Course
Ohio APRN Renewal Bundle – Part 2
Course Highlights
- Understand the ANA Code of Ethics for Nurses as it applies to telehealth nursing.
- Discuss the different treatment options available for people diagnosed with end-stage renal disease.
- Understand the importance and time-sensitive nature of sepsis care.
- Identify two reasons why learning about conflict management is important when fulfilling a nurse leader role.
- Discuss non-pharmacological and pharmacological methods of treating and managing acute pain.
- Recognize the risk of stroke in those with atrial fibrillation.
About
Total Contact Hours Awarded: 24 , including 12 pharmacological contact hours.
Course By:
Multiple Authors
Begin Now
Read Course | Complete Survey | Claim Credit
➀ Read and Learn
The following course content
Ethics for the Telehealth Nurse
With the increasing utilization of telehealth in the healthcare industry, it is vital that nurses become aware of the ethical principles involved in this hands-off, virtual approach to providing patient care. This course provides basic, ongoing, and applicable knowledge of nursing ethics to improve patient outcomes specifically for a telehealth nurse. All nurses are responsible for being familiar with the American Nurses Association’s (ANA) Code of Ethics for Nurses no matter the specialty they are in. The information offered in this course is being given as a guideline and does not replace the laws governing nursing practice.
Introduction
Although the utilization of telehealth has been incorporated into patient care for many decades, the impact of the COVID-19 pandemic has increased its prevalence in the industry; leaving many professionals with no choice but to adapt. With this recent change, most healthcare facilities were forced to create strategies that allowed them to not only prevent viral exposure but continue to provide quality patient care remotely.
As a result, healthcare professionals faced many challenges, especially nurses (2). When considering that the nursing process has been taught, referenced, and utilized as one of the overarching ethical guidelines for hands-on nursing care for hundreds of years, it is evident that nurses have overcome many obstacles in a short period of time.
It is vital for the telehealth nurse to continue to assess and interact with patient populations through this newer method of care while strictly following the American Nurses Association’s (ANA) Code of Ethics for Nurses.

Self Quiz
Ask yourself...
- What do you think it means to be a telehealth nurse?
- What interactions may present ethical or professional challenges for the telehealth nurse while conducting a virtual assessment?
- In what specific ways does the ethical requirements of the nurse differ from face-to-face interactions versus through telehealth?
Nursing Practice for the Telehealth Nurse
The practice of telehealth allows a trained nurse the ability to communicate with patients and their families, provide assessments in real-time, and implement appropriate interventions virtually.
The first telehealth nursing practice standards were published in 1997 by the American Academy of Ambulatory Care Nursing (AAACN) in response to the increased growth in popularity and utility of the field (2). The standards are divided into the domains of either Clinical Practice or Professional Performance; each standard has a set of competencies that the professional nurse must meet when practicing.
Although telehealth nursing does not require direct patient contact, a nurse should uphold the same standards and ensure that their quality of care and compliance with ethical nursing practices does not change (2). It is of the utmost importance that the care provided remains patient-centered and quality-focused, and that the telehealth nurse continues to utilize the nursing process in all patient interactions.

Self Quiz
Ask yourself...
- Is there a difference in the ‘Code of Ethics for Nurses’ practice and those for telehealth nursing practice?
- What is your nursing ethical statement?
Code of Ethics for Nurses
The ANA Code of Ethics for Nurses with Interpretive Statements is the non-negotiable framework surrounding how those in the nursing profession should incorporate both ethical and moral practices into their patient care (2). This code of ethics consists of nine principles that should be strictly followed, these include ():
- The nurse practices with compassion and respect for the inherent dignity, worth, and unique attributes of every person.
- The nurse’s primary commitment is to the patient, whether an individual, family, group, community, or population.
- The nurse promotes, advocates for, and protects the rights, health, and safety of the patient.
- The nurse has authority, accountability, and responsibility for nursing practice; makes decisions; and takes action consistent with the obligation to provide optimal patient care.
- The nurse owes the same duties to self as to others, including the responsibility to promote health and safety, preserve wholeness of character and integrity, maintain competence, and continue personal and professional growth.
- The nurse, through individual and collective effort, establishes, maintains, and improves the ethical environment of the work setting and conditions of employment that are conducive to safe, quality health care.
- The nurse, in all roles and settings, advances the profession through research and scholarly inquiry, professional standards development, and the generation of both nursing and health policy.
- The nurse collaborates with other health professionals and the public to protect human rights, promote health diplomacy, and reduce health disparities.
- The profession of nursing, collectively through its professional organization, must articulate nursing values, maintain the integrity of the profession, and integrate principles of social justice into nursing and health policy (1).
It is of the utmost importance that nurses abide by these nine provisions of the Code of Ethics for Nurses; this is no different for the telehealth nurse (1).
Caring for a patient virtually does not relinquish the telehealth nurse of their duty to be accountable, responsible, compassionate, and respectful.

Self Quiz
Ask yourself...
- What are some areas of ethical responsibility that should be demonstrated by the telehealth nurse during a virtual patient interaction that may differ from a nurse in a face-to-face clinical setting?
Privacy
Telehealth nurses most often are in the same area as other nurses when working and interacting with patients, so it is crucial that patient confidentiality is ensured. The Code of Ethics for Nurses indicates that privacy must be maintained, and the patient should feel comfortable in disclosing sensitive information, even through the utilization of telehealth methods (1).
Because the patient does not have the privacy of an exam room, the nurse should communicate to the patient that measures are in place to provide protection and privacy of their information during the telehealth visit. If the patient verbalizes concern in confidentiality, the nurse must document the patient concerning the patient record (1).

Self Quiz
Ask yourself...
- You are the nurse completing a telehealth call and you are informed by the patient that they do not own a digital device and are staying at a friend’s house for their visit. The patient has given consent to have information disclosed via the connected health interaction. As the telehealth nurse, what would be an ethical decision which you would address during the encounter?
- During a telehealth encounter the patient expresses concern about privacy. How would you provide reassurance to the patient?
Trust
The telehealth nurse has an obligation to initiate and ensure there is trust with the patient, as it is one of the main components of the Code of Ethics for Nurses (1, 2).
As the telehealth nurse, your patient must feel like you are giving accurate information when you are assisting them in making the right decision(s) for their treatment plan. When the patient makes the call to obtain information regarding their care, they are entrusting the nurse to have necessary and applicable knowledge. It is important to note that any initial information provided to the patient prior to consulting with a physician must be supported by evidence-based practices (1).

Self Quiz
Ask yourself...
- What would be an example of unethical documentation during a telehealth encounter which would indicate infringement of trust?
- The safety of patients and healthcare professionals must always be ensured. How could the ethical opinion of the nurse be swayed if the behavior of a physician does not demonstrate user competency in providing safe telehealth practice? What would be the ethical dilemma for the nurse?
Communication and Documentation
Any patient calls or interactions during telehealth visits must be documented. The nurse must communicate with the patient regarding their health or treatment plan in a way that is digestible allows them the opportunity to verbalize any questions or concerns.
In order to ensure effective communication during telehealth visits, there are a number of things a telehealth nurse can do, these include:
• At the beginning of the visit, provide a call back number in case the call is disrupted (allow the patient or family member to repeat the number back to establish the number is correct).
• Allow the patient or family member to verbalize feedback if the visit met expectations and was satisfactory.
• Ensure that the patient can hear and understand you clearly.
• If the visit is through a virtual conferencing platform, ensure that you are incorporating forms of non-verbal communication such as eye contact, body language, and appropriate facial expressions that would be used in an in-person visit.
• If necessary, explain the process of the telehealth visit and how it may differ from in-person.
• Remain confident, unbiased, and professional while upholding patient confidentiality (2).
Explain how a nurse conducting telehealth nursing interventions may have a stricter adherence to ethics than face-to-face encounters?
By what reasoning would the effect of software compliance and security standards jeporadize the ethical behavior of a telehealth nurse?
Nursing documentation via telehealth is no different than in-person clinical settings, and it must embody the nursing process, Code of Ethics for Nurses, and your facility’s documentation protocols (2).

Self Quiz
Ask yourself...
- While conducting a telehealth call, a patient is claiming that domestically violent behavior is being inflicted on their roommate and it is causing a stressful environment for them. What are the ethical obligations of the nurse, which must be documented if any?
ANA Principles for the Telehealth Nurse
In addition to the ANA Code of Ethics for Nurses and the AAACN Scope and Standards of Practice for Professional Telehealth Nursing, the ANA has 13 principles of connected health that the telehealth nurse must follow, these read (2):
- The use of connected health technologies does not alter the standards of professional practice when delivering healthcare, conducting research, or providing education. Developed by each profession, in this case nursing, these standards focus on the healthcare professional’s responsibility to provide lawful, evidenced-based and high-quality personalized care regardless of the method of delivery, grounded in the Nurses Code of Ethics.
- As connected health is a method of healthcare delivery, the healthcare provided is subject to the same healthcare laws and board oversight as the healthcare provided in-person. Healthcare professionals should understand, however, that due to the nature of connected health business models, certain interstate commerce, fraud and abuse another applicable state and federal laws not commonly encountered when delivering healthcare in-person may apply.
- Healthcare services delivered via connected health technologies should prioritize improving access to quality healthcare that is guided by best available evidence, accepted clinical standards, and best practices. These services must include deployment of appropriate technological modalities which meet the patient’s needs, are practical and easy to use, and align with specific patient location and care setting.
- Professional practice and healthcare delivery, regardless of venue and channel of delivery, mandates that healthcare professionals meet state specific regulatory and institutional requirements in accordance with scope of practice. Due to variations in practice rules and regulations across states and facilities, providers must practice respective of these variations whilst delivering care via connected health.
- Nursing and other healthcare professions are responsible for developing their own competencies to ensure the safe, effective and competent delivery of healthcare via connected health technologies using a patient-and family-centered team-based approach.
- Healthcare services delivered via connected health technologies should be congruent with in-person care and must adhere to the best available evidence that represents current and emerging interdisciplinary standards of care, while recognizing the limitations inherent in technology to ensure optimal patient-centered outcomes.
- When using connected health technologies, the integrity and therapeutic value of the patient-healthcare professional relationship should be established, maintained, and promoted via connected health.
- Safeguards must be taken with the transmission of electronic information and communication conducted using connected health technologies in all connected health practice settings. This practice upholds the highest level of ethical conduct in the secure management of patient health information, patient privacy and confidentiality and protection against unauthorized breach of information. This includes informing patients of the use of third-party technology providers, the risk of disruption in the integrity of those providers’ data management practices, and a commitment to protecting patients from such event.
- Documentation requirements for healthcare services delivered via the utilization of connected health technologies should be consistent with requirements applicable to all other patient encounters.
- Patients involved in a connected health encounter should be informed about the process, the inherent risks and benefits, and their rights and responsibilities, in compliance with applicable federal and state laws. Informed consent for connected health may not need to be independent from other informed consent for treatment although mechanisms for obtaining electronic consent should comply with applicable federal and state laws.
- The safety of patients and healthcare professionals must be ensured. Hardware and software compliance with safety and security standards, the appropriateness of a connected health approach to the situation and demonstrated patient and provider user competency are essential components of safe connected health practice.
- In order to inform connected health, and ensure the best outcomes, it is essential that the assessment, evaluation, and study of all aspects of connected health are ongoing and systematic. This research should include key stakeholders as primary informants and the resulting evidence utilized in the development and implementation of connected health guidelines and best practices.
- Policies governing the practices and reimbursement of healthcare should be continuously updated and modernized to allow for the integration, national adoption, and sustainability of connected health (2).
Although the telehealth nurse solely relies on the utilization of technology in order to interact with patients, this does not allow for altering of professional standards; providing quality-focused and patient-centered care is always required.
Additionally, it is unethical for the telehealth nurse to falsely indicate time spent in teaching and discharging. Time spent gathering discharge follow up and future appointments should not be counted as patient interaction, if conducted prior to making the call to complete the after-visit discharge summary. The nurse is responsible for knowing the laws in their state in accordance with their scope of practice for telehealth (2).

