide Prevention Lifeline, and the Crisis Text Line). What are other strategies that might be valuable to the nurse’s prognosis?
Recommendations
All nurses and healthcare professionals in the same respect should engage in continuing education which addresses suicide prevention. Principally, it takes a collaborative approach to provide individualized and organizational support to a nurse/colleague in crisis. For best results, there should be programs in place and resources available which promote suicide awareness, highlight protocol, and offer ongoing support. Ultimately, the goal of promoting mental health and wellness for nurses is to reduce the likelihood of suicide.
What is Domestic Violence?
Domestic violence is a pattern of abusive behaviors that is utilized by one individual within the relationship to gain and maintain control and power over the other individual(s) in a relationship. Domestic violence can include but is not limited to any of the following: sexual, physical, economical, psychological/emotional, and technological (16).
For reference, the Kentucky statute defines domestic violence as: “Physical injury, serious physical injury, stalking, sexual assault, strangulation, assault, or the infliction of fear of imminent physical injury, serious physical injury, sexual assault, strangulation, or assault between family members or members of an unmarried couple” (16).
The relationship of those involved is not always romantic in nature, as it can be between parents and children, friends, roommates, family, and other individuals that live together in the same household (16).
In recent years, domestic violence has taken on a new name: intimate partner violence. While intimate partner violence is used for those experiencing abuse in an intimate/romantic relationship, some individuals use the terms interchangeably. It is important to note the definitions of each term to clearly understand that while the two can overlap they are not the same (11).
To provide a clear picture, here is an example of domestic violence and intimate partner violence:
- Example of Domestic Violence: a 20-year-old male named Sam lives with his 21-year-old roommate Danny. Danny has physically abused Sam by hitting, kicking, and slapping him often. Danny and Sam are not in a romantic/intimate relationship, and they share their apartment with one other person who is attending the same university as them.
- Example of intimate partner violence: Shelly is a 27-year-old who is in a relationship with her 35-year-old boyfriend Marcus. Marcus often forces Shelly to perform sexual acts she does not want to do as well as control her through threats and acts of physical harm. Shelly does not live with Marcus, but she often finds him always around.
If Danny and Sam had been in an intimate/romantic relationship, the abuse could have been classified as intimate partner violence or domestic violence. If Shelly had been living with Marcus the term domestic violence could have been used; however, since they are not, the term intimate partner violence is more appropriate.
Domestic violence can also incorporate elder abuse and child abuse if the victim resides in the household (16).
For child abuse, the age range is from newborn to age 17 and encompasses a recent act or a failure to act as a parent or caretaker, that results in serious physical or emotional harm, exploitation, sexual assault/abuse, or death or an act or failure to act that can lead to an imminent risk of severe harm (9). Age-related considerations will be discussed later in this course. With elder abuse, the victim must be 65 years of age or older and can be carried out the same way as domestic violence (53).
As mentioned, domestic violence, intimate partner violence, elder abuse, or child abuse can occur in a variety of ways. While there is no full comprehensive list, there are many behaviors that the abuser may utilize to ensure the compliance of the victim (Table 1).
| Sexual | Physical | Economical | Psychological/ Emotional | Technological |
| Definition: Coercion or attempt to coerce any type of sexual contact, act, or behavior without the consent of the victim.
|
Definition: Intentional acts that lead to physical injury.
|
Definition: Limiting or controlling an individual’s ability to earn, use, or manage financial resources. | Definition: Threatening fear of harm as well as undercutting an individual’s sense of worth or self-esteem. | Definition: Any act done with the intention to threaten, harass, control, harm, stalk, impersonate, monitor, or exploit another individual that occurs by utilizing technology. |
| Examples: Rape (including marital rape); forcing sexual acts after violence has happened; treating the victim in a sexually demeaning manner; attacking sexual parts of the body. | Examples: Shoving, hitting, biting, slapping, hair pulling, burning; strangulation; forcing the victim to consume alcohol and/or drugs, denying medical care or assistance to the victim. | Examples: Using methods of coercion, manipulation, or fraud to limit an individual’s access to assets, money, credit/financial information; exploiting powers of attorney or guardianship; or neglecting to act in the individual’s best interest. | Examples: intimidation that leads to fear, threats of physical harm to victim, abuser, children, and family; forcing isolation; and destruction of property. Name-calling, constant criticism, damaging relationships with family and/or friends, threatening to take children. | Examples: Invading online spaces such as public and private social media sites; using cameras, computers, phones, and location tracking devices. |
| Sources: (3, 59, 60) | ||||
Case Study:
Nora and Keith were both born overseas with Nora currently living in the United States. Keith lives overseas and has completed tertiary education. English is Nora’s second language, but she does require an interpreter to assist her for anything other than basic communication. Keith works in a well-paid, professional job.
The two initially met through an online dating website and agreed to meet in the United States where Keith came for a vacation. The relationship progressed quicker than Nora expected. She was willing to assist Keith in obtaining a tourist visa for Keith and within a few weeks of the visa going through they got married. During the sixth month of marriage, Nora became pregnant.
Since their marriage, Keith has changed. Nora is not allowed to leave the house without Keith’s knowledge of where she is going, what she is doing, who she is with, and when she will be home. If she is not home on time, Keith becomes angry and yells at her. He tells her “You’re stupid and can’t remember anything!” Demeaning names are often used in the household and Keith once told Nora she’d never be able to hold a job and is useless. He insists he is the only one who does anything around the house while working a full-time job. He makes it hard for her to access an interpreter when they are conducting financial business, insisting that he will “take care of it” and that she “doesn’t need to worry about that.” Once he took her phone because he didn’t think it was a good idea to use when pregnant.
At one of her obstetric appointments, Keith was not present due to being at work, Nora admitted to the nurse that she felt worried for herself and her unborn child. She wonders if she could continue helping Keith become a United States citizen, but she quickly brushes that idea away. “He’s just worried about the baby,” she says. “He’s never hit me, so it’s not abuse.”

Self Quiz
Ask yourself...
- Based on the case study do you think Nora is a victim of domestic violence? If so what type or types of abuse could Nora be experiencing?
- Do you agree with Nora’s assessment that what Keith is doing is not considered abuse?
- What could you say to Nora in response to her statement?
- What would be the best way to explain to Nora what the definitions of abuse are? How would you ensure she receives information in her preferred language?
- Do you think you are obligated to call the police in this particular case?
Etiology and Pathophysiology
Etiology: Domestic violence, including child and elder abuse, and intimate partner violence begins because of the abuser’s desire for domination or control of the victim.
Reasons abusers may have the need to control vary, and while this is not a complete list, it does highlight the many reasons why someone may become an abuser in a relationship (8):
- Individual:
- Jealous
- Young age
- Learned behavior from a home where domestic violence occurred or was viewed as acceptable.
- Lack of nonviolent social problem-solving skills
- Low self-esteem
- Anger management or aggressive behavior especially in youth
- Personality or psychological disorders such as antisocial or borderline personality disorder traits
- Alcohol and/or drug use (those who are impaired have a more challenging time controlling urges)
- Low academic success
- Impulsiveness or poor behavior control
- Depression and suicide attempts
- Support/belief of firm gender roles such as male dominance or hostility toward women
- History of being physically abusive
- Relationship:
- Desire for dominance or control in the relationship or the partner
- Unhealthy family dynamics or relationships
- Financial stress
- Witnessing violence, physical discipline, or poor parenting during childhood
- Association with antisocial or aggressive peers
- Parents with less than a high school degree
- Community:
- High poverty, unemployment, and crime/violence rates
- Limited education and economic opportunities
- Low comradery among the community such as not looking out for each other or intervening during a situation
- Society:
- Traditional gender roles and inequality
- Supporting aggression toward others
- Income inequality
Pathophysiology: Research on domestic violence is not definitive when it comes to the pathological findings in perpetrators, there have been several reoccurring characteristics that are common (8):
- Jealous, possessive, or paranoid
- Controlling every activity such as finances and social events
- Low self-esteem
- High consumption of alcohol and/or drugs
- Emotional dependence is present more often in the abuser but can be present in the victim as well.
Case Study
Dominic started off as a nice guy, that’s how Cara always described him. He was always dotting on her and her younger sister Chloe despite Chloe being nine. Most of Cara’s other boyfriends wouldn’t have found Chloe interesting, nor would they want to date her after they found out Cara was given custody of Chloe since their parents passed away. Dominic had been different, in more ways than one.
After a year of dating, Dominic began pushing boundaries in their relationship. If Cara didn’t want to have sex and Dominic did, she ended up giving in despite not wanting to. They fought more than they ever had and after having one of these fights in front of a few friends, there was talk of breaking up. Dominic didn’t like that and promised to change.
For a while, things were okay. They collaborated with a therapist to help them talk through disagreements and they were able to work together. However, Dominic became jealous of Cara when she got a job promotion and promptly started a fight with her when she went to his home that evening. He had been in the same position at work for years and was taught from a young age that women were expected to stay home and care for the children.
Cara ended up breaking up with Dominic a few days later and moving to a new apartment with Chole when her lease was up for renewal.

Self Quiz
Ask yourself...
- What about Dominic’s story would lead you to believe he could be an abuser?
- What other information would you want to know regarding his past history?
- Do you think Cara could have handled the situation differently? If so, what do you think she should have done?
- Would you classify this situation as domestic violence or intimate partner violence? What information made you pick one over the other?
The Cycle of Abuse Model
The cycle of abuse is a four-phase wheel that depicts how abuse continues within a relationship (Image 1).
Phase One: Building Tension
In the first stage of the abuse cycle, tension is created and grows. This type of tension can be caused by anything: family, work, financial concerns, catastrophic events, minor to major illnesses, or conflict. These types of stressors are common in everyday life and a majority of individuals are able to cope with them in a healthy manner. Abusers use the stressor(s) as an excuse and as a justification for their actions (19).
Some victims of abuse are likely to try and placate the abuser as a means of avoiding the phase of violence that often follows. They may try to act more submissive or “stay out of the way” or even try and be more helpful to please the abuser. Other victims may do the opposite, provoking the abuser to act and become violent. They are essentially trying to “get it over with” (19).
Phase Two: Incident
The incident phase is where the act of abuse occurs. This can range from physical, psychological/emotional, or verbal abuse and occur in any of the ways listed in Table 1 (please note Table 1 is not a comprehensive list) (19).
As discussed earlier, domestic violence and intimate partner violence are the abuser’s way of gaining and maintaining control and power over the victim. The entire abuse cycle is the abuser’s way of doing that; however, the incident phase is when the abuser is more dangerous and frightening to the victim (19).
Phase Three: Reconciliation
This phase of the cycle is where the abuser may make excuses for the behavior. They may apologize as a way to earn sympathy from the victim: “work has been stressful” or “my mother recently had a stroke, and I don’t know how we will care for her.” Other abusers will blame the victim for their behavior with statements like “don’t make me angry and I won’t have to do this.” Denying the event occurred can be another act the abuser does during the reconciliation phase: “that never happened” (19).
The term gaslighting can be used during the phase and is defined as the attempt of the abuse to create confusion or self-doubt by distorting reality and making the victim question their own intuition, judgment, or memory (40).
Phase Four: Calm
The final stage of the cycle is the calm phase. Often referred to as the “honeymoon phase,” this part of the abuse cycle consists of a period of normality or even better than what life was before the abuse occurred (19).
Love-bombing, defined as an individual manipulating another individual through the act of going above and beyond, may occur as the abuser attempts to “make up for” their actions. This, however, is false as the abuser’s goal is to keep the victim in the relationship and unaware (10).
The cycle remains a cycle because the relationship does not stay in the “calm phase” and instead leads to tension building once again. The cycle will repeat through the relationship with various periods of time between calm and tension building. As the relationship progresses, the time between calm and tension building shortens. This could be attributed to the abuser realizing they can “get away with” their actions since the victim did not leave them or has returned to the relationship/abuser (13).
Breaking the cycle can be extremely difficult for victims. The victim may be ashamed to admit they are a victim of abuse. They may also experience fear due to the violent nature of their abuser; when faced with leaving, the abuser may retaliate and take drastic measures to ensure that the victim does not leave. This can consist of severe physical, mental, or financial abuse. Some acts done by abusers can result in death. Some victims think the abuse is their fault or that they deserve it (13).
Love is a large factor in staying within the cycle. Those who are victims may be or think they are in love with their abuser and that they can “save” the abuser by “fixing them.”
Accepting the abuse as part of an otherwise “good” relationship is another reason why victims may not leave. Other reasons for staying in the relationship can include (19):
- Religion or family pressure
- Lack of financial means
- Lack of knowledge of available services or support network
- Losing children
- Cultural, race, or gender barriers
A Note: Healthcare providers should keep in mind that the abuse cycle model is a simplified version of the complex problem of domestic violence or intimate partner violence. It is important for healthcare providers to not victim blame those in the cycle of abuse; those in the cycle may not see the patterns that those removed from the situation can and may experience denial. Time, distance from the situation, and a different perspective from the situation are often needed for the victim to realize they are or were in the cycle.
Case Study
Nicole presents to her primary care physician’s office for a routine medical exam. Nicole is 20 years old, unemployed, and has a cat at home. Recently, Nicole has decided to move in with her girlfriend Iris but is hesitant to do so. When prompted to discuss it further, Nicole states that her girlfriend “doesn’t understand personal space, but only when she’s at home.”
Iris comes from a conservative family with traditional values. She has not told her family about her relationship with Nicole, presenting Nicole as a “friend that needs a place to stay for a while.” Despite understanding the situation, Nicole says she feels hurt by this since Iris has admitted to telling her family about other girlfriends in the past.
Nicole admits to bringing this up with Iris after they’d been drinking one night. Iris got mad and hit Nicole in the face, possibly breaking her nose. Nicole was too scared to go to the hospital and was admitted Iris said her nose “looked better” and “wasn’t as crooked as before.”
After the fight, Iris seemed like a different person. She showered Nicole and her cat with gifts, making promises about how things would change and that she would introduce Nicole to her family as her girlfriend soon. Things seemed to be okay for a while and Nicole started looking for jobs. She could tell Iris was frustrated with her lack of “trying” to contribute to the household. However, when Nicole was offered a position, Iris yelled and her and guilted her into not accepting the job.

Self Quiz
Ask yourself...
- Would you classify the scenario described above as part of the abuse cycle? What stages of the cycle were you able to identify?
- What other information as a provider would you want to know from Nicole?
- What if Iris had been in the room with Nicole, do you think she would have told as much information as she did? What would you have expected to happen instead when asked about domestic violence or intimate partner violence if Iris had been in the room?
- As a healthcare provider, how can you create a safe environment for your patients and help them recognize the abuse cycle?
- What resources could you provide to patients about the abuse cycle to assist them in understanding how it can appear?
Those at Risk
While anyone can be at risk for domestic violence or intimate partner violence, there are groups that are at a higher risk.
Children:
The year 2015 produced nearly four million reports of alleged maltreatment to the child protective agencies in the United States. Of that nearly four million, 683,000 children were officially reported to have been maltreated, abuse being second to neglect. Children from birth to the age of three had the highest rate of being victims with 27.7%. This is important to note because infants and young toddlers rely heavily on parents or caregivers to provide them with food, water, hygiene, interaction, and affection. All of which are vital to proper growth and development. Child victims were slightly more female than male at 50.9% which is consistent with adult statistics as females predominantly being the victim (46).
Data on children exposed to abuse varies as there is no national survey that is dedicated to focusing on children and their exposure to domestic violence. However, there are a few statistics that continue to be cited throughout literature. It is estimated that there is between 3.3 million to 10 million children are exposed to severe parental violence annually in the United States. The research for these statistics varied in collection methods, but one study produced interesting results. Approximately 12.6% of adults who were asked to reflect on their teenage years reported that there had been some type of abuse in the house: 50% reported their father hitting their mother, 19% reported their mother hitting their father, and 31% reported both parents hitting each other (46).
More recent data supports this research. A study conducted by Dong et al. in 2004 discussed adverse childhood experiences with 8,600 adults. Of those that participated 24% stated they had been exposed to child abuse before the age of 18. In this study, the abuser was often the father or stepfather abusing the mother or stepmother. 550 college students were evaluated in another study that showed 41.1% of females and 32.3% of males witnessing abuse as children (46).
While these statistics are staggering, it is important to note that these numbers are only an estimate and can be assumed to be higher or lower based on reporting rates, definitions of domestic violence (physical as well as psychological/emotional, sexual), and time ranges that the surveyor sets (lifetime versus a specific period in time) (46).
Sexual abuse is another concern that regards children and can be a form of domestic violence. Statistics show that one in four girls and one in 13 boys will experience some form of sexual abuse during childhood, and often the perpetrator is someone the child or family knows. More often than not, this type of abuse is carried out by a parent or stepparent, sibling or stepsibling, or other relative who lives in the home. In contrast to teenage or adult victims of sexual assault, child victims are usually brought to a healthcare provider after injury to the genitalia is noted or signs of a sexually transmitted infection are present (2).
While some sexually transmitted infections are transmitted from mother to infant during the delivery phase and can remain present for some time after birth, there is a general rule that any sexually transmitted infection diagnosis after the neonatal phase is considered as evidence of sexual abuse. Care should be taken when collecting specimens and conducting assessments on children to minimize pain and physical and/or psychological trauma (7).
When determining if a patient should be evaluated for sexual assault, healthcare providers should consider if the patient has a recent, evidence of a recent, or healed penetrative injury to the genitals, anus, or oropharynx. A child could present with signs and symptoms such as pain in the genital region, bleeding, tearing, or bruising. If the child or parent/caregiver reports or suspects that the abuse, sexual or physical, was caused by a stranger is another reason to err on the side of caution and consider a sexually transmitted infection screening (45).
If the perpetrator is known to have a high chance of or is infected with a sexually transmitted infection. This can include members of the household that the child lives with. Children with signs and symptoms of sexually transmitted infections such as genital itching and/or odor, vaginal discharge and/or pain, genital legions ulcers, or other urinary symptoms they should be evaluated. If a parent or child requests sexually transmitted infection testing or if the child cannot verbalize the assault that occurred, the provider should consider it (7).
Tests for sexually transmitted infections should have high specificity due to the nature of the situation. Treatment should wait until all samples have been obtained to prevent false results. Healthcare providers should discuss and collaborate with trained professionals on how to ensure testing and treatment is appropriately carried out. Recommendation for Human Papillomavirus vaccinations are encouraged for children with a history of sexual abuse over the age of nine due to the increased risk of unsafe sexual practices in the future. Human immunodeficiency virus testing may be indicated based on the assailant’s history and circumstances of the abuse (7).
Children may also be victims of domestic violence through Munchausen by Proxy where the caregiver or parent exaggerates or fabricates physical or mental health disorders the child has or does not have; Munchausen itself involves the individual, not someone else. The motivation for this is to gain sympathy and attention from family, friends, and others within the community (21).
Young Adults/Adolescents:
Defined as the ages of 13 to 17, adolescent years are more prone to intimate partner violence than domestic violence as opposed to younger children due to the start of dating; however, domestic violence can co-occur with intimate partner violence. Data shows that 1.5 million United States high school students are the victim of physical violence annually. Of the 1.5 million, only 33% discussed abuse with anyone, meaning only 500,000 adolescents are reporting it. When looking into reasons why this may be, as an addition to all the reasons discussed previously, 81% of parents do not believe that teen dating violence is a concern, or they are unaware that it is an issue. Adolescents may not be willing to share with their parents or caregivers due to fear of not being believed or taken seriously (17).
Technology and social media applications can be unmonitored areas of abuse that family and friends are unaware of. Technology abuse was mentioned earlier in this course, but healthcare providers should be aware of how it can appear. Victims of technology abuse may report that someone they are interacting with or dating is forcing them to share passwords or locations, change information on their profiles, and participate in activities online that can be interpreted as humiliating. There may be comments about posts on social media that are seen as jealous; private photos may be leaked, or the abuser may threaten to leak them (48).
Sexual abuse might be harder to diagnose in the adolescent population. This age range is often associated with risky behaviors such as sexual behaviors and using illicit drugs. Healthcare providers should ensure they are screening adolescents thoroughly when they present to any healthcare facility for treatment regarding suspicious injuries or complaints. They may present with serious changes in emotion—anger, low self-esteem, cries for no reason, withdrawal or scared, confusion about sexual orientation—changes in the way they dress, participation in harmful sexual behavior or using alcohol and/or drugs, or avoiding activities they used to enjoy. Physical symptoms may include swelling or redness in the genital area, difficulty walking or sitting, pain or burning when using the restroom, penile or vaginal discharge, or bruising on the buttocks or thighs (45).
Elders:
Elder abuse consists of financial, sexual, emotional, and physical abuse as well as abandonment and neglect. More often than not, elder abuse occurs in the home of the victim which could be classified as domestic violence if they live together. The abuser in the situation is someone the victim has trust with as they are often in charge of many aspects of the victim’s life. The abuse can consist of children, grandchildren, other family members, friends, or other caregivers; studies show that 76.1% of abusers are a member of the victim’s family (30).
It is estimated that four million older Americans are victims of some form of elder abuse annually. Those who require assistance with activities of daily living have an increased risk of emotional abuse or financial exploitation, over 13% of those have suffered emotional abuse since the age of 60. Emotional abuse can be done through the act of demeaning comments about how the victim is “useless” or “helpless” or “weak.” These comments can be seen as embarrassing or humiliating. Since individuals who require assistance to carry out daily tasks may not be able to leave the house often, financial exploitation can be easy for an abuser to carry out. Those who are victims of financial exploitation lost approximately $2.9 billion in the year 2011 (30).
Most sexual abuse cases with elderly patients consist of female victims and male abusers, with only 15.5% of cases being reported to the police. This could be due to fear, cognitive deterioration—50% of older adults diagnosed with dementia are mistreated or abused in some way—or any other reason discussed previously in this course (30).
Women:
On a national level, one in four women have experienced physical violence in their lifetime—often carried out by an intimate partner while one in seven have been injured by an intimate partner. The most abused women fall in the age range of 18 to 24 years old (36). As 18 years old is when most go to college or university or move out of the family home, this age range may not be surprising to some healthcare providers.
For every seven women, one woman states that she was stalked to the point she feared for the safety of herself and/or her family, worrying she or they would be harmed or killed; 19.3 million women have reported being stalked in their lifetime (55). As covered earlier, stalking can be via technology or in-person, depending on the situation and the abuser involved. It is important to remember that intimate partner violence covers past partners or spouses. Data shows that 60.8% of women who have been the victim of stalking report that the stalker was a former or current intimate partner (36).
The number of women who have been a victim of severe physical violence such as strangulation, burning, beating, etc. in their lifetime is one in four. The same number (one in four) consists of those who have experienced severe intimate partner violence. This type of violence contains any of the following: sexual violence and/or intimate partner stalking that can include injury, use of victim services, post-traumatic stress disorder, sexually transmitted infections, or other effects. On average, three women are killed daily as a result of current or previous intimate partners (36).
One in five women have been raped during their lifetime while one in ten women have been raped by an intimate partner, but rape is not the only part of sexual abuse that women can face. In addition to unwanted touching, kissing, and sexual acts, women can also be the victim of reproductive coercion. This type of sexual assault involves the sabotage of contraception medications or forcing a partner to use them, intentionally expose a partner to sexually transmitted infections or human immunodeficiency virus, refusing to practice safe sex, controlling pregnancy through forcing the woman to continue the pregnancy or terminating it through an abortion, refusing sterilization, or controlling the victim’s access to reproductive health care (36).
Data shows that 20% of the women who seek care in family clinics and had a history of abuse reported that they experienced pregnancy coercion and 15% of them had some form of birth control sabotage. Women who were diagnosed with a sexually transmitted infection were hesitant to notify their partner of the diagnosis for fear of the abuser denying they were infected or that the woman had been cheating. Those who did discuss their diagnosis reported threats of harm or experienced actual harm as a result (36).
Domestic violence or intimate partner violence with pregnancy occurs in approximately 342,000 women annually in the United States. Women who experience domestic violence or intimate partner violence are more likely to not receive prenatal care, or they are waiting longer to seek out care than what is medically recommended. Depression in the postnatal period for those who are victims of abuse is three times more common than those not experiencing abuse in the home. Women may also experience a higher risk of perinatal death; a three time increase from those not experiencing abuse (55).
It is important for healthcare providers to understand that pregnancy may increase or decrease the amount of abuse experienced by a woman. Each situation varies, but one study showed that abuse peaked during the first trimester and tapered off after that in women who recently experienced abuse. Women who did not have a recent history of abuse did not experience it throughout the pregnancy. This same study noted that psychological and sexual abuse rates were high within the first month postpartum (39).
Domestic violence or intimate partner violence can affect the fetus as well. There is a higher risk of low birth weights, fetal injury, early placenta separation, infection, hemorrhage, and preterm birth (27). After birth, infants can display signs of trauma that include feeding problems, high irritability, sleep disturbances, and delays in development. One good thing is that these can be alleviated with a secure relationship with a safe caregiver (39).
Men:
Men as victims of domestic violence or intimate partner violence is a growing topic in society and data varies. Research states that one in nine men experience severe physical violence at the hands of an intimate partner while one in 25 reports being injured by an intimate partner. Those who have been a victim of severe physical violence such as burning, strangulation, beating, etc. is one in seven men. Of males who experienced any form of domestic violence or intimate partner violence or stalking, 97% reported the abuser was female (6).
Five million males in the United States report being the victims of stalking in their lifetime. It is stated that 43.5% of men who reported stalking stated that a current or former intimate partner was stalking them. Of the data collected, 46% of males were stalked by only female perpetrators, 43% were stalked by male perpetrators only, and 8% were stalked by both male and female perpetrators (6).
Sexual violence data for male victims starts with one in four men having experienced some form of it in their lifetime; one in 14 were forced to penetrate someone—sexually penetrating someone without the other individual’s consent as a result of intoxication, unconsciousness, incapacitation—within their lifetime. Victims of rape, completed or attempted, consisted of one in 38 men with 71% of them experiencing this prior to the age of 25 (6).
Of those that were victims of complete or attempted rape, 87% reported only male perpetrators, 79% reported only female perpetrators, sexual coercion was done by female perpetrators as reported by 82% of victims, unwanted sexual contact was reported at 53%, and done by female perpetrators only, and 48% of non-contact unwanted sexual experiences—such as unsolicited photos—were done by male perpetrators (6).
The data collected and reported is important in healthcare due to the seriousness of the situation. As covered previously in this course, gender roles and society’s expectations of how individuals are expected to act based on their gender can lead to a lack of support or recognition within a certain community. It is the job of the healthcare provider to assess all patients they come in contact with and never make assumptions based on appearances. As this section has shown, males can very well be the victims of domestic violence or intimate partner violence (6).

