Course
Obesity Management
Course Highlights
- In this Obesity Management course, we will learn about the underlying pathophysiology of obesity, including genetic, environmental, and physiological factors.
- You’ll also learn significant health risks and comorbidities associated with obesity.
- You’ll leave this course with a broader understanding of the relationship between social determinants of health (SDOH) and obesity.
About
Contact Hours Awarded: 3
Course By:
Abbie Schmitt, MSN-ED, RN
Begin Now
Read Course | Complete Survey | Claim Credit
➀ Read and Learn
The following course content
Introduction
Obesity is becoming a global health crisis, significantly increasing the risk of several serious non-communicable diseases, including cardiovascular disease, diabetes, and cancer. This issue is driven by multiple factors. However, the surge in sedentary lifestyles and unhealthy eating habits are primary culprits.
Effective weight management interventions could not only help control the obesity epidemic but also reduce the associated health risks. This course will explore the various factors contributing to obesity and related health outcomes.
We will highlight the major health risks linked to obesity and delve into management guidelines and treatment.
Definition and Background
Obesity is defined as an abnormal or excessive fat accumulation that presents a risk to health (12).
Obesity is considered a disease based on rigorous criteria. Many organizations have debated for decades about whether or not obesity is a disease; in 2004, the Centers for Medicare and Medicaid Services (CMS) removed their language that obesity is not a disease, and organizations like the Obesity Society, Obesity Medicine Association, American Association of Clinical Endocrinologists, and Endocrine Society strongly argued that it should be classified as a disease. The American Medical Association recognized obesity as a disease in 2013 when the scientific committee approved this label and debated it within their house of delegates (6).
The AMA has criteria to determine if they will label something as a disease: (1) the disease must show impairment of normal functions and cause morbidity, which obesity met by the impairment of normal functions due to inflammation, insulin resistance, dyslipidemia, as well as the impairment of hypothalamus (6). The characteristic of harm or morbidity was met due to obesity-related complications such as cardiovascular disease, type II diabetes, metabolic syndrome, cancers, and early death (6). The majority of the medical organizations accepted the AMA’s determination.
A chronic disease can be defined as a disease that causes the entire body, specific organ(s), or system to malfunction over time (6). Chronic stages of diseases have the potential to initiate end-organ dysfunction and cause other diseases. The Obesity Society supports that obesity is a chronic disease. Obesity leads to structural abnormalities such as left ventricular hypertrophy, ectopic fat deposits, lymphedema, and excess or enlarged adipose tissue; manifestations include insulin resistance, dyslipidemia, chronic inflammation, and urinary incontinence (6).
Obesity has been associated with 236 other conditions and is a positive cause for many chronic conditions such as diabetes, hypertension, hyperlipidemia, and non-alcoholic fatty liver disease (NAFLD) (6).
Essentially, these terms and definitions are used to illustrate the desperate need to manage obesity to reduce morbidity and mortality. A prominent physician, Dr. Hamdy, proclaimed; “obesity is indisputably the greatest preventable health-related cause of mortality after cigarette smoking” (6).


Self Quiz
Ask yourself...
- Can you discuss the process of classifying a condition as a disease?
- What medical organizations and regulatory agencies are involved in the obesity crisis?
- Can you name conditions that are associated with obesity?
- Are you familiar with the impact and harm that obesity has on specific organs?
Epidemiology
Recent studies found that roughly 16% of adults across the world are obese, and the worldwide prevalence of obesity more than doubled between 1990 and 2022 (12). The prevalence of overweight and obesity among children and adolescents aged 5–19 has risen dramatically from just 8% in 1990 to 20% in 2022 (12). Nearly one-third of adults in the United States are obese (9).
Obesity was once considered to be an issue only among high-income countries; however, obesity is on the rise in low- and middle-income countries.
The prevalence of obesity is slightly higher among women than men and is currently highest among adults aged 40–59 (4). In the United States, the economic burden is estimated to be about $100 billion annually (9).
Obesity is complex and involves a variety of genetic, environmental, and physiological factors.
Here is an overview of the key components:
Genetic Factors
Genetics plays a significant role in determining an individual’s susceptibility to obesity. Variations in genes that control appetite, metabolism, and fat storage can contribute to obesity. Epigenetic changes and environmental factors can cause changes in gene expression, which doesn’t alter the DNA sequence, but potentially affects body weight regulation (4).
Environmental Factors
Obesity occurs when energy intake exceeds energy expenditure over a prolonged period. The body stores excess energy as fat. High-calorie, high-fat, and high-sugar diets contribute to excessive calorie intake and weight gain. Sedentary lifestyles and low physical activity reduce energy expenditure and promote weight gain.
Significant physiological factors include hormonal regulation, energy balance, adipose tissue function, inflammation, neuroendocrine abnormalities, and psychological factors (11). This will be further explored in the next section.

Self Quiz
Ask yourself...
- Can you describe the genetic and environmental factors that correlate with obesity?
- Considering one-third of the population is considered obese, how does this impact your view of the patient population you care for?
- Can you explain the modifiable risk factors associated with obesity?
- How can the nurse provide education on the environmental factors of obesity?
Etiology
The traditional understanding of obesity solely focuses on increased caloric intake compared to energy expenditure (10). However, obesity can also occur secondary to diseases, medications, and other dysregulation of normal body functions. Essentially, nutrition management and increased activity are vital to weight loss, they are no longer the sole appropriate management.
Common mechanisms involved in the development of obesity include lifestyle, inflammation, dysbiosis in the microbiome of the GI system, and genetic mutations.
Genetics and epigenetics can cause alterations or resistance in storing adipose tissue or driving appetite (10). The microbiome of the GI system can alter the gut’s immunologic and absorptive ability as well. Diseases and medications can cause large shifts in metabolism, which causes higher adiposity (10).
Physical Activity and Diet
An individual’s lifestyle as a cause of obesity mainly accounts for physical activity and diet. The pathophysiology of obesity is closely linked with physical activity and diet, and are the first behavioral factors that are modified in the initial treatment of obesity. Minimal physical activity leads to lowering energy expenditure and expediting age-related loss of lean mass, coactively resulting in fat weight gain.
Physical activity is particularly important to energy balance, and minimal physical activity is associated with higher rates of chronic diseases and reduced life expectancy (10). The medical community proclaims that physical inactivity is on par with the risk factors established with smoking.
In a study that followed 50,277 women for 6 years, each was diagnosed with obesity but free from diagnosed cardiovascular disease, diabetes, and cancer, it was found the following: (1) A 2-hour increment per day in TV-watching was associated with a 23% increase in obesity, (2) each 2-hour additional increment per day sitting at work was associated with a 5% increase in obesity; but with the addition of a 1-hour daily spent brisk walk, there was a 24% reduction in obesity (10).
Similarly, diet is an important component of healthy weight. The number of calories is important; however, the composition of the nutrients in food intake is a critical aspect.
Food distribution and processed foods (since the 1970s) have shifted the average diet towards increased caloric intake, increased carbohydrates, refined fats, increased glycemic index, and increased portion sizes at each meal. Between 1962 and 1990, the use of vegetable oils correlated with a 10–13% global increase in fat availability, with an overall decrease availability of fruits, fiber, and other complex carbohydrates (10). These dietary fats negatively affect metabolism and alter gut epithelial permeability, which ultimately compromises macronutrient absorption, inflammation, and microbiome flora. In addition, the decrease in fiber causes a decrease in bowel motility, intestinal absorption, colonic microbiota, and fermentation (10).