Self Quiz
Ask yourself...
- How are ethics in telehealth patient-centered?
- How are ethics a factor for nursing professionals in developing their own competencies in the delivery of safe and competent healthcare through telehealth?
Conclusion
No matter their specialty, field, or scope of practice, all nurses are accountable for their actions. Although the healthcare setting may vary, a telehealth nurse must be knowledgeable of their facility’s expectations during patient interactions as well as how to effectively deliver quality care virtually.
With the prevalence of the utilization of telehealth continuing to rise in the healthcare industry, it is vital for the telehealth nurse to ensure they are abiding by the ANA Code of Ethics for Nurses, consistently upholding professionalism, and overall, ensuring patient confidentiality.
One Hour Sepsis Bundle
Introduction
Sepsis is a significant problem today, so much so that the government released a 2023 report on the dire state of sepsis in the United States. Congress directed the Agency for Healthcare Research and Quality (AHRQ – the lead Federal agency charged with improving the safety and quality of healthcare for all Americans) to conduct research to help identify sepsis’ burden on the U.S. healthcare system related to morbidity, hospital readmission rates, and mortality. Congress stressed special focus on pediatrics, maternal care, nursing homes, rehabilitation, and pandemic-related changes. [1]. It is nothing new to healthcare workers that sepsis is a big deal and often at the top of the provider's differential diagnosis when clients begin to decompensate, and the cause is not yet clear.
The incidence of sepsis from 1979 – 2000 increased by 8.7%, from 82.7 to 240.4 per 100,000 clients [10]. The incidence of sepsis is rising as a result of the aging population, progressive increase in antimicrobial resistance, reliance on implanted devices, organ transplantation, and an increasing prevalence of clients with long-term immunosuppressive diseases who are at risk for severe infection and sepsis [10].
To understand the importance of the sepsis bundle, you must understand why there is an emphasis on treating sepsis as a medical emergency, similar to a heart attack or stroke.
Sepsis is a “syndrome characterized by life-threatening organ dysfunction caused by a dysregulated host response to infection” [King, para 3]. Septic shock is sepsis with “persistent hypotension despite fluid resuscitation” characterized by a high immune and inflammatory responses that result in vascular dilation and poor perfusion of tissues [King].
Sepsis Statistical Evidence
Sepsis affects over 49 million people worldwide. In the U.S., more than 1.7 million people are diagnosed with sepsis each year. While some recover, many do not; 350,000 adults die each year from the illness. In fact, sepsis is the number one cause of death in hospitals and delaying sepsis care significantly increases the risk of mortality – by 4 to 9% for every hour of treatment delay [16]. In 2021, 1 in 6 patients with sepsis died in the hospital and in cases involving septic shock, 1 in 3 hospital stays resulted in patient death [2].
Individuals aged 65 and over are especially at risk of dying from sepsis. In 2021, sepsis-related deaths among adults aged 65 and older was nearly 331 deaths per 100,000 people and death rates increased with age, most occurring among those age 85 and older [3]. Sepsis also causes many deaths in other age groups, particularly children. Sepsis is the largest killer of children worldwide (3.4 million each year) [16]. In the U.S., however, 6,800 children die from sepsis each year [17].
Sepsis is the number one cost of hospitalization in the U.S, costing the hospital system more than $53 billion each year [16]. Not only is sepsis associated with increased inpattient, outpattient, and readmission costs, it leads to long-term health outcomes (like cognitive and physical impairments) that can lead to loss of employment and increased caregiving needs, adding to its economic burden [2]. Additionally in 2021, about one-third of sepsis-related hospital stays ended with a transfer to a post-acute care health facility which is also costly [2].
While sepsis has a high mortality rate in hospitals, it originates in the community – hence, why most sepsis diagnoses occur in the emergency room [2][16]. In recent years, sepsis has been complicated by the COVID-19 pandemic. COVID-19 has changed the epidemiology of sepsis by increasing the risk of developing sepsis in the first place and by increasing the incidence of viral sepsis, which leads to complex diagnosis and treatment [2].
While these numbers are bleak, sepsis death rates in the U.S. have decreased from over 35% in the early 2000s to 15–20% recently [9].

Self Quiz
Ask yourself...
- How often do you see cases of viral or fungal sepsis?
- Does your facility have a “code sepsis” that’s called whenever a client presents with suspected sepsis?
- When was the last time you witnessed a client recover from a sepsis diagnosis? Was treatment started early?
- How quickly have you witnessed a client progress from sepsis to septic shock (if applicable)?
- Is suspected sepsis treated like an emergency in your facility?
Diagnostic Approach to Sepsis
Early phases of sepsis can be subtle even in the carefully monitored client, but if the subtle signs are missed, and the clinical signs of septic shock become glaringly apparent, you and your clinical team have already acted much too late.
Below is a table depicting the most common hemodynamic changes seen in sepsis [10].
| Parameter | Finding in Sepsis | Comments |
|
Heart Rate
|
≥ 100 BPM | HR is a major compensatory mechanism for low systemic vascular resistance |
| Mean Arterial Blood Pressure | <65 mmHg | Hallmark sign of septic shock if it remains low after adequate fluid resuscitation |
| Cardiac Index | >4 L/min/m2 | CI usually is elevated in early septic shock; may be depressed in late septic shock |
| Central Venous Pressure | 6-8 mmHg |
CVP is an indicator of volume status. If it is <6, the client is likely volume depleted. A normal or high CVP value can have different causes. |
| Systemic Vascular Resistance | <800 dynes/cm2 | SVR is often low in early septic shock; it may become elevated in later phases of septic shock |
|
Svo2 scvO2 |
< 70% <65% |
Low mixed venous o2 saturation or central venous o2 saturation indicates poor oxygenation to the tissues |
| Oxygen Consumption (V02) | >180L/min/m2 | Typically increased in early septic shock |

Defining Sepsis
The updated guidelines on sepsis use the Sequential (Sepsis Related) Organ Failure Assessment Score (SOFA) to define sepsis [19]. The SOFA score assesses the degree of organ dysfunction across numerous domains.
The score is based on the information obtained in each domain. The higher the score, the higher the mortality risk [19].A score of 2+ reflects an overall mortality of about 10% in the setting of suspected infection [7][10]. Organ systems include neurologic, blood, liver, kidney, and blood pressure/hemodynamics. The laboratory data included in the SOFA score focuses on coagulopathy, hepatic dysfunction, and/or renal dysfunction [10][19]. Other laboratory data (such as WBC) can aid in the diagnosis of infection but are not used to define sepsis or septic shock.
| Organ System Measurement | SOFA Score | ||||
| 0 | 1 | 2 | 3 | 4 | |
|
Respiration (PaO2/FiO2)
|
Normal | <400 | <300 | <200 with respiratory support | <100 with respiratory support |
|
Coagulation (platelets)
|
Normal | <150 | <100 | <50 | <20 |
|
Liver (bilirubin)
|
Normal |
1.2 – 1.9
|
2.0 – 5.9 | 6.0 – 11.9 | >12 |
|
Cardiovascular (hypotension) |
Normal | MAP >70* |
Dopamine 5 or less OR dobutamine (any dose)** |
Dopamine >5 OR Epinephrine 0.1 or less OR Norepinephrine 0.1 or less
|
Dopamine >15 OR Epinephrine >0.1 OR Norepinephrine >0.1 |
|
Central Nervous System (Glasgow Coma Scale)
|
Normal | 13 – 14 | 10 – 12 | 6 – 9 | <6 |
|
Renal (creatinine or urine output) |
Normal |
1.2 – 1.9
|
2.0 – 3.4
|
3.5 – 4. 9 OR <500 ml urine output per day) |
>5 OR <200 ml urine output per day)
|
*MAP= diastolic BP + 1/3 (systolic BP – diastolic BP)
**Adrenergic agents administered for at least 1 hour (doses given are in mcg/kg/min)
Table 1. Sequential Organ Failure Assessment (SOFA) Score Criteria [7][19]
A bedside tool called qSOFA (Quick SOFA) was developed to quickly identify adult clients with suspected infection who are likely to have poor outcomes [7][10][18].
The presence of any 2 of the following is equal to a positive qSOFA [7][18]:
- Respiratory rate = 22 breaths per minute or more
- Altered mental state (Glasgow Coma Score <15)
- Systolic BP = 100 mmHg or below
***The qSOFA is best used to identify early organ dysfunction in adults in nonhospital, emergency, or general hospital conditions, whereas the SOFA score is used more in the critical care setting [7][10][19].
The qSOFA tool can be used to quickly screen and identify clients who are at risk for deterioration. It is being used both on admission and as ongoing tool to track changes in client condition. Most recent sepsis guidelines recommend against using qSOFA alone for sepsis and septic shock screening as opposed to other tools like Systemic Inflammatory Response Syndrome (SIRS), National Early Warning Score (NEWS), or Modified Early Warning Score (MEWs) [4].
The chart below illustrates common laboratory findings seen in sepsis [10].
| Laboratory Study | Typical Findings | Comments |
| White Blood Cell Count | Leukocytosis or Leukopenia | Stress Response, increased margination of neutrophils in sepsis can cause transient neutrophenia; transient granulation |
| Platelet Count | Thrombocytopenia | Look for evidence of fragment hemolysis; thrombocytopenia may be accompanied by DIC |
| Coagulation Studies | Elevated Prothrombin Time (INR), aPTT, low fibinogen levels, elevated D-dimer; evidence of fibrinolysis | Coagulopathy very common but overt DIC is not common, (>15% of clients |
| Liver Enzymes | Elevated alkaline phosphatase, bilirubin, and transaminases; low albumin | Generally a late finding in clients with sepsis; indicates hemphatic ischemia and transamin typically >10 times upper limit |
| Plasma Lactate | >2.2mmol/L caused by hypermetabolism, anaerobic metabolism, inhibition of pyruvate dehydrogenase |
Poor prognostic feature if not improved rapidly by fluid resuscitation; diagnosed criterion for septic shock (with suspected infection). Can have other causes of elevation – high sensitivity with low specificity |
| C-Reactive Protein | Elevates as an acute phase reactant from hepatic synthesis | Acute-phase reactant, sensitive, but not specific for sepsis |
| Glucose | Hyperglycemia or hypoglycemia | Acute stress response can lead to hyperglycemia, inhibition of gluconeogen can lead to hypoglycemia |
| Arterial Blood Gas (ABG) | Respiratory alkalosis (early); metabolic acidosis (late) | Reduced arterial 02 content and mixed venous 02 saturation |