People of Color:
Rates of domestic violence or intimate partner violence are higher among people of color. In the 2010 National Intimate Partner and Sexual Violence Survey, those who identified as Native American/Alaska Native and non-Hispanic Black females reported rates of lifetime abuse at 46% and 43.7% respectively. This was in comparison to non-Hispanic White women’s 34.6% and Hispanic women who had a reported percentage of 37.1 (51)
Intimate partner violence was one of the leading causes of death among Black women. Nearly 50% of Indigenous Americans report that they have been “beaten, raped, or stalked by an intimate partner” while over 50% of Asian women have reported physical and/or sexual violence by an intimate partner during their lifetime (26).
Data on males presented challenging to find. Statistics show that 38.6% of African-American men report domestic violence or intimate partner violence (58).
There are many reasons for the increased statistics among people of color. Discrimination is still prevalent, leading to financial hardships, unemployment, and lack of insurance. This may cause the victim to rely on the abuser for economic support. Oppression may lead people of color to distrust the justice system. They may also be fearful of ending up abused by the system. Stereotypes that depict men and women of color in certain light can lead to conflict between the victim and their depicted “culture.” Women and men may not want to be viewed as weak for being a victim of domestic violence when society depicts them as strong or reinforcing the negative stereotypes about their partners (26).
Religion and spirituality can have certain views on relationships and separation or divorce. Religious leaders may be held in high esteem and be viewed as the only person a couple should go to in order to solve relationship issues (26).
Individuals Classified as Immigrants and Refugees:
Those born outside of the United States have a higher chance of domestic violence or intimate partner violence than other people of color physically born in the United States. One study revealed that 48% of Latinas reported violence from their intimate partners increased after immigration to the United States. Study results ranged from 24% to 60% of women who have immigrated from Asia. Asian immigrant women are at a higher risk for homicide when compared to American-born Asians (47).
Abusers may utilize the legal system to ensure control and hold power over the victim. Legal documents such as passports or identification cards might be taken or destroyed, legal paperwork may not be properly filled out or submitted, or threats of deportation may occur. If the victim has a culture that could be different from the country they are in, there may be some cultural barriers that they are unable to overcome because of the abuser. Victims may not be permitted to learn English (or the primary language of the country they are in) or be prohibited from speaking their native language. The abuser may accuse the victim of abandoning the community, they may use racial slurs against the victim, or they might deny the victim from working or obtaining an education (15).
Domestic violence or intimate partner violence can occur for many reasons within the immigrant or refugee community. Language barriers, difficulty understanding legal rights, and stress in adaptation to a new set of cultural/societal norms can be contributing factors to people of color becoming a victim. Women are at a higher risk due to poverty, disparities in social resources between her and her partner, immigration status, and social isolation (15).
Immigrants or refugees may not be aware that victims of crime, regardless of citizen or immigration status, are entitled to access law enforcement services or the courts. They can receive assistance from government and non-government agencies that can include safety planning, counseling, interpreters, emergency housing, and potentially financial assistance (15).
When services are offered to these individuals they should be focused on the specific and unique needs of the victim. Services are not “one size fits all” and should be tailored to the needs of the victim such as shelters that address specific cultural needs, legal assistance maintaining immigration status or child custody, and access to other victim-specific services (15).
Those that are considered refugees or displaced individuals can experience the same hardships as immigrants. Data about refugees or displaced women who are living in the most forgotten and underfunded locations state that 73% of women reported an increase in domestic violence, a 51% increase in sexual violence, and a 32% growth in early and forced marriage within the first ten months of the COVID-19 pandemic (22).
Members of the LGBTQIA+ Community:
Overall, awareness of domestic violence and intimate partner violence has primarily focused on heterosexual individuals, leaving the members of the LGBTQIA+ community to be underrepresented in the conversations. In recent years, there has been a shift, focusing on all individuals, and data is being collected to provide an accurate picture of how domestic violence and intimate partner violence impacts everyone (35).
Data shows that 43.8% of women who identify as lesbian and 61.1% of women who identify as bisexual have experienced some form of physical violence, rape, and/or stalking by an intimate partner in their lifetime. In comparison, 35% of heterosexual women reported the same experiences (35).
Discussing gay and bisexual men, 26% and 37.7% respectively, reported physical violence, rape, and/or stalking by an intimate partner as opposed to heterosexual males at 29%. Of those who are in male same-sex relationships, 26% reported calling the police for assistance for near-lethal violence (35).
Less than 5% of members within the LGBTQIA+ community sought out orders of protection after experiencing domestic violence or intimate partner violence. The type of violence experienced by this community ranges from physical violence at 20%, threats and intimidation at 16%, verbal harassment at 15%, and sexual violence at 4%. Of the intimate violence cases reported in 2015, 11% of them involved a weapon (35).
White members of the LGBTQIA+ community are more likely to experience sexual violence while Black/African American members of the LGBTQIA+ community are more likely to experience physical violence at the hands of an intimate partner. Transgender victims are more likely to experience acts of domestic violence or intimate partner violence in public spaces as opposed to those who do not identify as transgender. Those who identify as bisexual have higher risks of sexual abuse, and anyone in the LGBTQIA+ community who is on public assistance is more likely to be a victim of domestic violence or intimate partner violence (35).
Members of the LGBTQIA+ community face unique challenges as it pertains to domestic violence or intimate partner violence. Some members of the community do not share their sexual orientation with others and the threat of “outing” could be used as a method of psychological/emotional abuse. This could also be a barrier to seeking help. Those who have experienced hate crimes or have been a victim of physical or psychological abuse in the past may be less willing to request assistance (35).
Other reasons for not seeking services include fear that bringing attention to the problem will set back equality in the LGBTQIA+ community; domestic violence shelters are sometimes listed as “female or male only” and transgender individuals may not be allowed in; healthcare providers may not be trained in assessing and managing LGBTQIA+ domestic violence or intimate partner violence concerns; fear of or experiencing homophobia/transphobia when reporting; low confidence with the legal system as depicted by media or personal experience; and society believes that domestic violence or intimate partner violence does not occur in the LGBTQIA+ community (35).
Individuals in the Military:
The number of active-duty members of the United States military is over 1.3 million individuals with 16% of that number being women. The spouses of those active-duty members consist of an additional 600,000 members; approximately 25% of them are under the age of 25 years old. Data that was collected showed that in the 2018 fiscal year, there were 16,912 reports of domestic violence or intimate partner violence; almost half of those reports (8,039) did meet the criteria for abuse under definitions created by the Department of Defense. Of those 8,039 cases 73.7% were classified as physical abuse, 22.6% were emotional abuse, 3.6% were sexual abuse, and 0.06% were domestic violence (12).
Comparing data to previous years, events that meet criteria based on the Department of Defense’s definitions have not changed much since the 2009 fiscal year. Reporting has fluctuated due to changes in the number of service members during any given time as well as the addition of sexual abuse reports increasing due to the inclusion of it in the Department of Defense’s definitions for domestic violence or intimate partner violence in the 2009 fiscal year (12).
Nearly 50% of those who reported domestic violence and 66% of those who reported intimate partner violence to the Department of Defense were members of the military when the abuse took place. The 2018 fiscal year resulted in 15 deaths caused by domestic violence or intimate partner violence, 13 being spouses and 2 being intimate partners. Three victims who died as a result of this violence had reported the abuse to the Department of Defense while four of the abusers had previous reports of at least one episode of abuse already on their record. Nine of the abusers were actually civilians acting against military victims (12).
Abusers within military relationships are likely to be underreported, especially if the victim is a civilian, they are not married to the abuser, or they do not live in the military space. Those who are not married to the service member cannot get treatment inside military hospitals or other treatment facilities. Coordination between civilian and military officials for reporting domestic violence or intimate partner violence can be challenging and lead to underreporting (12).
As discussed previously, intimate partner violence can begin in adolescents, leading to the increased risk of future events of violence later on. Those who report sexual violence, domestic violence or intimate partner violence, or stalking do so by the age of 25: 71% of them are females and 58% of them are males. As a note, 23% of women reported their experience occurred by the age of 18. Domestic abuse was prominent in junior enlisted military couples (classified as E-3 and lower), ranging in age from 18 to 24. The 2018 fiscal year showed that 15.1 per 1,000 married couples experienced domestic violence, compared to the overall domestic violence rate of 5 per 1,000 married couples (12).
Data comparing civilian to military populations shows that those within the military sector have lower rates of domestic violence or intimate partner violence overall. Over the lifetime 20% of civilian women and 13.7% of active-duty women report sexual violence; 56.7% of civilian women and 47.2% of active-duty women experience psychological aggression; and 26.9% of civilian women and 21.9% of active-duty women experience severe physical violence. The active-duty women were deployed within three years of the report (12).
Those with Cognitive and/or Physical Disabilities:
Disability is an all-encompassing word to describe individuals with a physical or mental impairment that leads to activity limitation and how they are able to participate in society. This could be termed as participation restrictions. Types of disabilities and how they affect the individual can vary, ranging from mild, to moderate, and severe in terms of how limited they are in terms of participation.
The list below is not all-encompassing but it does highlight some of the more common impairments (5).
- Physical Impairments:
- Visual
- Movement
- Hearing
- Mental Impairments:
- Thinking
- Learning
- Communication
- Social Relationship
- Remembering
These disabilities can present at birth as a result of genetics or the mother’s exposure to something during pregnancy. They can also develop later on in life and present in the form of traumatic brain injuries, illicit substance use, or progressive medical diagnoses (5).
In comparison to women without disabilities, women with disabilities have a 40% greater risk of being victims of violence; these women are at a concerning risk for severe violence. The primary abuser of women with disabilities is their male partners. Sexual abuse is reported to be around 80% of women with disabilities; this is three times more than women without disabilities. A single study reported that 47% of women with disabilities had been sexually abused on more than 10 different occasions (31). Overall, those with disabilities are three times more likely to be sexually abused, and 19% of rapes or sexual abuse were reported to police in comparison to the 36% reported by those without a disability (42).
While those with a disability account for 12% of the population, 26% of the victims of nonfatal violent crimes had a disability. Those with cognitive disabilities had the highest rates of victimization at a rate of 83.3 per 1,000 individuals. Law enforcement responded to 90% of the reports made by victims without disabilities as opposed to the 77% of reports that they responded to as it pertains to victims with disabilities (29). This can lead to mistrust in the justice system that keeps victims from initially reporting the events or seeking assistance in the future. Several studies seem to suggest this view as between 70% to 85% of abuse cases against those with disabilities are not reported. Another study noted that only 5% of crimes committed against those with disabilities were prosecuted; 70% of crimes committed against individuals without disabilities were prosecuted (29).
Those with disabilities face challenges when it comes to leaving domestic violence or intimate partner violence situations. Those providing shelter services may not be trained in disability awareness, studies report approximately 35% have this type of training. Sixteen percent of shelters have an individual dedicated to providing services to women with disabilities. Some individuals may see violence as a way to manage those with disabilities and blame the victim for the abuse, justifying the abuse (42).
Individuals with Mental Illness:
Similar to those diagnosed with disabilities, those who have a severe mental illness—a psychotic disorder such a schizophrenia, schizoaffective disorder, depressive disorder with psychotic symptoms, or bipolar; or being under the case of secondary mental health services—are more likely to be victims of domestic violence or intimate partner violence. Data is limited, but there is some information regarding domestic violence and sexual abuse. A range of 15% to 22% of women diagnosed with a severe mental illness reported recent domestic violence while men had a range of 4% to 10%. Another study produced similar results: 27% for women and 13% for men. Regarding sexual abuse, women had a 9.9% prevalence in the first study and a 10% in the second. Sexual abuse in men was only reported in the first study with a value of 3.1%. One interesting data point is that sexual abuse in adulthood leads to a 53% increase in suicide attempts among women (25).
Studies also showed that those at the highest risk for physical violence were young males with severe mental illness. As they get older, become employed, and live independently or have a family with responsibilities the risk decreases. Some theorize that not having societal roles for those with severe mental illness can cause them to become victims of domestic violence or intimate partner violence as a method to provide for themselves (25).
As highlighted in other groups, those with mental illness can have a difficult time reporting and leaving an abusive or violent situation. As is with those with disabilities, a diagnosis of a severe mental illness may be seen as less credible when giving reports to law enforcement. Others may accuse the victim of being the abuser due to their diagnosis—media often portrays those with mental illness as dangerous, violent individuals because of stigma. Feelings of hopelessness, low self-esteem, increased symptoms of the mental illness can all be causes of stigma and domestic violence or intimate partner violence (25).
Substance use disorders are prominent in those diagnosed with mental illness. More than one in four individuals with a serious mental illness—depression, anxiety, schizophrenia, and personality disorders—also have a substance use disorder. As discussed earlier in this course, substance use can increase an individual’s susceptibility to becoming an abuser, as well as making an individual a victim due to impairment (52).
Individuals Without a Home (Homeless):
For women and children, domestic violence or intimate partner violence is a major cause of homelessness in many communities. It is reported that between 22% to 57% of women who were experiencing homelessness directly attributed domestic violence as the cause for their homelessness. Thirty-eight percent of all domestic violence victims will become homeless at some point; victims may often experience multiple periods of homelessness due to them leaving and returning to the abuser several times before finally escaping the abuser for good. Of women experiencing homelessness, 90% report that they have been sexually abused or have been severely physically abused in their lifetime (37).
The major concern for those experiencing homelessness is safety rating at 85% while finding affordable housing is the second concern rating at 80%. An average stay in an emergency shelter is 60 days, but it takes approximately six to 10 months to secure affordable housing. Only 30 affordable rental units are available for every 100 extremely low income, meaning shelter stays are longer and other victims may be turned away due to a lack of space. These victims who cannot gain access to a shelter may return to their abuser to avoid living on the streets. The 2010 fiscal year revealed that 172,000 requests for shelter were unable to be met due to max capacity (37).
Victims might be evicted or denied housing due to records of domestic violence, regardless of the individual being the victim. Some landlords may not want to risk having violence taken upon them, their families, or their properties by providing housing to the victim. Other landlords have a “zero tolerance” rule when it comes to crime, and they will evict those involved in the crime of violence if it occurs. A Michigan study revealed that women who were victims of domestic violence or intimate partner violence were more likely to be evicted than other women. This can lead to victims failing to report their situation to law enforcement for fear of eviction. A study showed that 65% of test applicants—those seeking housing on behalf of a victim of domestic violence or intimate partner violence—were denied housing or were offered lease terms and conditions that were highly unfavorable in comparison to non-victim applicants (1).
Low-Income:
Individuals who rely on others for financial stability are at a higher risk for domestic violence or intimate partner violence. The lack of financial stability limits the victim’s choice and the ability to escape a violent situation or relationship (49). Women with an income of less than $75,000 are seven times more likely to experience domestic violence than women who have an income over $75,000. Hosing and the neighborhoods that individuals live in can be a contributing factor to domestic violence or intimate partner violence. Women who rent housing can experience intimate partner violence at a rate of three times the amount than women who own their own home. Interestingly, women living in poor neighborhoods and having financial hardship are twice as likely to be victims of domestic violence or intimate partner violence as opposed to women who live in affluent neighborhoods but still have financial hardship (28).
Data suggests that domestic violence or intimate partner violence and finances are related: loss of employment or income can lead to increased stress, both of which have been identified as causes of domestic violence. Difficulty maintaining work can be a contributing factor as well, or relying on part-time, low-paying jobs—as over 70% of low-income parents do now have a high school degree—adds to stress and income instability (28).
Domestic violence or intimate partner violence situations may not lead to unemployment; however, it can be a significant barrier. Physical abuse can lead to missed workdays due to injury, psychological or emotional abuse can lead to poor work performance or severe anxiety, and technology abuse can affect communication with coworkers or management. This creates a cycle that is hard to break; victims may lose jobs due to the increased number of barriers preventing them from working. This can force them to rely on welfare or other assistance programs or their abuser (28).
Individuals Living in Rural Communities:
According to the United States Department of Agriculture the definition of a rural community that has a population density of less than 500 individuals per square mile in open countryside and places with a population of less than 2,500 individuals (54). These locations are significant distances from urban areas and can be an unanticipated place where domestic violence or intimate partner violence can occur (44).
One study evaluated the number of reports of intimate partner violence against women in both small rural and isolated areas—22% and 17.9% respectively—in comparison to women who lived in urban areas at 15.5%. Higher cases of physical abuse were reported among women living in rural settings. This study also evaluated the distance from the rural areas and the closest intimate partner violence program(s) which reported it was three times greater than in urban areas. These services served more counties and limited on-site services or shelters. At least 25% of women in rural or isolated areas live over 40 miles from the nearest program. Less than 1% of women in urban areas are over 40 miles from a domestic violence or intimate partner violence program (44).
As reflected on in this section, many of the individuals listed considered high-risk overlap in categories. Victims are more than male or female, adult, or child, hetero or homosexual. They are more than an individual with or without a disability or mental illness. They are those with and without financial stability. They live in a variety of neighborhoods, cities, and states. It is important that healthcare providers be aware that anyone can be a victim of domestic violence or intimate partner violence—regardless of how minor or severe the abuse is—and assumptions and judgments should be disregarded. Providers should be prepared to assess all patients that come in contact with and be ready to provide assistance and/or resources based on the patient’s needs and wants (44).

Self Quiz
Ask yourself...
- Out of all the listed individuals at risk, which one surprised you the most? Why did it surprise you?
- Based on the data provided, do you think what is reported is accurate, higher, or lower in terms of domestic violence cases?
- In your area of work what populations at risk do you encounter more?
- What at risk population do you think faces the most challenges when being a victim of domestic violence? Why do you think that?
Assessing for Domestic Violence
Healthcare organizations have different ways of assessing for domestic violence or intimate partner violence and it is important that providers are aware of their facility’s specific procedures. If no specific screening tool is utilized, healthcare providers may make the decision to implement one of many available (50).
Written questions can be one method of assessment that can be utilized in the waiting room setting and save time on the provider’s end; however, it is important to follow up with the patient regardless of the answer. Many victims will check “no” or be forced to check “no” by the abuser. The healthcare provider should make a verbal statement addressing the “no” and seek reassurance with the answer. A clear statement that could be used is as follows: “I see that you selected “no” to the question regarding domestic violence or intimate partner violence. I want to ensure you do not have any questions about this issue.” If the patient once again answers “no” the provider can reassure that if that were to change, during the visit or in the future, the provider and facility is a safe place to discuss the situation and receive help (50).
The provider should be asking this question in private with the patient as the abuser may be the one who is present with the patient. Finding a way to get the abuser to step out of the room can be challenging. Implementing organizational policies that require providers to have a set time when they discuss healthcare concerns with the patients can be a way to mitigate this, but it is not guaranteed (50).
It is recommended that written assessment forms are kept and signed by the healthcare provider, incorporated into the patient’s permanent medical record, and a provider note added that domestic violence or intimate partner violence was verbally discussed with the patient to ensure that a “yes” is not overlooked (50).
Oral questions are the second method for assessing domestic violence or intimate partner violence. This method does take more time, but sometimes this process can allow patients and providers to ease into the topic.
Providers can start with broad questions such as (50):
- “How are things going at home/work/school?”
- “What is the stress level like?”
- “How are you feeling about your relationships? How is your partner treating you? Are there any problems?”
Patients may wonder why their healthcare provider is asking these questions. They may feel like these are invasive or wonder why it is important to their appointment.
If these concerns are brought up, providers can use that opportunity to shed light on how common domestic violence or intimate partner violence is (50).
- “Since violence is very common in society and can effect health, I ask all of my patients about this.”
- “Many of my patients are experiencing abusive relationships. Some of them may be too scared to bring up the topic themselves, so I have started asking about it to every patient I interact with.”
The other method is to ask direct questions about domestic violence or intimate partner violence.
One set of direct questions is the SAFE Questions adapted from Ashur M. (50):
Stress/Safety
- What stresses do you experience in your relationships?
- Do you feel safe in your relationship?
Afraid/Abused
- 3) People in relationships sometimes fight. What happens when you and your partner disagree?
- Have there been situations in your relationship where you have felt afraid?
- Have you been physically hurt or threatened by your partner?
- Has your partner forced you to engage in sexual activities you didn’t want?
Friends/Family
- Are your friends and family aware of what is going on?
Emergency
- Do you have a safe place to go in an emergency?

Other direct questions can be created based on policy, situation, patient, or age level. Below is a list of questions that can be utilized with young adult and adult patients (50):
- Are you afraid of your partner? Do you feel you are in danger?
- Do you feel safe at home?
- All couples fight, what are fights like at home? Do these fights become physical?
- You have mentioned that your partner has a problem with drinking/drugs/temper/managing stress. When that happens, does your partner ever hurt you?
- Since we last saw each other have you been hit/kicked/punched/etc. or scared?
- Is there anyone in the home that has tried or successfully hit/kicked/etc. or injured you since I last saw you?
- What kind of experiences, if any, have you experienced in your lifetime?
- Do you ever feel controlled or isolated as a result of your partner? This can be in your work life, finances, or relationships.
- Does your partner try to control you through threats of hurting you or your family?
- Has anyone you live with threatened to hurt you or your family?
- Have you ever been slapped, shoved, or pushed by your partner or someone you live with?
- Have you ever been kicked, hurt, or threatened by your partner or someone you live with?
- Have you ever been touched in a way that made you feel uncomfortable?
- Have you ever been made to participate in something sexual despite not wanting to? Regardless of if you said “no” or not.
- Has your partner refused to practice safe sex when you requested it?
- Have you been with your partner and had an episode or episodes of blacking out or not remembering what happened?
- Are you afraid to go home? If so, is there somewhere safe you can go?
- Do you have a safe person you can rely on?
- Have you ever contacted a crisis hotline in the past?
- If so, do you have a contact person there?
- If not, why not?
- Do you know the local and national crisis center hotline numbers?
- Do you know the numbers of a few emergency shelters?
There are many other tools providers can use to assess for aspects of domestic violence or intimate partner violence. One is titled the Danger Assessment and is separated into two parts. The first part is a calendar for victims to document the frequency and severity of the abuse. This can be useful for victims who may be in denial or are trying to minimize the actions of the abuser. The second part of the tool is a set of 20 yes/no questions that are scored to determine the risk for intimate partner homicide (18).
The MOSAIC questions assess how the victim’s situation is similar to other situations that escalated in severity. This method does require a confidential account, but once an account is made and the questions have been answered, a report is created rating the situation on a scale of one to 10. This tool has been utilized by the police employed in determining threats against members of the United States Supreme Court, Congress, and House of Representatives (18).
For children, the Adverse Childhood Experiences quiz allows the individual proving the quiz to score the various types of hallmark signs of abuse, neglect, and rough childhood. The higher the score on the test, the greater the risk was for that child to develop negative outcomes as it pertains to behavior, health, and opportunities later in life (18).
Since stalking is a major topic when it comes to domestic violence the Stalking and Harassment Assessment and Riks Profile is an option for those who are worried they may be a victim of stalking. This test is similar to the MOSAIC in that it requires a confidential account to be made and requires those to answer some questions via an assessment. This assessment takes approximately 15 minutes to complete, and results are generated shortly after, summarizing the situation, and providing the victim with suggestions on how to improve their safety. This assessment is consistent with legal definitions of stalking and was developed with attorneys, law enforcement, victim advocates, prosecutors, and prominent organizations like the Stalking Resource Center (18).
The last tool to be discussed is the Ontario Domestic Assault Risk Assessment. This assessment is done on the abuser, comparing them to other perpetrators. This makes a determination of how likely the abuser is to assault the victim again. There are 13 items on this assessment, and they have a score between zero and one. The result is the total score of all questions, making a maximum number of 13, which is converted into a percentage that estimates the likelihood of abusing the victim again (18).
It is important for healthcare providers to approach this subject after assessing the situation to determine the best way to do so. Trust is very fragile, and it may take several attempts for a victim to feel comfortable enough to speak on the subject. Some may never do so, but asking at every visit or interaction can let the victim know help is available, they are not alone, and they are cared for.
Barriers for Disclosure:
While victims of domestic violence or intimate partner violence can present to any healthcare office or facility, many of them end up in the nearest emergency department. Regardless of where the healthcare provider encounters the victim, they need to be aware of how to assess for domestic violence or intimate partner violence (20).
One major part of the assessment process is the barriers to disclosure. Many barriers exist that healthcare providers have identified, including time constraints. This is something that many healthcare providers can vocalize; limited time leads to rushing through questions and treatments. Lack of training can consist of a lack of knowledge about community services, including 24-hour services; lack of confidence; and concern on how to respond if the patient discloses domestic violence or intimate partner violence. Providers may be worried about offending the patient or have personal discomfort in discussing these topics with individuals (20).
Providers can overcome these barriers through a variety of ways. Time management can assist healthcare providers by adding extra time to each appointment or incorporating the questions while performing other parts of the patient assessment. Lack of knowledge of community resources gives healthcare providers a way to investigate the specific global and community resources to ensure that the patient has a plethora of material they can utilize when they choose to (20).
If worry of offending patients is a barrier to asking patients about domestic violence or intimate partner violence healthcare providers can easily explain that it is best practice, hospital or organizational policy, or the legal obligation of the provider to ask all patients questions regarding domestic violence. Many organizations do have policies that require providers to ask these questions during every visit; note, ensure that your organization’s policies and procedures are properly followed. By explaining that this is a question that everyone is asked, patients may not be offended (20).
Discomfort may lead healthcare providers to avoid the question completely or rush over it in hopes of not having to deal with it. Unfortunately, sensitive topics can lead to discomfort during discussion, but it is important to remember that someone’s life might be in danger, and asking that single question can save a life (20).
Some patients do not leave their abuser despite the resources healthcare providers give them as covered earlier in this course. Regardless of how many times a patient presents to a hospital or doctor’s office, the healthcare provider is responsible for asking, offering resources and support, and providing treatment to the patient. In time the patient may be able to leave the abuser, and trust in a healthcare provider can be pivotal in that moment (20).

Self Quiz
Ask yourself...
- What is your organization’s policy regarding domestic violence or intimate partner violence screenings or tools?
- Depending on what you are expected to use, do you feel like this tool is effective? Why do you feel this way?
- Is there a tool that you have seen work particularly well?
- From the list of tools provided above which would you think would work best in your area of practice? Why do you think it would be effective?
- Would you be willing to advocate for the use of that tool in your area of practice?
The History Assessment
Commonly known as a “history and physical,” this is the part of the assessment that delves into the patient’s full medical history and where a physical assessment from head to toe is conducted. Depending on the location of the exam—a doctor’s office versus an emergency department—the collection of this data may vary. A primary care provider’s examination greatly contrasts with an exam performed in the emergency department. Regardless, attention to detail can reveal concerning or conflicting information (41).
A patient’s medical history consists of any and all medical conditions the patient has been diagnosed with, past and present. Treatment for these diagnoses is collected with additional information gathered to determine if there are any side effects or adverse reactions to any treatments. Determining if the patient smokes, drinks, takes any illicit drugs, or uses other tobacco products is the goal of obtaining a social history from the patient. The social history assessment also includes asking about spirituality, sexual activity/habits, occupation, relationship status, and hobbies (41).
Family history is often collected with the medical history to assess the patient for genetic predisposition to certain medical conditions. The surgical history is a record of all elective and emergent surgeries done in the patient’s lifetime. This can include any anesthesia reactions or complications that happened as a result of the surgery. The provider also assesses for allergies and any medications the patients take, both prescribed and over-the-counter (41).
Pediatric considers consist of immunization status and developmental milestones. Parents of infants should be asked about pregnancy challenges or diagnoses such as pre-eclampsia, delivery, prematurity, and postpartum complications. For those of childbearing age, or if menstruation is suspected, asking young adult and adult females about their last menstrual period and the possibility of pregnancy is important (41).
When assessing a victim of domestic violence, collecting a history and physical can produce some challenges. The abuser may present with the patient, dominating the conversation or answering the questions for the patient. They may act like a dotting partner or parent or family member, doing everything they can to be the “perfect” support person for the patient. They may point blame at the patient in a causal manner. “She’s just clumsy” or “he’s such an adventurous toddler; he climbs on everything.” Those phrases may prove to be useful when comparing it to the information gathered from the physical assessment (41).