Pathophysiology
Understanding the pathophysiology of obesity requires a holistic approach that considers the various factors, including adipose tissue function, inflammation, hormonal imbalances, gut microbiome impact, and psychological health.
Adipose tissue is essentially known as body fat. Adipose tissue is a key part of maintaining physiologic homeostasis because it stores lipids as a long-term energy reservoir. This tissue is found all over the body, including under the subcutaneous skin layer (subcutaneous fat), packed around internal organs (visceral fat), between muscles, within the bone marrow, and in breast tissue (11).
In obesity, adipose tissue enlarges and expands to adapt to higher demands of energy storage. Adipose inflammation presents as enlarged adipocytes which turn apoptotic, which are surrounded by macrophages, and appear as crown-like structures (10). These interactions between adipocytes and immune cells cause increased inflammatory responses, which target tissue and ultimately result in insulin resistance and hyperinsulinemia, hyperglycemia, hyperlipidemia, and vascular injury (10).
- Adipose Tissue Function (11):
- Adipocyte Hypertrophy: The adipocytes (adipose tissue cells) enlarge as they store more fat.
- Adipokines: Adipose tissue cells secrete various signaling molecules (adipokines) that can influence inflammation, insulin sensitivity, and energy metabolism.
Insulin resistance can lead to increased fat storage and difficulty regulating blood sugar levels. Inflammation and poor energy metabolism further the damage and fat storage, and a cycle occurs.
Inflammation
Chronic low-grade inflammation is common in obesity, driven by increased production of pro-inflammatory adipokines and infiltration of immune cells into adipose tissue (10). This inflammation is seen in the circulatory system and often seen in organs that impact metabolism, such as the liver, brain, pancreas, and adipose tissue (10).
The immune system is then impacted as well. Additionally, this inflammation is linked to an increased risk of cancer and infectious disease in obese patients. It is estimated that 3.6% of all new cancer diagnoses are due to excess adiposity (10).
Hormonal Imbalance
Hormonal regulation and appetite are a key factor in obesity. Leptin is produced by fat cells and signals the brain to reduce appetite. Obesity is often associated with leptin resistance, where the brain does not respond appropriately to leptin signals.
Ghrelin is a peptide hormone, known as the “hunger hormone,” and is responsible for the stimulation of appetite, energy homeostasis, and carbohydrate metabolism (13). Ghrelin’s orexigenic (appetite-stimulating) effects are controlled by a need-driven homeostatic state and have central actions on reward, memory, and motivated feeding behavior (10). Levels of ghrelin increase before meals and decrease after eating. Studies have found that ghrelin is commonly lower among those with obesity (10).
Adiponectin is an adipocyte-derived hormone with complex biology. It is widely researched as a possible treatment for obesity due to reported anti-hyperglycemic, anti-atherogenic, and anti-inflammatory effects (11).
Gut Microbiome Dysbiosis
The composition of gut bacteria can influence nutrient absorption, energy balance, and inflammation. Disturbances in gut microbiota have been linked to obesity. Gut bacteria can instigate obesity and insulin-resistance (IR)-associated inflammatory state through lipopolysaccharide (LPS; a component of gram-negative bacterial cell-wall), which triggers inflammation by binding to toll-like receptor-4 (TLR-4) complex at the surface of innate immune cells. A high-fat-high-carbohydrate meal induces significant elevations in postprandial plasma LPS, revealing that endotoxemia may play a pathological role in an obesity-associated inflammatory state and that food ingestion may affect plasma endotoxin levels (10).
Neuroendocrine Factors
The hypothalamus, located in the brain, plays a role in regulating hunger and energy expenditure. Dysregulation of hypothalamic function can contribute to obesity. Foods high in sugar and fat can activate the brain’s reward system, involving neurotransmitters like dopamine, which can also influence eating behavior and lead to overeating.
Psychological Factors
Stress, depression, and other psychological factors can impact eating habits, physical activity levels, inflammation, hormonal balances, and other disease processes. Psychological stress has significant indirect and direct roles in the development of obesity over time. Stress impacts decision-making capacity, reasoning, and self-regulation.
Stress also causes the release of glucocorticoids, which cause physiological changes in the hypothalamic-pituitary-adrenal axis, which affects reward processing in the brain and can lead to “emotional eating” (10).
The HUNT-2 study assessed 65,648 adults between 20 and 89 years of age and found a pattern between abdominal obesity and both anxiety and depression (10).
Complications of Obesity
Obesity may cause the following complications:
- Type 2 diabetes
- High blood pressure
- High cholesterol
- Heart disease
- Stroke
- Metabolic syndrome
- Fatty liver diseases
- Some cancers, such as pancreatic, colon, breast, and liver cancers
- Respiratory problems
- Osteoarthritis
- Gout
- Diseases of the gallbladder and pancreas
- Kidney disease
- Pregnancy problems
- Fertility problems
- Sexual function problems
- Urinary incontinence
- Mental health problems
Medications Associated with Weight Gain
Anti-hypertensive medications are sometimes associated with body weight gain; these include some beta-blockers and calcium channel blockers (8). Hormone therapies can promote body weight gain, including glucocorticoids and injectable progestins (8). Certain anti-seizure medications are associated with weight gain including carbamazepine, gabapentin, valproate, and pregabalin. Antidepressants that are associated with body weight gain include some tricyclic antidepressants, selective serotonin reuptake inhibitors (paroxetine), some selective serotonin and norepinephrine reuptake inhibitors (venlafaxine), as well as mirtazapine, brexpiprazole, and trazodone (8). Migraine medications most associated with body weight gain include amitriptyline, gabapentin, paroxetine, valproic acid, and some beta-blockers. Antipsychotics, chemotherapeutic, and anti-inflammatory agents are also reported to cause weight gain (8).

Self Quiz
Ask yourself...
- How does the physiology of the gut microbiome impact nutrient absorption and hormonal balance?
- Can you describe the relationship between inflammatory and immunological factors in obesity?
- Have you noted a correlation between obesity and depression or anxiety among patients you have cared for?
- Can you name other conditions that can correlate with immunological response (such as cancer, and autoimmune diseases)?
Social Determinants of Health (SDOH) and Obesity
Social determinants of health (SDOH) refer to the conditions in which people are born, grow up, reside, work, and age (7). These factors significantly influence health outcomes, including the prevalence of obesity. Understanding the relationship between SDOH and obesity is vital in creating effective interventions to combat this complex health issue.
 Figure 1. Social Determinants of Health (7)
Figure 1. Social Determinants of Health (7)
Here are key social determinants that impact obesity:
- Healthcare Access and Quality
- Access to preventive services, including nutritional counseling and weight management programs, is essential.
- Disparities in healthcare access and quality can exacerbate obesity rates in underserved communities.
- Economic Stability
- Lower income levels are often associated with higher rates of obesity (7). Limited financial resources can restrict access to healthy foods and opportunities for physical activity. Individuals or families with lower incomes may rely on cheap, calorie-dense foods, leading to weight gain.
- Job security and job environments can influence lifestyle choices. Sedentary jobs, long working hours, and stress can contribute to weight gain (7).
- Education
- A lack of knowledge about healthy eating and cooking can result in poor dietary choices.