Self Quiz
Ask yourself...
- Think about your clinical experiences. Have you seen clients with sepsis who presented with atypical signs (hypothermia, respiratory alkalosis, etc.)?
- Do you think this delayed their diagnosis and care?
- How will you use this information to better detect clients who may have sepsis?
- Over the years, many tools have been identified in hopes of detecting sepsis early. How does the sensitivity and specificity of each of these tools affect their usability?
- Which sepsis identification tool does your facility use? What are some components of the tool?
A Word on Septic Shock
Septic shock occurs in up to 15% of clients with sepsis [10]. The management of the client in septic shock hinges on prompt recognition of the client’s deteriorating condition and expeditious administration of antibiotic therapy coupled with infectious source control. Simultaneously, the failing organ systems must be supported through measures such as, fluid resuscitation, vasopressors, blood transfusions, respiratory support, and inotropic agents. You can find more details regarding the initial management of sepsis in the Surviving Sepsis Campaign guidelines.
Septic Shock is defined as hypotension requiring intravenous vasopressors to maintain a MAP ≥65mmHg and serum lactate of >2mmol/L [10].
Early Septic Shock:
- Hemodynamics: High Cardiac Output (CO) and Low Systemic Vascular Resistance (SVR)
- Extreme vasodilation leading to an increase in cardiac output. This is the body’s attempt to preserve peripheral vascular perfusion.
Late Septic Shock:
- As shock progresses, myocardial performance diminishes and circulating blood volume is continually lost to the interstitial space, leading to a profound hypotensive state.
- Sepsis-induced myocardial dysfunction may ensure. This results in a potentially reversible heart failure state due to myocardial depression.

What Is a Sepsis Bundle and Why Are They Used?
The Sepsis Bundle or ‘Severe Sepsis and Septic Shock Management Bundle’ (SEP-1 Measure) is a set of priorities and interventions for hospitals to assist in identifying sepsis early, initiating treatment right away, and preventing septic shock and death [14][15]. The sepsis bundle is different from Sepsis Guidelines. The guidelines offer general recommendations/suggestions regarding sepsis screening and education, initial resuscitation, ICU admission, ventilation, and more [4]. The bundle, however, is a concise version of the clinical recommendations of the guidelines with focus on what to do once sepsis is suspected from obtaining specific labs to administering certain medications [King][14].
The sepsis bundles consist of various components of sepsis care [4][King][11]:
- Early identification
- Fluid resuscitation
- Timely and appropriate antibiotic administration
- Blood cultures
- Serum lactate levels
The sepsis bundle elements were designed in such a way to be updated as new evidence emerged [15].
Evidence has shown an association between compliance with bundles and improved survival in clients with sepsis and septic shock. In a multi-center, retrospective, observational study of adult clients with a hospital discharge diagnosis of severe sepsis or septic shock, overall mortality was lower in those who received bundle-adherent care (17.9%) when compared to those who did not (20.4%) [11]. Interestingly, when the clients in the study were divided into subgroups by the suspected source of infection, there was only a statistically significant mortality benefit to bundle-adherent sepsis care in clients diagnosed with pneumonia [11].
While some feel that the bundle is a helpful guide, there are some critics. The bundle’s main elements are early recognition and immediate administration of broad-spectrum antimicrobials. However, some feel that this contributes to antimicrobial resistance as there’s no time permitted for determining microbial sensitivity which ideally would guide clinicians in administering the most effective antimicrobial [15]. Experts are attempting to find ways to treat sepsis early while also preventing antimicrobial resistance. For example, encouraging clinicians to continue reevaluating the client, searching for alternative diagnoses, and discontinuing broad-spectrum antimicrobials once another diagnosis is strongly suspected or confirmed [4]. Other critics of the bundle feel that the push to perform interventions within a specific timeframe “promotes harmful diagnostic tests and treatments” [14]. The bundle, however, has been proven effective in lowering mortality in hospitalized clients.

Self Quiz
Ask yourself...
- In your practice, have you found sepsis bundles to be effective in preventing septic shock in your clients?client
- What might be a barrier to the healthcare team’s adherence to sepsis bundles?
- Does your facility have a sepsis champion? If so, what is their primary role?
- Can you think of a strategy to prevent antimicrobial resistance when adhering to sepsis bundles?
- How comfortable are you with the idea of administering broad-spectrum antibiotics prior to culture sensitivity results? If not, what do you suggest?
Sepsis Guidelines Updates
In the last section, we discussed the difference between Sepsis Guidelines and the Sepsis Bundle. The following are most recent Sepsis Guideline updates made in 2021. Some recommendations are new and others are changed from the 2016 version [4].
SEPSIS GUIDELINES
|
|
2021 Updated Recommendations/Suggestions |
Prior Recommendations From 2016 |
|
Administer 30 ml/kg of IV crystalloid fluid (lactated ringers) within the first 3 hours of resuscitation for both sepsis-induced hypoperfusion and septic shock.
|
Administer 30 ml/kg of IV crystalloid fluid within the first 3 hours of resuscitation for sepsis-induced hypoperfusion. |
|
Use balanced crystalloids instead of normal saline for fluid resuscitation in adults with sepsis or septic shock.
|
Use balanced crystalloids or normal saline for fluid resuscitation in adults with sepsis or septic shock. |
| Defer use of gelatin for fluid resuscitation in adults with sepsis or septic shock. |
Use balanced crystalloids over gelatin for fluid resuscitation in adults with sepsis or septic shock.
|
|
Use capillary refill to guide resuscitation as an adjunct to other measures of perfusion (for adults with septic shock).
|
|
|
Administer antimicrobials immediately, ideally within 1 hour of recognition for adults with (a) possible septic shock or (b) high likelihood for sepsis.
|
Administer IV antimicrobials as soon as possible after recognition and within 1 hour of both (a) septic shock and (b) sepsis without shock. |
|
Start a time-limited course of rapid investigation for adults with possible sepsis without shock and if concern for infection persists, administer antimicrobials within 3 hours from the time when sepsis was first recognized.
|
Administer IV antimicrobials as soon as possible after recognition and within 1 hour for both (a) septic shock and (b) sepsis without shock. |
|
Defer antimicrobials while continuing to closely monitor the client (for adults with a low likelihood of infection and without shock).
|
Administer IV antimicrobials as soon as possible after recognition and within 1 hour for both (a) septic shock and (b) sepsis without shock. |
|
Use empiric antimicrobials with MRSA coverage over using antimicrobials without MRSA coverage for adults with sepsis or septic shock at a high risk of MRSA.
|
Use empiric broad-spectrum therapy with one or more antimicrobials for clients presenting with sepsis or septic shock to cover all likely pathogens (including bacterial and potentially fungal or viral coverage) |
|
Defer empiric antimicrobials with MRSA coverage for adults with sepsis or septic shock at a low risk of MRSA.
|
|
|
Use empiric antifungal therapy over no antifungal therapy for adults with sepsis or septic shock at a high risk of fungal infection.
|
|
|
Defer empiric antifungal therapy for adults with sepsis or septic shock at a low risk of fungal infection.
|
|
|
Use levosimendan in adults with septic shock and cardiac dysfunction with persistent hypoperfusion despite adequate fluid volume and arterial blood pressure.
|
|
|
Start vasopressors peripherally to restore MAP rather than delaying initiation until a central venous access is secured.
|
|
|
Use high-flow nasal oxygen over non-invasive ventilation for adults with sepsis-induced hypoxemic respiratory failure.
|
|
| Use IV corticosteroids in adults with septic shock who have an ongoing requirement for vasopressor therapy. |
Defer using IV hydrocortisone to treat clients with septic shock if adequate fluid resuscitation and vasopressor therapy are able to restore hemodynamic stability. If this is not achievable, administer IV hydrocortisone 200 mg per day.
|
|
Defer using polymyxin B hemoperfusion in adults with sepsis or septic shock.
|
“We make no recommendations for the use of blood purification techniques.” |
|
Defer using IV vitamin C in adults with sepsis or septic shock.
|
|
Table 2. Current 2021 Updates/Changes to the 2016 Sepsis Guidelines [4]