Self Quiz
Ask yourself...
- Have you encountered a time when you wanted to get the victim alone and could not do so? What did you do in that situation?
- What are some other methods to ensure that the victim is given some time alone with a healthcare provider?
- What other barriers could cause providers to obtain an incomplete history from a victim of domestic violence or intimate partner violence?
- How could the age of the victim present challenges when collecting a medical history?
- How else can providers collect data about victims who may have challenges providing a history by themselves (diagnoses, etc.) to determine if there is reasonable cause to suspect abuse?
The Physical Assessment
Depending on what a patient’s chief complaint is upon presentation to the provider’s office or hospital, some type of physical examination is done. This consists of inspecting, palpating, percussing, and auscultating areas of the body. Some exams are more thorough than others depending on location. An emergency room provider is not going to perform an in-depth head-to-toe assessment on every patient. Instead, they assess the area of complaint and determine a diagnosis or other tests that need to be done. Family providers are more invested in the patient as a whole as they manage the patient’s chronic medical conditions as well as collaborate with specialists to ensure the patient is receiving the best treatments (61).
Below is a table of each body system and how a perfect patient—no medical conditions or diagnoses—would appear versus any signs and symptoms that could indicate a patient is a victim of domestic violence. It is vital to remember that many medical conditions can look like domestic violence: those with clotting disorders are more prone to bruising, so multiple bruises in various stages of healing could be attributed to the medical condition. This is why it is important for healthcare providers to collect a comprehensive medical history as well as a detailed description of why they are seeking help. Some injuries are caused in particular ways that do not match the story being told (61).
| System | Typical Assessment | Potential Domestic Violence |
| Integumentary System |
|
|
| Head, Neck, Face, Eyes, Ears |
|
|
| Mouth, Throat, Nose |
|
|
| Thoracic |
|
|
| Cardiac |
|
|
| Abdominal |
|
|
| Genitalia |
|
|
| Musculoskeletal |
|
|
| Neurologic |
|
|
| Psychosocial |
|
|
| Sources: (27, 41, 45, 59) | ||
The list provided is by no means complete. Healthcare providers may see patients who are coming in for a routine physician appointment, or those patients may be the victims of severe trauma and are fighting for their lives. The case study below depicts one such instance.
Case Study:
A 27-year-old woman is brought to the emergency department via emergency medical services as “car versus pedestrian”. The initial report stated she ran over several times an SUV-sized vehicle. Upon receiving the patient at the hospital, the trauma team was activated for severe crush injuries and internal hemorrhage. Lifesaving interventions were started in the emergency department and continued in the operating room.
What the emergency department staff was unaware of was the driver of the vehicle was the woman’s husband. The couple was outside of their house arguing when the husband stepped into the vehicle and proceeded to run his wife over with the car. Their two children aged seven and two were in the vehicle.
Investigation into the patient’s medical history, phone records, and testimony from friends and family revealed that the woman had been worried about something like this happening. She had confided in a friend that her husband had been making threats to her their entire relationship, but recently they “seemed different.” While her friend was concerned, she did nothing to assist, instead, telling the victim it would all pass.
Author’s Note: Domestic Violence of the Child and Burns
Burns in children experiencing domestic violence are not uncommon. Many abusers try to use the excuse that the child “put their hand into the hot pot of water” which led to the burn. Instinctively, when their hand is forced into hot water the child is going to clench their fist, essentially “sparing” the palm from being burned. This would not happen if the child were to willingly put their hand in the hot water. This sparing happens on other parts of the body when immersed in hot water. When the body is in a tub, they will curl their legs up to their chest, saving the abdomen and creases of the limbs from severe burns or being burned at all. The soles of the feet might be saved due to them being pressed against the bottom of the tub (56).
Glove pattern burns or “waterlines” are indicators that the child was held in the water and has a clear line of demarcation. If someone were to fall in, the burn marks would be in a splash-like pattern with no uniform end line. While these types of injuries are most common in children, they can happen in adults (56).

Self Quiz
Ask yourself...
- The case study above is an extreme case of how domestic violence can present; however, have you encountered a situation like this in your nursing career?
- If so, what do you recall from this case? What stood out to you the most regarding the situation?
- What could the victim’s friend have done differently in the situation besides brushing off the victim’s concern?
- How may the children be affected by this situation?
- If the abuser was not found, what could the hospital staff do to ensure the victim is safe while she is recovering?
Effects of Domestic Violence
Victims report many short and long-term effects that result from domestic violence or intimate partner violence. It may take a long time for these effects to go away, or victims may live with them for the rest of their lives. For healthcare providers, it is important that encouragement is present in conversations and providing reminders that recovery is possible and looks different for everyone. If a victim’s definition of recovery is that they can sleep three hours a night, then that is recovery for that particular individual. If a victim wants to be able to rebuild relationships they lost when living with the abuser, then that is recovery for that individual (23).
Below is a small list of short and long-term effects that individuals can experience during and after abuse.
| Short Term Effect | Long Term Effect |
| · Cuts
· Bruising · Broken or fractured bones · Trauma to vital organs · Changes in sleep patterns · Menstrual cycle or fertility issues · Shortness of breath · Unmotivated · Discouraged or hopeless · Concussions · Sexually transmitted infections · Unwanted pregnancy · Vaginal bleeding or pelvic pain · Anger
|
· Anxiety
· Depression · Thoughts of suicide · Self-harm · Post-traumatic stress disorder · Eating disorders · Chronic pain · Heart problems · Pain during sex or other sexual problems · Self-isolation · Lack of trust in others · Low self-esteem · Alcohol and/or drug use · Developmental delays
|
| Sources: (14, 23, 43) | |
Case Study:
Jeremy arrives at his physician’s office looking to make an appointment. He appears to be in distress and panicking. “This is the only time she’s not home. I don’t know when I’ll be able to get away again,” he tells the receptionist when asked to schedule an appointment at a later date. Fortunately, there was an opening, so Jeremy was brought back to an exam room where he confessed to the provider that he is having a hard time sleeping and seeing that “she is still around.”
When asked about who “she” is, Jeremy immediately stops talking. Unsure of what to do, the staff leaves Jeremy alone and calls for a law enforcement officer and mental health counselor to come assess Jeremy who ends up being transported to the nearest emergency department.
In the emergency department, Jeremy tells the physician that he just wants to be left alone so “she” can’t find him. One of the other staff members recognizes Jeremy and tells the provider that Jeremy was in an abusive relationship a year ago. Jeremy had some “rough patches” with drinking and self-isolation. but he had been doing better. Since the staff member has a good rapport with Jeremy, he goes in to talk with him.
Jeremy admits that he’s been having dreams of “her”, his ex-wife Sharon. He reports he sometimes sees her in different places in the house, just out of reach but always watching. “Sharon’s always there, but today she wasn’t. So, I left.” He states that he cannot tell if it is really her or not since she would sneak up on him without noticing. The staff member notices self-inflicted scratch marks on Jeremy’s arms and his anxious pacing.

Self Quiz
Ask yourself...
- If you had been working in the physician’s office when Jeremy came in, how would you have handled the situation?
- Were you worried about the safety of the staff in the physician’s office? Why or why not?
- What did the staff do that was good, and what were some things they could improve on?
- In the emergency department, Jeremy seemed to have a good rapport with one of the staff members, why is it important to have a support person the victim can trust?
- How could the emergency department have provided reassurance to Jeremy during his stay?
Statistics and Prevalence of Domestic Violence
General:
Looking at the overall data for domestic violence or intimate partner violence, there is a large prevalence and many factors that can contribute to or exacerbate the problem.
On average, there are 20 individuals living in the United States who are physically abused by an intimate partner every minute. That is approximately 28,800 people in a 24-hour period. Annually, the estimated total is over 10 million men and women. According to data, approximately 20,000 phone calls are made to nationwide domestic violence hotlines daily. This does not account for chat services offered online or via text message. Comparing that information to the estimated number of individuals experiencing physical abuse within a 24-hour period, it appears as though many may be seeking help or assistance. However, it is important to keep in mind that abuse can be more than just physical as mentioned. Data does not provide how many individuals are sexually, psychologically/emotionally, or technologically abused every minute (33).
Intimate partner violence affects more than 12 million people annually in the United States; daily that is approximately 32,876,712 individuals. Between 1994 to 2010 four in five victims of intimate partner violence were women. Seventy-seven percent of women from ages 18 to 24 who were victims of intimate partner abuse had been abused by the same partner previously; from ages 25 to 34 the percentage was 76%, and those aged 35 to 49 had a rate of 81% (33).
Rape accounts for a large part of intimate partner violence as one in 10 women have been victims of rape by their intimate partner. Fifty-one percent of women report rape is carried out by their intimate partner, while 40.8% report the rape was carried out by an acquaintance. Experiencing sexual coercion is estimated to encompass around 13% of women and 6% of men; victims are non-physically forced to participate in sexual acts they do not want to do (33).
Workplace:
Being a victim of domestic violence can create problems in areas outside of the relationship. School or work can be drastically affected. One survey shows that 64% of those who self-identified as victims of domestic violence or intimate partner violence report that their work was affected as a result of the violence. This ranged from being distracted at 57% while fear of being discovered at work was 45%. Two out of every five victims reported they were worried an unexpected visit from their intimate partner would occur or the partner would unexpectedly call work (36).
The fear of an abuser unexpectedly showing up to a place of work is real for victims. Some may use work as a way to plan their escape from the abusive situation. Going to work might be an act to make the abuser think all is well in the relationship while the victim is fleeing. As discussed, many victims do not share their abuse with others. Coworkers may not know what is going on and let the abuser know the victim is not at work or let them enter the building, unaware that they are putting the victim or others at risk. It is important to note that 20% of homicides related to domestic violence or intimate partner violence do not result in the death of the victim. Instead, those who are killed consist of law enforcement officers or other first responders, individuals who try to intervene during an abusive episode, or bystanders caught in the middle of the situation (36).
Interestingly, 63% of cooperate executives report domestic violence is a major societal problem and 55% report it impacts productivity in their companies. The percentage of executives saying that domestic violence impacted the bottom line was 43%, a substantial number. However, when compared to the employees of these companies 43% is insignificant as 91% of employees said violence impacted the bottom line. Seventy-one percent of those same executives did not believe domestic violence or intimate partner violence was a major concern in their company. Despite this statement, domestic violence contributes to approximately 8 million lost days of paid work annually, this is the equivalent of over 32,000 full-time jobs. Data continues to support the need for awareness on all levels of the corporate ladder to better help victims (36).
Weapons:
Reports put emphasis on how weapons can affect the situation. Nineteen percent of domestic violence or intimate partner violence cases involve a weapon. An estimated 13.6% of women living in the United States report they have been threatened by their intimate partner with the use of a firearm. Out of that 13.6%, 43% of women report being physically injured. In a seven-year period between 2010 and 2017 intimate partner homicides using firearms increased by 26% while homicides using other weapons decreased. Having access to a firearm increases the risk of homicide is increased by 500% and increases the chance of femicide—homicide of a woman by a man based on their gender—by 1,000% (36).
Other data on firearms and homicide in domestic violence or intimate partner violence situations show that incidences involving firearms result in death twelve times more than other weapons or use of bodily force. Twenty percent of women who obtain an emergency protective or restraining order are murdered within the first two days of obtaining that order; about 33% of them are murdered within the first month. Stalking plays a large factor in domestic violence as well; 58% of the women who survived a murder attempt and 76% of those who were murdered were initially victims of stalking (36).
Some may suggest the victim purchasing a firearm for safety, and this can be met with mixed reviews. If the victim lives with the abuser, this may not be a reasonable option due to the risk of the abuser locating the firearm and using it. Data shows that victims owning a firearm is not a protective factor against domestic abusers and there is a 50% increase of intimate partner homicide while doubling the chances of a firearm homicide (36).
Some states have created legislation and laws to prevent abusers from owning or possessing firearms. In those states, the rate of intimate partner homicide is 13% lower than in states that do not have these types of laws or legislation in place. States that require abusers to relinquish firearms and prohibit them from purchasing additional firearms have a 12% decrease in homicide. Federal law does exist to control abusers from owning or purchasing firearms based on certain criteria; however, no process is without fault or room for abusers to evade the system, and providers should be aware of such by always assessing for a victim’s safety and the presence of any weapons within the home or where the abuser could easily access them. This could be through friends, family, neighbors, legal purchase, or illegal obtainment (36).

Kentucky Specific Data:
According to research, 45.3% of women and 35.5% of men that reside in Kentucky report having been a victim of domestic violence or intimate partner violence and/or rape in their lifetime. Out of all 50 states, Kentucky is ranked 11th for the highest rate of femicide in the country with 1.77 per 100,000 females; Alaska had the highest rating with 396 per 100,000 females. Comparing this data with the lowest states Maine, Nebraska, and New York tied for 44th with a 0.73 per 100,000 femicide rate. It is fair to note that Alabama and Florida did not have data collected and/or submitted for this particular study which may have impacted the results of ranking (32).
On any given day in 2015, Kentucky’s domestic violence services provided for 1,420 adult and child victims of domestic violence or intimate partner violence. Unfortunately, 128 service requests had to be unmet due to the lack of resources within the communities. While this is inspiring data, it is important that services are expanded and properly funded so the unmet requests in any state are zero (32).
As mentioned, some states have laws regarding abusers and firearms. While Kentucky is not a state that has this particular law, judges who issue ex parte orders, as well as final protective orders, can include the prohibition of owning and surrendering currently owned firearms within those orders. Those under an ex parte or final protective orders may be prohibited from carrying concealed weapons and surrendering any concealed carry permits to law enforcement or the court. This is based on the judge’s decision, however, so consistency is nonexistent in these situations. With the exception of surrendering concealed weapon permits and not being allowed to carry concealed, intimate partners or dating partners are offered the same relief under a separate statute (32).
COVID-19 Considerations:
The global pandemic caused by the acute respiratory syndrome coronavirus 2 (SARS-CoV-2), commonly referred to as COVID-19, has led to a global increase in domestic violence cases. Data collected by the local police In China’s Hubei Providence reported that domestic violence rates tripled in February 2020 compared to a year prior. France’s rates increased by 30% after their lockdown on March 17th. Three days later, on March 20th, Argentina initiated its own lockdown and saw a 25% increase. Domestic violence or intimate partner violence hotlines through the United Nations entity UN Women reported a 30% and 33% increase in their hotline services in Cyprus and Singapore respectively (4).
Data gathered from United States police departments showed similar results. In Portland, Oregon, public schools closed on March 16th with stay-at-home orders going into effect on March 23rd. Statistics collected after that date showed a 22% increase in arrests for domestic violence or intimate partner violence in comparison to prior weeks. Schools in San Antonio, Texas closed on March 20th and four days later stay-at-home orders were in place. There was an 18% increase in calls regarding domestic violence. Jefferson County, Alabama had a 27% increase in calls in March 2020 as opposed to March 2019. The police department of New York City had a 10% increase in March 2022 domestic violence reports in comparison to March 2019 (4).
As covered previously in this course, many factors can influence acts of domestic violence or intimate partner violence. Many individuals were living in fear, worried about their health, jobs, food, housing, and money. Many people started working from home, had fewer work hours, or were laid off due to decreases in the number of employees needed to keep businesses open. In addition to triggering or exacerbating factors, these emotions can also lead to stress, another factor (57).

Self Quiz
Ask yourself...
- What statics surprised you the most? Why did it surprise you?
- Were there any statistics you were not surprised by? How can we work to decrease these numbers?
- In discussing COVID-19’s impact on domestic violence data, what other reasons for the increase can you think of?
What can Nurses do?
Nurses play a large role in the healthcare setting when it pertains to domestic violence. Nurses are some of the first individuals that victims may encounter in the healthcare setting and that first interaction is vital in developing trust. As has been covered in this course, those who are in a domestic violence or intimate partner violence situation will often refrain from telling others about their situation. Nurses can continue to screen every patient they come in contact with, advocate for better funding for services, and legislature to better protect victims of domestic violence (24).
Many states have mandatory reporting laws, including Kentucky. The particular law initially required the reporting of child abuse or suspected child abuse, dependency, and neglect along with the abuse, financial exploitation, or neglect of an adult who has been diagnosed with a physical or mental disability and who cannot care for or protect themselves, including an elderly individual. This report is made to the Cabinet for Health and Family Services and/or the local or state police department. Other entities may be contacted as instructed by the police, organizational policy, or the Cabinet for Health and Family Services (38).
A revision to the law that occurred in 2017 made some adjustments to Kentucky’s mandatory law for victims of domestic violence or intimate partner violence by changing it to a mandatory information and referral provision. The law requires certain professionals to provide education to victims of domestic violence or intimate partner violence if they have a professional relationship with that person and there is reasonable cause to suspect abuse. These professionals are required to contact law enforcement if the victim requests them to. The professionals must also notify law enforcement if they suspect the death of an individual was a result of domestic violence or intimate partner violence (40).

Self Quiz
Ask yourself...
- In your nursing career, have you been required to make a call regarding suspected or confirmed abuse? How did the process go?
- What parts of the process were difficult for you as a nurse?
Resources
Many of the resources below can be accessed nationally and many have safeguards in place for “quick exit” of webpages that close the page and prevent individuals from hitting the “back” button. They do not clear history or other browsing tracking that might be in place. A quick reference list should be available in healthcare organizations with both national and local services.
National Domestic Hotline
800-799-7233 (SAFE)
Text “START” to 88788
National Dating Abuse Helpline
1-866-331-9474
National Child Abuse Hotline/Childhelp
1-800-4-A-CHILD (1-800-422-4453)
National Sexual Assault Hotline
1-800-656-4673 (HOPE)
National Center for Victims of Crime
1-202-467-8700
National Network for Immigrant and Refugee Rights
1-510-465-1984
National Coalition for the Homeless
1-202-737-6444
National Resource Center on Domestic Violence
1-800-537-2238
www.nrcdv.org and www.vawnet.org
National Deaf Domestic Violence Hotline (NDDVH)
855-812-1001 (Voice/VP)
https://www.thedeafhotline.org/
Email: hotline@adwas.org
The Ion Center for Violence Prevention
835 Madison Ave, Covington, KY 41011
859- 491-3335
The Kentucky Coalition Against Domestic Violence
111 Darby Shire Cir, Frankfort, KY 40601
502-209-5382
Domestic Shelters
https://www.domesticshelters.org/help/ky
Louisville Police
Domestic violence 24-hour crisis line staffed with domestic violence counselors: 1-844-BESAFE1 (237-2331)
https://www.louisville-police.org/320/Domestic-Violence

Diabetes Management Updates
Introduction
Diabetes Mellitus (DM), also known as diabetes, is a condition in which the body develops high levels of blood glucose due to the inability to produce insulin or for the cells to use insulin (1) effectively. If left untreated or mismanaged, it can lead to health complications such as heart disease, chronic kidney disease, blindness, nerve damage, oral and mental health problems (1)(15).
There are several classifications of DM, and the following will be discussed: T1DM, T2DM, gestational diabetes, and idiopathic diabetes.
Classifications of Diabetes
Type 1 Diabetes Mellitus (T1DM)
T1DM is formerly known as juvenile diabetes or insulin-dependent diabetes and usually occurs in children and young adults (1). Although, it can also occur at any age and accounts for 5 – 10% of cases. T1DM develops when one’s own immune system attacks and destroys the beta cells that produce insulin in the pancreas (6).
Type 2 Diabetes Mellitus (T2DM)
T2DM, formerly known as adult-onset diabetes or non-insulin-dependent diabetes, develops because of the body's inability to use insulin effectively. It is the most common type of diabetes and mainly occurs in adults aged 30 years and older (1). However, it is also becoming common in children and young adults due to obesity. It accounts for 90% of the population diagnosed with diabetes (6).
Gestational Diabetes
Gestational Diabetes occurs during pregnancy and in women who have never had a previous diagnosis of diabetes. It is a result of pregnancy hormones that are produced by the placenta or because of the insufficient use of insulin by the cells (1). Gestational diabetes can be temporary or in some cases can become chronic. It is also likely that children whose mothers have gestational diabetes can develop diabetes later in life (6).
Prediabetes
Prediabetes, also referred to as impaired glucose tolerance, is a stage when a person is at risk of developing diabetes. If well managed through proper diet management and exercise, this can help with the prevention or delay of type 2 diabetes (1).
Other Forms of Diabetes
Other forms of diabetes include monogenic diabetes syndrome, diabetes from the removal of the pancreas or damage to the pancreas from disease processes such as pancreatitis or cystic fibrosis, and drugs or chemical-induced diabetes from glucocorticoids used to treat HIV/Aids or organ transplant (1) (6).

Self Quiz
Ask yourself...
- What are the four named types of diabetes?
- What are the differences between T1DM and T2DM?
- What is the most common type of diabetes?
Statistical Evidence/Epidemiology
Diabetes is now ranked as the 8th leading cause of death in the United States (6). There is no known cure for diabetes. It is one of the fastest-growing chronic diseases and the most diagnosed noncommunicable disease. It is also one of the leading causes of chronic kidney disease, adult blindness, and lower limb amputations (6).
In 2019, it was estimated that 37.3 million American adults have diabetes, which equals 11.3% of the population (4). Of those, 41% were men and 32% were women. 28.7 million were diagnosed with diabetes, and 8.5 million were undiagnosed.
There are 96 million American adults who are prediabetic, which means they are at risk of developing diabetes, but their blood glucose levels are not high enough to be diagnosed with diabetes (5).
Most of the population that is pre-diabetic is 65 years old or older. Type 2 diabetes accounts for 90% to 95% of cases (5). The risk of developing diabetes increases with age.
The prevalence of diabetes is much higher in both black and Hispanic/Latino adult men and women. Men are more likely to develop diabetes compared to women. Due to the rise in obesity in younger adults, there has been an increase in the number of new cases of diabetes in black teens (4).
The figure below represents trends in incidence of type 1 and type 2 diabetes in children and adolescents 2002–2018; results show the incidence of type 2 diabetes has significantly increased (4)
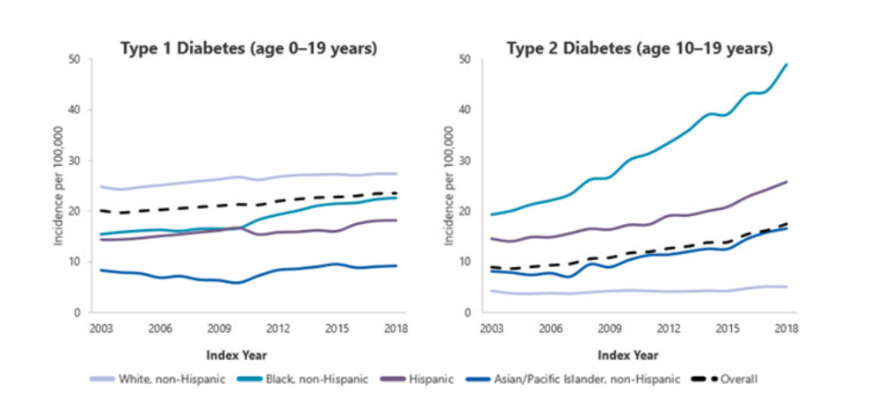

Self Quiz
Ask yourself...
- What is one of the major comorbidities caused by diabetes?
- What age group is at risk for developing type 2 diabetes?
- What is a risk factor that is contributing to the rise of diabetes in younger adults?
Etiology and Pathophysiology
In normal glucose metabolism, blood glucose is regulated by the two hormones insulin and glucagon (11). Insulin is secreted by the beta cells in the Islet of Langerhans in the pancreas and glucagon is secreted by the alpha cells in the pancreas.
When there is an increase in blood glucose, the function of insulin is to reduce blood glucose by stimulating its uptake in the cells. Glucose is stored as glycogen in the liver and muscles or as fat in the adipose tissues. When blood glucose levels start to fall, glucagon promotes the release of glycogen from the liver, which is used as a source of energy in the body (8) (13).
When there is a deficiency of insulin or a decreased response of insulin on the targeted cells in the body, it leads to hyperglycemia (high blood glucose). Meaning that the glucose that remains in the blood is not able to get to the cells. Diabetes develops mainly because of lifestyle and genetic factors (13).
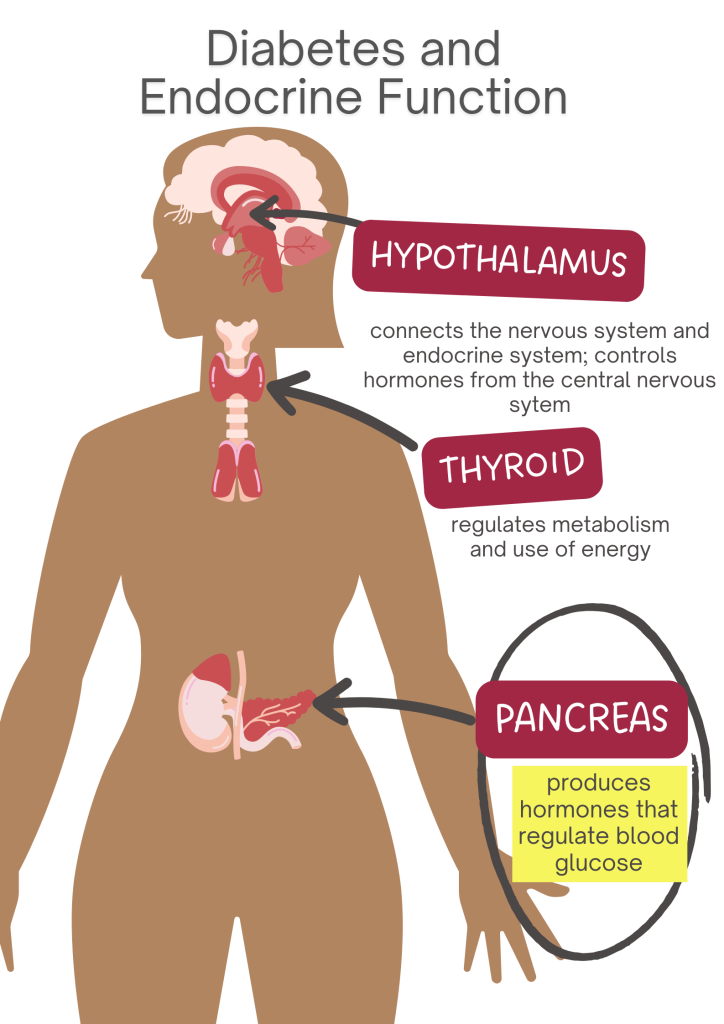
T1DM
The etiology is not well understood, though it is thought to be influenced by both environmental and genetic predispositions that are linked to specific HLA alleles. T1DM is considered an autoimmune disorder that is characterized by T-cell-mediated destruction of the pancreatic B-cells (13).
As a result, this leads to complete insulin deficiency and ultimately hyperglycemia, which requires exogenous insulin. The rate of destruction of the pancreatic B-cell-specific disorder is known to develop rapidly in infants and children or gradually in adults (8)(13).
T2DM
The etiology of T2DM is characterized by decreased sensitivity to insulin and decreased secretion of insulin. Insulin resistance occurs due to the disruption in the cellular pathways that result in a decreased response in the peripheral tissues, particularly the muscle, liver, and adipose tissue.
T2DM diabetes can progress slowly and asymptomatically over a period. Obesity and age can play a key role in the homeostatic regulation of systemic glucose because they influence the development of insulin resistance, which affects the sensitivity of tissues to insulin. Therefore, most patients with type 2 diabetes are overweight or obese 7) (8).