- Higher levels of education are generally linked to better health outcomes, including lower obesity rates. Education provides knowledge about nutrition and healthy lifestyles that can improve health literacy.
- Access to education about healthy eating and physical activity within the community and schools is crucial.
- Social and Community Context
- Strong and positive social networks can promote healthy behaviors through shared activities and encouragement. Conversely, social isolation can lead to unhealthy eating and inactivity.
- Cultural attitudes toward nutrition, body image, and physical activity can impact obesity rates.
- Neighborhood and Physical Environment
- Access to healthy and affordable food options is meaningful to weight management. Living in a food desert, where access to fresh, healthy foods is limited, can increase the risk of obesity. Conversely, areas with abundant fast-food outlets and convenience stores can promote unhealthy eating habits.
- Unsafe neighborhoods can discourage outdoor physical activities, leading to sedentary lifestyles.
- The availability of walking areas, parks, recreational facilities, sidewalks, and safe neighborhoods encourages physical activity. Urban planning that promotes walkability and physical activity can help reduce obesity rates.
- Cramped living conditions can have a negative impact on nutritional choices and physical activity.
Addressing Social Determinants
Effective strategies to combat obesity must address these social determinants. This includes (7):
- Policy Interventions: Implementing policies that ensure equitable access to healthy foods, safe environments for physical activity, and affordable healthcare.
- Community Programs: Developing community-based initiatives that educate and support individuals in making healthy choices.
- Cross-Sector Collaboration: Engaging multiple sectors, including education, healthcare, housing, and urban planning, to create a supportive environment for healthy living.
Understanding and addressing the social determinants of health is crucial in the fight against obesity. By tackling these underlying factors, we can create a healthier society and reduce the prevalence of obesity-related health issues. By understanding the demographics of obesity, healthcare providers, public health officials, and policymakers can design and implement more effective strategies to reduce its prevalence and associated health risks

Self Quiz
Ask yourself...
- How does access to fast food restaurants versus fresh markets impact overall weight management?
- Do you think that communities can have a positive impact on obesity?
- How can job security and workplace environments impact health?
- Can you name the five categories of Social Determinants of Health (SDOH)?
Assessment
Screening for obesity is critical. The United States Preventative Services Task Force (USPSTF) recommends that all children six years and older, adolescents, and all adults should be screened for obesity (9). This screening is an ongoing assessment.
Providers should carefully screen for underlying causes contributing to obesity.
Obesity is a key pathophysiologic driver of diabetes, other cardiovascular risk factors (e.g., hypertension, hyperlipidemia, nonalcoholic fatty liver disease, and inflammatory state), and ultimately cardiovascular and kidney disease (10). Diabetes can further exacerbate obesity, setting up a vicious cycle that contributes to disease progression and the occurrence of complications.
A thorough history and physical exam are essential.
Collect History
- Childhood weight history
- Prior weight patterns
- Weight loss efforts and results
- Sleep patterns
- Physical activity routine
- Nutritional intake and diet regimen
- Past medical histories
- Cardiovascular, diabetes, thyroid disorders, mental health disorders.
- Surgical history
- Medications
- Note and discuss medications that contribute to weight gain
- Social histories
- Tobacco, alcohol, or illicit drug use
- Family history (8)
Body Weight History
- The pattern of body weight gain over their lifetime (e.g., slow & gradual, rapid & sudden, or combination)
- Factors influencing weight change
- Physical health or surgeries
- Mental health
- Medications
- Life circumstances (family, newborn, stress, work, moving, finances, abuse)
- Past strategies/behaviors/interventions proven effective and ineffective
- Impact of current and past body weight on mobility, interaction with family and friends, work
- Current or anticipated barriers to future weight loss (8)
Nutrition History
- Meals and Snacks:
- Frequency or timing
- Nutritional content and amount
- Food preparation habits
- Physical/financial access to foods
- Location of food sources
- Behavior
- History of diets (successful or unsuccessful)
- If unsuccessful, what were short- and long-term barriers to achieving or maintaining weight loss
- Triggers (hunger, cravings, anxiety, boredom, reward, etc.)
- Nighttime eating habits
- Readiness for change
Physical Activity History
- Success and/or failure of previous physical activity/exercise efforts
- If routine physical activity/exercise regimen was discontinued:
- When? (Date of change)
- What? (Cause of change)
- Why? (Identify barriers to re-engagement)
- Current physical activity (FITTE)
- Frequency
- Intensity
- Time or Duration
- Type
- Enjoyment (physical activity/exercise preferences)
- Endurance capacity
- Mobility limitations
- Access to locations amenable to increased physical activity/exercise (e.g., exercise facilities, walking paths, urban or rural home settings)
- Physical, social, financial, and perceived barriers to increased physical activity
Focused Physical Examination
Following a general head-to-toe physical examination, a focused examination is vital. This should include body mass index (BMI) measurement, weight circumference, and vitals.
A standard screening tool for obesity is the measurement of body mass index (BMI). BMI is calculated using weight in kilograms divided by the square of height in meters.
Obesity can be classified according to BMI (9):
- Underweight: Less than 18.5 kg/m2
- Normal range: 18.5 kg/m2 to 24.9 kg/m2
- Overweight: 25 kg/m2 to 29.9 kg/m2
- Obese, Class I: 30 kg/m2 to 34.9 kg/m2
- Obese, Class II: 35 kg/m2 to 39.9 kg/m2
- Obese, Class III: more than 40 kg/m2
The waist-to-hip ratio should be measured. More than 1:1 in men and more than 0:8 in women is considered significant.
Make note of the following:
- Acne patterns and appearance
- Excessive hair growth (Hirsutism)
- Skin tags
- Darkening or thickening of the skin (Acanthosis nigricans)
- Usually occurs in intertriginous areas. This hyperpigmentation usually occurs in skin fold areas, such as the back of the neck, axilla, and groin, and may include thickening of the skin (3).
- Gynecomastia, abdominal pannus, hepatosplenomegaly, hernias, hypoventilation, pedal edema, varicoceles, stasis dermatitis, and gait abnormalities can be present.
The following additional evaluations can be performed (9):
- Skinfold thickness
- Bioelectric impedance analysis
- CT, MRI, DEXA
- Water displacement
- Air densitometry studies
Laboratory Studies
Laboratory studies include a complete blood count, basic metabolic panel, renal function, liver function study, lipid profile, HbA1C, TSH, and vitamin D levels. Labs should be ordered based on individualized care for higher risk factors, signs and symptoms, and medical conditions.
- Complete blood count (CBC)
- Comprehensive metabolic panel (CMP)
- Fasting blood glucose
- Liver enzymes
- Renal function
- Electrolytes
- Fasting lipids
- Triglycerides
- Low-density lipoprotein (LDL) cholesterol
- High-density lipoprotein (HDL) cholesterol
- Total cholesterol
- Hemoglobin A1c (HbA1c)
- Thyroid-stimulating hormone (TSH)
- 25-hydroxyvitamin levels
Individualized Laboratory Studies:
- Urinalysis and/or urine for microalbumin/creatinine for patients at risk for kidney disease
- Diabetes, hypertension, nephrotic syndrome, etc.
- Glucose tolerance testing
- Fasting insulin testing or other indices of insulin resistance
- Prolactin, estradiol, follicle-stimulating hormone, luteinizing hormone, and pregnancy test in women with unexplained oligomenorrhea or amenorrhea.