Self Quiz
Ask yourself...
- Why do you think normal saline is no longer recommended for fluid resuscitation in sepsis?
- Are antimicrobials typically administered within 1 hour and IV fluids within 3 hours for the treatment of sepsis at your facility?
- What are some potential delays to IV fluid and antimicrobial administration in sepsis?
- How might IV corticosteroids be helpful to clients in septic shock?
- How might you determine a client is at a high risk of viral or fungal sepsis, therefore warranting early administration of antimicrobials?
One Hour Sepsis Bundle Components and Strategies to Expedite Care
The most critical change in the Surviving Sepsis Campaign bundles is that the previous 3-hour and 6-hour sepsis bundles are now combined into a single "hour-1 bundle" with the intention of beginning resuscitation and management immediately upon presentation [4]. While more than one hour may be needed for client resuscitation to be completed, the initiation should begin immediately upon suspicion that the client may be presenting with sepsis.
Measure Lactate Level
Serum lactate level (or lactic acid level) determines the degree of tissue perfusion in the body [5]. In the absence of oxygen - anaerobic metabolism ensues, and lactate levels rise. It often represents the degree of tissue hypoxia present, and increased levels are associated with worse outcomes [5]. Lactate levels alone are not enough to finalize a diagnosis of sepsis but a high lactate level significantly increases the likelihood [4]. Lactate levels from 2 to 4 mmol/L are mild, and levels above 4 are severe and indicate sepsis-induced hypoperfusion with a high mortality rate [5]. If the initial lactate is >2mmol/L but <4, it should be re-measured in 3 hours and used to guide resuscitation with the goal of achieving a lactic acid <2mmol/L [King].
Hospitals should have a threshold of > 2mmol/L for a critical lactic acid value, which will prompt any abnormal value to be communicated to the provider. Consider having non-nursing personnel collect the lactate level so that the nursing staff is free to focus on other tasks. The re-collection of lactates >2 can be automated by many electronic order entry systems and will help reduce fallouts due to re-collection. Point of care lactate is now readily available which can be valuable.
All critical lactate values should be communicated to both the nurse and the provider. Traditionally this has been done by the lab through a call to the nurse who then notifies the provider. Depending on your facility’s protocol, the lab may call both the provider and the nurse directly to reduce the potential for error.
Obtain Blood Cultures Prior to Antimicrobial Therapy
Blood cultures should be obtained prior to beginning antimicrobial therapy. Drawing cultures after the first antimicrobial dose has already been started can lead to lower detection of pathogens in the blood by up to 50% [13]. By obtaining cultures before administering antimicrobials, there is a better opportunity to identify pathogens and therefore improve client outcomes. Appropriate cultures include at least two sets of both aerobic and anaerobic cultures from two separate venipuncture sites. If the client has a central venous catheter, a culture should be drawn from each lumen of the catheter as well as a peripheral site [King]. Administration of antibiotic therapy should not be delayed past 1 hour in an effort to obtain cultures, particularly for clients who are hemodynamically unstable/critically ill [4][King] .
Administration of Empiric Antimicrobial Therapy
Empiric broad-spectrum antibiotic therapy with one or more IV antimicrobials to cover all likely pathogens should be started immediately [4]. Once a pathogen is identified, and sensitivities are established, the empiric antimicrobials should be narrowed or discontinued if the client is found not to have an active infection [4].
Since time is of the essence when treating a client presenting with sepsis, the empiric antimicrobials should be kept in the on-unit medication storage for ease of access. Nurses should have immediate access to these medications.
All orders for sepsis antimicrobials should be ordered as STAT (for the first dose). The providers should be trained to enter antimicrobials orders directly after examining clients, if possible. Delays in ordering obviously lead to a delay in medication delivery. The goal should be to have a culture that recognizes and treats sepsis as a medical emergency, just as a cardiac arrest, heart attack, or stroke.
Administer IV Fluids
Early effective fluid resuscitation is critical for the stabilization of sepsis-induced tissue hypoperfusion and septic shock (3). Initial fluid resuscitation should begin immediately upon recognizing that a client is presenting with sepsis and/or hypotension and elevated lactate [4][King]. Fluid resuscitation should be completed within 3 hours of recognition [4]. Current guidelines recommend that intravenous fluid resuscitation consists of 30 mL/kg bodyweight of crystalloid fluids (lactated ringers) [4][King]. A relative contraindication to lactated ringers is profound hyperkalemia. Fluids should be administered even in clients at a high risk for fluid overload (like those with heart or kidney failure) but the client should be monitored more frequently in this case [King].
Providers should communicate the need for IV fluids verbally to the nursing staff and place orders into the order entry system directly after examining clients. Rather than waiting for central line placement, the client should have a peripheral IV placed [4]. It would be beneficial to place 2-3 large-bore IVs to facilitate the administration of IV fluids and IV antimicrobials without sacrificing the timing of one or the other. Oftentimes, placing a central line takes anywhere from 15-30 minutes and will delay overall client care during the first minutes. If additional venous access is needed, it is advisable to wait until the client is stabilized so long as adequate, reliable IV access is obtained.
Start Vasopressors
A critical part of sepsis resuscitation is restoring perfusion to the vital organs. If a client's blood pressure does not return to normal after the initial fluid resuscitation, then vasopressors should be initiated to maintain a MAP of at least 65 mmHg [King]. If a client has profound hypotension and the decision is made by the medical team to initiate vasopressor therapy, there is no need to wait to initiate until central access is obtained. Vasopressors can be infused through a large-bore peripheral IV (must be in or proximal to the antecubital fossa), safely for less than 24 hours [King][12].
Within the ER and ICU, there should be easy access to vasopressors, specifically norepinephrine, vasopressin, and epinephrine, in the event that a client needs a vasopressor started. Additionally, institutions may have standing protocols for nurses to initiate a vasopressor if a client is consistently hypotensive despite adequate fluid resuscitation. This will save vital time by allowing the nurse to use their clinical judgment and restore vital organ perfusion quickly and efficiently while awaiting provider guidance.


Self Quiz
Ask yourself...
- What are some barriers you anticipate facing if you attempted to adopt these strategies?
- Your client has suspected sepsis and the provider orders IV fluid resuscitation. Your client has a history of heart failure. How do you address this order?
- Your client with suspected sepsis has a central line. How should you draw blood cultures?
- Your client is suspected of having sepsis and blood cultures have already been drawn. Should you start the antibiotic or IV fluids first?
- Your client is consistently hypotensive despite fluid resuscitation attempts. What step do you take next?
Code Sepsis
Despite sepsis bundle care and the diligent work of healthcare providers and beside nurses alike, many hospitals have identified an opportunity to save lives and reduce suffering through early sepsis detection, compliance with current standards of care, and determining the appropriate level of care.
The Emergency Department Code Sepsis Project focuses on timely implementation of the sepsis bundle to reduce mortality and costs and to ensure appropriate level of care placement. By activating a 'code sepsis,' it allows not only doctors and nurses to be aware of the urgency at hand but also pharmacists, respiratory therapists, lab technicians, nursing support staff, and unit secretaries.
In some facilities, a 'code sepsis' is worked into the rapid response team's framework. For example, if a nurse screens a client for SIRS criteria and the client meets the criteria, a page can be sent out from the client's current floor. This will mobilize the appropriate resources to facilitate swift and effective resuscitation.
The multidisciplinary nature of the code sepsis project creates a strong sense of teamwork centered around applying best evidence-based practice, mobilizing resources, avoiding procedure variability, and improving client care and safety [6].
Hospitals that are struggling to meet sepsis measures should consider the addition of a "code sepsis" or "sepsis response team".
Each organization should strive for a culture that treats sepsis with the same urgency as any other medical emergency. Much of the delay in treatment with sepsis is due to a lack of standardized processes. Hospitals should work to develop sepsis protocols and sepsis response teams to increase compliance with bundles and decrease mortality.

Self Quiz
Ask yourself...
- How could a code sepsis benefit your clients with sepsis?
- Do you think that a code sepsis would expedite care in your facility?
- Which interdisciplinary team members might come to the bedside when a code sepsis is called?
- You arrive on shift, review your client’s medical record, and perform an assessment. You realize that your client meets SIRS criteria. What is the first thing you should do?
- What specific steps can hospital leaders take to decrease sepsis-related mortality rates in their facilities?
Conclusion
With sepsis being the number one killer of hospitalized clients in the U.S. and the number one cause of pediatric deaths, knowledge of the entire healthcare team, with an emphasis on nurses is imperative to decrease this statistic and provide expedited care to our clients to save lives. As a nurse, having the knowledge to recognize early symptoms of sepsis and act accordingly to prevent the progression, it will allow you increase care and improve client morbidity and mortality.

Renal Failure Stages, Treatment and Outcomes
Introduction
According to the Centers for Disease Control and Prevention (CDC), about 37 million adults in the United States, or 14% of the adult population, have chronic kidney disease (CKD) [1]. Estimates are that more than one in seven U.S. adults, equating to about 35.5 million people, have CKD, with 90% unaware of the condition [1][3].
Furthermore, about one in three adults with severe CKD are unaware of their diagnosis. The prevalence of CKD varies by age, sex, and race/ethnicity; CKD is more common in individuals aged 65 years or older (34%) compared to those aged 45–64 years (12%) and 18–44 years (6%) [1]. Females are more affected by CKD (14%) than males (12%) [1]. Among racial and ethnic groups, non-Hispanic Black adults have a higher prevalence (20%) compared to non-Hispanic Asian adults (14%) and non-Hispanic White adults (12%), with Hispanic adults also showing a prevalence rate of 14% [1].
Despite these statistics, a sizable portion of those with reduced kidney function, including 40% of those with a notable decrease and one-third of those with severe CKD, remain undiagnosed [2]. CKD occurs when damage to kidneys occurs over time, impairing their ability to perform these critical functions [3]. Moreover, CKD accelerates the risk of additional health complications, including heart disease and stroke [4]. Often, the progression of CKD is slow, with few symptoms in the initial stages, leading to its classification into five stages to facilitate treatment planning [5].
The kidneys play an integral role in preserving health, crucial for activating hormones, stabilizing blood's key molecules, and removing toxins, ranking them just behind the liver in toxin elimination importance [6][8]. The kidney contains millions of nephrons with filtering glomeruli that send fluid through the ureters, bladder, and urethra for excretion, or through the renal vein for return to the body [12]. Key functions include filtering natural waste and surplus water, supporting red blood cell production, balancing essential minerals, regulating blood pressure, and promoting bone health [7][8].
With 20% to 25% of the heart's output flowing through them, the kidneys filter blood up to 60 times daily [9]. They eliminate a range of metabolic byproducts like ammonia, urea, uric acid, and creatinine, along with hemoglobin breakdown products, hormone byproducts, liver-processed water-soluble toxins, and excrete industrial substances such as heavy metals and synthetic chemicals [7][8]. They also remove excess intake of nutrients or dietary elements, including salt, vitamin C, and B vitamins [7][8].
Chronic kidney disease (CKD) has become a significant cause of mortality and morbidity in the 21st century, with its prevalence exacerbated by increasing rates of risk factors including obesity and diabetes mellitus. In 2017, CKD affected 843.6 million individuals across the globe [2]. While mortality rates for those with end-stage kidney disease (ESKD) have seen a decline, studies from the Global Burden of Disease (GBD) indicate that CKD ranks as a leading cause of death worldwide [10]. As such, early detection, monitoring, and treatment of CKD, alongside the implementation of preventive and therapeutic strategies on a global scale, are essential.