Self Quiz
Ask yourself...
- What are the two hormones that are responsible for maintaining blood glucose levels in the body?
- Can you describe the etiologies of both T1DM and T2DM?
- What are some of the factors that contribute to T2DM?
Diagnostic and Screening tools
There are a variety of tests that are used to diagnose and monitor diabetes. These vary based on the type of symptoms that a patient may have. Diagnosis of DM requires at least two abnormal test results, which should include fasting glucose and A1C. The tests should be one of two from the same sample or two abnormal test results drawn on different days (3).
The recommended diagnosis guidelines for diabetes must be based on the following criteria:
- Fasting Plasma Glucose (FPG) concentration with results greater than 126 mg/dL. This test involves measuring blood glucose at a single point. To have accurate results, the test should be conducted after one has had nothing to eat or drink for at least 8 hours (3).
- Glycated hemoglobin (Hb A1C) is indicative of the average levels of blood glucose in a period of two to three months. Results greater than 6.5% mean diagnosis of diabetes. This blood test does not require fasting. The A1C test is not suitable for pregnant women or those who have certain blood conditions (anemia) - NIDDK. This test should only be used for prediabetes screening (3).
- Oral Glucose Tolerance Test (OGTT): prior to conducting this test, an FPG level needs to be measured. One must ingest 75 grams of glucose liquid. Thereafter, their glucose level is measured 2 hours after they have taken the liquid. Test results greater than 200 mg/dL are indicative of diabetes. This test is commonly used in pregnant women (3).
- Random plasma glucose of 200 mg/dL. This test is suitable when one has symptoms of hyperglycemia, which are polydipsia, polyuria, and polyphagia (3).
Screening
Screening is generally recommended for adults aged 45 or older regardless of present risk factors. The updated recommendation guidelines for prediabetes screening include adults 35 years and older who are overweight or obese (3).
Screening for Prediabetes
Prediabetes is associated with the impairment of blood glucose levels between 100 – 125 mg/dL. The diagnosis of prediabetes should be confirmed with glucose testing when there is impaired glucose tolerance with plasma levels between 140 – 199 mg/dL 2 hours after one has ingested 75g of oral glucose. A1C levels of prediabetes are between 5.7% to 6.4% (3).
Screening for Pregnant women
It is recommended that all pregnant women between 24 – 28 weeks be screened for gestational diabetes to avoid missing those that are at risk. A positive 3-hour OGTT test of greater than 140 mg/dL meets the criteria for diagnosis (3).
Medication Management
Monitoring of blood glucose levels in patients is useful in determining the effectiveness of antidiabetic medication. To achieve better patient outcomes, it is important to recognize individual needs (11).
It is recommended that the approach to medication management should be based on each patient's hyperglycemic index and should include the following: the presence of comorbidities, risk of hypoglycemia, vascular disease, life expectancy, and disease duration (3).
When the management of diabetes cannot be achieved through diet and exercise alone, oral antidiabetic agents are the preferred treatment (14). Oral antidiabetics can help maintain and achieve glycemic goals for patients who are diagnosed with T2DM) (10)(14).
Diabetes Education and patient engagement is essential to managing diabetes (11). There are several classes of anti-diabetic medication. Below are some of the most utilized antidiabetic medications (9)(14).
Biguanides
Metformin is the only medication in this category.
- It is considered the 1st line of treatment in patients with T2DM unless contraindicated.
- Metformin helps to decrease hepatic glucose production.
- Decreases intestinal absorption of glucose by improving insulin sensitivity. Must be titrated initially to minimize adverse effects.
- Avoided in clients with chronic kidney disease.
- Side effects: Lactic acidosis, hypoglycemia.
GLP 1- Receptor Agonists (RAs)
Mimics glucagon-like peptide 1 (GLP -) hormone. Binds to GLP-1 receptors stimulate glucose-dependent insulin release and delay gastric emptying, which increases satiation.
- Known to have cardiovascular benefits.
- Can be taken orally or subcutaneously.
- Special considerations: Can cause weight loss, GI side effects such as nausea, vomiting and diarrhea, dehydration, increased satiation (fullness), acute pancreatitis, and reactions at the injection sites.
- Some labels may require renal dose adjustment.
- GLP - 1 RAs should be considered before starting clients on insulin to help reduce A1C then oral antihyperglycemic medications are not effective in treating diabetes.
Sulfonylureas 2nd generation
Stimulates insulin release in pancreatic beta cells.
- Risk for prolonged hypoglycemia. Therefore, it should be avoided with the concurrent use of insulin.
- Can cause weight gain.
- Can cause photosensitivity.
- Avoid use in clients with sulfa allergies and photosensitivity.
- Avoid use in clients with chronic kidney disease and liver disease.
Dipeptidyl Peptidase (DPP) - 4 inhibitors
Prevents DPP-4 enzymes from breaking down to GLP-1 hormone.
- Neutral weight.
- Monitor for acute pancreatitis, which can cause joint pain.
- May require renal dose adjustment with these brands: Saxagliptin (Onglyza), Sitagliptin (Januvia), and Alogliptin. Linagliptin does not require dose adjustment.
Sodium-Glucose transporter - 2 (SGLT-2) inhibitors
Reduce the reabsorption of glucose by up to 90%, therefore promoting the exclusion of glucose from the body.
- Known to have cardiovascular benefits for clients with cardiovascular disease.
- Use with caution in clients with increased risk of fractures.
- Avoided in clients with diabetic ketoacidosis and those prone to have frequent urinary tract infections.
- This medication should be avoided in clients with pure poor kidney function due to volume depletion and hypotension.
- There’s also a risk for Fournier gangrene.
Thiazolidinediones
Pioglitazone and rosiglitazone can help reduce insulin resistance which promotes improved sensitivity to insulin. As a result, it can help reduce the A1C levels.
- Can cause weight gain.
- Potential risk for heart failure when taking thiazolidines (brands: pioglitazone, rosiglitazone).
- Generally, it is not recommended for clients with renal impairment as medication has the potential to cause fluid retention.
- Risk for bone fractures, bladder cancer, and increased LDL cholesterol (rosiglitazone).
- Thiazolidines do not cause hypoglycemia and can be used in combination with other antidiabetic medications including insulin.

Self Quiz
Ask yourself...
- Which class of antidiabetic medications are known to put patients at risk for bone fractures?
- Can you name a condition that thiazolidines and sulfonylureas 2nd generation are generally not recommended for?
- What is a common side effect in both thiazolidines and sulfonylureas?
- What class of medication is suitable for clients with insulin resistance?
- Can you name two antidiabetic medications that can be used in combination with other antidiabetics because it has the benefit of not causing hypoglycemia?
Insulin therapy
Insulin therapy is commonly recommended for patients with T1DM. It can be used to help prevent the development and progression of diabetes (2). The ideal insulin regimen should be tailored based on individual needs and glycemic targets to better contend with physiological insulin replacement to maintain normoglycemia. Insulin therapy is also recommended for patients with hemoglobin A1c of greater than 9% - 10% and when symptoms of hyperglycemia are present (3).
Other Diabetes Interventions
The automation of glucose monitoring devices and insulin delivery systems is revolutionizing glucose management mainly because it promotes lifestyle flexibility and improved glucose management (2).
- Glucose Monitoring Devices- these devices are ideal for clients who are on insulin regimens and may become the standard for assessing glycemic controls in clients with DM (7).
- Continuous Glucose Monitoring (CGM)- devices that are inserted subcutaneously and measure interstitial blood glucose levels. CGMs are devices that are used to provide glucose readings, trends, and alerts to the user in real-time to inform diabetes treatment decisions. (2)(3)
- Importance- CGM is recommended for all patients with diabetes who receive treatment with intensive insulin therapy, defined as three or more insulin injections per day for all individuals with hypoglycemia (frequent, several, nocturnal) (3).
- Known to reduce hyperglycemia and A1C levels.
- Insulin Pump Therapy- also known as Continuous Subcutaneous Insulin Infusion (CSII) has had notable advances over the years. CSII is recommended for those with type 1 diabetes, although in recent studies, conventional CSII is also recommended for use in T2DM patients (2)(3). CSII is a small computer that is programmed to deliver fast-acting insulin continuously to the body using mechanical force via a cannula that is inserted under the skin (2).
- It is more precise and flexible in insulin dosing.
- Known to improve glycemic control.
- Cheaper than using Multi-Dose Insulin.
- Automated Insulin Delivery Systems (AIDS) - This is a diabetes management system that utilizes an insulin pump in conjunction with an integrated CGM and computer software algorithm (3).
- Advantages: precision and flexibility with insulin dosing.
- Recommended for T1DM: Achieve glycemic targets with less burden.

Self Quiz
Ask yourself...
- What is the main type of insulin used in CSII pumps?
- What type of diabetes category is more suitable for using CSII?
Upcoming Research
Islet cell transplant has been a biological solution to help treat patients with T1DM due to poor graft survival rates. Future research will focus on manipulating the beta cells in the pancreas to make them more viable. Other treatments that have been recently made available include incretins and Amylin which improve the absorption of insulin in the body (1).
- The development of other types of insulin that can be administered by inhalation.
- The development of immunosuppressant drugs that will help treat T1DM.

Self Quiz
Ask yourself...
- Can you name two recently developed medications to help with insulin absorption in the body?
Conclusion
Diabetes is a complex disease that requires a multi-disciplinary and patient-centered approach to help with effective management. Regular and early screening are necessary for those at risk for developing diabetes. Most importantly, ease and access to choices of managing diabetes are necessary.
Hospice and Palliative Care: What’s the Difference?
Introduction
Hospice and palliative care are unique health concepts often incorrectly used interchangeably. During my career as a hospice and palliative care nurse, I often heard the question, "What's the difference between Hospice and Palliative Care?"
I usually answered with a common phrase the Hospice and Palliative Care community uses to explain the difference, "All Hospice is palliative care, but not all Palliative Care is hospice." The statement is accurate but still confusing.
This course aims to shed light on these topics and emphasize the importance of enhancing end-of-life care, but let's start with Merriam-Webster's dictionary definitions.
- Hospice: "a program designed to provide palliative care and emotional support to the terminally ill in a home or homelike setting so that quality of life is maintained, and family members may be active participants in care” (4).
- Palliative: "relieving or soothing the symptoms of a disease or disorder without effecting a cure” (4).
The Merriam-Webster definitions help to clarify the differences further: Hospice is a program, and palliative care is a practice. They are two distinct approaches to providing comprehensive medical care and support for patients with serious illnesses, and they have essential differences worth exploring.
This course aims to delve into the different types of care, their philosophy, eligibility criteria, duration of services, and common myths and misconceptions surrounding hospice and palliative care. Additionally, it highlights nurses' crucial role as advocates and resources in these specialized fields.

Hospice Care
The modern hospice movement originated in the late 1960s in the United Kingdom, primarily through the work of Dame Cicely Saunders. Saunders, a nurse, and social worker, recognized the need for specialized care for patients with terminal illnesses. She founded St. Christopher's Hospice in London in 1967, which became the model for modern hospice care (12).
Saunders emphasized care that was less focused on disease treatment and more focused on an individual's physical, emotional, social, and spiritual needs. This approach prioritized providing comfort, pain management, and dignity for patients nearing the end of life (12).
The concept of hospice care gained international recognition and spread to other countries. By 1974, the first hospice program in the US was formed in Connecticut, and the hospice movement expanded rapidly (11).
Hospice care was primarily provided by volunteers who went into families' homes to care for their loved ones when no curative care was available. These same volunteers helped write the federal regulations adopted as the Medicare Hospice Benefit (MHB) in 1982 (5).
It is essential to discuss the MHB because the US government benefit made hospice a fundamental part of comprehensive medical care. It is the benefit through which most patients nearing the end of life receive care, and it has defined how we provide hospice care throughout the United States.
An integral part of hospice care is visits from a nurse, social worker, chaplain, and nurse aides. In addition, the patient and family have access to a hospice physician specializing in Hospice and Palliative Care (5). Hospice care focuses on providing compassionate, holistic, patient-centered care for individuals with terminal illnesses. The primary goal is to enhance the quality of life for patients and their families by addressing physical, emotional, social, and spiritual needs (5).
The MHB covers 100% of the financial cost for hospice services, including medications, supplies, and treatments required due to a terminal illness. The medicines commonly covered under the hospice benefit are for treating pain, nausea, anxiety, and other distressful symptoms, such as constipation (5).
Who can receive this care?
The MHB was designed for patients who are terminally ill with a six-month life expectancy, as determined by a physician (5). Life expectancy is one of the critical differences between Palliative Care and Hospice Care.
Healthcare providers, unlike statisticians or actuaries, are unskilled at predicting a six-month or less life expectancy. As part of the hospice federal regulations, local coverage determinations set by government intermediaries help healthcare providers determine who meets the criteria and, therefore, is eligible for hospice.
Key indicators predicting the end of life due to a specific disease process have been defined so that we can compare each patient to determine their eligibility for hospice care. Some key indicators are activity level, the times the patient has sought emergent care or has been hospitalized in the past six months, weight loss, and neurological status.
Patients generally receive hospice care when curative care is no longer an option. This is another crucial difference between Hospice and Palliative Care. There are exceptions, commonly for children, where curative and hospice care are provided. This is termed "concurrent" care.
How long do they receive services?
The key indicators that hospice physicians use to determine eligibility are based on averages of patients who have died with the specifically defined disease process. However, the average time to death is unreliable when judging how long an individual may live.
Therefore, hospice care is provided for as long as the patient's condition remains terminal, according to local coverage determinations, and they choose to continue receiving this specialized type of palliative care. In fact, the MHB has no end date, and the duration of services may vary depending on the progression of the illness and the patient's preferences.
For example, patients with chronic illnesses, such as heart failure, chronic obstructive pulmonary disease (COPD), and Alzheimer's, tend to have a less predictable trajectory of terminal illness due to periods of exacerbation and stability, which are common. Patients with chronic diseases tend to have a longer stay in hospice care. A waxing and waning pattern of decline is less typical with cancer-related disease, and these patients generally use fewer days of hospice care.

Self Quiz
Ask yourself...
- What is your understanding of the philosophy behind hospice care?
- How do you determine the appropriate duration of services for a hospice patient?
Palliative Care
The long-held theory regarding palliation, or soothing symptoms as defined by Merriam-Webster, is that if the treatment causes suffering with the result of a cure, the benefit of the treatment outweighs the burden. In other words, a person should be able to tolerate suffering for a positive end result. On the other hand, if no cure is available, suffering is inhumane.
Palliative Care emerged as an integral part of hospice care, focusing on providing comfort and support to patients with terminal illnesses (14). However, for people without terminal illnesses, some treatments and symptoms of curable diseases are so intolerable that patients may be unable or unwilling to continue curative treatment. Why should patients and families not receive physical, psychosocial, or spiritual support simply because they are not at the end of life?
The need for Palliative Care beyond hospice was identified in other healthcare settings, such as hospitals and home care. Over time, the philosophy and principles of Palliative Care gained recognition beyond the hospice setting. This led to the development of specialized palliative care services that aimed to provide comprehensive support to patients with serious illnesses, regardless of their prognosis (14).
In 1990, the World Health Organization (WHO) formally defined palliative care, emphasizing its holistic approach. The WHO defines palliative care as improving the quality of life of patients and their families facing life-threatening illnesses by preventing and relieving suffering through early identification and treatment of pain and other physical, psychosocial, and spiritual problems (13).
The American Academy of Hospice and Palliative Medicine (AAHPM) was established to promote and advance Palliative Care, and it has now become a recognized medical specialty. Palliative care education programs, certifications, and fellowships have been established to ensure the development of skilled professionals who provide palliative care (14).
Palliative Care is an essential part of healthcare, aiming to improve the quality of life for patients with serious illnesses and their families. It focuses on relieving symptoms, addressing psychosocial and spiritual needs, and enhancing communication and decision-making throughout the illness trajectory.
Philosophy
Palliative care aims to improve the quality of life for patients who suffer regardless of life expectancy, a key differentiator from hospice care. Palliative care focuses on symptom management, pain relief, and addressing patients' and their families' physical, emotional, and psychosocial needs.
Who can receive this care?
In the modern healthcare system, "palliative" is often used to define comfort care for patients with "serious illnesses." Palliative Care is available to individuals of any age and at any stage of a serious illness, including those undergoing curative treatments. It can be provided concurrently with curative treatments, such as chemotherapy and radiation, another differentiator from hospice care. Individuals with serious illnesses may receive palliative care during a hospitalization, at home, or office visits.
How long do they receive services?
Unlike Hospice Care, Palliative Care can be provided for an extended duration even if the patient's condition is not terminal. The duration of services varies based on the individual's needs.

Self Quiz
Ask yourself...
- How does Palliative Care differ from Hospice care in terms of philosophy and approach?
- Can you explain the eligibility criteria for receiving palliative care?
Common Myths and Misconceptions
| Myth |
Fact |
|
Hospice care hastens death. |
Studies show that patients with the same diagnosis and burden of illness live longer with hospice than without (2). |
|
Palliative care is only for people who are dying. |
Palliative care is available to people of any age and stage of serious illness. |
|
Hospice is a place. |
Hospice is a form of care provided to people wherever they reside. |
|
Palliative care is only available in hospitals. |
Palliative care is available in hospitals, at home, or in a doctor's office. This is dependent on the availability of practitioners in your area. |
|
Hospice is only for the last days of life. |
Hospice is for the terminally ill with a life expectancy of 6 months or less and continues as long as a person remains terminally ill (15). |
|
Palliative care is only for the elderly. |
Palliative care is for all individuals with a serious illness. |
|
Hospice is the same as Palliative Care. |
Hospice is palliative care for the terminally ill. Palliative care is for all patients receiving curative treatment no matter the stage of illness, depending on the Palliative Care team's defined practice. |
|
Hospice and Palliative Care mean you are giving up hope. |
Hospice and Palliative Care aim to manage symptoms and improve the quality of life. |
|
Hospice and Palliative Care are expensive and not covered by insurance. |
Hospice care is 100% covered by Medicare and most other insurance (15). Palliative care is covered as a medical practitioner's visit in most Palliative Care programs. |

Self Quiz
Ask yourself...
- What are common misconceptions you have encountered regarding hospice or palliative care?
- How did you resolve the misconceptions surrounding palliative and hospice care?
Handling Difficult Conversations
Conversations, especially regarding end-of-life, are difficult for the clinician, the patient, and the family. Sensitive conversations also take time, patience, and empathy. Often, more time than a general practitioner or clinician has available. In my experience, patients approaching the end of life are often referred to as Palliative Care practitioners because of the practitioner's experience with difficult conversations. I also believe this referral practice is part of the confusion in understanding the difference between Palliative and Hospice Care.
Palliative Care Practitioners are not the only ones with the time and the skill to broach difficult conversations. Nurses also play a critical role in facilitating difficult conversations about end-of-life decisions, goals of care, and advance care planning.
Nurses often spend more time with patients and families than other disciplines. The relationship and trust nurses build with patients and caregivers makes them especially adept at starting difficult conversations.
A nurse must take the following actions before, during, and after a difficult conversation (3).
- Build a strong relationship with the patient and their family through active listening, empathy, and creating a safe space for open communication.
- Assess the patient's and family's readiness and preferences to engage in discussions. Ask patients and families questions regarding the amount and detail of information they want and the personspeople that need to be involved in decision-making. This information helps to tailor the discussion.
- Use practical communication skills such as clear and concise language aimed at providing information in a way that is understandable and sensitive to the emotional needs of the patient and family.
- Begin the conversation by assessing the patient and family's understanding of the diagnosis and prognosis to address any misconceptions or gaps in knowledge and ensure everyone is on the same page.
- Engage in a collaborative discussion about the patient's goals and values. Exploring their priorities and preferences regarding treatment options, symptom management, and quality of life helps align the care plan with the patient's values and wishes.
- Acknowledge and validate emotions, offering support and empathy throughout the conversation. Referral to appropriate psychosocial or spiritual support services may be necessary.
- Document the discussion and decisions made in the patient's medical records. Follow-up conversations should be scheduled to address any further questions, concerns, or changes in the patient's condition or preferences (3).
Should you find yourself in a position to start a difficult conversation, the following practical framework may be of assistance (3):
- Set aside time and make a plan to minimize interruptions.
- Before the conversation, take a moment to center yourself and release stress.
- Acknowledge the family and offer support by inquiring about their immediate needs.
- Open the conversation by asking what the patient and family know about their condition.
- Repeating what they know, ask them how they want to experience the time they have left.
- Empathize and allow them time to discuss and consider what they want.
- Based on their desires, educate them about the options for care.
- Consult with the interdisciplinary team and make appropriate referrals.

Case Study
Emily is a registered nurse who works the day shift on a bustling med-surg floor. She has a reputation for excellent communication skills and the ability to handle difficult conversations with empathy and grace, but she admits she never feels comfortable doing so. When she must have a difficult conversation, she uses a structured format to guide her to maintain her composure and empathy. Emily needed to use this framework when the physician asked her to talk to the family of Mr. Johnson about hospice care.
Mr. Johnson was a 75-year-old man admitted with advanced pancreatic cancer. His condition was deteriorating rapidly, and it was clear that curative treatments were no longer effective. Mr. Johnson's wife, Judy, was consistently by his bedside, her worry and sadness evident in her eyes. Emily knew Mrs. Johnson needed a plan because the fear of not knowing can be far worse than the reality. Emily asked her co-workers to cover for her other patients for the next 20 minutes so she could have a conversation about hospice.
Emily approached the room; she stopped momentarily and took a deep, centering breath. She released the day's stress and gave herself space to focus on this task. Emily gathered her thoughts and reminded herself of the framework she would use. She knew this conversation would be challenging but discussing the next steps in Mr. Johnson's Care was necessary. She entered the room with a warm smile, acknowledging both Mr. and Mrs. Johnson.
Emily began by asking how Mr. Johnson was feeling, allowing him to express any concerns or symptoms he was experiencing. She listened attentively, validating his feelings, and reassuring him that his comfort was a top priority.
After addressing Mr. Johnson's immediate concerns, Emily asked, "Mr. Johnson, what has the doctor told you about your prognosis?" Mr. and Mrs. Johnson began to verbalize that they knew Mr. Johnson was not getting better and was worsening. Mr. Johnson offered that the doctor told them curative care was not an option and that his prognosis may be short. Emily noticed Mrs. Johnson's eyes welling up with tears as Mr. Johnson spoke. Sensing her emotional distress, Emily offered her a comforting hand.
Emily asked, "How do you see spending your remaining time?"
Mr. Johnson quickly stated, "I want to go home."
Mrs. Johnson had a worried look on her face. Emily turned to her, and Mrs. Johnson stated, "I don't know how I can care for him at home."
Emily reassured Mrs. Johnson that this was a fear expressed by many spouses experiencing similar circumstances. Then, Emily introduced the concept of hospice care, explaining that it could provide specialized support and comfort to Mr. Johnson in the comfort of his own home. She highlighted the benefits of hospice, such as nurse visits, pain management, emotional support, and assistance with daily activities by an aide.
Understanding the gravity of the situation, Mr. Johnson and his wife looked at each other, their love and concern evident. After a moment of silence, Mr. Johnson nodded, expressing his willingness to explore hospice care to enhance his quality of life during this challenging time.
Emily continued the conversation, outlining the next steps and assuring the couple that the hospice team would work closely with them to develop a customized care plan. She provided them with a referral to hospice and assured them that she would be available to answer any questions.
As the conversation came to a close, Emily thanked Mr. and Mrs. Johnson for their trust and assured them that their decision was an essential step towards ensuring Mr. Johnson's comfort and dignity. She could see more lightness in Mrs. Johnosn's eyes. She was standing taller and breathing easier.
Emily left the room, knowing that this difficult conversation had set the foundation for a new chapter of Care focused on providing the support and compassion that Mr. Johnson and his wife deserved.
Nurse Role as Advocate
Nurses are the center of the interdisciplinary team, often providing communication and updates from patients and families to other practitioners such as social workers and physicians. The focused time they spend with patients in guided conversations and daily assessments allows nurses to gain a more in-depth understanding of the patient, family dynamics, and care goals.
A particular time of vulnerability for patients and families is during a serious illness and at the end of life. Nurses are responsible for advocating for patients' rights, respecting their wishes, and facilitating open communication between healthcare providers, patients, and their families. They play a pivotal role in ensuring the patient's voice is heard, and their needs are met.
Here are some ways nurses advocate for patients:
- Patient-centered care: Nurses help guide decision-making processes and ensure care aligns with the patient's values and goals when they ensure patients' preferences, values, and goals are at the center of their care (18).
- Shared decision-making: Nurses facilitate shared decision-making between patients, families, and healthcare providers by acting as intermediaries, ensuring patients' voices are heard and respected during discussions about treatment options, advanced directives, and end-of-life care planning (19).
- Psychosocial and spiritual needs: Nurses advocate for patients by providing emotional support, facilitating discussions about fears and concerns, and connecting patients with appropriate resources (20).
- Pain and symptom management: Nurses advocate for optimal comfort by assessing and addressing patients' physical distress, collaborating with the healthcare team, and advocating for timely interventions (21).
- Patient autonomy: Nurses who involve patients in decision-making processes, including information about treatment options, risks, and benefits, support patients in making informed choices (24).
- Informed consent: Nurses ensure patients understand the nature of their treatment, potential risks, and alternatives serve to advocate for informed consent (23).
- Healthcare disparities: Nurses who identify and address healthcare disparities based on race, ethnicity, socioeconomic status, or geographic location work toward eliminating inequitable healthcare (8,10).
By advocating for patients during these critical times, nurses can help ensure that patients’ wishes are respected, their quality of life is optimized, and they receive compassionate and patient-centered care.