- Testosterone for men with impotence or hypogonadism.
- Iron studies in patients with a history of bariatric surgery.
- High-sensitive C-reactive protein (hs-CRP) can also be used for cardiovascular risk management (8)
Diagnostic Testing
Additional studies such as ECG, cardiac testing, and sleep studies may also be appropriate to evaluate associated medical conditions (8, 9).
- Cardiac stress testing
- Echocardiogram
- Coronary calcium scores
- Ankle-brachial index
- Sleep studies
- Imaging of the liver
- Resting metabolic rate (RMR)

Self Quiz
Ask yourself...
- How would you calculate an individual’s body mass index (BMI)?
- What are the categories of obesity using BMI?
- What labs are typically used in the evaluation of a patient with obesity?
- Are you familiar with measuring the waist-to-hip ratio?
Diagnosis
To diagnose obesity, BMI measurement and clinical assessment of weight-related complications are recommended (5).
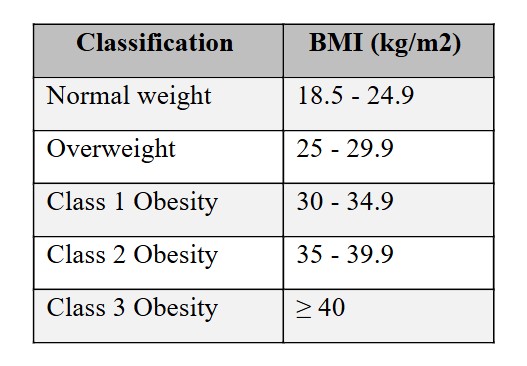 Figure 2. Body Mass Index (5)
Figure 2. Body Mass Index (5)
The severity of obesity should be evaluated based on an overall assessment of adipose tissue mass, distribution (using measurements like waist circumference, waist-to-hip circumference ratio, or waist-to-height ratio), and the presence of associated health or well-being harm, including metabolic, physical, or psychological well-being (6).
Body mass index (BMI) is helpful in the overall classification, but BMI should not be solely relied on as a diagnostic and staging tool. BMI can lead to misclassification, especially in those who are very muscular or frail, as well as in populations with different body composition and cardiometabolic risk (6). BMI is an imperfect measurement of adipose tissue mass and does not measure adipose tissue distribution or function and does not factor in the presence of weight-related health or well-being consequences.
Body composition is an optimal tool for determining health risks. In this regard, several techniques have been developed; for example, an Air Displacement Plethysmograph (ADP) that uses whole-body densitometry to determine body composition (body fat vs. muscle mass). Lean tissue, which is >70% water, is a good conductor of electrical current, whereas fatty tissue, which is hydrophobic and low in water, is not. An increase in body fat is associated with increased electrical resistance combined with a skinfold thickness measure for subcutaneous fat.
Men and women have significant differences in their fat mass and distribution patterns. A healthy body fat amount in men is considered to be between 12 and 18% (3% is essential for insulation and protecting vital organs). For women, a healthy body fat level falls between 20 and 25% (12% is considered essential for normal reproductive function).

Self Quiz
Ask yourself...
- Why is solely using a BMI for diagnosing obesity unreliable?
- How does fat mass distribution differ between men and women?
- What are ways that obesity can have a psychological impact on a patient?
- Is muscle tissue or fat tissue higher in water content?
Guidelines for Management of Obesity
The current standard of care in the management of overweight and obesity in adults was outlined in two guidelines developed by the following organizations (5):
- The American College of Cardiology (ACC), the American Heart Association (AHA), the Obesity Society (TOS)
- The American Association of Clinical Endocrinologists (AACE) and the American College of Endocrinology (ACE)
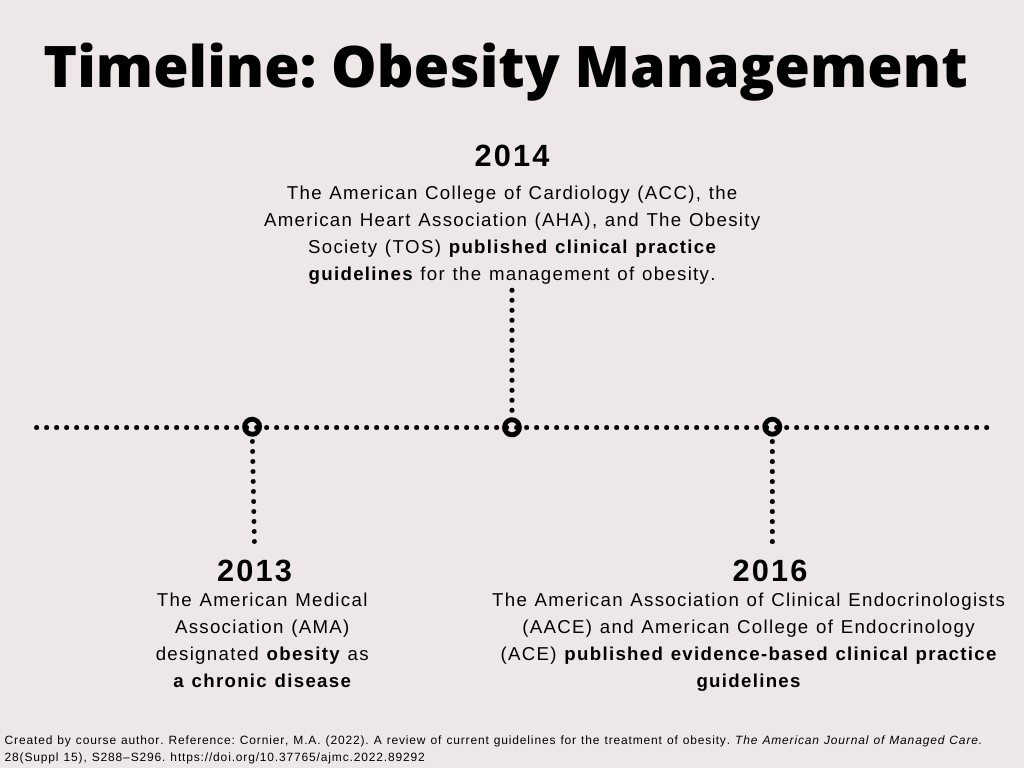 Figure 3. Timeline: Obesity Management
Figure 3. Timeline: Obesity Management
Various leaders in the field have developed complementary guidance. Additionally, several pharmacotherapies have been approved by the FDA for the treatment of obesity, as well as procedures and devices for weight loss. Research in obesity treatment continues to progress.
The primary entity in charge of guidelines for obesity and weight management in the United States is the National Institutes of Health (NIH), specifically the National Heart, Lung, and Blood Institute (NHLBI). This organization publishes the clinical guidelines for the identification, evaluation, and treatment of overweight and obesity in adults.
The NIH collaborates with the American College of Cardiology (ACC) and the American Heart Association (AHA) to develop and endorse these guidelines.
On a global scale, the World Health Organization (WHO) provides international guidelines and standards for obesity and weight management.
Other notable organizations involved in creating and updating guidelines include:
- Centers for Disease Control and Prevention (CDC)
- American Medical Association (AMA)
- American Academy of Pediatrics (AAP)
- Obesity Society
These organizations work together to provide evidence-based recommendations for healthcare providers and the general public.