Self Quiz
Ask yourself...
- How might public awareness and early screening programs be optimized to address the disparities in CKD prevalence among different age groups, sexes, and racial/ethnic groups?
- How does the gradual decline in eGFR values from Stage 1 through Stage 5 of CKD reflect the underlying progression of kidney damage?
- Considering that albumin should remain in the blood, what does the presence of albumin in urine indicate about the integrity of the kidney's filtration system?
- Given that eGFR values define the stages of CKD, how should clinicians balance the benefits and potential harms of early diagnosis and intervention?
Acute Versus Chronic Renal Failure
Kidney damage can manifest as either acute or chronic conditions. A rapid onset characterizes acute kidney injury (AKI), where the kidneys lose the ability to function, often as a response to physical injury, toxic substance exposure, infections, or a temporary reduction in blood flow [19]. In cases of AKI, there is an expectation for the kidneys to recover normal function after addressing the immediate cause healing has occurred [20].
Chronic kidney disease (CKD) develops over a period and is irreversible [20]. It falls under the broader category of acute kidney diseases and disorders (AKD), encompassing conditions where there is a gradual reduction in kidney performance or sustained kidney issues [20]. This often results in the irreversible destruction of kidney cells and nephrons progressing to chronic kidney disease (CKD) [20].
Lifestyle factors play a significant role in the onset of CKD, with uncontrolled diabetes and high blood pressure being the leading causes [21]. Other factors contributing to CKD include long-term use of specific drugs (such as NSAIDs, heroin, and certain antibiotics), recurring infections (for example, urinary tract infections and glomerulonephritis), inherited conditions like polycystic kidney disease, and the presence of kidney stones [22]. In some instances, an event causing AKI may result in permanent kidney damage if the organs do not recover within 90 days, at which point the condition receives classification as chronic kidney disease (CKD) [23].

Self Quiz
Ask yourself...
- Acute kidney injury (AKI) can transition into chronic kidney disease (CKD) if the kidneys do not recover within 90 days. What does this suggest about the importance of early intervention and monitoring?
- Given the significant role of lifestyle factors, what preventive measures can individuals take to minimize their risk of developing CKD?
- Reflecting on the contribution of long-term medication use, recurring infections, inherited conditions, and the presence of kidney stones to CKD, how might public health strategies address these issues and their impact on kidney health?
Types of Dialysis
Dialysis serves as a substitute for kidney functions, with hemodialysis and peritoneal dialysis being the primary methods. These techniques employ a semi-permeable membrane to filter out waste, toxins, and residual fluids from the body [24][25].
These membranes permit the passage of small molecules and fluids through their pores, restricting larger molecules [24][25]. During dialysis, substances including urea and selected electrolytes (sodium, potassium, magnesium, calcium, and phosphorus), which are present in excessive amounts in the blood, pass through this membrane [25][26].
Meanwhile, blood cells, due to their larger size, remain in the bloodstream. Unlike the constant operation of healthy kidneys, dialysis can only mimic a portion of renal function, regardless of the frequency or efficiency of the treatments [25].
Hemodialysis
Hemodialysis remains the primary form of renal replacement therapy, leveraging a dialysis machine equipped with a pump designed to emulate the cardiac function of circulating blood throughout the organism [28]. To facilitate access to the vascular system implanted accesses are employed to bridge an artery and a vein.
The primary access types include arteriovenous fistulas (AVFs), arteriovenous grafts (AVGs), and central venous catheters (CVCs), with AVFs being the most favored due to their employment of the patient's native arterial and venous system [29]. AVGs utilize synthetic materials to form the arterial-venous connection, representing permanent solutions [30]. CVCs are less desirable due to elevated risks of infection and thrombosis and positioning the catheter's tip within the heart's right atrium. CVCs are viewed as interim solutions pending the establishment of permanent access [31]. For patients lacking suitable vasculature for permanent access, CVCs may represent a final alternative.
The operational mechanism of AVFs and AVGs necessitates the insertion of two large-bore needles into the access point to facilitate blood flow into the dialysis circuit, which houses a dialyzer (artificial kidney) [32]. Myriad semi-permeable microtubules line the interior of the dialyzer that permits blood passage in one direction and a specially formulated dialysate—comprising ultrapure water produced via reverse osmosis (RO), sodium bicarbonate, and an acid solution enriched with electrolytes like sodium, potassium, calcium, and magnesium—in the reverse [33].
This setup generates a pressure differential, enabling diffusion and osmosis within the dialyzer to aid the body in achieving homeostasis by expelling waste, toxins, and superfluous fluid [33]. Post-filtration, the effluent discharges into a drain, while the purified blood is reintroduced into the patient's circulation through the second needle.
Peritoneal Dialysis
Peritoneal dialysis involves the surgical insertion of a catheter into the patient's abdomen, facilitating the inflow and outflow of fluid within the peritoneal space [34]. The peritoneum, a semi-permeable membrane, acts as the filtration barrier in this process [34]. During treatment, the introduction of a dialysis solution rich in dextrose occurs into the peritoneal cavity, drawing waste, toxins, and excess fluid from the bloodstream across the peritoneum [34].
After a designated period known as the dwell time, this fluid, now containing the filtered waste products (referred to as the effluent), drains away through the catheter [34]. The procedure, or exchange, repeats several times based on the individual's remaining kidney function and laboratory values, which are indicative of their stage of renal failure. Unlike hemodialysis, this method does not require vascular access, thereby eliminating the need for needles.

Self Quiz
Ask yourself...
- How does the semi-permeable nature of the dialysis membrane influence the efficiency of toxin and waste removal from the bloodstream?
- Given the different access methods for hemodialysis, what are the comparative advantages and disadvantages of each in terms of infection risk, clotting, and long-term vascular health?
- Considering dialysis can mimic the functions of healthy kidneys, what are the potential physiological or metabolic imbalances that patients might experience?
- In peritoneal dialysis, how does the concentration of dextrose in the dialysis solution affect the process of osmosis and the overall efficiency of fluid and toxin removal from the body?
Treatment Goals
The primary objectives of dialysis treatments are to compensate for the loss of renal function and restore equilibrium within the body [32]. Achieving and maintaining fluid balance is vital, making precise patient weight measurements critical. Estimated dry weight serves as a reference for regulating fluid extraction during outpatient hemodialysis treatments [35]. Nephrologists determine an estimated dry weight (EDW) for each patient, representing their optimal weight minus any excess fluid [35].
Dialysis machines receive precise calibration to extract fluid to align the patient's weight with their EDW by the treatment's conclusion. Inaccuracies in fluid removal or its rate can result in complications like hypervolemia, characterized by symptoms such as shortness of breath, pneumonia, edema, congestive heart failure, pulmonary edema, and hypertension. Hypovolemia is another complication manifesting as cardiac issues, hypotension, nausea, vomiting, cramps, and dizziness [28]. Fluid imbalance and infection are leading causes of hospitalization among patients with end-stage renal disease (ESRD) [36].
Another crucial aim of dialysis is waste elimination and electrolyte regulation, often measured through clearance or adequacy metrics. Several factors influence clearance, including the semi-permeable membrane's size, treatment duration and frequency, membrane exposure duration, access functionality, dialysate concentration, and the effectiveness of anticoagulants or thrombolytics [28]. A more concentrated dialysate enhances clearance, but concentrated solutions may harm the peritoneal membrane or cause red blood cell crenation in hemodialysis [28].
To simulate various kidney functions including hormone regulation and infection prevention, patients receive medications during dialysis sessions. These include erythropoietin-stimulating agents (ESAs) and iron to promote healthy red blood cell production, vitamin D for calcium absorption, and protein supplements to increase albumin levels, aiding in fluid shift to the vascular space for elimination [37].
In addition, heparin prevents blood clotting, thrombolytics address catheter clots, and IV antibiotics combat infections [38]. Vaccinations against Hepatitis B, influenza, pneumonia, and Covid-19 protected against infectious diseases [38]. Phosphorus binders enhance calcium absorption by limiting phosphorus intake during meals [38].

Self Quiz
Ask yourself...
- How does the determination of a patient's estimated dry weight (EDW) by a nephrologist impact the effectiveness and safety of fluid removal during hemodialysis?
- How do variables such as semi-permeable membrane size and dialysate concentration interact to optimize waste and electrolyte removal without compromising the patient's health?
- How do the medications administered during dialysis sessions, such as erythropoietin-stimulating agents, vitamin D, and phosphorus binders, contribute to mimicking the kidney's hormonal functions and managing the complications associated with end-stage renal disease (ESRD)?
Treatment Goals
Dialysis Settings
Both hemodialysis and peritoneal dialysis offer administration flexibility in various settings, including hospitals, outpatient facilities, or the comfort of a patient's home. Hemodialysis requires electricity for the dialysis and reverse osmosis (RO) machines, as well as a water source for producing RO water [39].
Depending on the specific equipment used, patients have the mobility to travel with their dialysis supplies and perform their treatments outside of dialysis centers. In contrast, peritoneal dialysis does not necessitate electricity or a clinic location secondary to a manual option that operates on gravity alone [39]. Regardless of the dialysis method selected or the location of treatment, maintaining strict infection control practices is critical.
Dialysis supplies are sterile upon packaging and must remain uncontaminated upon opening to prevent the introduction of microbes into the bloodstream or peritoneal cavity [40]. Between 2017 and 2020, adults undergoing dialysis were at a 100-fold increased risk of experiencing a staphylococcus bloodstream infection compared to adults who were not on dialysis [40]. Employing aseptic techniques is essential to reduce the risk of infection and/or cross-contamination.
Incenter Hemodialysis
In the United States, the outpatient hemodialysis clinic is the most prevalent venue for dialysis, with thousands of such facilities nationwide [41]. Patient care technicians (PCTs) and licensed practical nurses (LPNs), supervised by registered nurses, deliver direct patient care in these clinics, managed by a nurse manager or facility administrator alongside a medical director.
The staff complement in these clinics may also include attending physicians, nurse practitioners, physician assistants, social workers, dietitians, biomedical technicians, and administrative staff. The size of a clinic is determined by the number of licensed and operational patient stations, each equipped with a specialized reclining chair or bed and a dialysis machine for administering treatments. A hemodialysis session lasts between 3.5 and 4.5 hours, during which patients receive monitoring from the care team [28].
Following treatment, they are re-evaluated by an RN, weighed, and then sent home. Treatments occur three times a week, either on a Monday, Wednesday, Friday, or Tuesday, Thursday, Saturday basis, although some may require more frequent sessions due to fluid management needs, depending on their stage of renal failure.
Many patients on dialysis prefer the outpatient setting for the social interaction it fosters and the reassurance of professional oversight [41]. However, this option imposes the most stringent dietary and fluid restrictions on patients due to the thrice-weekly treatment regimen and offers less flexibility in scheduling due to the set operating hours and staffing considerations.
Home Hemodialysis
Hemodialysis can occur at home, including during sleep hours. Patients and their care partners receive training on how to insert needles and manage their treatments independently.
Similar to facilities, patients at home can use a recliner for comfort during dialysis. Supplies arrive at the patient’s home either weekly or biweekly, depending on the available storage space. This system of supply delivery, which can reach almost any location, ensures patients can travel with ease while continuing their dialysis regimen uninterrupted.