Self Quiz
Ask yourself...
- How is advocacy different with hospice and palliative care patients than patients with non-serious illness?
- During your career, in what ways have you advocated for patients with serious illness?
Providing Resources
To provide comprehensive care, nurses must be knowledgeable regarding hospice and palliative care and what each provides. Educating families and patients about their options is a great way to provide emotional support and help them navigate complex medical decisions.
As part of the MHB and many other insurers, hospice care is funded 100%. As a result, hospices are required to provide a specific set of resources (15). Medicare and private insurers frequently cover the cost of a Palliative Care practitioner on a per-visit basis. Thus, Palliative Care resources can vary widely per program. Knowing what resources are available through your local palliative care program is essential. Below is a chart of common hospice and palliative care resources and their benefits.
| Resource | Hospice | Palliative | Benefits |
| MD | Yes | Yes | Palliate symptoms through medical assessment and treatment. |
| NP | Maybe | Often | Palliate symptoms through medical assessment and treatment. |
| Registered nurse | Yes | Maybe | Care coordination, assessment, monitoring, symptom management, education, and communication with interdisciplinary teams. |
| Social Work | Yes | Maybe | Assist with community resources, counseling, advance directives, and other support. |
| Chaplain | Yes | Maybe | Assist with spiritual support, counseling, and connecting patients with their church affiliation and practices. |
| C.N.A. | Yes | Rare | Assist patients with physical care such as bathing and dressing. This is often a great support to caregivers. |
| Dietician | Yes | Rare | Assist and support patient’s dietary needs. |
| Pharmaceuticals | Yes | No | Alleviate common symptoms. |
| Medical Supplies | Yes | No | Wound care, other treatments, continence, and cleanliness needs. |
| DME | Yes | Maybe | Supports a patient’s ability to be independent. |
| PT, OT, ST | Yes | Able to make referrals | Support to maintain function, non-pharmacological pain management, assistance with communication, swallowing, wound care, and ADL support. |

Self Quiz
Ask yourself…
- How do you advocate for patient’s rights and ensure their wishes are respected in your healthcare setting?
- How do you support patients and their families during difficult conversations about end-of-life decisions?
- How do you provide emotional support to patients and families in need?
- What strategies do you employ to ensure effective communication between patients, families, and the interdisciplinary team?
- How do you manage your emotional well-being when working with families and patients nearing the end of life?
Becoming a Hospice or Palliative Care Nurse
Even though Hospice and Palliative Care are different, the skills and qualities of successful hospice and palliative nurses are similar. As previously discussed, Hospice and Palliative Care payment differs, with Palliative Care primarily funded by payment to medical practitioners. Because of the funding, it is rare for Palliative Care practices to employ nurses to the same degree as hospice. Many Palliative Care programs do not have nurses in their daily practice but may have them for patient follow-up or coordination of care.
For this education, we are focused on the requirements of becoming a hospice and palliative care nurse, understanding that positions for Hospice nursing are more prolific than strictly Palliative Care nurses.
Educational Requirements
While many nurses can specialize in a specific area of care, for example, geriatric, cardiac, critical care, surgical, or emergency care, hospice, and palliative care nurses care for patients with a wide range of illnesses, ages, and abilities.
Hospice and palliative care nurses need to understand the ordinary course of numerous conditions in multi-aged patients to anticipate, prepare, and quickly palliate symptoms of the specific disease. They must be skilled in the assessment of patients and able to detect subtle changes in conditions that affect the patient’s plan of care.
Certain requirements need to be met to become a hospice and palliative care nurse (17). Here are the general requirements:
- Licensure: Current, unrestricted license as a registered nurse (RN) or licensed practical/vocational nurse (LPN/LVN) in the state where they practice. The specific licensure requirements may vary by state.
- Certification: Hospice nurses are often required to have specialized certifications related to hospice and palliative care. The most common certification for hospice nurses is the Certified Hospice and Palliative Nurse (CHPN) credential, offered by the Hospice and Palliative Credentialing Center (HPCC). This certification demonstrates expertise in providing care to patients with life-limiting illnesses. This certification requires two years of hospice experience for eligibility to take the certification test (16).
- Education and Experience: There are no specific education requirements for hospice nurses required by regulatory bodies. However, most hospice agencies prefer nurses with a bachelor’s degree in nursing (BSN) or higher. As written above, hospice and palliative care patients range in age and illness. Therefore, many agencies also prefer nurses with two years of experience in a medical-surgical healthcare setting (17).
- Training: Hospice nurses must receive comprehensive training in hospice care and be knowledgeable about the philosophy, principles, and practices of hospice and palliative care. The hospice agency typically provides this training and covers pain management, symptom control, psychosocial support, communication, and end-of-life care (17).

Self Quiz
Ask yourself…
- What is your experience with the importance of certification as perceived by patients and families?
- What is your experience with the importance of certification as perceived by healthcare professionals?
Skills and Qualities
Hospice and palliative care nurses must thrive on working independently since more than 80% of hospice and palliative care is provided in patient's homes. While hospice and palliative care are under the management of the physician, the hospice nurse is the primary assessor and at the patient's bedside.
Hospice nurses must be organized, have firm boundaries, and be able to systematize their practice to see multiple patients in one day, with the requirements of driving, documenting, communicating with the interdisciplinary team, and providing care according to the individual patient care plan. In addition, they must provide support and education to the patients and their families.
Nurses in hospice and palliative care settings require excellent communication, empathy, and the ability to navigate complex ethical dilemmas and difficult conversations.

Self Quiz
Ask yourself...
- How do you stay current on the latest research and best practices regarding caring for patients with serious illnesses or at the end of life?
- Can you describe a situation where you had to manage complex pain or symptoms?
- What additional training or education have you pursued to better manage patients with serious illnesses or near the end of life?
Conclusion
In conclusion, Hospice and Palliative Care represent two distinct but interconnected approaches to providing comprehensive medical care for individuals with serious illnesses. While hospice care focuses on terminal patients and aims to enhance their quality of life, Palliative Care addresses the needs of individuals at any stage of a serious illness.
Nurses are crucial in advocating for patients, facilitating difficult conversations, and providing resources to support patients and their families. By understanding the philosophy, eligibility criteria, and duration of hospice and palliative care services, nurses can contribute to the holistic well-being of patients in these specialized fields.
As society continues to recognize the importance of providing comprehensive end-of-life care and support for patients with serious illnesses, it is crucial to foster awareness, education, and support for hospice and palliative care services. By doing so, we can collectively work towards enhancing the experiences of those facing life-limiting illnesses, offering comfort, compassion, and dignity throughout their journey.
Navigating Difficult End of Life Conversations
Introduction
Talking about death is generally difficult for the average person. It is even considered taboo in some cultures or situations. For some nurses, having end of life conversations is a routine part of the profession. A hospice nurse, for example, carries the responsibility of managing care for a dying patient, and ultimately informing the patient’s family that death is imminent.
A lack of training, experience, or confidence in this area could result in poor delivery, unrealistic expectations, and an overall negative dying experience. Most people do not have experience or even a baseline when it comes to death and dying. This makes end of life conversations much more important in the delivery of patient care.
Perspectives About Dying and Death (Philosophical, Psychological, and Spiritual)
Philosophical
The human experience of death and dying is not one sided. On the contrary, there are many things to be considered to understand it fully. This goes beyond a scientific approach. An understanding of philosophical reasoning related to death is imperative to provide a thorough explication of the human dying experience. Historically, death has been an intrinsic part of life throughout various civilizations.
Ancient Egyptians spent much time preparing for the next life. Life was perceived as a dream that passed quickly. Death was viewed as eternal. Egyptians believed that the dead would make their way over to The Kingdom of Orisis, where they would spend eternity.
Ancient Greek civilization also viewed death in a particular light. According to San Filippo, “Greeks perceived death as a release of the soul from the body. The soul, which was considered to be part of the mind, was believed to be immortal. It was considered that the soul lived before the body and would live again in another life” (1).
Lastly, it has been noted that when it comes to fearing death, people create philosophies and theologies due to an inability to visualize our own death and afterlife.
Psychological
The psychological aspect of death is just as important as the physical. The thought of death alone has the potential to evoke various memories and feelings. You will typically find that a person either accepts or fears death (positive outlook vs negative outlook). This can be a fear of suffering, pain, or of the unknown. These views are typically formed based on past experiences with death.
Often, a person may have no underlying baseline when it comes to dying or death. That first experience with death can potentially shape someone’s entire perspective. Fearing death could be attributed to a fear of the unknown, lack of relatable experience, a negative experience, or a lack of communication regarding death, due to a cultural taboo, for example.
On the other hand, things like faith, positive experiences, and imminent death may cause someone to be more accepting of death. Often, someone facing imminent death may be forced to think about it and come to terms with it. In a study of terminally ill patients facing death, “The participants were afraid of death and earnestly desired to live but felt that death was imminent. To escape their distress, they attempted to accept the situation by thinking that all lives are finite, and death had to be accepted” (2). This is an example of coming to terms with an impending death and accepting it.
Spiritual
Spiritual perspectives on death should be considered when discussing views on dying. History shows that humans have long held beliefs that life does end when the body dies. Many tend to believe that once a person dies, their soul is then freed, and can go on to another life or be reincarnated into someone or something else. Religious ideologies contain a vast amount of knowledge and wisdom regarding death. “Religion and spirituality help individuals make sense of what awaits them near the end of life and help the dying cope with their terminal condition” (7).
What happens after death may vary from one religion to the next. Many religions also have a heaven or heaven like final place where the deceased can rest and be with other who have also died. One of the oldest ideologies of human history is the belief that there can be life after death.

Self Quiz
Ask yourself...
- Historically, how has death been viewed in different civilizations?
- Why might a patient fear death and dying?
- What causes patients to be more accepting of death?

Impact on Nurses
Imagine working as a hospice nurse. Your sole purpose is to provide end-of-life care for terminally ill patients. This includes providing information on what to expect at the end of life. At any given time, you have patients that could be imminently dying.
You are a source of knowledge and comfort for a patient and their family during this time. In the end, you will likely be there when the patient takes their last breath. How can one prepare to handle this scenario time and time again? Should a nurse feel sadness for a patient that was expected to die, or should they emotionally separate themselves?
The latter may prove hard to do. The reality is that nurses are frequently exposed to death and dying in a variety of settings. A patient’s dying process can be planned or not and this distinction may mean different things for different people. Typically, nurses are taught skills to help prevent death.
This may be a hard thought process to overcome when the goal is not curative, but comfort focused. These patient interactions help to shape a nurse’s feelings on death and dying. “Nurses are frequently exposed to dying patients and death in the course of their work. This experience makes individuals conscious of their own mortality, often giving rise to anxiety and unease.
Nurses who have a strong anxiety about death may be less comfortable providing nursing care for patients at the end of their life” (3). This ‘death’ anxiety could lead to disastrous outcomes for both the nurse and the patient. Nurses should be aware of their own thoughts and attitudes towards death, and how these could affect their ability to provide patient care.
Caring for the dying involves both skill and emotional support from nurses. Younger nurses and nurses with less experience with death may have greater difficulty caring for dying patients. End of life education and an introspective look at oneself are imperative when it comes to providing quality care. “Nurses’ professional experience is positively correlated with their position, professional level (rank), EOL care experience, competence in EOL, and another knowledge.
Nurses who have a positive attitude seem more likely to have more competence in dealing with patients’ symptoms at EOL and better knowledge of EOL care (3). The more palliative knowledge nurses had, the more competence they felt. Moreover, competence dealing with patients’ symptoms in EOL care was correlated with older nurses” (8). Positive conversations about death and dying usually lead to a positive dying experience.
To reach this point, nurses and other healthcare professionals need to know how to have these conversations. In a society that is so focused on the living, receiving education on death can be difficult. When death is perceived as a part of life, only then will people feel more comfortable talking about it.

Self Quiz
Ask yourself...
- What role do nurses play in death and dying?
- In what ways are nurses affected by death?
- How do previous experiences shape our views about death?
- What are some potential indicators of a nurse’s ability to provide quality care at EOL?
Communication Strategies
Many people are uncomfortable talking about death and dying and tend to shy away from such conversations. This may also be true for nurses. Talking about death should not be a formidable task. Nurses should be able to comfortably implement these conversations in their practice when needed. Effective communication is imperative throughout a patient’s trajectory.
Conversations about death and dying can impact patient care. “Research has shown that talking about and planning the EOL is important for how the final days in a patient’s life may play out and is associated with reduced costs as well as a higher quality of care in the final weeks of life” (4). In a society so focused on life, it may be difficult for nurses and other health professionals to obtain the skills needed to confidently speak with patients about death.
To effectively talk to patients about death, nurses should first be willing to initiate and discuss the topic. There are important strategies to remember when talking about the end of life. “Qualitative research on the end of life has revealed that medical personnel should consider the following strategies when conducting EOLD: open and honest conversation, setting treatment goals, and balancing hope with reality” (13).
Patients should also be encouraged to express their thoughts, fears, and to ask questions. It is also important to be honest and forward with patients. No “beating around the bush”. This means using words like “dying” and “death” while having these conversations.
One communication strategy, VALUE, “recommends to value and appreciate statements of family members, acknowledge their emotions, as well as to listen and ask questions to understand who the patient was as a person” (9). Nurses should keep the following in mind: a patient’s comfort level with death, goals of care, expectations, and cultural factors. Having this knowledge will help to guide the conversation.
Lastly, when a nurse feels confident and exhibits calmness while talking about death, a patient will more than likely feel the same way.

Self Quiz
Ask yourself...
- How do conversations about death impact patient care?
- What can nurses do to effectively communicate with their patients about death?
- What strategies should be utilized when talking about death?
Stages of Grief
Nurses are not immune from experiencing grief or loss. We mourn personally and we mourn alongside our patients and their families. “Grief and loss are something that all people will experience in their lifetime. The loss may be actual or perceived and is the absence of something that was valued. An actual loss is recognized and verified by others while others cannot verify a perceived loss.
Both are real to the individual who has experienced the loss. Grief is the internal part of the loss; it is the emotions related to the loss” (4). Grief allows a person to begin to deal with the pain associated with loss and to heal. There are five stages of grief which were identified in Dr. Elisabeth Kübler-Ross in her book Death and Dying.
- Denial: This stage Is not necessarily about denying that the loss happened. Instead, it is more about denying the feelings associated with the loss. Denial lets us face our feelings of grief. “As an individual is able to accept that this loss is their reality, they will be able to move into the healing process and denial will begin to diminish” (5).
- Anger: A grieving person may feel anger towards a variety of people associated with the loss. This is a normal and a necessary part of the healing process. “Under the anger is the individual’s pain. Anger provides structure, and that is better than preceding numbness. It can be a challenge for some to feel the anger; sometimes it is easier to try and suppress the anger. Feeling anger and addressing anger is part of the grieving process” (5).
- Bargaining: Grieving people may begin to say things to themselves like, “If this__, then this __”, or “I will do anything if you take the hurt away” (5). This stage may occur at any point in the grief process. Once this step is reached, the person can begin to move through the stages in different ways.
- Depression: This stage involves a realization that the situation is real. “Empty feelings come forward, and one’s grief moves in on a deeper level than before. This type of depression is not a sign of mental illness; although reaching out for help may be the right step. It is an appropriate response to a great loss. An individual may withdraw from their daily life activities, and they may feel a fog of intense sadness” (4). Depression after a major loss is normal and necessary in the healing process.
- Acceptance: Entering this final stage does not mean one is completely okay with what has happened. In fact, one may never be as they once were prior to the loss. “Acceptance, as a stage, is about accepting that this is their new reality, and it is permanent. Life cannot go on as it once did, but through acceptance, life can and will go on” (5). Individuals in this stage must realize that change is necessary to adjust to the new normal.
Not everyone experiences grief in the same way. Grief is a very personal experience that affects people in different ways. Nurses should be familiar with the stages of grief to be able to offer optimal patient care to grieving patients and their families. This includes recognizing signs of depression and possible suicidal ideation, providing empathy, compassion, education, and resources to those in need.

Self Quiz
Ask yourself...
- What are the stages of grief?
- Why should nurses be familiar with the stages of grief?
- What purpose does grief serve?
End of Life Process
Phases of Dying
Although everyone experiences death differently and on their own terms, there are two main pathways that most people take before dying. The dying process can be broken up into two phases: the transitioning phase, and the actively dying phase. The amount spent in each phase varies from person to person.
The transitioning phase usually begins 2-3 weeks prior to death. Major changes in function and the ability to do activities of daily life are observed during this time. Patients may even begin falling prior to entering this phase. Becoming bedbound is common as one will begin to spend most of their time sleeping.
This means decreased responsiveness, less interest in normal activities and hobbies, decreased interaction with family and friends, and an overall decline in one’s interest in external factors. It is possible to be roused during this phase, but this may only be possible in short intervals. It is not uncommon for transitioning patients to speak to or about loved ones that have already passed away. They may even report seeing deceased family in the room with them (11).
This should not be feared and is an important part of a person’s dying process. Incontinence may also begin during this time and briefs will be needed. Perhaps one of the most noticeable and difficult changes to witness, especially by friends and family, is changes in appetite. Patients will begin to show less interest in food and liquids. A greater difficulty swallowing will become apparent. “Refusal of food and fluid by a dying person is a common occurrence, particularly as the body slowly shuts down, and this may be the evidence signifying an actively dying process rather than starvation” (11).
Lastly, symptoms like restlessness, agitation, and pain may arise and detract from one’s comfort level. Although most patients will spend about two weeks transitioning, time can vary from days to weeks. The transitioning phase can also be skipped altogether, depending on the person.
Once the transitioning phase has concluded, the actively dying phase will begin. Actively dying immediately precedes death. This phase is usually short, lasting about 48 hours. Once actively dying, death is imminent, and a patient is expected to pass away at any moment. This phase is markedly different from the previous phase, and symptoms tend to become more apparent. “The following five changes constitute objective evidence of the end of life: diminished daily living performance, decreased food intake, changes in consciousness and increased sleep quantity, worsening of respiratory distress, and end-stage delirium” (12).
One key difference is one’s ability to response to tactile or verbal stimuli. The actively dying patient is obtunded and no longer responds to external forces. There could be slight reactions, but nothing meaningful. This is a comatose state.
There are many observable changes, including changes in vital signs. Blood pressure begins to drop, heart rate speeds up and eventually slow, respiratory rate picks up, and temperature may become elevated. Respiratory differences tend to be the most common observable changes. Cheyne-Stokes may occur, and the overall breathing pattern can be very irregular. Apnea is also common (11).
Many patients experience what is known as the “death rattle”. This very noticeable sound is due to an accumulation of secretions in the upper airway. This is a hallmark of the actively dying phase, but it is not experienced by everyone. “Death rattle is a strong predictor of imminent death, and nearly 80% of people die within 48 hours after its onset” (11).
Skin changes also occur. The body may become cool to touch, cyanosis may develop in the nail beds of fingers and toes, and mottling can occur usually beginning in the lower extremities and later spreading to other parts of the body. Skin may also become very pale. Urine output will decrease and become concentrated as evidenced by an amber color.

Self Quiz
Ask yourself...
- What are the dying phases?
- What changes are observed when someone is transitioning?
- What are some expected physical changes in the active dying phase?
- What education should a nurse provide to someone taking care of a patient that is actively dying?
Nursing Assessment and Care
Since there are so many drastic changes observed during the transitioning phase, proper education is crucial for caregivers. Nurses should reassure them that what the patient is experiencing is normal and to be expected. “At the end of life, most patients are in a state of lethargy, wherein their consciousness progressively declines, and sleep duration increases; therefore, it is necessary to provide appropriate explanations to patients and their families so that they can accept these symptoms as part of the natural end-of-life process” (12).
Family members usually try to wake the sleeping transitioning patient and have them attempt activities that could be done in the past. This is dangerous for the pt and can lead to injuries and more agitation. Becoming bedbound is a major change and puts the patient at risk for pressure injuries and increased pain. Fragile skin combined with new episodes of incontinence are topics that should be discussed, and proper supplies should be used.
Other potential barriers to a peaceful transitioning period are force feeding and aspiration. Nurses should provide education on what is acceptable and needed at this point. Patients will not die of hunger or lack of water. Allowing the patient to eat and drink small amounts is okay (12).
This amount will decrease as the body starts shutting down. Ice chips can be used while the patient is still alert. Utilizing mouth swabs with water is enough to hydrate the oral cavity and keep the patient comfortable until the end. During this time, symptoms can seemingly come out of the blue.
A once calm patient can become highly agitated in a short period of time. Medications should be added timely to ensure that the patient has a peaceful death. Information on medication and interventions to control uncomfortable end of life symptoms like pain, agitation, and restlessness should be provided to caregivers. Hospice patients, for example, have a comfort kit with various medications to use during this time.
Medications can be used as needed or scheduled to keep patients comfortable. (12). As the patient enters the actively dying phase and becomes less alert and aware, it is important that friends and family continue to talk to the patient and keep conversations positive around the patient. Hospice nurses, for example, are sure to tell caregivers that hearing is the last thing to go, so they should continue to speak to their loved one. Since vital signs start to become abnormal, reassurance is usually needed to keep family comfortable.
Not all vital signs need to be taken in the final stages. Taking blood pressure, for example, could cause discomfort. Death education related to respiratory changes is imperative. “Abnormal breathing patterns such as shallow breathing sound become increasingly common starting 1 week before death” (12).
Caregivers should be informed that breathing too fast or too slow at this point is not an emergency and there are things that can be done to promote comfort like applying oxygen, keeping the head of the bed upright, and keeping the room cool. Medications can also be given to decrease the death rattle. It should be noted that patients do not experience discomfort from the death rattle.
Lastly, not having a bowel movement or passing urine during the last few days of life is normal and interventions are not needed. Education and support are especially important during the final phases of life. With their peaceful words and deep knowledge base, nurses can be instrumental in facilitating a peaceful death.

Self Quiz
Ask yourself...
- Is it reasonable to obtain vital signs every two hours? Why or why not?
- If the family expresses concern about changes in bowel or urinary habits, what can you say to reassure them?

Resources and Support
Planning, coordinating, and executing quality end of life care can be challenging for health care workers. This period can also be one of the most challenging times for both patients and their loved ones. There are available resources for health care workers, patients, and their loved ones that provide information on end-of-life care.
Hospice care is an invaluable resource and source of support. This is available to terminally ill patients with a life expectancy of 6 months or less.” Hospice care is the term given to the care provided when a patient is given a prognosis of death within 6 months, and they do not pursue curative treatments They focus on improving the quality of life which can mean many things” (10).
Care can be provided in any setting that a patient calls home. The hospice team includes a medical director, registered nurse, chaplain, social worker, home health aide, and often a nurse practitioner. Symptoms and care can be managed at home with the help of covered medications, supplies, and medical equipment. Hospice allows patients to reach their goal of dying peacefully at home. A bereavement team also provides support during the process. (10?)
Palliative care, another form of comfort care, can also be utilized to maintain comfort at the end of life. Unlike hospice, patients receiving palliative care do not need to have a life expectancy of 6 months or less. “Research found that timely EOL care discussions allowed family members to make use of hospice and palliative care services sooner and maximize their time with the patient” (6).
Nurses should be educated in other end of life resource topics such as advanced directives, POLST (Physician Orders for Life Sustaining Treatment), and Durable Medical Power of Attorney. Looking ahead and having meaningful discussions regarding end-of-life planning can help prevent the stress of needing to address these things when death is imminent.

Self Quiz
Ask yourself...
- What care options are there for patients at the end of life?
- What is the difference between palliative and hospice care?
- What tools can the nurse use to help patients in end-of-life planning?
Conclusion
End of life conversations have a profound impact on not only patient care, but also on the dying process itself. Research shows that when implemented appropriately, these conversations improve patient relationships with healthcare workers, lead to better outcomes, and allow for a more positive dying experience. Nurses play a critical role in end-of-life processes in many different settings. With education, practice, experience, and confidence, nurses can incorporate conversations about death and dying to provide quality care.
➀ Read and Learn
The following course content
Introduction
Ventilator management can be an intimidating subject, especially if the user is not savvy with technology. Fortunately, modern ventilator manufacturers have put significant effort into making ventilators “user-friendly”. This course will further support those who manage ventilators. We will discuss basic respiratory function, the types and mechanism of action of ventilators, and indications for use. It is also important to gain understanding of the settings, modes, alarms, and essential nursing care.
Ventilator Fundamentals
Mechanism of Action
Knowledge of basic respiratory function is essential for understanding mechanical ventilation (MV). The respiratory system is comprised of the airway, lung, and chest wall. Respiratory mechanics represents the lung function in terms of pressure, gas flow, and volume (1).
Pressure refers to the physical movement of the lungs and chest wall muscles. During spontaneous and unassisted inspiration, our lungs expand due to the transpulmonary pressure caused by negative pleural pressure that is created by the inspiratory muscles (2). Essentially, the lung spontaneously pulls inwards while the chest wall pushes outwards.
Gas exchange refers to the process of transferring atmospheric oxygen (O2) from the alveolar gas into the bloodstream and carbon dioxide (CO2) from the bloodstream transferred to the alveolar gas phase; CO2 is then eliminated into the atmosphere by ventilation (1). Gas exchange occurs within areas of the lung lined by alveoli, which are tiny air sacs encased in capillary beds (1).
Volume simply refers to the amount of airflow, which is affected by factors such as lung elasticity, space to expand, presence of fluid, and surface tension.
The mechanism of action of mechanical (artificial) ventilation had evolved over time. The first type of mechanical ventilators provided negative pressure ventilation, which applied external negative pressure to mimic chest muscle pressure (1). Although it was helpful and prolonged life to many patients, this method was not effective for gas exchange abnormalities.
Controlled positive pressure ventilation was first applied in 1952 and pushes air into the central airways, causing air to flow into distal airways and alveoli (1). Positive pressure does not work in the same way as spontaneous respiration, which is negative pressure. This forced airflow provides the encounter for gas exchange to occur. This airflow also provides pressure that prevents the alveoli from collapsing.
Types
As we discussed, modern mechanical ventilators apply positive pressure that pushes air into the lungs. The types of positive pressure ventilators include invasive and noninvasive.
Invasive Mechanical Ventilation. Invasiveness refers to the intrusion of medical instruments into the body. In invasive ventilation, a tube from the ventilator is connected to the airway. When a tube enters the mouth and into airway, it is called intubation. A tracheostomy is utilized when the tube must enter the airway through the trachea (2).
Noninvasive Mechanical Ventilation. A noninvasive ventilation type is less intrusive into the body cavities. A facemask with straps is typically used.

Figure 1. Algorithm for Types of Ventilation. Photo credit: (1)
Understanding Ventilation Terminology
Ventilation describes the bulk movement into and out of our lungs (3). Ventilation can be categorized into tidal volume (VT), respiratory rate (f), and minute ventilation (VE). Tidal volume is the volume of gas exhaled following a normal inspiration; respiratory rate is the number of breaths taken over one minute; minute ventilation is the tidal volume times the respiratory rate (3). These will be important terms as we review mechanical ventilator settings and modes.
Ventilator capacity refers to the amount of air that a ventilator pump can push into the lungs. The ventilatory capacity is significant because this amount must be sufficiently maintaining tissue oxygenation and carbon dioxide (CO2) removal (3). When you hear the term respiratory drive, think about the neurological system driving the respiratory vehicle. Essentially, breathing is generated by neuron activity located in the brainstem, which produces a neural signal directed to respiratory muscles to create inspiratory effort and tidal breathing (4). There are receptors that monitor carbon dioxide levels in the body and when a high level of carbon dioxide is detected a signal is sent to stimulate the drive to breathe to blow off the excess carbon dioxide (5). Essentially, the level of carbon dioxide dictates the drive to breath and the respiratory rate.

Self Quiz
Ask yourself...
- Have you ever cared for a patient on a mechanical ventilator?
- Can you explain how the physiology of the lungs (airway, alveoli) impacts gas exchange?
- Can you describe the difference in pressure between spontaneous breathing and mechanical ventilation?
- The nervous system is a vital part of the breathing process. Have you ever performed a neurological and respiratory assessment with abnormal findings?
Indications for Use
Mechanical ventilation is indicated when spontaneous breathing is insufficient (tachypnea, hypercapnia) or absent (apnea). Respiratory failure is the inability of the heart and lungs to adequately supply the tissue with oxygen and remove carbon dioxide (3).
Indications for Invasive Mechanical Ventilation
Compromised or Diseased Airway: (4)
- Trauma to airway
- Oropharyngeal infection.
- Proximal airway obstruction
- Angioedema
- Anaphylaxis
- Distal airway obstruction
- Asthmatic bronchospasm
- Acute exacerbation of chronic obstructive pulmonary disease (COPD).
Hypoventilation: (4, 5)
- Impaired central drive
- Pharmacology or illegal drug overdose
- General anesthesia for surgery
- Traumatic brain injury
- Respiratory muscle weakness
- Muscular dystrophy and myositis
- Peripheral nervous system defects
- Guillain-Barré syndrome
- Myasthenic crisis
- Restrictive ventilatory defects
- Trauma or impact to chest wall
- Pneumothorax
- Pleural effusion
Inability to exchange oxygen or delivery to the peripheral tissues (hypoxemic respiratory failure): (4)
- Alveolar unable to fill.
- Pneumonia
- Acute respiratory distress syndrome (ARDS)
- Pulmonary edema
- Pulmonary vascular insufficiency
- Massive pulmonary embolism
- Air emboli
Failure to meet increased ventilatory demand: (4)
- Severe sepsis
- Shock
- Severe metabolic acidosis
Indications for Noninvasive Pressure Ventilation
Noninvasive pressure ventilation attempts to deliver oxygen to the lungs without endotracheal intubation (1).
Before intubation
- Acute exacerbation of COPD
- Hydrostatic pulmonary edema
- Asthma
- Bronchoscopy
- Chest Trauma
Used instead of invasive mechanical ventilation (intubation)
- Acute respiratory failure (ARF) [According to the latest ATS/ERJ (American Thoracic Society and European Respiratory Society) guidelines from 2020] (4)
- BPAP for acute or acute-on-chronic respiratory acidosis secondary to COPD exacerbation where pH < or = 7.35 (8)
- BPAP or continuous positive airway pressure (CPAP) for cardiogenic pulmonary edema (8)
- Obesity hypoventilation syndrome (1)
- Obstructive sleep apnea (4)
- Restrictive thoracic disorders (4)
**ATS/ERJ guidelines carry a conditional recommendation for the following in the setting of ARF:
- Early NIV (non-invasive ventilation) for immunocompromised patients with ARF
- Palliative care for terminal conditions
- Chest trauma patients with ARF
Following Intubation
- Post-operative ARF
- Preventative measure in high-risk patients following extubating.