Treatment
Weight management and weight loss are fundamental goals in treating obesity. Managing obesity requires ongoing collaboration with a committed patient and informed clinicians. In patients diagnosed with obesity, weight-related complications should be evaluated at regular intervals. Obesity requires a multifaceted, patient-centered, individual approach, not a “one size fits all” approach.
A reduction in caloric intake forms the foundation of any weight-loss strategy. According to both guidelines, individuals with obesity who intend to lose weight should be given guidance on:
Both guidelines recommend that patients pursue behavioral interventions that foster adherence to physical activity and meal plan prescriptions. Interventions are often multidisciplinary, including dietitians, psychologists, and psychiatrists. Participation could be in-person or remotely, but consistency is key.
Several factors can impact the management of obesity:
- Age
- Race
- Gender
- Individual physiology
- Economic status
- Understanding of nutrition and physical activity
- Current medications
- Concurrent illnesses
- Home environment (e.g., employment, food access, stressors, family dynamics, culture, school, travel)
- Work environment (e.g., food access, stress, nature of work, wellness programs, travel
- Use of apps, text messages, and social media
- Ability to obtain wearable technologies
- Bariatric surgery
Use of Sensitive Terminology on Obesity
It is meaningful to be mindful of the harm terminology can cause. Certain words are attached to shame, and shame has no place in the management of obesity. “People-first” language recognizes the potential hazards of referring to or labeling individuals by their disease. “Patient who has pre-obesity or obesity” or “patient with overweight or obesity” are preferred over “obese patient.”
- Encouraged Words:
- Weight
- Overweight
- Body mass index
- Affected by obesity
- “Patient who has obesity”
- Discouraged Words:
- Morbidly obese
- Heavy
- Fat
- Large size
- “Obese patient”
Healthcare Environment Consideration
Patients with obesity may likely have negative feelings or prior experiences when in healthcare environments. Providers and staff should receive training on weight bias and providing a supportive environment.
Appropriate medical equipment should be available, including large adult blood pressure cuffs (or thigh cuffs on patients with an upper-arm circumference greater than 34 cm), longer needles to draw blood, larger gowns, large vaginal specula, and scales with the capacity to measure weight more than 400 pounds. Privacy should be a priority, ensuring their right to privacy and dignity; thus, weight scales are optimally located in a private area wherein the value is only seen by the patient and provider (8).

Self Quiz
Ask yourself...
- Which of the following statements reflects “people-first” language: (1) “Have you tried a diet plan for obese people? Or (2) “Specific and achievable goals are meaningful for individuals who are affected by obesity”?
- Do you consider weighing scales in a general waiting area, with a large digital reading of the weight, as a violation of privacy rights?
- Can you discuss why obesity management plans should be highly individualized?
- Why is it important to provide larger gowns or apply larger cuffs initially?
Initial Management of Overweight and Obesity
A structured lifestyle intervention program designed for weight loss that includes a healthy meal plan, physical activity, and behavioral intervention is recommended for all patients who are overweight or obese (5). These include (5):
- Recommend 30–60 min of moderate physical activity on most days of the week, taking physical impairments and medical conditions into consideration.
- Nutrition education focuses on decreased caloric intake, encouraging healthy food choices, and minimizing restaurant and social eating situations.
- Encourage consumption of 5–6 servings of fruits and vegetables daily.
- Weekly weight checks.
- Encourage nonfood rewards for positive reinforcement.
- Stress management techniques.
Nutrition Interventions
Maintaining healthy nutrition habits is essential. It is important to emphasize life-long maintainable habits instead of “crash diets”.
When providing guidance on nutrition, the following are important points to recognize (8):
- Nutrition therapy has optimal health outcomes when the dietary interventions are evidence-based, quantitative, qualitative, and achieve patient adherence.
- A low-calorie diet is 1200 to 1800 kcal/day; a very low-calorie diet is generally < 800 kcal/day. Each recommendation should be individualized.
- The substitution of saturated fats with ultra-processed carbohydrates does not improve cardiovascular disease risk.
- Low-carbohydrate diets typically consist of 50 – 150 grams of carbohydrates per day; very low-carbohydrate diet is < 50 grams of carbohydrates per day
- A ketogenic diet plan restricts carbohydrate intake and typically encourages avoidance of ultra-processed and refined foods, foods high in glycemic index/load, and foods rich in trans fatty acids.
- A Mediterranean diet plan encourages the intake of vegetables, fruits, legumes, whole grains, nuts, seeds, seafood, olive oil, poultry, eggs, and red wine; this diet discourages high amounts of red meats, meat products, and ultra-processed carbohydrates.
- A DASH dietary pattern encourages vegetables, fruits, whole grains, fat-free or low-fat dairy products, fish, poultry, lean meats, nuts, seeds, legumes, fiber, high-calcium foods, potassium, and magnesium. A major component of this diet is the following restrictions:
- Sodium intake less than 2300 mg per day
- Total fat intake less than 27% of total daily calories
- Cholesterol intake of less than 150 mg per day
- Vegetarian diets encourage vegetables, fruits, whole grains, legumes, seeds, and nuts.
- Fasting (alternative day, intermittent, or time-restricted eating) has been shown to contribute to overall caloric restriction and weight reduction.
- In general, low-calorie and non-nutritive sweeteners may have physiologic and/or metabolic effects of unknown clinical significance. Saccharin may increase body weight compared to aspartame, rebaudioside A, and sucralose (8).
 Figure 4. Energy Consumption Intended to Cause Negative Calorie Balance and Loss of Fat Mass (8)
Figure 4. Energy Consumption Intended to Cause Negative Calorie Balance and Loss of Fat Mass (8)
Consider the following:
- Comorbidities that could be affected by the nutrition plan
- Eating behaviors
- Cultural background
- Food availability
- Time constraints and financial issues
- Nutritional knowledge and cooking skills
The AACE/ACE guidelines recommend that behavioral interventions be escalated for patients who do not achieve 2.5% weight loss within 1 month of starting treatment (5). An in-person, high-intensity program (≥14 sessions in 6 months) is considered the most effective behavioral treatment for overweight or obesity (5).
Referral to a nutrition professional can be prescribed in patients who are agreeable to this intervention. It is important to evaluate their current understanding and habit

Self Quiz
Ask yourself...
- What are the key elements of the Mediterranean diet?
- What is the weight loss percentage goal within the first month of treatment?
- Are you familiar with effective diet plans such as the DASH or ketogenic plan?
- Can you describe a holistic diet plan for patients with kidney or heart disease in addition to obesity?
Individualized Exercise / Activity Guidance
Physical activity is essential in the management of obesity, but the plan must be highly individualized.
Considerations to ensure safety:
- Assess current physical limitations and mobility status.
- Review previous injuries or surgeries.
- Assess the patient’s readiness
- Discuss expectations and goals
- Assess potential need for medical testing/evaluation (i.e., cardiac stress testing, pulmonary function tests, musculoskeletal assessment, etc.)