Self Quiz
Ask yourself...
- How do the differences in the operational and environmental requirements of hemodialysis and peritoneal dialysis affect the strategies for infection control?
- How does the structured nature of outpatient hemodialysis clinics impact the patient's quality of life and treatment adherence when compared to the more flexible options available with peritoneal dialysis?
- How does the training process for patients and their care partners in home hemodialysis affect the safety and effectiveness of home treatments compared to those conducted in clinical settings?
- What are the potential challenges and benefits of managing dialysis at home considering supply delivery and the ability of patients to travel?
Kidney Transplants
In the U.S., 13% of patients on dialysis, about 100,000 individuals, are on the waitlist for a kidney transplant [43][44]. A kidney transplant involves providing a patient with end-stage renal disease (ESRD), at Stage 5 of renal failure, a kidney from either a living or deceased donor. This procedure has the potential to restore the patient's quality of life to pre-failure conditions.
The existing, non-functional kidneys remain unless removal is necessary. Kidneys from living donors are often more successful and have a longer functional lifespan than those from deceased donors [45].
Candidates for transplantation undergo thorough medical and psychosocial evaluations by the transplant center to minimize the risk of transplant failure and to ensure the recipient is prepared for post-surgery care. Being on the active transplant list requires patients to ensure they are contactable by the transplant center and can promptly reach the center when notified of a potential kidney match.
Addressing any medical issues and risk factors, such as the need for weight loss or smoking cessation, is crucial before listing for a transplant [46]. Regular lab monitoring, conducted by either the dialysis clinic or the transplant center, is essential to remain on the transplant list. Candidates must not have cancer or other severe conditions that could compromise the transplant's success. Monitoring adherence to post treatment protocols can identify those at a higher risk of post-transplant issues [47].
Financial considerations can pose barriers for some candidates. Since 1972, Medicare has provided coverage for ESRD patients with sufficient contributions to the system, offering benefits irrespective of age [48]. Medicare covers about 80% of transplant and associated costs, but offers limited coverage post-transplant, affecting the patient's eligibility for benefits if the new kidney functions well until they reach the standard Medicare eligibility age without ESRD [49].
Medicare stops covering patients who received kidney transplants 36 months post-transplant if the patient needs ongoing dialysis or another kidney transplant. Yet, the Comprehensive Immunosuppressive Drug Coverage for Kidney Transplant Patients Act of 2020 eliminated the three-year limit on coverage for immunosuppressive drugs [49].
Palliative Care
A diagnosis of Stage 5 renal failure does not signify a terminal phase unless the patient opts not to pursue further intervention. Those who choose against starting or continuing dialysis or seeking a transplant can receive palliative care to ensure comfort during their final days.
Pre-arranging treatment preferences, appointing a health care proxy, and establishing power of attorney contribute to a more managed transition. Patients who undergo dialysis may receive palliative care to alleviate common symptoms such as fatigue, itching, diarrhea, and restless leg syndrome, enhancing their quality of life during treatment [50].

Self Quiz
Ask yourself...
- How do the medical and psychosocial evaluations required for kidney transplant candidacy impact the overall readiness and eligibility of patients on the active transplant list?
- How does the integration of palliative care with ongoing dialysis treatment for patients with Renal Failure Stage 5 affect their management of symptoms and overall quality of life?
- What role do pre-arranged treatment preferences, health care proxies, and powers of attorney play in the decision-making process for patients at Renal Failure Stage 5?
Home Hemodialysis
Hemodialysis can also be performed at home, even while the patient sleeps. The patient and care partner are trained to cannulate (insert needles) and facilitate the treatments. In the U.S., patients usually use either a NxStage machine or a Fresenius 2008K at home machine (often referred to as a Baby K because it is slightly smaller than the larger K machines utilized in the outpatient clinics and hospitals).
Both machines have the same function and operate the same way. The patients receive a recliner for their home just like the incenter patients use. There are weekly or biweekly shipments of supplies, depending on how much storage space the patient has available. The supplies can be delivered virtually anywhere, which allows the patients to be able to travel easily without skipping their dialysis treatments.

Self Quiz
Ask yourself...
- How does the choice between outpatient hemodialysis, home hemodialysis, peritoneal dialysis, and kidney transplantation reflect the individual health goals, lifestyle, and treatment preferences of patients with chronic kidney disease?
- What factors should patients and their healthcare teams consider when determining if home hemodialysis is most suitable for their situation?
- How should patients weigh the potential benefits against the long-term commitments and risks associated with transplant surgery and post-operative care?
Future State of Patients with End Stage Renal Disease
One in three adults faces a risk of developing kidney disease [52]. There is a compelling need to enhance the number of transplants and to establish home-based therapies as the primary treatment approach for patients with end-stage renal disease (ESRD). The current infrastructure will not suffice to accommodate the increasing number of patients requiring in-clinic dialysis treatments.
On July 10, 2019, the announcement of the Advancing American Kidney Health initiative by President Trump sets forth three main goals and seven specific objectives [53].
- Aim for a 25% reduction in new ESRD cases within a decade.
- Elevate the adoption of home-based therapies and transplants to 80% by the year 2025.
- Increase the availability of kidneys for transplantation twofold by 2030.
Efforts to combat kidney disease are expanding through research. The National Kidney Foundation is supporting this cause with grants and clinical trials aimed at discovering a cure or more effective treatments for chronic kidney disease (CKD). Two decades ago, the Kidney Disease Outcomes Quality Initiative (KDOQI) introduced guidelines to enhance the diagnosis and treatment of kidney disease, benefiting thousands of patients [53].


Self Quiz
Ask yourself...
- What challenges and opportunities might arise from the goal to reduce new ESRD cases by 25% within a decade, and how could this impact the overall healthcare landscape for kidney disease?
- How might the shift towards 80% adoption of home-based therapies and transplants by 2025 transform patient experiences and outcomes in managing end-stage renal disease?
- What advancements or changes in policy and practice are necessary to meet the aim to double the availability of kidneys for transplantation by 2030?
Conclusion
Given the complex landscape of chronic kidney disease management and the evolving strategies for treatment, including the push for increased transplants and home-based therapies as outlined in the Advancing American Kidney Health initiative, the future state of patients with end-stage renal disease (ESRD) appears poised for significant transformation.
The initiative's ambitious goals aim to address the critical shortages in available treatment options and the pressing need for a broader implementation of preventative measures and early intervention strategies. The emphasis on home-based therapies and the drive to double the availability of kidneys for transplantation by 2030 reflect a holistic approach to tackling the multifaceted challenges of kidney disease management, promising a future where patients can expect more personalized, accessible, and effective care.
The ongoing support for research and the development of new treatment modalities further underscore the commitment to improving outcomes for those affected by chronic kidney disease, highlighting the potential for advancements in care that could dramatically alter the ESRD treatment paradigm.

Self Quiz
Ask yourself...
- Explain how palliative care could help a patient who is undergoing dialysis treatments.
- Why is it important for patients, regardless of renal failure stage, to set treatment goals, decision-makers, and power of attorney as soon as possible?
Pros and Cons of Treatment Modalities
Every patient diagnosed with chronic kidney disease must choose which treatment option(s) works best for them. Open and honest communication between the patient, family, caregivers, and the interdisciplinary team must take place to ensure that the patient is being treated in accordance with their wishes.
Patients must be seen monthly, if not more frequently, by their nephrologist to ensure that they are enrolled in the safest and effective modality to help them reach their optimal health. Each patient is unique, and their needs can vary depending on their health, preferences, and lifestyle. Each treatment option discussed has its pros and cons, which must be weighed when trying to decide which to choose.
As written above, the most prevalent option in the U.S. is the outpatient hemodialysis clinic. Many patients choose this option because they feel safer with the presence of direct patient care staff that provide and oversee their treatments. They also enjoy the social connections that are made in the clinic with other patients and staff. Cons of this modality include:
- Having to travel back and forth to the clinic at least three days per week
- Being at the mercy of the dialysis clinic's schedule, which can be inflexible due to the number of patients admitted, clinic's operating schedule, and staff scheduling
- Being vulnerable to the staff's level of competency and professionalism
- An increased risk of infection due to the invasive nature of the procedure, exposure to microbes, and proximity to other patients
- Cardiac complications due to the increased workload on the heart.
The most preferred hemodialysis access is the AV fistula, followed by the AV graft, so a fear of needles would be another consideration of this modality, no matter the setting.
Performing hemodialysis treatments at home is another option that is growing in popularity. There are three ways in which a patient can perform hemodialysis at home. Conventional "home hemo" is performed 3-4 days per week for 3-4 hours each time, just as with incenter. Short daily home hemo is completed 5-7 days per week for about 2 hours each time. Nocturnal home hemo treatments are done slowly (6-8 hours) while the patient sleeps. Treatments are either prescribed 6 nights per week or every other day. (1)
Any dialysis treatment to be done at home requires an assessment of the home by a dialysis nurse. The nurse assesses if the patient will be able to aseptically perform their treatments in their home environment. A clean space in the home must be devoted to the patient's dialysis treatments.
If pets or plants are present, they must be kept out of the room to prevent infection risks. The patient and/or care partner is trained by the nurse to maintain aseptic technique when handling their supplies, equipment and initiating and terminating their treatment. They are also taught how to properly disinfect their equipment and household items utilized in the treatment.
The positive benefits associated with home hemo are being able to perform dialysis treatments in the comfort of the patient's own home; flexible scheduling, fewer trips to the dialysis clinic, and in the case of the conventional and nocturnal options, slightly more liberal diet and fluid allowance since treatments are performed more frequently.
Patients are shown to thrive more when dialyzing at home. Generally, the more dialysis a patient receives, the more waste removal and balancing of electrolytes occurs; thus, these patients usually feel better and have a better quality of life. Patients tend to sleep better, with decreased restless leg syndrome and neuropathy. And they have more energy day to day. Less medication is required to control blood pressure, anemia, and phosphorus levels. Morbidity and mortality rates are also decreased (1).
The cons of home hemodialysis treatments include:
- The physical space that the machine and supplies take up in the patient's home
- The absence of trained staff to perform the treatments
- Shifting the responsibility solely to the patient or care partner
- There could be fear of putting in one's own needles.
- In the case of nocturnal hemodialysis, having a care partner is nonnegotiable for safety reasons.
The training time to safely perform treatments at home requires a commitment of weeks to months, depending on the progress of the patient and/or care partner. They will not be released home until the training nurse is confident that the treatments can be performed safely at home. This may mean a leave of absence from work or school to meet the training time requirements.
Peritoneal dialysis is the treatment that most nephrologists and nurses would choose if they were diagnosed with renal failure. It is considered to be gentler on the body than hemodialysis. Because it is performed every day, patients report feeling better and having a more liberal diet and fluid restrictions. There are no needles used in PD, and patients feel more comfortable dialyzing in their home environment, at whatever time they choose. Cons include:
- Having to dialyze daily
- Potential complications such as peritonitis
- Drain pain (pain in the abdomen when fluid is being emptied by the catheter pulling the fluid out)
- Intolerance of fluid in the belly during the dwell period
- Dialyzing in the home environment requires ample storage space for the supplies that are needed. Delivery of supplies can be more frequent if the patient has limited storage space.
The benefit of a kidney transplant is that the patient no longer has to undergo dialysis treatment, and so their lives can almost return to life as it was prior to their kidney failure. It is important to remember that a kidney transplant is not a cure. If the same circumstances exist that caused renal failure in the first place, the transplanted kidney may not last long. While eating and drinking can return to normal, it is advised that the patient follow a heart-healthy diet (1). Even if the patient does everything perfectly, there is always a chance that the new kidney will fail eventually, and the patient may find themselves having to decide which treatment option is best for them again. It is the hope that the kidney will last for years; however, many patients require more than one transplant in their lifetime. Kidney transplant recipients must take anti-rejection medications so that their body's immune system does not attack the new kidney. These medications can be expensive, have side effects, and can leave the patient susceptible to illness. In any surgery, there are inherent risks, and the kidney transplant surgery is no different.