Self Quiz
Ask yourself...
- Can you think of certain populations or diseases that are at a high risk for needing mechanical ventilation?
- Have you experienced caring for a patient following general anesthesia?
Ventilator Settings
Knowledge of the settings on mechanical ventilators is critical for care. Each parameter should be initially determined and adjusted based on the patient’s condition and unique needs. This is within the scope of practice of qualified physicians and respiratory therapists only. The nurse should know the settings and include them in the nursing handoff report.
There are several types of ventilator settings to be familiar with, including the following:
- Tidal Volume
- FiO2
- Respiratory Rate (Frequency)
- PEEP
- Mode
- Alarms
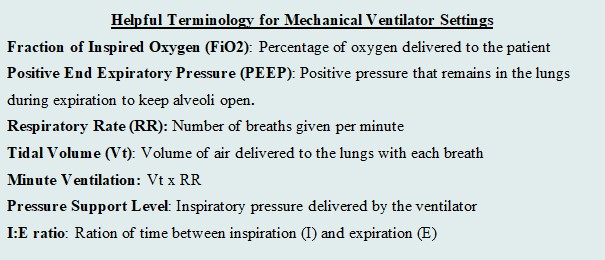
Figure 3. Helpful Terminology for Mechanical Ventilator Settings. (Designed by course author)
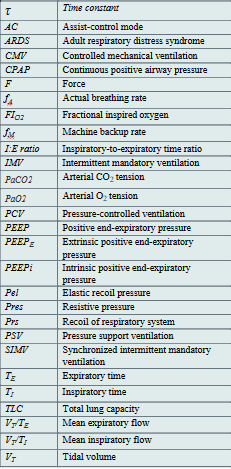
Table 1. List of Abbreviations for Ventilation. (1, 2, 5) (Designed by course author)

Self Quiz
Ask yourself...
- Are you familiar with the settings of mechanical ventilator?
- Have you ever cared for a patient that needed to “wean” from something, such as medication, addiction, etc.?
- Consider the feeling of wearing a breathing mask. How can the nurse provide physiological and psychological support?
As we discuss the settings, it is important to recognize short and long-term goals of mechanical ventilation. Short-term goals prioritize airway, breathing, circulation (ABCs) and maintaining respiratory gas exchange. Long-term goals should focus on weening and encouraging the patient to have a safe return of spontaneous breathing if possible. Independence should be a goal in certain circumstances.
The settings will reflect the minimal amount of assistance to maintain perfusion. Evidence supports the concept that hyperoxemia increases the risk of mortality in critically ill patients (2). An excess of oxygen is dangerous, as it can reduce respirations and heart rate. Tidal volume refers to the volume of air that is inhaled and exhaled from the lungs during spontaneous breathings, so the tidal volume setting determines the amount of the air delivered to the lungs by the machine (2).
Fi02
Fi02 stands for fraction of inspired oxygen. The range is 21% - 100% (Will). The Fi02 should be set to the lowest level to maintain a pulse oximetry (SP02) of 90% to 96% (2). A patient may initially require an FiO2 of 100% when mechanical ventilation is initiated, but the goal is to gradually wean the FiO2 percentage down to the lowest possible level that still provides adequate oxygenation for the patient. Research supports that a patient who receives mechanical ventilation with an Fi02 greater than 60% for an extended period of time is at greater risk of oxygen toxicity (1).
Positive End Expiratory Pressure (PEEP)
The PEEP settings refer to the positive pressure (greater than the atmospheric pressure) that will remain in the airways at the end of the respiratory exhalation (1). PEEP serves to distend the distal alveoli and prevent collapse. Imagine a balloon that you would like to keep inflated but air continuously seeps out. PEEP would determine the appropriate pressure to keep the balloon inflated. There are two types of PEEP: extrinsic and intrinsic (or auto-PEEP). Pressure that is applied during an inspiration is known as pressure support.
Extrinsic PEEP (PEEPe), or applied PEEP, is a setting on the ventilator and typically selected upon initiation of mechanical ventilator. Extrinsic PEEP ranges to small/ moderate (4 to 5 cmH2O) to high (>5 cmH2O). The level of PEEP is usually set at 5 cmH2O and titrated based on the underlying condition and oxygenation or perfusion needs (2). There is research and evidence-based guidelines to guide healthcare providers in properly setting and adjusting the PEEP on the mechanical ventilator. For example, in ARDS, there is a specific level of PEEP titrates according to regulatory evidence and guidelines.
Intrinsic PEEP, or auto-PEEP, refers to an incomplete expiration prior to the initiation of the next breath, which causes trapping and accumulation of air (2). If auto-PEEP is found, steps should be taken to stop or reduce the pressure build-up.
Respiratory Rate (RR)
Respiratory rate (RR) is the setting that simply determines how many breaths are delivered by the ventilator per minute. The RR is typically set at 12 to 16 breaths/minute (2). Certain circumstances warrant a higher RR (up to 35 breaths/minute). Higher RR is sometimes selected to achieve adequate minute ventilation. Examples include patients with ARDS, which would protect lung integrity and avoid severe hypercapnia, and patients with acidosis (2). Respiratory acidosis usually occurs due to failure of ventilation and accumulation of carbon dioxide, so increased respiration rate be used to balance acidosis (5). Important nursing implications are to closely monitor ABGs and titrate as ordered.
Flow Rate
The inspiratory flow rate is a rate that controls how fast a tidal volume is given by the ventilator; the setting can be adjusted depending on the patient’s inspiratory needs. The normal inspiratory flow rate should be set at around 60 L/min (2). In circumstances such as obstructive diseases, the ventilator can deliver up to 120 L/min if a patient needs a prolonged expiratory time (2). If the flow rate is set too low, it could cause unsynchronized patient-ventilator flow and an increased work of breathing; if the flow rate is set too high, it could result in lower airway pressure (2).
Respiratory therapists are an incredible resource and should be notified, as well as the physician, if this is suspected. Ventilator alarms are an essential tool for assessing inappropriate settings, we will discuss alarms later in the course. Please review the image below for a visual aid.

Self Quiz
Ask yourself...
- Can you think of professionals in your workplace that are qualified to adjust the settings on a mechanical ventilator?
- What do you think the respiratory rate should be set to?
- What do you think the inspiratory flow rate should be set to?
- Do you think positive pressure is greater than or less than atmospheric pressure?
Ventilator Modes
Mechanical ventilation without patient effort is delivered by the ventilator with control of either volume or pressure. Volume and pressure-controlled ventilation modes differ from one another based on transpulmonary pressure generation (5). There are three basic ventilatory modes based on respiratory cycles to consider: Assist/Control ventilation (A/C), Pressure Support Ventilation (PSV) and Synchronized Intermittent Mandatory Ventilation (SIMV) with PS, which is a hybrid mode of the first two (1).
Interpreting Waveforms
Scalars and Loops. Modes are depicted and illustrated as waveforms. Ventilator waveforms are graphical descriptions of how the ventilator is delivering a breath to a patient. These include scalars, which are graphics that illustrate the entire breath from the beginning of inspiration to the end of expiration, and loops, which are graphics that represent either pressure or flow, and plotted against the volume during a breath (1). Most ventilators have three scalars displayed on the main screen: flow versus time, volume versus time, and pressure versus time (1). There are typically two loops: pressure-volume and flow-volume. It is vital that the bedside clinician can interpret these scalars and loops to understand if the patient’s ventilation demands are met.

Figure 4. Example of Volume vs Time Scaler. Photo Credit: (9)
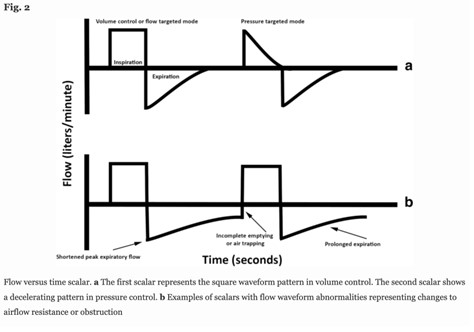
Figure 5. Example of Flow versus Time Scaler. Photo Credit: (9)
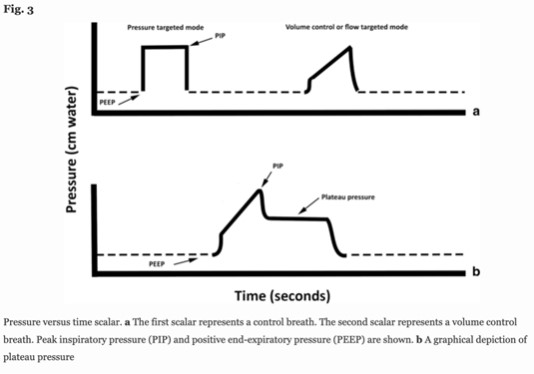
Figure 6. Example of Pressure versus Time Scaler. Photo Credit: (9)

Figure 7. Example of Pressure-Volume Loop. Photo Credit: (9)

Figure 8. Example of Flow-Volume Loop. Photo Credit: (9)
Volume and Pressure Controlled Modes
Monitoring respiratory mechanics in dynamic or stagnant conditions is extremely important to lung protection and adequate respiratory care. We will review the characteristics of volume and pressure-controlled modes.
Controlled mechanical ventilation (CMV) is when the ventilator controls one variable from the equation of motion, either flow (𝑉) or airway pressure (Paw) during the inspiratory phase. The flow or pressure must be a variable, because the others are constants: Rrs and Crs are intrinsic properties of the respiratory system, V(t) is the instantaneous volume above end-expiratory volume, PEEP is the end-expiratory pressure, and Pmus represents the pressure generated by inspiratory and expiratory muscles (1). Essentially, in this equation, the ventilator determines either the volume or the flow.
Paw(𝑡) = 𝑉(𝑡) / 𝐶𝑟𝑠 + 𝑅𝑟𝑠 × 𝑉 (𝑡) + PEEP – 𝑃𝑚𝑢𝑠 (𝑡)
This formula serves as a foundation for the common mechanical ventilator modes: Volume and Pressure Controlled.
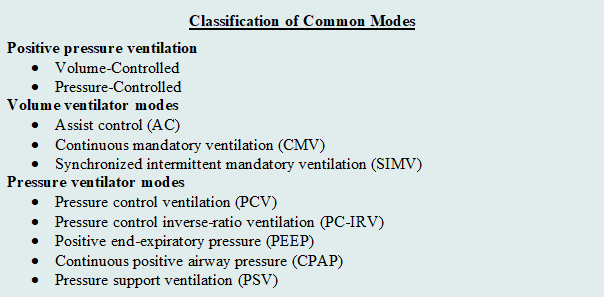
Figure 9. Classification of Common Modes. (Designed by Author)
Selection of mode differs from settings, as the mode of mechanical ventilation refers to the characteristics and phases of ventilation. The characteristics or phases mainly include trigger, cycle, and limit. (2)
Trigger: How does inspiration begin? The trigger is a type of signal that initiates the inspiratory phase by the ventilator.
- Patient-triggered: patient’s inspiratory effort triggers the ventilator to begin the inspiratory phase.
- Time-triggered: a time interval is set on the ventilator to begin the inspiratory phase.
Cycle: How does the inspiration end? The cycle is a type of signal that ends the inspiratory phase by the ventilator.
- Volume-cycled ventilation: the inspiratory phase ends when a set volume exits the ventilator.
- Pressure-cycled ventilation: the inspiratory phase ends according to a set driving pressure, airway resistance, lung compliance, and inspiratory effort of the patient.
- Time-cycled ventilation
Limit: When should inspiration be aborted? The limit is a set value (e.g., pressure) on the ventilator that should not be exceeded. If the preset limit is exceeded, the inspiration will be aborted. (2).
Volume Controlled (ACV/ VCV)
When you hear “volume”, think amount. The main characteristic of volume-controlled ventilation (VCV) is the delivery of fixed tidal volumes (1). The clinician sets the volume and how often it is delivered. Considering the respiratory rate is also set, minute ventilation is guaranteed. Essentially, this mode is driven by the amount of air entering the patient’s airway and how often. Inspiratory airway flows in predefined flow waveforms and the most common is square (1).
A max flow rate of the air being delivered is also set—think of it as the “speed” of the air being pushed into the lungs. The time it takes to deliver the inspiration will change because of the max flow rate that is set on the ventilator (1). If the flow rate is higher, the the inspiratory time of the breath to deliver the set volume will be shorter as a result.
It may be more likely nurses will be exposed to this type of mode in critical care settings. Volume-controlled ventilation (VCV) was the most used ventilatory mode in critical care when surveys were completed; however, both pressure-controlled and pressure-support modes have been reportedly utilized more frequently in recent years (1). VCV is primarily used when the patient is unable to breath on their own and essentially no spontaneous breathing occurs. VCV has also been the traditional controlled ventilation mode with anesthesia (3).
The concern of VCV is the constant flow may cause high peak pressures and increases the patient’s risk of barotraumas. Barotrauma is defined as physical tissue damage caused by a pressure difference between a closed space inside the body and the surrounding gas or fluid (7). Imagine trying to inflate a balloon in a glass bowl, if the pressure pushing air into the bowl continues and the glass bowl will not let it expand, the balloon itself will be damaged. Due to these risks, patients with lung disease and neonatal patients are not ideal candidates for this type of mode.
The nurse can gather information, such as the volume that is delivered per breath. If the volume is set at 4.5 liters, at a rate of 18, then the volume delivered with each breath will be 250mls per breath (4500mls / 18 = 250mls). The inspiratory time may fluctuate. The nurse must critically think and become aware of ventilation demands, considering factors including the set tidal volume, respiratory rate, and max flow rate. At end of shift nurse reporting, the nurse should communicate the following: mode, rate, tidal volume, fraction of inspired oxygen (Fi02), PEEP, and pressure support (PS).
Pressure Controlled (PCV)
In pressure-controlled ventilation, there is a set airway pressure for a given inspiratory time. Remember that the ventilator is programed with certain constants (specific setting and should not change) and variables (fluctuates based on constant settings). In the PCV mode, the peak airway pressure is constant (inspiratory pressure + PEEP) while the tidal volume is variable and can fluctuate depending on patient characteristics (compliance, airway/tubing resistance) and driving pressures (3). The clinician sets the inspiratory pressure level, PEEP, I:E ratio, respiratory rate, and FiO2.
Pressure-controlled mode provides the following advantages over volume-controlled breaths:
- Lower peak airway pressures to deliver the same volume amount.
- More efficient volume distribution within the lungs
- Better oxygenation
- Less risk of barotrauma
- Ability to ventilate every patient type.
As mentioned, PCV has a lower risk of barotrauma, so patients who already have lung disease and tissue damage are not appropriate for this type of mode. The tiny lungs of infants also have greater impact of tissue damage if barotrauma occurs. Nurses within the neonatal intensive care unit (NICU) may be more likely exposed to Pressure-controlled ventilation modes. PCV has become the standard approach to ventilation in the early days of neonatal care in small preterm infants, making it the prevailing mode of ventilation in the NICU in many parts of the world, including the US (3).

Self Quiz
Ask yourself...
- What are reasons for depicting the modes in waveforms?
- Can you name the three phases/characteristics of respiration that we discussed?
- What do you think the difference is between pressure and volume-controlled ventilation?
- Can you explain why pressure-controlled ventilation has a lower risk of barotrauma than volume-controlled ventilation?
Continuous Positive Airway Pressure (CPAP)
Continuous positive airway pressure (CPAP) is a type of positive airway pressure for patients that are breathing spontaneously. The goal of CPAP is to maintain a continuous pressure to constantly stent the airways open (7). If you recall, positive end-expiratory pressure (PEEP is the pressure within the alveoli at the end of expiration. CPAP is a method of maintaining PEEP and preserving the set pressure in the airway throughout the respiratory cycle. It is measured in centimeters of water pressure (cm H2O) (7). CPAP is aimed to prevent airway collapse in patients at risk. CPAP alone is often inadequate for supporting ventilation, but helpful for non-invasive ventilation. CPAP can support oxygenation via PEEP prior to intubation (6).
CPAP delivers air through the typical method of respiration; air is inhaled through the nose, travels through the nasopharynx, oropharynx, into the larynx, trachea, bronchi, bronchioles, and alveoli (7). This form of ventilation support can be used in inpatient and outpatient settings, long-term care facilities, and at home.
Common indications for CPAP include the following:
- Hypoxia: (7)
- Decrease the work of breathing
- Bronchiolitis or pneumonia
- Respiratory failure associated with congestive heart failure.
- Obstructive sleep apnea (OSA). Predisposition: Obesity, hypotonia, adenotonsillar hypertrophy, family history, use of alcohol or sedatives, etc. (8)
- Preterm infants
- Their lungs have not yet fully developed and respiratory distress syndrome can occur (2)
- Within NICU setting
- CPAP can be administered in several ways based on the type of mask used: (7)
- Nasal CPAP: Nasal prongs inserted directly into the nostrils or a small mask that fits over the nose.
- Nasopharyngeal (NP) CPAP: An airway tube placed through the nose that the tip travels to the nasopharynx.
- Face Mask CPAP: A full face mask is placed over the nose and mouth. The seal is critical.
High Frequency Ventilation (HFV)
High-frequency ventilation (HFV) delivers breaths at a rapid rate because conventional ventilation modes have failed (7). The respiratory rate set on the ventilator significantly exceeds the normal breathing rate and the tidal volume delivered is significantly less. An advantage is the reduced risk of barotrauma, thus reduced risk of lung tissue damage. However, the mode has many contraindications and HFV is not frequently used in adults, more commonly in neonates (7).

Self Quiz
Ask yourself...
- Do you have experience with patients who wear a CPAP for sleep apnea?
- Can you name other indications for CPAP?
- Do you think high-frequency ventilation would be a first or last choice for early choice of ventilator types?
Ventilator Alarms
Ventilator alarms can be a nurse’s best friend when coupled with in-depth understanding of types of alarms and troubleshooting techniques. These alarms are essential during mechanical ventilation because they notify the healthcare team of changes in a patient’s condition that may require intervention. Each alarm represents a different potential problem.
What is a Ventilator Alarm?
A ventilator alarm is a safety feature on the mechanical ventilator that applies a set of parameters to provide alerts whenever there is a problem related to the patient-ventilator interaction. The alarms can be visual, audible, or both, depending on the type of ventilator and settings. Ventilator manufacturers have taken various approaches to alarms. The majority of ventilators allow the user to program default alarm thresholds based on various patient populations (6). Many apply predefined settings, such as +/- 30% of the current minute ventilation. Typical ventilators provide the ability to set alarm thresholds for peak inspiratory pressure, tidal volume, frequency, and minute ventilation, while others do not provide limits (6).
There are many types of ventilator alarms, including:
- High Pressure
- Low Pressure
- Low Volume
- Apnea
- High or Low PEEP
High Pressure Alarm
A high-pressure alarm is triggered whenever the circuit pressure exceeds a preset pressure limit during the inspiratory phase of breathing. The preset limit for the high-pressure alarm is typically set around 10 cmH2O above the peak inspiratory pressure (PIP).
This alarm would be beneficial for patients with respiratory conditions that cause decreased lung compliance or increased airway resistance (2). Other causes of the alarm sounding include coughing, kinking of the airway, or thick and copious secretions. Correctly setting tidal volume alarms is imperative. In VCV, the action of the ventilator is directly controlling tidal volumes, so alarms can alert if this process has abnormalities.
Troubleshooting tips include: (8)
- Check for patient-ventilator asynchrony.
- Perform respiratory assessment.
- Provide endotracheal suctioning if needed.
- Check for a kink in tubing of the artificial airway.
- Relocate the endotracheal tube if it’s not in the correct position.
- Check for a malfunction of the inspiratory or expiratory valves.

Self Quiz
Ask yourself...
- Have you ever been able to recognize various alarms on medical equipment?
- Do you have experience with troubleshooting alarm notifications once you determine the alarm sounded due to an error?
Low Pressure Alarm
A low-pressure alarm is triggered when the peak inspiratory pressure (PIP) pressure in mechanical ventilation is below a preset level. This most commonly occurs whenever there is a leak or disconnection in the system (8). If the cause of the alarm is unknown, the patient should be manually ventilated until the source of the leak is identified.
Troubleshooting tips include:
- Check for a leak or disconnection in the circuit and exhalation valve.
- Check for a leak in the pilot balloon.
- Ensure that the endotracheal tube is properly located.
- Ensure that the endotracheal tube cuff is adequately inflated.
- Ask respiratory therapist or physician if the ventilator settings should be adjusted.
Low Volume Alarm
A low volume alarm is triggered whenever the expiratory volume decreases below a preset low volume threshold (6). This alarm is helpful because it assesses if the patient is receiving and exhaling a minimum tidal volume. If this alarm sounds, the respiratory therapist should be consulted.
Apnea Alarm
An apnea alarm is triggered whenever the total frequency decreases below a preset frequency limit. The alarm is critical to determine if the patient is receiving an adequate number of breaths. The apnea alarm most commonly sounds when there is a disconnection of the circuit from the endotracheal tube (6). If this occurs, the respiratory therapist must ensure that the patient is being ventilated by delivering manual breaths until the disconnection source is identified.
High or Low PEEP Alarm
A high or low PEEP alarm is triggered whenever the level of PEEP exceeds or falls below a preset PEEP limit. The high PEEP alarm most commonly sounds whenever auto-PEEP or air trapping is present (2). A potential cause of the low PEEP alarm is active inspiration by the patient (6). Active inspirator by the patient causes the PEEP level to drop below the preset alarm setting and the settings may be adjusted based on changes in the patient’s condition.
Alarm Fatigue
Although ventilator alarms have invaluable meaning, the alarms can sound frequently without a meaningful reason. Alarm fatigue is frustration felt by healthcare providers with unactionable or insignificant alarms (6). A recent study found that alarms can sound as many as 942 alarms per day (6). Nurses must become familiar with the sounds so they can prioritize their responsiveness. Research suggests that 80–99% of ventilator alarms in general are false or nonactionable (6). There have been policy changes and interventions regarding alarm fatigue and overwhelming alarms with no true significance.
The Joint Commission introduced “Use alarms safely” as a National Patient Safety Goal in 2014 (6). Phase 1 required hospitals to identify the most important alarm signals to manage and inquired, “what mechanical ventilation alarms are important?” and “who determines if an alarm is unnecessary?” (6). Policy changes like this are impactful to the individual nurse and patient, as it made practical changes that impact practice. Although nurses and clinicians appreciate meaningful alarms, it can take them away from issues with higher priority if it constantly alarms for unnecessary reasons.

Self Quiz
Ask yourself...
- Can you name the most common alarms on a mechanical ventilator?
- What do you think contributes to alarm fatigue (ex: high workload, patient frustration)?
- Can you name members of the healthcare team that can help with setting alarm parameters?
- Can you imagine how alarms can impact patient anxiety and sleep habits?
Nursing Care
Nursing care should prioritize maintenance of a patent airway, gas exchange, prevention of trauma, therapeutic communication, and assessment of cardiac and pulmonary complications.
Nursing Priorities
- Ensuring a patent airway and assessing for proper placement of the endotracheal tube
- Monitoring the patient’s respiratory status
- Assessing lung sounds
- Oxygen saturation levels, and
- End-tidal carbon dioxide (EtCO2) monitoring.
- Monitoring patient comfort and pain levels.
- Preventing complications associated with mechanical ventilation.
- Ventilator-associated pneumonia
- Ventilator-induced lung injury
- Collaborating with the healthcare team
- Optimize ventilator settings
- Weaning protocols
- Providing ongoing education for patient and family
Nursing Assessment
- Adventitious breath sounds
- Diminished lung sounds
- Increased or decreased respiratory rate.
- Dyspnea
- Decreased oxygen saturation (Sao2 <90%)
- Arterial pH less than 7.35
- Decreased tidal volume.
- Decreased Pao2 level (>50 to 60 mm Hg)
- Increased Paco2 level (50 to 60 mm Hg or higher)
- Restlessness
- Excessive secretions
- Ineffective cough
Nursing Interventions and Actions
- Assess the client’s respiratory rate, depth, and pattern, including the use of accessory muscles.
- Count the client’s respirations for one full minute and compare with ventilator set rate and desired respiratory rate.
- Observe changes in the level of consciousness.
- Early signs of hypoxia include disorientation, irritability, and restlessness; late signs include lethargy, stupor (8).
- Assess the client’s heart rate and blood pressure.
- Tachycardia may be a result of hypoxia (8).
- Auscultate the lung for normal or adventitious breath sounds.
- Bilateral basilar crackles may indicate pulmonary edema or volume overload, other signs of that includes jugular vein distention and lower limb edema (8). Wheezing and rhonchi are present in obstructive lung disease (8). Absent lung sounds may indicate massive pleural effusion or pneumothorax (8).
- Assess the skin color and examine the lips and nailbeds for cyanosis.
- Monitor oxygen saturation using pulse oximetry.
- Maintain the client’s airway.
- Use suctioning as needed.
- Monitor arterial blood gases (ABGs) as indicated.
- ABGs during respiratory failure may reveal increasing PaCo2 and decreasing PaO2 (8).
- Assess for correct endotracheal (ET) tube placement through observation for symmetrical chest rise, auscultation of bilateral breath sounds, and X-ray confirmation.
- Upon auscultation, if frequent crackles or rhonchi are heard and do not clear with coughing or suctioning, it may indicate developing atelectasis, acute bronchospasm, pneumonia, or pulmonary edema (6).
- Assess for the client’s comfort and pain level.
- Assess the ventilator settings and alarm system every hour.
- Patient positioning.
- Maintain the client in a High-Fowler’s position as tolerated and frequently check the position. This position encourages chest expansion and increases oxygenation.
- Promote optimal nutritional balance.
- Weigh the client regularly.
- Assess if patient can safely eat.
- Auscultate for bowel sounds. Document and report loose stool or absence of bowel movements. -Document abdominal girth measurements.
- Monitor gastric residual volumes following enteral feedings. Gastric residual volumes should be monitored to avoid gastric distention and avoid risk of regurgitation and aspiration.
- Offer food that the client desires and document when oral intake resumes.
- Consult nutritionist and be knowledgeable on nutrients that are vital. For example, protein is a vital nutrient to support wound healing and immune function and to maintain lean body mass (8)
- Assess the client’s and caregiver’s perception and understanding of mechanical ventilation.
- Assess the client’s readiness and ability to learn.
- Encourage the client or significant others to express feelings and ask questions about care.
- Provide ongoing education to patient and caregivers. Use material in multiple formats; for example, books, printed pamphlets, audiovisuals, demonstrations, and instruction sheets. Examples include, but not limited to:
- Explain the need for suctioning as needed.
- Explain that alarms, what they indicate, and that they may periodically sound off, which may be normal.
- Explain the weaning process.
- If long-term ventilation is anticipated, discuss, or plan for long-term ventilator care management and use appropriate referrals: long-term ventilator facilitates versus home care management.
- Community resources may include food and meal services, physical and occupational therapy transportation, and access to client support groups. Social workers should become involved if patient is going home with an invasive mechanical ventilator.