- Evaluate medications for contraindications with activity
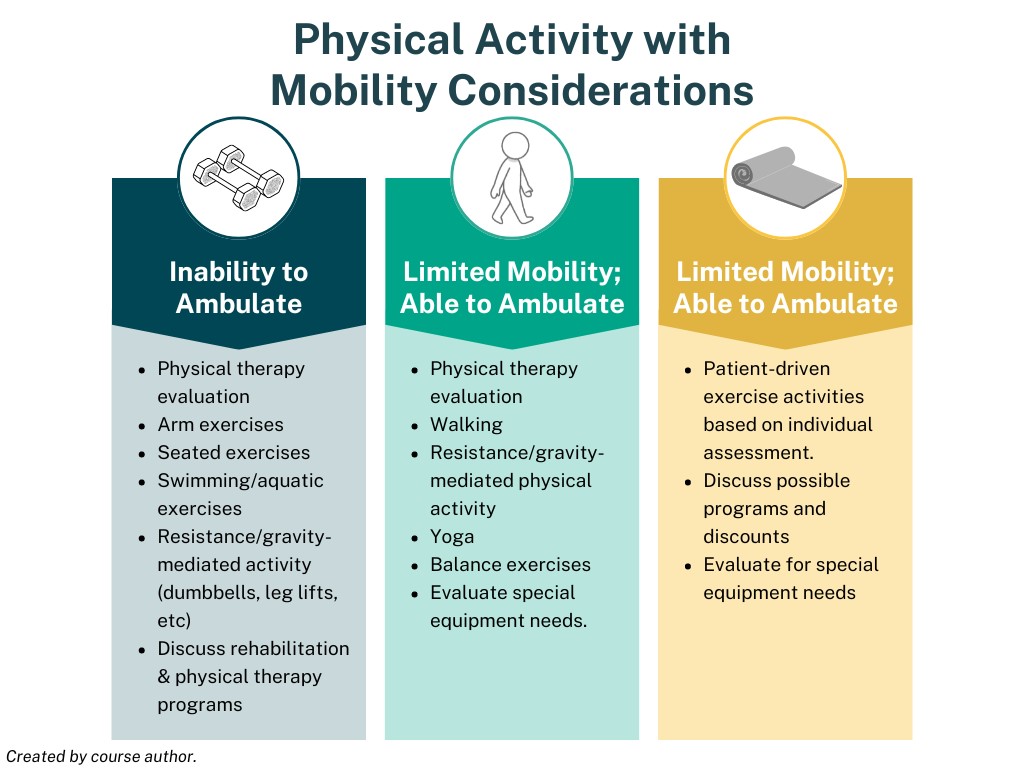 Figure 5. Physical Activity and Mobility Considerations
Figure 5. Physical Activity and Mobility Considerations
Metabolic Equivalent Tasks
- Metabolic Equivalent Tasks (METS) are used to assess the intensity of physical exercise (Kcal = METS x weight x time) and are equal to the amount of energy expended in one minute while lying down at rest (8)
- METS = 3.5 milliliters of oxygen consumption per kilogram of body weight per minute (3.5 ml/kg/min)
- Note: Oxygen consumption and demand vary with increased age and respiratory or cardiac diseases.
- Standing = 2 METS
- Walking 4 miles per hour = 4 METS
- Running 10 miles per hour = 16 METS
Behavioral Interventions
The recruitment of behavioral therapies can be an effective tool. The following specialties are resources:
- Dietitian
- Nurse educator
- Physical activity professional trainer
- Mental-health professional
- Certified health coach
- Web-based mental health support programs
Therapies and techniques can include self-monitoring, stimulus control, cognitive restructuring, goal setting, problem-solving skills, and social support (8).

Self Quiz
Ask yourself...
- What are the key components for effective behavioral intervention in the management of obesity?
- What role do self-monitoring and self-regulation play?
- How can physical exercise regimens be tailored to the individual needs of patients?
- How can social support systems influence better outcomes?
Pharmacological Treatment
Research has found that pharmacotherapy used with lifestyle modifications correlates with greater and more sustained weight loss when compared with lifestyle modifications alone (8).
The amount and duration of weight loss varies among patients taking an anti-obesity medication. Patients have an average of 5 – 10% weight reduction (8).
FDA-approved Anti-obesity Medication Indications:
- Patients with obesity (e.g., BMI > 30kg/m2)
- Patients with overweight (e.g., BMI > 27kg/m2) with the presence of complications (e.g., type 2 diabetes mellitus, hypertension)
- If no clinical improvement (e.g., at least 3 – 5% loss of baseline body weight) after 12-16 weeks, consider alternative anti-obesity medication or increasing dose of current regimen.
BMI is the only measure listed in the prescribing information for these anti-obesity medications, but prescribers must recognize the limitations of BMI measurement, especially in those with higher mass of lean muscle.
In general, anti-obesity drugs are contraindicated in pregnancy, and should be avoided in women who are pregnant, trying to become pregnant, or who are breastfeeding (8).
All anti-obesity medications have contraindications for hypersensitivity to the drugs.
Medications Approved for Short-Term Use:
- Phentermine
- Diethylpropion
- Phendimetrazine
- Benzphetamine
Medications Approved for Long-Term/ Chronic Use:
- Orlistat
- Liraglutide
- Phentermine HCl/topiramate extended-release
- Naltrexone HCl/bupropion HCl extended-release
- Semaglutide
The table below outlines medications that are approved for use in obesity management.
| Drug | Description | Pharmacokinetics / Warnings | Primary Side Effects |
|
Sympathomimetic Amines Examples:
|
Approved for use in 1959. Used to increase satiety. Drug Enforcement Agency (DEA) Schedule weight management agents:
|
Use with caution in patients with renal impairment; urinary excretion may be 62-85%. Complexed drugs (e.g., phentermine ion-exchange resin) often require gastric enzymes or intestinal flora to become activated. |
|
| Orlistat |
Gastrointestinal lipase inhibitor Not a Drug Enforcement Agency Scheduled drug Dose: One 120-mg capsule three times a day with each main meal containing fat (during or up to 1 hour after the meal). An over-the-counter formulation is available at 60 mg capsule with each meal containing fat |
Orlistat is contraindicated in patients with chronic malabsorption syndrome or cholestasis. Gastrointestinal events may increase when orlistat is taken with a diet high in fat (>30% total daily calories from fat). Orlistat has been shown to reduce the absorption of some fat-soluble vitamins, so patients should be strongly advised to take a multivitamin supplement that contains fat-soluble vitamins to maintain adequate nutrition. |
|
| Liraglutide |
Liraglutide is a glucagon-like peptide-1 (GLP-1) receptor agonist. Not a scheduled DEA drug Subcutaneous injection, pre-filled, multi-dose pen that delivers doses of 0.6 mg, 1.2 mg, 1.8 mg, 2.4 mg, or 3.0 mg Inject subcutaneously in the abdomen, thigh, or upper arm. The recommended dose of liraglutide for treatment of obesity is 3.0 mg. Dosing:
Slower dose titration may improve tolerability and gastrointestinal side effects |
Contraindicated history or medullary thyroid cancer or Type 2 Multiple Endocrine Neoplasia syndrome. Discontinue with suspected pancreatitis, gall bladder disease, or suicidal ideation. May contribute to hypoglycemia. |
|
| Phentermine / Topiramate |
Combination of phentermine and topiramate DEA Schedule IV drug. Topiramate is a drug used to treat seizures and migraine headaches. |
Phentermine is metabolized by the liver, with most excreted by the kidney. Topiramate is excreted primarily by the kidney. May potentiate central nervous system depressants such as alcohol Can potentiate hypokalemia of non-potassium-sparing diuretics Phentermine is contraindicated during or within 14 days following the administration of monoamine oxidase inhibitors due to risk of hypertension. |
|
| Naltrexone / Bupropion |
Combination of naltrexone (opioid antagonist used for addictions) and bupropion (antidepressant). Tablets: 8 mg/90 mg (naltrexone HCl/bupropion HCl extended release) Dosing:
(8) |
Clinicians should monitor for suicidal thoughts and discontinue naltrexone HCl/bupropion HCl if these symptoms are present. Monitor blood pressure and heart rate in all patients, especially those with cardiac or cerebrovascular disease Cases of hepatotoxicity have been reported. |
Patients may report changes in mood (including depression and mania), psychosis, hallucinations, paranoia, aggression, agitation, or suicidal ideation. |
| Semaglutide |
Glucagon-like peptite-1 receptor agonist. Injectable drug. Semaglutide, 2.4 mg weekly is approved for treatment of obesity.