Self Quiz
Ask yourself...
- How would you approach a patient who is new to dialysis that has a fear of needles?
- Discuss which modalities might be appropriate for a patient who lives in a rural environment.
- Explain why a patient may not be a good candidate for home therapies.
Future State of Patients with ESRD
1 in 3 adults is at risk for kidney disease (1). Currently, there is a huge urgency to increase transplants and make home therapies the prevalent modality for ESRD patients. There will not be enough chairs available in clinics to treat the potential pipeline of dialysis patients incenter.
In 2019, President Trump addressed this issue and set 3 goals in an executive order:
- Prioritize a reduction of new ESRD cases by 25% in 10 years.
- Increase home therapy and/or transplant utilization to 80% by 2025.
- Double kidneys available for transplant by 2030.
In the meantime, there is ongoing research to strengthen the fight against kidney disease. Through the National Kidney Foundation, there are grants and clinical trials underway to find a cure or better treatment options for the CKD population. Kidney Disease Outcomes Quality Initiative (KDOQI) guidelines were established about 20 years ago to improve the diagnosis and treatment of kidney disease, and that has had profound effects in the lives of thousands of patients.

Self Quiz
Ask yourself...
- What do you think is the motive for President Trump's executive order given in 2019?
Conclusion
In conclusion, there is a lot to know about renal failure and the renal failure stages. This course provided an overview of chronic renal failure stages, causes, treatments, and outcomes. Though a lot has been learned through research and advocacy efforts, there is much more to be learned about how to slow this disease's prevalence and progression.
Managing Conflict in a Nurse Leader Role
Conflict
Conflict is a natural occurrence within human interactions. It is an internal discord resulting from actual or perceived differences in ideas, objectives, values, goals, preferences, attitudes, expectations, beliefs, or feelings between two or more parties (8). Conflict can occur between any healthcare team member, including nurses, nursing students, managers or nurse leaders, physicians, patients, and family members.
Evoking feelings of hostility, anxiety, and stress can be highly disruptive to a unit or department's functioning. Another definition includes a disagreement through which the parties involved perceive a threat to their needs, interests, or concerns. In the workplace, conflict often involves personal agendas, insights, or goals (11).
Conflict is often seen as unfavorable, but if managed correctly, it can be positive and lead to personal and organizational growth. Conflict can promote team-building skills, critical thinking, new ideas, and alternative resolutions (11). If conflict is not managed effectively, it can hinder a healthcare team from providing quality patient care and can escalate into violence and abuse (16). Because of this, nurse leaders need to be aware of how conflict can escalate and be prepared to prevent or manage it in the workplace (8).
Stages
Once you have accepted that conflict is inevitable, you can learn how to deal with it within the nursing leader role. Awareness of these five stages will help you identify conflict and intervene before it escalates. Conflict within organizations often follows five different stages.
Stage 1: Potential opposition or incompatibility – Organizations themselves can cause conflict due to environmental factors. Factors within the organization include:
- A lack of communication or misunderstandings can cause communication difficulties.
- Leadership styles, role hierarchy, or reward systems
- Personal variables such as differences in values or beliefs
Stage 2: Condition and personalization- Those within the organization become aware of the environmental factors causing conflict and perceive them as unpleasant. Negative emotions develop, such as anger, frustration, or anger, and are aggressively directed at management or supervisors.
Stage 3: Intentions—Once one or both parties involved have identified conflict, it needs to be decided how the conflict should be managed. Conflict is often handled using five conflict management strategies: accommodating, avoiding, collaborating, compromising, and forcing.
Stage 4: Behavior- conflict has become visible to others, and managers or human resources intervene.
Stage 5: Outcomes—Conflict has now resulted in positive consequences that can lead to improved outcomes. Alternatively, it can remain unresolved and divide individuals, creating cliques or "sides," which leads to gossip, hostility, chronic complaining, competing for power, and decreased productivity.

Self Quiz
Ask yourself...
- When fulfilling a nurse leader role, why should you be responsible for conflict management?
- Think about a work conflict. At what stage was it managed?
- List three stages of a conflict?
- Give one definition of conflict.
Types of Conflict
The first step in managing conflict is to identify the type of conflict. Conflict can be categorized into three different types that nurse leaders will encounter. Understanding what type will help dictate how you will respond and enhance your conflict resolution skills. Healthcare and nursing present a unique environment, which can lead to different kinds of conflict. We all bring our values, ideas, thoughts, and education to this work environment. Conflict can occur in other types: interpersonal, organizational, intrapersonal, intra-group, or inter-group. Let’s break these down.
Interpersonal conflict (3)
- Most common type of conflict
- This can occur between fellow nurses, nursing students, patients, or colleagues.
- This occurs when two people can not agree on a topic; in other words, they can not see eye to eye.
This can often happen due to the following:
- Shortage of information
- Environmental stressors
- Differences in morals or opinions
- This can lead to social distancing, dominance, miscommunication, stigmatization, prejudice, stereotyping, coercion, and bullying.
- Obstructs professional interactions between healthcare teams, which weakens overall collaboration
- Example: When a team member feels another team member is not pulling their weight, or they disagree with another nurse’s assessment or a physician’s recommendation
Intrapersonal conflict (3)
- Internal disagreement with your thoughts, emotions, or values
- Can arise from ethical concerns, work-life imbalance, or uncertainty about role
- It can be the most challenging to solve
- This can often result in burnout
- Example: Nurse is overwhelmed with nursing tasks while trying to find the time for bathroom and meal breaks or if they are at work and their child is at home sick
Organizational (3)
- Disagreement occurs within large organizations such as hospitals. When policies, procedures, or communication patterns. differ
- Example: How are hospital funds distributed? Does the money go to the lab for new equipment or the emergency room for new stretchers? Conflict arises when one group believes their need is more important than the other.
Inter-group (3)
- Conflict exists between members of different organizational groups that have different values, beliefs, or goals. It could be team members who feel like their needs are unheard of or feel undervalued by administration or management, or it can occur between different units or departments. Conflict such as this can decrease productivity and interrupt quality patient care throughout the organization.
Intra-group (3)
- Conflict occurs between members of the same team (unit or department). Teamwork and a sense of belonging are essential for running a unit smoothly. Differences and disagreements can cause tension for everyone, even if they are not directly involved in the conflict. If this type of conflict is left untreated, it will divide the unit/department into groups, creating cliques or "sides," which leads to gossip, hostility, chronic complaining, competing for power, and decreased productivity.

Self Quiz
Ask yourself...
- Can you identify the different types of conflict?
- What signs would you see when experiencing an interpersonal conflict?
- Have you experienced any of the types of conflict listed?
- How would you explain the differences between inter-group and intra-group to a fellow nurse manager?
Generational Conflict (4)
Generational Differences
The generational conflict has grown within organizations due to having more generations than ever working together, especially in healthcare. Unprecedented, the nursing workforce spans five generations, each with distinct characteristics and work ethics. The various generations are described as follows:
- Baby Boomers: Born between 1947 – 1964. Characteristics include a belief that workers need to pay their dues. Often, the generation includes workaholics with traditional learning styles; rewards are expected for hard work (3).
- Generation X: Born between 1965 – 1977. Characteristics include independence, self-reliance, and skepticism of authority. This generation tends to work better with flexibility (3).
- Millennials (or Generation Y): These people were born between 1978 and 1991. Their characteristics include being goal-oriented, technological, entrepreneurial, and needing feedback. This generation wants to be coached and mentored (3).
- Generation Z: This generation was born after 1991. Although we do not know much about this generation yet, some of its characteristics include tech-savviness, self-starting, and pragmaticity (3).
Most of you know the phrase, "nurses eat their young." This is not a new concept, and despite the valiant efforts of organizations, this type of conflict has persisted. Usually, horizontal, nurse-to-nurse bullying with the older generations makes the new generations feel unwelcome, incapable, and unwilling to help when asked (4). However, it is essential to note that the opposite is also a workplace issue. Younger, newer nurses are perceived as faster, able to utilize technology at lightning speed, and can cope better with variable shifts than older nurses. This gives the newer nurse a perceived power gradient over the older nurse and can be used as a form of bullying (4).
Types of Generational Conflict (4)
As previously discussed, each generation has its own defining characteristics, and conflict can arise when they are forced to work together. Each generation will have a different outlook on how work should be done, and with that comes different expectations. Let’s take a look at intergenerational conflicts and the three major differences among generations within organizations.
Behavior-based conflict
- It arises when the other's behavior due to generational differences conflicts with their own and comes from how each generation communicates. They often do not communicate with one another, which causes conflict. Examples of communication styles between the generations:
- Baby Boomers prefer face-to-face
- Gen X prefers using what they believe is most efficient
- Gen Y prefers instant messaging, social media, or emails and is often considered poor communicators
- Gen Z and Millennials prefer text messaging and instant messaging
These differences in communication styles lead to conflicts of communication and collaboration between different generations. This lack of communication can cause team members to work individually instead of collaboratively. It can also lead to work-value conflicts, intrapersonal conflicts, and other conflicts. The success of the organization or the team depends on managing these different types of communication styles.
Another behavior-based conflict is the difference in each generation's expectation of feedback. Examples of feedback expectations per generation:
- Baby Boomers like feedback but not constantly
- Gen Y and Z require constant feedback
Conflicts arise based on how different generations view and expect feedback; it can cause frustration among team members and potentially affect teamwork and patient care.
Value-based conflict
The perception is that each generation has different values (intrinsic or extrinsic) and what motivates them. Conflicts can arise if team members are not motivated with certain methods.
- Baby Boomers believe in hard work and are motivated extrinsically (promotions, titles, corner offices, reserved parking)
- Gen Xs are distrustful of organizations and are intrinsically motivated by work independence and achieving work-life balance.
- Gen Y is motivated both extrinsically and intrinsically. They value personal achievement and work-life balance and place high importance on technology's ability to make work faster and easier.
- Gen Z is intrinsically motivated and values financial stability. They understand the importance of work but will not sacrifice their lives for work success.
Identity-based conflict
This type of conflict arises when there are differences between how generations see their own identity and the identities of other generations. It comes from wanting to belong to a group or comparing themselves to different groups. Conflicts arise when generations make comparisons to one another. This is often where hostile generalizations and stereotypes that create stigma against a group come from.