Self Quiz
Ask yourself...
- Do you feel comfortable with airway suctioning?
- What do you think the most optimal patient position is for mechanical ventilation?
- Why would supine position not be appropriate for proper ventilation?
- Can you explain the interventions for maintaining nutrition in the mechanically ventilated patient?

Self Quiz
Ask yourself...
- What are some problems that may occur in the mechanically ventilated patient?
- What do you think the nurse should prioritize in the ventilated patient?
- Can you think of possible questions the patient or family may have regarding ventilator care?
- Can you name interventions to provide holistic care for patients on long-term mechanical ventilation?
Conclusion
Hopefully this course has equipped you with a better understanding of basic respiratory function, the types and mechanism of action of ventilators, and the indications for their use. The settings, modes, and alarms are not so intimidating once you become more comfortable with the common parameters and indications. It takes a village to care for a mechanically ventilated patient, so the nurse should collaborate with medical providers, respiratory therapy, speech therapy, nutrition, the ventilator manufacturer representative, and patient family and caregivers to optimize holistic patient care.
References + Disclaimer
- Kumar, A., Sidhu, J., Lui, F., & Tsao, J. W. (2024, February 12). Alzheimer Disease. StatPearls – NCBI Bookshelf. https://www.ncbi.nlm.nih.gov/books/NBK499922/
- DeTure, M. A., & Dickson, D. W. (2019). The neuropathological diagnosis of Alzheimer’s disease. Molecular Neurodegeneration, 14(1). https://doi.org/10.1186/s13024-019-0333-5
- FastStats. (2024). Alzheimers Disease. https://www.cdc.gov/nchs/fastats/alzheimers.htm
- Reitz, C., Rogaeva, E., & Beecham, G. W. (2020). Late-onset vs nonmendelian early-onset Alzheimer disease. Neurology Genetics, 6(5). https://doi.org/10.1212/nxg.0000000000000512
- Sirkis, D. W., Bonham, L. W., Johnson, T. P., La Joie, R., & Yokoyama, J. S. (2022). Dissecting the clinical heterogeneity of early-onset Alzheimer’s disease. Molecular Psychiatry, 27(6), 2674–2688. https://doi.org/10.1038/s41380-022-01531-9
- Gonzalez-Ortiz, F., Kac, P. R., Brum, W. S., Zetterberg, H., Blennow, K., & Karikari, T. K. (2023). Plasma phospho-tau in Alzheimer’s disease: towards diagnostic and therapeutic trial applications. Molecular Neurodegeneration, 18(1). https://doi.org/10.1186/s13024-023-00605-8
- What happens to the brain in Alzheimer’s disease? (2024, January 19). National Institute on Aging. https://www.nia.nih.gov/health/alzheimers-causes-and-risk-factors/what-happens-brain-alzheimers-disease
- Igarashi, K. M. (2023). Entorhinal cortex dysfunction in Alzheimer’s disease. Trends in Neurosciences, 46(2), 124–136. https://doi.org/10.1016/j.tins.2022.11.006
- Lott, I. T., & Head, E. (2019). Dementia in Down syndrome: unique insights for Alzheimer disease research. Nature Reviews Neurology, 15(3), 135–147. https://doi.org/10.1038/s41582-018-0132-6
- Stages of Alzheimer’s disease. (2024, February 29). Johns Hopkins Medicine. https://www.hopkinsmedicine.org/health/conditions-and-diseases/alzheimers-disease/stages-of-alzheimer-disease
- Cascella, M., & Khalili, Y. A. (2024, June 8). Short-Term memory impairment. StatPearls – NCBI Bookshelf. https://www.ncbi.nlm.nih.gov/books/NBK545136/
- Jadhav, D., Saraswat, N., Vyawahare, N., & Shirode, D. (2024). Targeting the molecular web of Alzheimer’s disease: unveiling pathways for effective pharmacotherapy. The Egyptian Journal of Neurology Psychiatry and Neurosurgery, 60(1). https://doi.org/10.1186/s41983-023-00775-83.
- About Alzheimer’s Disease | aging. (2024). https://www.cdc.gov/aging/alzheimers-disease-dementia/about-alzheimers.html
- Saeed, A., Lopez, O., Cohen, A., & Reis, S. E. (2023). Cardiovascular Disease and Alzheimer’s Disease: the Heart–Brain axis. Journal of the American Heart Association. Cardiovascular and Cerebrovascular Disease, 12(21). https://doi.org/10.1161/jaha.123.030780
- Dementia Risk Reduction | CDC. (2024). https://www.cdc.gov/aging/publications/features/dementia-risk-reduction-june-2022/index.html
- Rom, S., Zuluaga-Ramirez, V., Gajghate, S., Seliga, A., Winfield, M., Heldt, N. A., Kolpakov, M. A., Bashkirova, Y. V., Sabri, A. K., & Persidsky, Y. (2018). Hyperglycemia-Driven neuroinflammation compromises BBB leading to memory loss in both diabetes mellitus (DM) type 1 and Type 2 mouse models. Molecular Neurobiology, 56(3), 1883–1896. https://doi.org/10.1007/s12035-018-1195-5
- Ravindranath, V., & Sundarakumar, J. S. (2021). Changing demography and the challenge of dementia in India. Nature Reviews Neurology, 17(12), 747–758. https://doi.org/10.1038/s41582-021-00565-x
- About Dementia | Aging. (2024). https://www.cdc.gov/aging/alzheimers-disease-dementia/about-dementia.html
- What is Alzheimer’s Disease? | CDC. (2024). https://www.cdc.gov/aging/aginginfo/alzheimers.htm
- Early detection and diagnosis. (2024). Alzheimer’s Disease and Dementia. https://www.alz.org/professionals/public-health/public-health-topics/early-detection-diagnosis
- Sheng, M., Fang, T., Chen, Y., Chang, M., Yang, C., & Lin, C. (2021). Is either anosmia or constipation associated with cognitive dysfunction in Parkinson’s disease? PLoS ONE, 16(6), e0252451. https://doi.org/10.1371/journal.pone.0252451
- Kelso, I. G., & Tadi, P. (2022, November 7). Cognitive assessment. StatPearls – NCBI Bookshelf. https://www.ncbi.nlm.nih.gov/books/NBK556049/
- Wei, Y., Chen, C., Lin, C., Chen, P., Hsu, P., Lin, C., Shyu, Y., & Huang, W. (2022). Normative data of Mini-Mental State Examination, Montreal Cognitive Assessment, and Alzheimer’s Disease Assessment Scale-Cognitive Subscale of Community-Dwelling Older Adults in Taiwan. Dementia and Geriatric Cognitive Disorders, 51(4), 365–376. https://doi.org/10.1159/000525615
- Korsnes, M. S. (2020). Performance on the mini-mental state exam and the Montreal cognitive assessment in a sample of old age psychiatric patients. SAGE Open Medicine, 8, 205031212095789. https://doi.org/10.1177/2050312120957895
- Pirau, L., & Lui, F. (2023, July 17). Frontal Lobe Syndrome. StatPearls – NCBI Bookshelf. https://www.ncbi.nlm.nih.gov/books/NBK532981/
- Maldonado, J., & Sher, Y. (2023). Neurocognitive disorders. In Springer eBooks (pp. 1–60). https://doi.org/10.1007/978-3-030-42825-9_81-1
- Article – Billing and coding: Cognitive Assessment and Care Plan Service (A59036). (2024). https://www.cms.gov/medicare-coverage-database/view/article.aspx?articleid=59036&ver=10
- Billing codes for Alzheimer’s and related dementia. (2024). Alzheimer’s Disease and Dementia. https://www.alz.org/professionals/health-systems-medical-professionals/billing-codes
- Centers for Medicare & Medicaid Services (CMS) Medicare Learning Network (MLN). (n.d.). MLN6775421 – Medicare Wellness Visits. https://www.cms.gov/Outreach-and-Education/Medicare-Learning-Network-MLN/MLNProducts/preventive-services/medicare-wellness-visits.html
- CDR® Dementia Staging Instrument | Knight Alzheimer Disease Research Center | Washington University in St. Louis. (2024). https://knightadrc.wustl.edu/professionals-clinicians/cdr-dementia-staging-instrument/
31, Mini-COG© – Quick Screening for Early Dementia Detection. (2024). https://mini-cog.com/
- Graf, M. S., The Hartford Institute for Geriatric Nursing, & New York University, College of Nursing. (2007). The Lawton Instrumental Activities of Daily Living (IADL) scale. Best Practices in Nursing Care to Older Adults, 23. https://www.alz.org/careplanning/downloads/lawton-iadl.pdf (Original work published 1969)
- CDR® Dementia Staging Instrument | Knight Alzheimer Disease Research Center | Washington University in St. Louis. (n.d.). https://knightadrc.wustl.edu/professionals-clinicians/cdr-dementia-staging-instrument/
- Cummings, J. L. & Daniel Kaufer, MD. (1994). The Neuropsychiatric Inventory Questionnaire: Background and Administration [Report]. https://www.alz.org/media/documents/npiq-questionnaire.pdf
- Alzheimer’s Association, Attea, J., Anonymous, Alzheimer’s Association Task Force, & American Medical Association. (2018). Cognitive Impairment Care Planning Toolkit. In Alzheimer’s Association Expert Task Force Recommendations and Tools for Implementation (No. 99483). https://www.alz.org/careplanning/downloads/care-planning-toolkit.pdf
- Alzheimer’s Association. (2023). CPT® Code 99483 Explanatory Guide for Clinicians. In alzimpact.org. https://portal.alzimpact.org/media/serve/id/5ab10bc1a3f3c
- Singh, R., & Sadiq, N. M. (2023, July 17). Cholinesterase inhibitors. StatPearls – NCBI Bookshelf. https://www.ncbi.nlm.nih.gov/books/NBK544336/
- Kaushik, V., Smith, S. T., Mikobi, E., & Raji, M. A. (2017). Acetylcholinesterase inhibitors: Beneficial effects on comorbidities in patients with Alzheimer’s Disease. American Journal of Alzheimer S Disease & Other Dementias®, 33(2), 73–85. https://doi.org/10.1177/1533317517734352
- Kuns, B., Rosani, A., Patel, P., & Varghese, D. (2024, January 31). Memantine. StatPearls – NCBI Bookshelf. https://www.ncbi.nlm.nih.gov/books/NBK500025/
- Research, C. F. D. E. A. (2021, June 7). FDA’s Decision to Approve New Treatment for Alzheimer’s Disease. U.S. Food And Drug Administration. https://www.fda.gov/drugs/our-perspective/fdas-decision-approve-new-treatment-alzheimers-disease
- Office of the Commissioner. (2023,5 July 6). FDA converts novel Alzheimer’s Disease treatment to traditional approval. U.S. Food And Drug Administration. https://www.fda.gov/news-events/press-announcements/fda-converts-novel-alzheimers-disease-treatment-traditional-approval
- Lilly’s Donanemab significantly slowed cognitive and functional decline in Phase 3 study of early Alzheimer’s disease | Eli Lilly and Company. (2023). Eli Lilly and Company. https://investor.lilly.com/news-releases/news-release-details/lillys-donanemab-significantly-slowed-cognitive-and-functional
- Hampel, H., Elhage, A., Cho, M., Apostolova, L. G., Nicoll, J. a. R., & Atri, A. (2023). Amyloid-related imaging abnormalities (ARIA): radiological, biological, and clinical characteristics. Brain, 146(11), 4414–4424. https://doi.org/10.1093/brain/awad188
- Moraczewski, J., Awosika, A. O., & Aedma, K. K. (2023, August 17). Tricyclic antidepressants. StatPearls – NCBI Bookshelf. https://www.ncbi.nlm.nih.gov/books/NBK557791/
- Chokhawala, K., & Stevens, L. (2023, February 26). Antipsychotic medications. StatPearls – NCBI Bookshelf. https://www.ncbi.nlm.nih.gov/books/NBK519503/
- Lee, D., Slomkowski, M., Hefting, N., Chen, D., Larsen, K. G., Kohegyi, E., Hobart, M., Cummings, J. L., & Grossberg, G. T. (2023). Brexpiprazole for the treatment of agitation in Alzheimer dementia. JAMA Neurology, 80(12), 1307. https://doi.org/10.1001/jamaneurol.2023.3810
- Hui, D. (2018). Benzodiazepines for agitation in patients with delirium: selecting the right patient, right time, and right indication. Current Opinion in Supportive and Palliative Care, 12(4), 489–494. https://doi.org/10.1097/spc.0000000000000395
- Jerjes, W. (2024). The importance of attentive primary care in the early identification of mild cognitive impairment: case series. AME Case Reports, 8, 56. https://doi.org/10.21037/acr-23-162
- Solan, M. (2024, May 1). Drugs for Alzheimer’s disease. Harvard Health. https://www.health.harvard.edu/mind-and-mood/drugs-for-alzheimers-disease
- Cabinet for Health and Family Services. (2019). Child abuse and neglect annual report of child fatalities and near fatalities. Retrieved from: https://chfs.ky.gov/agencies/dcbs/dpp/cpb/Documents/reportofchildfatalitiesandnearfatalities.pdf
- Centers for Disease Control. (2020). Child abuse and neglect prevention strategies. Retrieved from: https://www.cdc.gov/violenceprevention/childabuseandneglect/prevention.html
- Healthy Children. (2020). Abusive head trauma: how to protect your baby. Retrieved from: https://www.healthychildren.org/English/safety-prevention/at-home/Pages/Abusive-Head-Trauma-Shaken-Baby-Syndrome.aspx
- Joyce, T. and Huecker, M. R. (2020). Pediatric abusive head trauma. Stat Pearls. Retrieved from: https://www.ncbi.nlm.nih.gov/books/NBK499836/
- Kentucky Cabinet for Health and Family Services. (2017) Child protection branch. Retrieved from: https://chfs.ky.gov/agencies/dcbs/dpp/cpb/Pages/default.aspx
- Kids Health. (2019). Abusive head trauma (shaken baby syndrome). Retrieved from: https://kidshealth.org/en/parents/shaken.html
- National Center on Shaken Baby Syndrome. (n. d.). Facts and info. Retrieved from: https://www.dontshake.org/learn-more
- National Center on Shaken Baby Syndrome. (n. d.). The period of PURPLE crying. Retrieved from: https://www.dontshake.org/purple-crying
- Rape Abuse and Incest National Network. (2020). Mandatory reporting requirements: children Kentucky. Retrieved from: https://apps.rainn.org/policy/policy-state-laws-export.cfm?state=Kentucky&group=4
- Adams, C, Thomas, SP (2018). Alternative prenatal care interventions to alleviate Black–White maternal/infant health disparities. Sociology Compass, 12:e12549. https://doi.org/10.1111/soc4.12549
- Association of American Medical Colleges. (2019). Diversity in medicine: facts and figures 2019. AAMC. https://www.aamc.org/data-reports/workforce/interactive-data/figure-18-percentage-all-active-physicians-race/ethnicity-2018
- Buchmueller, T. C. and Levy, H. G. (2020). The ACA’s Impact on racial and ethnic disparities in health insurance coverage and access to care. Health Affairs, 39(3). https://doi.org/10.1377/hlthaff.2019.01394
- Cameron, K. A., Song, J., Manheim, L. M., & Dunlop, D. D. (2010). Gender disparities in health and healthcare use among older adults. Journal of women’s health, 19(9), 1643–1650. https://doi.org/10.1089/jwh.2009.1701
- Centers for Disease Control and Prevention. (September 23, 2021). Data and statistics about ADHD. CDC.https://www.cdc.gov/ncbddd/adhd/data.html#:~:text=Boys%20are%20more%20likely%20to,12.9%25%20compared%20to%205.6%25).
- Centers for Disease Control and Prevention. (April 22, 2021). The tuskegee timeline. Retrieved from: https://www.cdc.gov/tuskegee/timeline.htm
- FitzGerald, C., and Hurst, S. (2017). Implicit bias in healthcare professionals: a systematic review. BMC Med Ethics, 18, 19. https://doi.org/10.1186/s12910-017-0179-8
- Gothreau, C. and Acreneaux, J. (2019). The effect of implicit and explicit sexism on reproductive rights attitudes. Temple University. https://sites.temple.edu/cgothreau/files/2019/09/Sexism-Paper.pdf
- Guevara, J. P., Wade, R., and Aysola, J. (2021). Racial and ethnic diversity in medical schools- why aren’t we there yet? The New England Journal of Medicine, 385(1732-1734) DOI: 10.1056/NEJMp2105578
- Hamel, L., Firth, J., Hoff, T., Kates, J., Levine, S., and Dawson, L. (September 25, 2014). HIV/AIDS in the lives of gay and bisexual men in the united states. Kaiser Family Foundation.
- Healthy People 2020. (2020). Data 2020. HealthyPeople.gov https://www.healthypeople.gov/2020/data-search/
- Institute for Policy Research. (May 18, 2018). Communication between healthcare providers and LGBTQ youth. Northwestern. https://www.ipr.northwestern.edu/news/2018/infographic-mustanski-lgbtq-patient-communication.html
- Johns Hopkins Medicine. (n.d.). The legacy of Henrietta Lacks. Retrieved from: https://www.hopkinsmedicine.org/henriettalacks/
- Kathawa, C. A., & Arora, K. S. (2020). Implicit Bias in Counseling for Permanent Contraception: Historical Context and Recommendations for Counseling. Health equity, 4(1), 326–329. https://doi.org/10.1089/heq.2020.0025
- Krahn, G. L., Walker, D. K., & Correa-De-Araujo, R. (2015). Persons with disabilities as an unrecognized health disparity population. American journal of public health, 105 Suppl 2(Suppl 2), S198–S206. https://doi.org/10.2105/AJPH.2014.302182
- Levine DA, Gross AL, Briceño EM, et al. Association between blood pressure and later-life cognition among black and white individuals. JAMA Neurology, 7(7):810–819. doi:10.1001/jamaneurol.2020.0568
- Mude, W., Oguoma, V. M., Nyanhanda, T., Mwanri, L., & Njue, C. (2021). Racial disparities in COVID-19 pandemic cases, hospitalisations, and deaths: A systematic review and meta-analysis. Journal of global health, 11, 05015. https://doi.org/10.7189/jogh.11.05015
- Regis College. (n.d.). Why ageism in healthcare is a growing concern. Regis College. https://online.regiscollege.edu/blog/why-ageism-in-health-care-is-a-growing-concern/
- Saluja, B. and Bryant, Z. (2021). How implicit bias contributes to racial disparities in maternal morbidity and mortality in the united states. Journal of Women’s Health, 30(2). https://doi.org/10.1089/jwh.2020.8874
- Tasca, C., Rapetti, M., Carta, M. G., & Fadda, B. (2012). Women and hysteria in the history of mental health. Clinical practice and epidemiology in mental health : CP & EMH, 8, 110–119. https://doi.org/10.2174/1745017901208010110
- Wall L. L. (2006). The medical ethics of Dr J Marion Sims: a fresh look at the historical record. Journal of medical ethics, 32(6), 346–350. https://doi.org/10.1136/jme.2005.012559
- Accardi, R., Sanchez, C., Zisook, S., Hoffman, L., Davidson, J.E. (2020). Sustainability and Outcomes of a Suicide Prevention Program for Nurses. Worldviews on Evidence-Based Nursing, 2020, 17(1), 24-31. Retrieved on July 5, 2022 from https://library.smh.com/sites/default/files/Sustainability%20and%20Outcomes%20of%20a%20Suicide%20prevention%20program%20for%20nurses.pdf.
- American Nurses Association (n.d.). Nurse Suicide Prevention/Resilience. Retrieved on June 21, 2022 from https://www.nursingworld.org/practice-policy/nurse-suicide-prevention/.
- American Foundation for Suicide Prevention (n.d.). Suicide prevention resources. Retrieved on July 6, 2022 from https://afsp.org/suicide-prevention-resources.
- Association of Clinicians for the Underserved (n.d.). Preventing Suicide in Providers and Staff: Organizational Approaches. Retrieved on July 5, 2022 from https://clinicians.org/programs/suicide-safer-care/preventing-suicide-in-providers-and-staff/.
- Bennington-Castro, J. (2021). How to Help Combat Rising Suicide Rates Among Care Providers. Retrieved on July 6, 2022 from https://huddle.florence-health.com/discover/content/article/how-to-help-combat-rising-suicide-rates-among-care-providers.
- Centers for Disease Control and Prevention (2022). Suicide Prevention: Fact About Suicide. Retrieved on June 21, 2022 from https://www.cdc.gov/suicide/facts/index.html.
- Davidson, J.E. et al. (2021). Nurse suicide prevention starts with crisis intervention: Make a plan to protect yourself and your colleagues. Retrieved on July 5, 2022 from https://www.myamericannurse.com/nurse-suicide-prevention-starts-with-crisis-intervention/.
- Davidson, J. E., Proudfoot, J., Lee, K., Terterian, G., Zisook, S. (2020). A Longitudinal Analysis of Nurse Suicide in the United States (2055-2016) With Recommendations for Action. Worldviews On Evidence-Based Nursing, 17(1), 6-15. Retrieved on June 21, 2022 from https://doi.org/10.1111/wvn.12419.
- Dowd, M. (2021). Ethical Responsibilities of Nurses. Retrieved on July 6, 2022 from https://work.chron.com/ethical-responsibilities-nurses-10778.html.
- Fischer, D. (2018). Preventing Nurse Suicides. Oncology Nursing News. Retrieved on July 6, 2022 from https://www.oncnursingnews.com/view/preventing-nurse-suicides.
- Fischer, L. (2022). Nurses Consider Suicide More Than Other US Workers. Oncology Nursing News. Retrieved on June 30, 2022 from https://www.oncnursingnews.com/view/nurses-consider-suicide-more-than-other-us-workers.
- Folmer, K., Howard, M.C. (2022). What Employers Need to Know About Suicide Prevention. Harvard Business Review. Retrieved on July 6, 2022 from https://hbr.org/2022/01/what-employers-need-to-know-about-suicide-prevention.
- Haskell, B. (2022). Suicide assessment and follow-up care: Nursing skills and implications. Retrieved on July 5, 2022 from https://www.myamericannurse.com/suicide-assessment-and-follow-up-care/.
- Hutton, A. (2015). Saving lives by preventing suicide. Retrieved on July 5, 2022 from https://www.myamericannurse.com/saving-lives-preventing-suicide/.
- Marfell, J., Norrod, P., Walmsley, L. (2022). Oped: Nurse Suicide Awareness. University of Kentucky College of Nursing. Retrieved on July 5, 2022 from https://www.uky.edu/nursing/about-us/news/oped-nurse-suicide-awareness#:~:text=In%20Kentucky%2C%20approximately%2058%20nurses,continuing%20education%20in%20suicide%20prevention.
- Merenda, L. (2019). How one program may help prevent suicide in nurses. Retrieved on July 6, 2022 from https://www.wolterskluwer.com/en/expert-insights/how-one-program-may-help-prevent-suicide-in-nurses.
- National Institute of Mental Health (n.d.). Ask Suicide-Screening Questions (ASQ) Toolkit. Retrieved on July 6, 2022 from https://www.nimh.nih.gov/research/research-conducted-at-nimh/asq-toolkit-materials/index.shtml.
- Rizzo, L.H. (2018). Suicide among nurses: What we don’t know might hurt us: Research, prevention programs, and open discussion are required to reduce nurse suicide. Retrieved on July 6, 2022 from https://www.myamericannurse.com/suicide-among-nurses-might-hurt-us/.
- America Civil Liberties Union. (2006). Domestic violence and homelessness. https://www.aclu.org/sites/default/files/pdfs/dvhomelessness032106.pdf
- American Academy of Child & Adolescent Psychiatry. (2014). Sexual abuse. Aacap.org. https://www.aacap.org/AACAP/Families_and_Youth/Facts_for_Families/FFF-Guide/Child-Sexual-Abuse-009.aspx
- Australian Government Department of Social Services. (2023). Psychological abuse. 1800RESPECT. https://www.1800respect.org.au/violence-and-abuse/psychological-abuse
- Boserup, B., McKenney, M., & Elkbuli, A. (2020). Alarming trends in US domestic violence during the COVID-19 pandemic. The American Journal of Emergency Medicine, 38(12). https://doi.org/10.1016/j.ajem.2020.04.077
- Centers for Disease Control and Prevention. (2020). Disability and health overview. Centers for Disease Control and Prevention. https://www.cdc.gov/ncbddd/disabilityandhealth/disability.html
- Centers for Disease Control and Prevention. (2021a, February 22). Intimate partner violence, sexual violence, and stalking among men. Www.cdc.gov. https://www.cdc.gov/violenceprevention/intimatepartnerviolence/men-ipvsvandstalking.html
- Centers for Disease Control and Prevention. (2021b, July 14). Sexual assault and abuse and STIs – STI treatment guidelines. Www.cdc.gov. https://www.cdc.gov/std/treatment-guidelines/sexual-assault-children.htm
- Centers for Disease Control and Prevention. (2021c, November 2). Risk and protective factors for perpetration. Centers for Disease Control and Prevention. https://www.cdc.gov/violenceprevention/intimatepartnerviolence/riskprotectivefactors.html
- Children’s Bureau. (2019). What is child abuse and neglect? Recognizing the signs and symptoms. https://www.childwelfare.gov/pubpdfs/whatiscan.pdf
- Cleveland Clinic. (2023, February 1). What is love bombing? 7 signs to look for. Cleveland Clinic. https://health.clevelandclinic.org/love-bombing/
- Committee on Health Care for Underserved Women. (2012, February). Intimate partner violence. Www.acog.org. https://www.acog.org/clinical/clinical-guidance/committee-opinion/articles/2012/02/intimate-partner-violence
- Congressional Research Service. (2019). Military families and intimate partner violence: Background and issues for congress. https://crsreports.congress.gov/product/pdf/R/R46097
- Connections for Abused Women and Their Children. (2023, March 8). What is the cycle of abuse? Connections for Abused Women and Their Children. https://www.cawc.org/news/what-is-the-cycle-of-abuse/
- Department of Justice Canada. (2002, March 29). A child’s age and stage of development make a difference. Www.justice.gc.ca. https://www.justice.gc.ca/eng/rp-pr/fl-lf/divorce/age/age2c.html
- Domestic Violence Awareness Project. (2019, June). What do we know about domestic violence within immigrant communities? Domestic Violence Awareness Project. https://www.dvawareness.org/sites/default/files/2019-06/Immigration&DV-TalkingPointsForm.pdf
- Domestic Violence Coordinating Council. (2011). Domestic violence dynamics – what domestic abuse what it does to family. Domestic Violence Coordinating Council (DVCC) – State of Delaware. https://dvcc.delaware.gov/background-purpose/dynamics-domestic-abuse/
- Domestic Violence Services, Inc. (n.d.). Teen dating violence statistics. Domestic Violence Services, Inc. https://www.dvs-or.org/teen-dating-violence-statistics/
- DomesticShelters.org. (2019). Domestic violence assessment tools. DomesticShelters.org. https://www.domesticshelters.org/resources/risk-assessment-tools
- DomesticShelters.org. (2022, September 21). What is the cycle of abuse? DomesticShelters.org. https://www.domesticshelters.org/articles/identifying-abuse/what-is-the-cycle-of-abuse
- Florida State University. (2014). National prevention toolkit on domestic violence for medical professionals. https://dvmedtraining.csw.fsu.edu/wp-content/uploads/2014/01/BarriersToScreening2014.pdf
- Huecker, M. R., & Smock, W. (2019, May 5). Kentucky domestic violence. Nih.gov; StatPearls Publishing. https://www.ncbi.nlm.nih.gov/books/NBK499924/
- International Rescue Committee. (2020, October 15). New report finds 73% of refugee and displaced women reported an increase in domestic violence due to COVID-19. International Rescue Committee (IRC). https://www.rescue.org/press-release/new-report-finds-73-refugee-and-displaced-women-reported-increase-domestic-violence