|
Contraindicated in patients with acute pancreatitis, acute gallbladder disease, kidney disease, adverse gastrointestinal reactions, diabetes retinopathy, tachycardia, or suicidal ideations. Associated with hypoglycemia. |
|
Table 1. Approved Obesity Managment Medications (6, 8, 11)


Self Quiz
Ask yourself...
- What are the primary mechanisms by which obesity medications function in the body?
- Can you compare the benefits and risks of the use of obesity medications?
- Which situations may medications be recommended for obesity over other forms of treatment?
- How would you explain the impact of medications on the long-term goals of obesity management?
Surgical Procedures and Devices
Surgical treatment, often referred to as bariatric surgery, can be an effective option for individuals with severe obesity when other weight loss methods have failed, and the patient meets specific criteria.
Bariatric surgery not only can reduce weight, but has the potential to improve obesity-related conditions. The surgery has significant risks to evaluate, so individualized care plans and risk mediation is vital.
The main types of bariatric surgery include (2, 8):
- Roux-en-Y Gastric Bypass (RYGB)
- Sleeve Gastrectomy
- Adjustable Gastric Banding (AGB)
- Biliopancreatic Diversion with Duodenal Switch (BPD/DS)
- Intragastric Balloon
Bariatric surgery programs must meet strict criteria and follow the guidance of the following:
- MBSAQIP Center of Excellence
- Managed by the Metabolic and Bariatric Surgery Accreditation and Quality Improvement Program of the American College of Surgeons
- The most widely used credentialing program for bariatric surgery programs
- Health insurance providers may have specific qualifications.
Eligibility is determined through a rigorous evaluation of patient status. The surgeries are typically only considered for individuals with a certain BMI (often 40 or higher, or a BMI of 35 or higher with obesity-related health conditions).
A Pre-Surgical Evaluation is a core component of the process. A comprehensive assessment including medical, nutritional, psychological, and surgical evaluations occurs. All surgeries carry risks, including infection, bleeding, and respiratory complications. These particular surgeries require a lifelong commitment to dietary changes, regular follow-up, and possibly supplementation to prevent nutrient deficiencies.
Roux-en-Y Gastric Bypass (RYGB)
This procedure involves creating a small pouch at the beginning portion of the stomach and connecting it directly to the small intestine, bypassing a significant portion of the stomach and the upper part of the small intestine (2). Essentially, the process reduces food intake and calorie absorption by altering the digestive process. Providers need to discuss the risks of this surgery, which include but are not limited to nutrient deficiencies, dumping syndrome, complications in surgery, and the potential need for revisional surgery (2).
Sleeve Gastrectomy
This surgery involves removing roughly 80% of the stomach, leaving a tube-like structure in the gastrointestinal tract. The mechanism reduces the stomach’s capacity to hold food, leading to reduced food intake. The is no intestinal bypass involved in this surgery. Potential complications include nutrient deficiencies and surgical complications, such as bleeding or gastric leakage (2).
Adjustable Gastric Banding (AGB)
This procedure involves an adjustable band that is surgically placed around the upper part of the stomach, creating a small stomach pouch above the band. The purpose of the encased and reduced stomach size is to restrict food intake by making the patient feel full after eating small amounts of food (8). The benefits of this surgery are that this banding is adjustable and reversible, and there is a lower risk of nutrient deficiencies. However, risks and complications can occur, including band slippage or erosion (2). Weight loss is typically slower with this procedure.
Biliopancreatic Diversion with Duodenal Switch (BPD/DS)
This is a more complex procedure that involves two processes: a sleeve gastrectomy and the rerouting of the small intestine to separate the flow of food from bile and pancreatic juices. Significant and sustained weight loss has been noted, which effectively improves obesity-related conditions (8). However, the is a higher risk of nutrient deficiencies and increased risk for surgical complications (8).
Intragastric Balloon
In this procedure, a balloon is endoscopically placed in the stomach and filled with saline or gas (2). This serves to reduce stomach capacity and reduce food intake. This procedure is minimally invasive and temporary. Common adverse effects and complications include nausea, vomiting, and deflation or migration of the balloon.
Bariatric surgery can be a life-changing option for many individuals struggling with severe obesity, offering substantial and sustained weight loss and improvement in health. However, it requires careful consideration, thorough and individualized evaluation, and a strong commitment of the patient to post-surgical lifestyle changes.

Self Quiz
Ask yourself...
- Who is the governing body for bariatric surgery accreditations and guidelines?
- Which of these surgeries is the least invasive?
- Can you describe the criteria for bariatric surgery appropriateness?
- Are you familiar with the pre-surgical consultation for bariatric surgery?
Self-Management
“When performance is measured, performance improves. When performance is measured and reported back, the rate of improvement accelerates.” – Pearson’s Law
Losing weight can be overwhelming. Changing lifestyle habits and adjusting to nutrition changes, increased activity, and medications take time and patience. Advocacy and support are essential. These are helpful tips to help maintain and achieve a healthy weight:
- Track progress
- Recruit trusted family and friends for encouragement and accountability.
- Use daily activity logs to track daily food intake and physical activity
- Apps
- Journals
- Notebook
- Whiteboard
- Pedometer logs
- Dynamic training metrics (i.e., miles run, laps swam, etc.)
- Daily weighing has been shown to have a positive impact on long- and short-term weight loss for many people.
- Set specific goals
- Examples: “Walk 30 minutes, 4 days a week”
- Goals must be realistic about time and abilities.
- Gradual changes lead to success.
- Lifestyle is a long-term process.
- Use rewards that are meaningful and non-food if goals are met.
- Identify environments or social activities that hinder goals.
- Example: Specific restaurants, emotional triggers, etc.

Self Quiz
Ask yourself...
- Why is tracking progress so important in obesity management?
- Can you discuss why specific goals are more beneficial than broad goals?
- Would you compare obesity management to a short- or long-term process?
- Can you think of rewards that are not related to food items?
Case Study: Management of a Patient with Obesity and Hypertension
Mr. T is a 52-year-old male who presents to the clinic for a routine check-up. He reports feeling increasingly fatigued and has noticed a significant weight gain over the past year. His blood pressure readings at home are consistently high. He reports taking his medications as prescribed. Mr. T denies any regular exercise, he works full-time as a bank manager.
Assessment
- Blood Pressure: 150/95 mmHg (medication taken at 0700 this morning)
- Heart Rate: 80 bpm
- Height: 5’10” (178 cm)
- Weight: 280 lbs. (127 kg)
- BMI: 40.1
- Waist Circumference: 45 inches
- Medical History: Diagnosed with hypertension 10 years ago, family history of cardiovascular disease, obesity, kidney disease, and diabetes.
- Medications: Lisinopril (10 mg daily) for hypertension.
Laboratory Test Results
- Fasting Blood Glucose: 110 mg/dL
- Lipid Profile:
- Total Cholesterol: 240 mg/dL
- LDL: 150 mg/dL
- HDL: 35 mg/dL
- Triglycerides: 200 mg/dL
- Lipid Profile:
Diagnosis
- Primary Diagnosis: Obesity (Class III)
- Secondary Diagnosis: Hypertension, uncontrolled
Management Plan
Lifestyle Modifications
- Diet: Referral to a registered dietitian for a personalized nutrition plan focusing on a caloric deficit, balanced macronutrients, and reduction of sodium intake.
- Goals: Achieve a weight loss of 1-2 lbs per week through dietary changes. Emphasize whole foods, fruits, vegetables, lean proteins, and whole grains.
- Physical Activity: Encourage a gradual increase in physical activity.
- Begin with 30 minutes of moderate-intensity exercise, such as walking, 5 days a week, increasing intensity and duration as tolerated.
Behavioral Therapy
- Referral to a behavioral therapist for cognitive-behavioral therapy (CBT) to address emotional eating and establish healthier coping mechanisms.
- Goals: Develop strategies for managing stress, triggers for overeating, and adherence to lifestyle changes.
Mr. T is motivated and desires to make these changes to improve his overall health. He becomes active in establishing short and long-term goals with his provider.
- Short-Term Goals (3-6 months):
- Begin walking in the evenings with his wife, after work, for 20-30 minutes at least 5 days per week.
- A coworker attends a weight loss support group that has educational offerings on nutrition and exercise; Mr. T plans to join and become active in this group.
- Achieve a 5-10% reduction in body weight.
- Long-Term Goals (1 year and beyond):
- Maintain weight loss and prevent weight regain.
- Sustain blood pressure control with minimal medication adjustments.
- Reduce the risk of cardiovascular disease.
- Reduce the risk of diabetes.
Follow-Up
- Schedule follow-up visits every 1-2 months to monitor progress, and blood pressure, and adjust the treatment plan as needed. Repeat fasting blood glucose, lipid profile, and other relevant labs every 3-6 months.
- If lifestyle modifications are not effective, consider and discuss pharmacotherapy for weight loss with Mr. T. Evaluate appropriate indications for Phentermine, Phentermine/Topiramate, Orlistat, or Liraglutide, based on the patient’s tolerance and contraindications.


Self Quiz
Ask yourself...
- What specific factors might have contributed to Mr. T’s obesity?
- How does Mr. T’s sedentary lifestyle impact his hypertension and obesity?
- What are the potential health risks associated with his current BMI and blood pressure?
- What alternative treatment options are available if Mr. T does not respond to the initial interventions?
- How might cultural, socioeconomic, or psychological factors influence Mr. T’s ability to follow the treatment plan?
Conclusion
Understanding the etiology, pathophysiology, and complications of obesity is essential in developing a plan to manage obesity. This requires a holistic approach and effective obesity management, and prevention strategies often involve addressing multiple aspects of this complex condition.
References + Disclaimer
- American Diabetes Association (ADA) Professional Practice Committee (2024). Obesity and Weight Management for the Prevention and Treatment of Type 2 Diabetes: Standards of Care in Diabetes–2024. Diabetes Care 1 January 2024; 47 (Supplement_1): S145–S157. https://doi.org/10.2337/dc24-S008
- Arterburn, D. E., Telem, D. A., Kushner, R. F., & Courcoulas, A. P. (2020). Benefits and risks of bariatric surgery in adults. JAMA : The Journal of the American Medical Association., 324(9). https://doi.org/10.1001/jama.2020.12567
- Brady, M.F. & Rawla P. (2023). Acanthosis Nigricans. In: StatPearls [Internet]. Treasure Island (FL): StatPearls Publishing; 2024 Jan-. Available from: https://www.ncbi.nlm.nih.gov/books/NBK431057/
- Centers for Disease Control and Prevention. (2020). Prevalence of obesity and severe obesity among adults: United States, 2017–2018. National Center for Health Statistics. https://www.cdc.gov/nchs/products/databriefs/db360.htm
- Cornier, M.-A. (2022). A review of current guidelines for the treatment of obesity. The American Journal of Managed Care., 28(Suppl 15), S288–S296. https://doi.org/10.37765/ajmc.2022.89292
- Golden, D. (2020). Treating obesity in primary care. Springer Nature.
- Healthy People 2030, U.S. Department of Health and Human Services, Office of Disease Prevention and Health Promotion. (2024). Retrieved from https://health.gov/healthypeople/objectives-and-data/social-determinants-health.
- Obesity Medicine Association. (2023). Obesity algorithm. https://dmiusd4kl5bx2.cloudfront.net/PDF-Files/obesity-algorithm-pdf-2023.pdf
- Panuganti K.K, Nguyen M., Kshirsagar R.K., & Doerr, C. (2023). Obesity (Nursing). In: StatPearls [Internet]. Treasure Island (FL): StatPearls Publishing; 2024 Jan-. Available from: https://www.ncbi.nlm.nih.gov/books/NBK568702/
- So, I., Yadav, H. (2020). Obesity and Its Complications Pathogenesis. In: Tappia, P., Ramjiawan, B., Dhalla, N. (eds) Pathophysiology of Obesity-Induced Health Complications. Advances in Biochemistry in Health and Disease, vol 19. Springer, Cham. https://doi.org/10.1007/978-3-030-35358-2_3
- Tappia, P. S., Ramjiawan, B., & Dhalla, N. S. (2020). Pathophysiology of obesity-induced health complications. Springer.
- World Health Organization (WHO). (2024). Obesity and overweight. Retrieved from https://www.who.int/news-room/fact-sheets/detail/obesity-and-overweight
- Young ER, Jialal I. Biochemistry, Ghrelin. [Updated 2023 Jul 17]. In: StatPearls [Internet]. Treasure Island (FL): StatPearls Publishing; 2024 Jan-. Available from: https://www.ncbi.nlm.nih.gov/books/NBK547692/
Disclaimer:
Use of Course Content. The courses provided by NCC are based on industry knowledge and input from professional nurses, experts, practitioners, and other individuals and institutions. The information presented in this course is intended solely for the use of healthcare professionals taking this course, for credit, from NCC. The information is designed to assist healthcare professionals, including nurses, in addressing issues associated with healthcare. The information provided in this course is general in nature and is not designed to address any specific situation. This publication in no way absolves facilities of their responsibility for the appropriate orientation of healthcare professionals. Hospitals or other organizations using this publication as a part of their own orientation processes should review the contents of this publication to ensure accuracy and compliance before using this publication. Knowledge, procedures or insight gained from the Student in the course of taking classes provided by NCC may be used at the Student’s discretion during their course of work or otherwise in a professional capacity. The Student understands and agrees that NCC shall not be held liable for any acts, errors, advice or omissions provided by the Student based on knowledge or advice acquired by NCC. The Student is solely responsible for his/her own actions, even if information and/or education was acquired from a NCC course pertaining to that action or actions. By clicking “complete” you are agreeing to these terms of use.
➁ Complete Survey
Give us your thoughts and feedback
➂ Click the Green MARK COMPLETE Button Below
To receive your certificate