- Joyful Heart Foundation. (2021). Effects of domestic violence. Joyfulheartfoundation.org. https://www.joyfulheartfoundation.org/learn/domestic-violence/effects-domestic-violence
- Kentucky Coalition Against Domestic Violence. (2016, September 14). Mandatory reporting. Kentucky Coalition against Domestic Violence. https://kcadv.org/resources/laws/mandatory-reporting
- Khalifeh, H., Moran, P., Borschmann, R., Dean, K., Hart, C., Hogg, J., Osborn, D., Johnson, S., & Howard, L. M. (2014). Domestic and sexual violence against patients with severe mental illness. Psychological Medicine, 45(4), 875–886. https://doi.org/10.1017/s0033291714001962
- Libertin, A. (2018, June 12). Erasing the stigma: Communities of color. Hawcdv.org. https://hawcdv.org/erasing-the-stigma-communities-of-color/
- Lowdermilk, D. L., Perry, S. E., Cashion, K., & Kathryn Rhodes Alden. (2016). Maternity & women’s health care. Elsevier.
- Maurer, K. (2023). Income support may reduce violence for poor families. https://poverty.ucdavis.edu/sites/main/files/file-attachments/maurer_family_violence_brieft.pdf
- National Coalition Against Domestic Violence. (2018a, March 13). Domestic violence and people with disabilities: What to know, why it matters, and how to help . Ncadv.org. https://ncadv.org/blog/posts/domestic-violence-and-people-with-disabilities
- National Coalition Against Domestic Violence. (2018b, June 12). Quick guide: Domestic abuse in later life. Ncadv.org. https://ncadv.org/blog/posts/quick-guide-domestic-abuse-in-later-life
- National Coalition Against Domestic Violence. (2020a). Domestic violence and disabilities. https://www.niwrc.org/sites/default/files/images/resource/fact_sheet_pdfs.pdf#:~:text=Women%20with%20developmental%20disabilities%20have%20among%20the%20highest
- National Coalition Against Domestic Violence. (2020b). Domestic violence in Kentucky. https://assets.speakcdn.com/assets/2497/ncadv_kentucky_fact_sheet_2020.pdf
- National Coalition Against Domestic Violence. (2021). National statistics. NCADV. https://ncadv.org/statistics
- National Coalition Against Domestic Violence. (2022). Domestic violence & firearms. https://assets.speakcdn.com/assets/2497/guns_and_dv_2022.pdf
- National Coalition against Domestic Violence. (2018, June 6). Domestic violence and the LGBTQ community . Ncadv.org. https://ncadv.org/blog/posts/domestic-violence-and-the-lgbtq-community
- National Domestic Violence Hotline. (2023). Domestic violence statistics. The Hotline. https://www.thehotline.org/stakeholders/domestic-violence-statistics/
- National Network to End Domestic Violence. (n.d.). Statistics contributing and exacerbating factors needs and policy recommendations domestic violence, housing, and homelessness. https://staging.nnedv.org/wp-content/uploads/mdocs/THousing_Handout_Domestic-violence-housing-and-homelessness.pdf
- National Network to End Domestic Violence. (2022, October 12). 403.720 definitions for KRS 403.715 to 403.785. Statutes: Kentucky. https://www.womenslaw.org/laws/ky/statutes/403720-definitions-krs-403715-403785
- National Partnership for Women & Families. (2021, May). Intimate partner violence endangers pregnant people and their infants. National Partnership for Women & Families. https://nationalpartnership.org/report/intimate-partner-violence/
- Newport Institute. (2021, November 4). How to tell if someone is gaslighting you. Newport Institute. https://www.newportinstitute.com/resources/mental-health/what_is_gaslighting_abuse/
- Nichol, J. R., Nelson, G., & Sundjaja, J. H. (2022, September 5). Medical history. PubMed; StatPearls Publishing. https://www.ncbi.nlm.nih.gov/books/NBK534249/
- Office for Victims of Crime. (2021, November). Crime against persons with disabilities, 2009–2019 – statistical tables | OVC. Office for Victims of Crime. https://ovc.ojp.gov/library/publications/crime-against-persons-disabilities-2009-2019-statistical-tables
- Office on Women’s Health. (2019, January 30). Health effects of violence. Women’s Health. https://www.womenshealth.gov/relationships-and-safety/effects-violence-against-women
- Peek-Asa, C., Wallis, A., Harland, K., Beyer, K., Dickey, P., & Saftlas, A. (2011). Rural disparity in domestic violence prevalence and access to resources. Journal of Women’s Health, 20(11), 1743–1749. https://doi.org/10.1089/jwh.2011.2891
- Raising Children Network. (2023, January 23). Signs of sexual abuse in children and teenagers. Raising Children Network. https://raisingchildren.net.au/school-age/safety/child-sexual-abuse/signs-of-sexual-abuse#sexual-abuse-in-children-and-teenagers-recognising-the-signs-nav-title
- Resource Center on Domestic Violence: Child Protection and Custody. (2015). Rates of child abuse and child exposure to domestic violence. Rcdvcpc.org. https://www.rcdvcpc.org/rates-of-child-abuse-and-child-exposure-to-domestic-violence.html
- Safe Voices. (2021). Refugee and immigrant abuse. Safevoices.org. https://safevoices.org/what-domestic-violence/refugee-and-immigrant-abuse
- Safety Net Project. (2022). Teens and tech abuse. Safety Net Project. https://www.techsafety.org/teens-and-tech-abuse
- Satyanathan, D., & Pollack, A. (2007). Michigan family impact seminars domestic violence and poverty. https://www.purdue.edu/hhs/hdfs/fii/wp-content/uploads/2015/07/s_mifis04c05.pdf
- Standford Medicine. (2023). How to ask. Domestic Abuse. https://domesticabuse.stanford.edu/screening/how.html
- Stockman, J. K., Hayashi, H., & Campbell, J. C. (2015). Intimate partner violence and its health impact on ethnic minority women. Journal of Women’s Health, 24(1), 62–79. https://doi.org/10.1089/jwh.2014.4879
- Substance Abuse and Mental Health Services Administration. (2023, February 7). Mental health and substance use co-occurring disorders. Www.samhsa.gov. https://www.samhsa.gov/mental-health/mental-health-substance-use-co-occurring-disorders
- The Oregon Coalition Against Domestic and Sexual Violence. (2023). Child and elder abuse. The Oregon Coalition against Domestic and Sexual Violence. https://www.ocadsv.org/resources/node-292-resource_public/
- U.S. Department of Agriculture. (2019, October 23). What is rural? Www.ers.usda.gov. https://www.ers.usda.gov/topics/rural-economy-population/rural-classifications/what-is-rural/
- UN Women. (2023). Explore the facts: Violence against women. Interactive.unwomen.org. https://interactive.unwomen.org/multimedia/infographic/violenceagainstwomen/en/index.html#mutilation-3
- United States Department of Justice. (2001). Burn injuries in child abuse. https://www.ojp.gov/pdffiles/91190-6.pdf
- University of Michigan. (2023). Intimate partner violence (IPV). Welfare and Safety. https://medicine.umich.edu/dept/psychiatry/michigan-psychiatry-resources-covid-19/healthcare-providers/covid-19-mental-health-toolkit/impact-pandemics/welfare-safety
- Valandra, Higgins, B., Murphy-Erby, Y., & Brown, L. (2019). An exploratory study of african american men’s perspectives of intraracial, heterosexual intimate partner violence using a multisystems life course framework. Journal of the Society for Social Work and Research, 10(1), 69–95. https://doi.org/10.1086/701824
- Vera, M. (2012, February 18). Head-to-Toe assessment: Complete physical assessment guide. Nurseslabs. https://nurseslabs.com/head-to-toe-assessment-complete-physical-assessment-guide/
- Washington State Department of Social and Health Services. (2012). Types and signs of abuse. Washington State Department of Social and Health Services. https://www.dshs.wa.gov/altsa/home-and-community-services/types-and-signs-abuse
- American Association of Clinical Endocrinology (2021). What you need to know about diabetes. About Diabetes. https://www.aace.com/disease-and-conditions/diabetes/what-you-need-know-about-diabetes
- Berget, C., Messer, L. H., & Forlenza, G. P. (2019). A Clinical Overview of Insulin Pump Therapy for the Management of Diabetes: Past, Present, and Future of Intensive Therapy. Diabetes spectrum: a publication of the American Diabetes Association, 32(3), 194–204. https://doi.org/10.2337/ds18-0091
- Blonde, L., Umpierrez, G. E., Reddy, S. S., McGill, J. B., Berga, S. L., Bush, M., … & Weber, S. L. (2022). American Association of Clinical Endocrinology clinical practice guideline: developing a diabetes mellitus comprehensive care plan—2022 update. Endocrine Practice, 28(10), 923-1049.
- Center for Disease Control and Prevention. (2022). Estimates of diabetes and its burden in the United States. National diabetes statistics report. cdc.gov/diabetes/data/statistics-report/index.html
- Center for Disease Control and Prevention. (2022). Prevalence of both diagnosed and undiagnosed diabetes. https://www.cdc.gov/diabetes/data/statistics-report/diagnosed-undiagnosed-diabetes.html
- Center for Disease Control and Prevention. (2023). What is Diabetes? https://www.cdc.gov/diabetes/basics/diabetes.html
- ElSayed, N. A., Aleppo, G., Aroda, V. R., Bannuru, R. R., Brown, F. M., Bruemmer, D., … & Gabbay, R. A. (2023). 7. Diabetes technology: standards of care in diabetes—2023. Diabetes Care, 46(Supplement_1), S111-S127.
- Galicia-Garcia, U., Benito-Vicente, A., Jebari, S., Larrea-Sebal, A., Siddiqi, H., Uribe, K. B., Ostolaza, H., & Martín, C. (2020). Pathophysiology of Type 2 Diabetes Mellitus. International journal of molecular sciences, 21(17), 6275. https://doi.org/10.3390/ijms21176275
- Ganesan, K., Rana, M. B. M., & Sultan, S. (2018). Oral hypoglycemic medications.
- Feingold, K. R., Anawalt, B., Boyce, A., Chrousos, G., Dungan, K., Grossman, A, & Kopp, P. (2020). Oral and injectable (non-insulin) pharmacological agents for type 2 diabetes. South Dartmouth (MA).
- E. (2022). Pancreas hormones. https://www.endocrine.org/patient-engagement/endocrine-library/hormones-and-endocrine-function/pancreas-hormones
- Kreider, K. E. (2021). Patient-centered medication selection for type 2 diabetes: A collaborative, patient-centered approach that considers a variety of factors will be most effective. American Nurse Journal, 16(11), 33-37.
- Banday, M. Z., Sameer, A. S., & Nissar, S. (2020). Pathophysiology of diabetes: An overview. Avicenna journal of medicine, 10(4), 174–188. https://doi.org/10.4103/ajm.ajm_53_20
- Draznin, B., Aroda, V. R., Bakris, G., Benson, G., Brown, F. M., Freeman, R., & American Diabetes Association Professional Practice Committee. (2022). 9. Pharmacologic approaches to glycemic treatment: standards of medical care in diabetes-2022. Diabetes care, 45(Suppl 1), S125-S143.
- World Health Organization. (2023). https://www.who.int/news-room/fact-sheets/detail/diabetes
- Hospice and Palliative Nurse’s Association. (2023, September 14). Hospice and Palliative Credentialing Center. Retrieved from AdvancingExpertCare.org: https://www.advancingexpertcare.
- Connor, S., Fitch, K., Iwaski, K., & Pyenson, B. (2006). Comparing Hospice and Nonhospice Patient Survival Among Patients Who Die Within a Three-Year Window. Journal of Pain and Symptom Management, 238-46.
- Coyle, N., Ferrell, B., & Paice, J. (2023). Oxford Textbooks in Palliative Medicine. In Oxford Textbook of Palliative Nursing. New York: Oxford Academic.
- Encyclopedia Brittanica. (2023, September 14). Retrieved from Merriam-Webster.com: https://www.merriam-webster.com/
- National Hospice and Palliative Care Organization. (2023, September 14). Hospice Care Overview For Professionals. Retrieved from NHPCO.org: https://www.nhpco.org/hospice-care-overview/ References:
- Cho, J., & Trent, A. (2006). Validating a decisional conflict scale. Medical Decision Making, 26(4), 373-380.
- Mullaney, T., et al. (2019). Informed consent: The role of the nurse. Journal of Radiology Nursing, 38(2), 177-183.
- Betancourt, J. R., Green, A. R., & Carillo, J. E. (2002). Cultural competence in health care: Emerging frameworks and practical approaches. The Commonwealth Fund.
- Institute of Medicine. (2000). To err is human: Building a safer health system. National Academies Press.
- American Nurses Association. (2019). Nursing: Scope and standards of practice. American Nurses Association
- National Hospice and Palliative Care Organization. (n.d.). History of Hospice Care. Retrieved from https://www.nhpco.org/about/hospice-care/history-of-hospice-care/
- Hospice UK. (n.d.). The History of Hospice Care. Retrieved from https://www.hospiceuk.org/about-hospice-care/the-history-of-hospice-care
- Philosophy 1. World Health Organization. (202).0 Palliative Care. Retrieved from https://www.who.int/news-room/fact-sheets/detail/palliative-care
- American Academy of Hospice and Palliative Medicine. (n.d.). History of Hospice and Palliative Medicine. Retrieved from https://aahpm.org/about/history-of-hospice-and-palliative-medicine
- Centers for Medicare & Medicaid Services. (n.d.). Medicare Benefit Policy Manual: Chapter 9 – Coverage of Hospice Services Under Hospital Insurance. Retrieved from https://www.cms.gov/Regulations-and-Guidance/Guidance/Manuals/downloads/bp102c09.pdf
- Hospice and Palliative Credentialing Center. (n.d.). CHPN – Certified Hospice and Palliative Nurse. Retrieved from https://www.nhpco.org/certification/chn-certified-hospice-nurse/
- National Hospice and Palliative Care Organization. (nice.d Nurse.). Hosp. Retrieved from https://www.nhpco.org/about/hospice-care/hospice-nurse/
- Patient-centered care(Reference: Institute of Medicine. (2014). Dying in America: Improving quality and honoring individual preferences near the end of life. National Academies Press).
- Shared decision making(Reference: Elwyn, G., et al. (2012). Shared decision making: A model for clinical practice. Journal of General Internal Medicine, 27(10), 1361-1367). 4.
- Psychosoc(Reference: Balboni, T. A., et al. (2010). Provision of spiritual support to patients with advanced cancer by religious communities and associations with medical care at the end of life. JAMA Internal Medicine, 170(15), 1109-1117).
- Pain and symptom management (Reference: Ferrell, B. R., et al. (2017). Integration of palliative care into standard oncology care: American Society of Clinical Oncology Clinical Practice Guideline Update. Journal of Clinical Oncology, 35(1), 96-112).
- Institute of Medicine. (2014). Dying in America: Improving quality and honoring individual preferences near the end of life. National Academies Press.
- Breen, C. M., Abernethy, A. P., & Abbott, K. H. (2011). Conflict associated with decisions to limit life-sustaining treatment in intensive care units. Journal of General Internal Medicine, 26(4), 389-394.
- Elwyn, G., et al. (2012). Shared decision making: A model for clinical practice. Journal of General Internal Medicine, 27(10), 1361-1367.
- Balboni, T. A., et al. (2010). Provision of spiritual support to patients with advanced cancer by religious communities and associations with medical care at the end of life. JAMA Internal Medicine, 170(15), 1109-1117.
- Ferrell, B. R., et al. (2017). Integration of palliative care into standard oncology care: American Society of Clinical Oncology Clinical Practice Guideline Update. Journal of Clinical Oncology, 35(1), 96-112.
- San Filippo, D. (2006). Philosophical, Psychological & Spiritual Perspectives on Death & Dying. Faculty Publications. 31. https://digitalcommons.nl.edu/faculty_publications/31
- Kyota, A. & Knda, K. (2019). How to come to terms with facing death: a qualitive study examining the experiences of patients with terminal cancer. https://doi.org/10.1186/s12904-019-0417-6
- Peters, L. et al. (2013). How death anxiety impacts nurses’ caring for patients at the end of life: a review of literature. The open nursing journal, 7, 14–21. https://doi.org/10.2174/1874434601307010014
- Bergenholtz, H. et al. (2020). Talking about death and dying in a hospital setting- a qualitative study of the wishes for end-of-life conversations from the perspective of patients and spouses. https://doi.org/10.1186/s12904-020-00675-1
- Oates J.R. & Maani-Fogelman P.A. (2022). Nursing Grief and Loss. https://www.ncbi.nlm.nih.gov/books/NBK518989/
- Bodi, S., Matus, C., & Hickey, D. (2022). Right place, right time: Facilitating end-of-life conversations. The Journal of family practice, 71(2), 74–79. https://doi.org/10.12788/jfp.0333
- Pentaris, P., & Tripathi, K. (2022). Palliative pProfessionals’ Views on the Importance of Religion, Belief, and Spiritual Identities Toward the End of Life. International journal of environmental research and public health, 19(10), 6031. https://doi.org/10.3390/ijerph19106031
- Lin, H. Y. et el. (2021). Nurses’ knowledge, attitude, and competence regarding palliative and end-of-life care: a path analysis. PeerJ, 9, e11864. https://doi.org/10.7717/peerj.11864
- Becker, C. et al. (2020). Communication challenges in end-of-life decisions. Swiss medical weekly, 150, w20351. https://doi.org/10.4414/smw.2020.20351
- Oates J.R. & Maani C. V. Death and Dying. [Updated 2022 Nov 29]. In: StatPearls [Internet]. Treasure Island (FL): StatPearls Publishing; 2023 Jan-. https://www.ncbi.nlm.nih.gov/books/NBK536978/
- Ijaopo, E. O. et al. (2023). A Review of Clinical Signs and Symptoms of Imminent End-of-Life in Individuals With Advanced Illness. Gerontology & geriatric medicine, 9, 23337214231183243. https://doi.org/10.1177/23337214231183243
- Lee, E. K. et el. (2021). End-of-Life Assessments and Communication for Dying Patients and Their Families. Journal of hospice and palliative care, 24(3), 194–197. https://doi.org/10.14475/jhpc.2021.24.3.194
- Onishi H. (2021). Communication at the End of Life. Journal of hospice and palliative care, 24(3), 135–143. https://doi.org/10.14475/jhpc.2021.24.3.135
- Brown, J. D., Harnett, J., Chambers, R., & Sato, R. (2018). The relative burden of community-acquired pneumonia hospitalizations in older adults: a retrospective observational study in the United States. BMC geriatrics, 18(1), 92. https://doi.org/10.1186/s12877-018-0787-2
- Centers for Disease Control and Prevention. (2022, May 18). Pneumococcal disease: Symptoms and complications. Retrieved from https://www.cdc.gov/pneumococcal/about/symptoms-complications.html
- Centers for Disease Control and Prevention. (2023, September 19). FastStats: Pneumonia. Retrieved from https://www.cdc.gov/nchs/fastats/pneumonia.htm
- Chen, S., Kent, B., & Cui, Y. (2021). Interventions to prevent aspiration in older adults with dysphagia living in nursing homes: a scoping review. BMC geriatrics, 21(1), 429. https://doi.org/10.1186/s12877-021-02366-9
- Coutts, K., & Pillay, M. (2021). Decision making and the bedside assessment: The Speech Language Therapists’ thinking when making a diagnosis at the bed. The South African Journal of communication disorders 68(1), e1–e8. https://doi.org/10.4102/sajcd.v68i1.790
- Ebihara T. (2022). Comprehensive Approaches to Aspiration Pneumonia and Dysphagia in the Elderly on the Disease Time-Axis. Journal of clinical medicine, 11(18), 5323. https://doi.org/10.3390/jcm11185323
- Gershonovitch, R., Yarom, N., & Findler, M. (2020). Preventing ventilator-associated pneumonia in intensive care unit by improved oral care: A review of randomized control trials. SN comprehensive clinical medicine, 2(6), 727–733. https://doi.org/10.1007/s42399-020-00319-8
- Hayes, B. H., Haberling, D. L., Kennedy, J. L., Varma, J. K., Fry, A. M., & Vora, N. M. (2018). Burden of Pneumonia-Associated Hospitalizations: United States, 2001-2014. Chest, 153(2), 427–437. https://doi.org/10.1016/j.chest.2017.09.041
- Heron M. (2021). Deaths: Leading Causes for 2019. National vital statistics reports: from the Centers for Disease Control and Prevention, National Center for Health Statistics, National Vital Statistics System, 70(9), 1–114.
- Jain, V., Vashisht, R., Yilmaz, G., & Bhardwaj, A. (Updated 2023, July 31). Pneumonia pathology. In StatPearls. StatPearls Publishing. Retrieved from https://www.ncbi.nlm.nih.gov/books/NBK526116/
- Nakamura, T., & Kurosaki, S. (2020). Effects of Early Dysphagia Rehabilitation by Speech-language-hearing Therapists on Patients with Severe Aspiration Pneumonia. Progress in rehabilitation medicine, 5, 20200020. https://doi.org/10.2490/prm.20200020
- National Heart, Lung, and Blood Institute. (Updated 2022, March 24). Pneumonia causes and risk factors. U.S. Department of Health and Human Services, National Institutes of Health. Retrieved from https://www.nhlbi.nih.gov/health/pneumonia/causes
- National Heart, Lung, and Blood Institute. (Updated 2022, March 24). Pneumonia prevention. U.S. Department of Health and Human Services, National Institutes of Health. Retrieved from https://www.nhlbi.nih.gov/health/pneumonia/prevention
- Peters, Z. J., Ashman, J. J., Schwartzman, A., & DeFrances, C. J. (2022). National Hospital Care Survey Demonstration Projects: Examination of Inpatient Hospitalization and Risk of Mortality Among Patients Diagnosed with Pneumonia. National health statistics reports, (167), 1–9.
- Regunath, H., & Oba, Y. (Updated 2022, November 15). Community-acquired pneumonia. In StatPearls. StatPearls Publishing. Retrieved from https://www.ncbi.nlm.nih.gov/books/NBK430749/
- Sanivarapu, R. R., & Gibson, J. (Updated 2023, May 8). Aspiration pneumonia. In StatPearls. StatPearls Publishing. Retrieved from https://www.ncbi.nlm.nih.gov/books/NBK470459/
- Sattar, S.B.A., & Sharma, S. (Updated 2023, August 14). Bacterial pneumonia. In StatPearls. StatPearls Publishing. Retrieved from https://www.ncbi.nlm.nih.gov/books/NBK513321/
- Sattar, S.B.A., Sharma, S., & Headley, A. (Updated 2023, August 14). Bacterial pneumonia (Nursing). In StatPearls. StatPearls Publishing. Retrieved from https://www.ncbi.nlm.nih.gov/books/NBK568697/
- Shoar, S., & Musher, D. M. (2020). Etiology of community-acquired pneumonia in adults: a systematic review. Pneumonia (Nathan Qld.), 12, 11. https://doi.org/10.1186/s41479-020-00074-3
- Torres, A., & Martin-Loeches, I. (2020). Invasive Pulmonary Aspergillosis in Ventilator-associated Pneumonia: The Hidden Enemy? American journal of respiratory and critical care medicine, 202(8), 1071–1073. https://doi.org/10.1164/rccm.202006-2605ED
- Troll, C., Trapl-Grundschober, M., Teuschl, Y., Cerrito, A., Compte, M. G., & Siegemund, M. (2023). A bedside swallowing screen for the identification of post-extubation dysphagia on the intensive care unit – validation of the Gugging Swallowing Screen (GUSS)-ICU. BMC anesthesiology, 23(1), 122. https://doi.org/10.1186/s12871-023-02072-6
- Bellani, G. (2022). Mechanical ventilation from pathophysiology to clinical evidence.
- Springer. https://doi.org/10.1007/978-3-030-93401-9
- Hickey SM, Giwa AO. Mechanical Ventilation. [Updated 2023]. In: StatPearls
- [Internet]. Treasure Island (FL): StatPearls Publishing; 2023 Jan-. Available from: https://www.ncbi.nlm.nih.gov/books/NBK539742/
- Keszler M. (2019). Volume-targeted ventilation: One size does not fit all. Evidence-based
- recommendations for successful use. Arch. Dis. Child. Fetal Neonatal Ed.; 104: F108–12.
- Shelledy, & Peters, J. I. (2020). Mechanical ventilation (Proud, Ed.). Jones & Bartlett
- Learning.
- Spinelli, E., Mauri, T., Beitler, J.R. et al. (2020). Respiratory drive in the acute
- respiratory distress syndrome: pathophysiology, monitoring, and therapeutic interventions. Intensive Care Med 46, 606–618. Available from: https://doi.org/10.1007/s00134-020-05942-6
- Walsh, B. K., & Waugh, J. B. (2020). Alarm Strategies and Surveillance for Mechanical
- Ventilation. Respiratory Care, 65(6), 820–831. https://doi.org/10.4187/respcare.07546
- Wilcox, Aydin, A., & Marcolini, E. G. (2019). Mechanical ventilation in emergency
- medicine. Springer. https://doi.org/10.1007/978-3-319-98410-0
- Williams, L. S., & Hopper, P. D. (2019). Understanding medical-surgical nursing. F.A.
- Davis Company.
Disclaimer:
Use of Course Content. The courses provided by NCC are based on industry knowledge and input from professional nurses, experts, practitioners, and other individuals and institutions. The information presented in this course is intended solely for the use of healthcare professionals taking this course, for credit, from NCC. The information is designed to assist healthcare professionals, including nurses, in addressing issues associated with healthcare. The information provided in this course is general in nature and is not designed to address any specific situation. This publication in no way absolves facilities of their responsibility for the appropriate orientation of healthcare professionals. Hospitals or other organizations using this publication as a part of their own orientation processes should review the contents of this publication to ensure accuracy and compliance before using this publication. Knowledge, procedures or insight gained from the Student in the course of taking classes provided by NCC may be used at the Student’s discretion during their course of work or otherwise in a professional capacity. The Student understands and agrees that NCC shall not be held liable for any acts, errors, advice or omissions provided by the Student based on knowledge or advice acquired by NCC. The Student is solely responsible for his/her own actions, even if information and/or education was acquired from a NCC course pertaining to that action or actions. By clicking “complete” you are agreeing to these terms of use.
➁ Complete Survey
Give us your thoughts and feedback
To receive your certificate