Self Quiz
Ask yourself...
- Identify which generations you currently work with.
- Identify your generation. What characteristics do you possess?
- Have you been bullied? How did it make you feel?
- Did you report being bullied? Was it handled?
- Think about the last conflict you had with a coworker. How did you handle the conflict?
- Can you identify generational conflicts you have witnessed or been involved in?
Examples of Nursing Conflicts (1)
- Staff conflicts regarding workloads, staffing ratios, and shift preferences
- Interdisciplinary disagreements about treatment plans, responsibilities, or the current decision-making process
- Ethical disputes on topics such as:
- End-of-life care
- Patient autonomy
- Organizational policies
- Poor communication resulting in misunderstandings or lack of information
- Role conflicts resulting from overlapping roles or uncertainty in responsibilities
- Resource conflicts due to limited supplies, equipment, or budget allocations
Leadership
A person’s conflict management skills are only one component of effectively managing conflict in the leadership role; they help raise future managers' emotional intelligence. Leadership skills and style are likely to affect the outcomes of conflict, while the relationship between leadership styles and conflict management (8)
Qualities
Leadership, by definition, is when one group or person sets the direction for others and helps them to achieve their goals (11). Leadership is a process that requires many different qualities; this should begin with relational intelligence. Relational intelligence revolves around the idea of how you positively navigate through relationships with others. For one fulfilling a nurse leader role, this skill is necessary for your team’s success (5). Although nurse leaders are looked to when there is conflict, it is not solely their responsibility to resolve it but that of all team members (5).
Other qualities needed include integrity, critical thinking, communication, dedication, self-awareness, and professionalism. There is not an adequate or inadequate strategy to deal with conflict. However, early detection of conflict and adoption of the most effective conflict resolution behavior is essential in organizations as soon as possible (6). How these qualities are learned is an important issue. Many nurse leaders need more training to prepare them for the responsibility of conflict resolution. However, unresolved or unmanaged conflict may end with work disruption, poor performance, tardiness, absenteeism, low staff morale, low productivity, increased psychological distress, and burnout (6). It can affect the productivity of the organization.
Another essential quality to develop at all levels of nursing, especially for those in a nurse leader role, is communication skills, including both how the message is sent and how the message is received. Listening skills are a vital aspect of nursing, and often, we move quickly and think about an answer before the person finishes speaking; misunderstandings are easy to cause but only sometimes so easy to fix.
For nurse leaders, it is essential to recognize and manage conflict. Barriers often exist, including time constraints, fear of retaliation, and fear of exclusion. Of course, no one wants conflict, which sometimes results in an attempt to soothe and prematurely find a solution. Those in the nurse leader role must learn to positively engage in conflict resolution and stay committed to promoting collaboration and effective care. Being successful includes dialogue, coaching, the identification of potential conflict, education, and training.
Styles
Leadership styles are management thoughts and behaviors related to your personality, communication preferences, strengths, weaknesses, and values (11). Styles can develop over time or be influenced by the organization. To prevent or limit conflict, leaders should implement a professional code of conduct, ground rules, and discipline (11). Leadership styles in healthcare are found to be strongly tied to quality care, patient outcomes, mortality rates, injuries, patient satisfaction, and pain (11). Leadership styles that are more successful and effective include collaboration, multifaceted, and dynamic. Believe it or not, leadership styles play a role in conflict resolution and team dynamics. The most common styles leadership styles are (11):
- Servant Leader and Lean Leader: This style is team-oriented and involves openness in conversations and management. It ensures others are a priority by focusing on their needs and growth and putting them first. This style improves processes, eliminates waste, and promotes high-quality, cost-effective care.
- Authoritarian Leader: This leader leads via dictation and controls all team actions and decision-making. All decisions are based on the leader's ideas, judgments, and personal beliefs, and the leader does not consider or consult team members. The leader and little input from team members involve a lot of enforcement.
- Transformational Leader: Transformational leaders assist the team in aligning their beliefs and values with those of the organization. This leader fosters trust, relationship building, and sharing of ideas and visions for the organization. The transformational style has defined goals, a clear direction, and looks at the big picture. Those in the leadership role share their vision with staff and think outside the traditional path. This has the idea that when involved in a conflict, responses will reflect the organization's greater good. The ability to manage conflict effectively is a quality seen by transformational leaders. This style is seen as being positive.
- Lassiez-Faire Leader: The laissez-faire style is casual and laid back, meaning there needs to be more leadership; they leave the decision-making to their team members. This type of leader trusts their team members to problem solve, create new projects, make and meet goals, and self-monitor. Authority is turned over to the staff; there is no feedback, oversight, direct leadership, discipline, or praise. Productivity is often low among team members, and conflict is highly likely. Generally, this style is seen as being negative because it wants to avoid conflict and is unsuccessful.
- Visionary Leader: This leader has a vision or long-term goal in mind. These leaders often have insight, imagination, and passion related to goals and ideas. They are constantly looking out for the team's best interests by sharing ideas and goals. They empower their team members by building a solid team dynamic capable of managing conflicts via communication in a positive way.
- Transactional Leader: Leaders with this style are focused on workflow, meaning they focus on incentives for “doing the work” in a timely and efficient manner. Components of this style include rewards and discipline based on finishing work ahead of schedule or if the work is delayed. These leaders need to plan for the future of their organization by being focused on the present. This type of leadership is harmful as it fails to promote ideas required for the rapidly changing healthcare industry.
While developing a style, it is essential to allow for the expression of multiple viewpoints and how to build better relationships (11). The absentee leader needs to do more to communicate, mentor, and plan. The incompetent leader needs more involvement in planning and faces severe moral issues. If the environment is maintained and cohesive, job satisfaction and performance can be positively impacted.
Nurse Leader Role: Conflict Strategy
As one involved in a nurse leader role, in order to effectively eliminate or manage conflict, it cannot be ignored. Engagement must be an ongoing process. To be successful, one must learn to not only engage in conflict, but remain engaged to promote collaboration and effective care coordination (11). The earlier conflict is identified, the better, as dysfunctional patterns can take place and can potentially define the culture of the department.
Common Strategies (11):
- Safe Space: It is important that staff feel they are meeting in a safe space, and that there is privacy and support.
- Coaching: Coaching can be in either group or individual settings. Coaching sessions are confidential (unless otherwise agreed upon), must follow a consistent format, and include a written summary of the session.
- Facilitation: There is usually a defined agenda. You will need someone neutral who can see past the fireworks or walls of silence and assist the group with arriving at the core problems or issues.
- Dialogue: The importance is to have a discussion that addresses the issue and clears the air; avoid saying “always” and “never.” Nursing leaders and direct care nurses need to engage in dialogues that address conflict and conflict management behavior as a first step in creating a healthy work environment (1).
- Collaborative: Collaborative works with the group problem solving together.
- Storytelling: Storytelling works with traditional stories that are told to help move from personal experiences to broader, helping to negotiate group conflict.
- Mediation: Can be formal or informal.
- Education and training: Nurses need to be educated on conflict and conflict management strategies that address and effectively resolve conflict. Learning conflict management strategies empowers nurses to resolve conflict early and influence the work environment in which they deliver patient care. "The training should not be limited to the handling of interpersonal conflicts; it should include all types of conflict commonly encountered in the healthcare setting. Additionally, individuals who have a propensity for managing conflict well should be identified and developed” (1). Education and training should also include communication skills.
"Leaders can change the climate in the workplace and promote better collaboration among workers by interrupting a group's dysfunctional behavior patterns," (12). Adding the skills of self-awareness and emotional skills helps to bring a team together. Relational ethics emphasizes the importance of mutually respectful relationships. People work to improve their awareness of how their choices and actions help shape their conversations and social interactions. The relational approach addresses conflict as it unfolds – just as a relationship evolves and unfolds over time. It incorporates the essential qualities that form the core of human relationships. It is hard to imagine an approach to conflict that excludes consideration of integrity, respect, identity, compassion, humility, shame, trust, fear, hope, pride, acceptance. Love, joy, and other human dynamics are at the heart of most conflicts (12).
Emotional and social intelligence are defined as "skills that enable an individual to understand the impact of emotions on behavior and thinking, to regulate emotions and behavior, to understand the importance of emotions in others, and to understand social interactions and engage in adaptive ways with others in social situations," (12).

Self Quiz
Ask yourself...
- Define two traits of Relational Intelligence. What is your strongest trait?
- List three traits of a leader.
- Identify the successful styles of leadership.
- What type of leadership does your work unit have?
Regulatory Issues and Conflict
In 2008, The Joint Commission released a sentinel event alert addressing disruptive behaviors and recommended how organizations should address their relational issues and conflicts. The defined behaviors recognized more physician-to-nurse issues but placed all disruptive behavior on its radar. Identified behaviors included verbal outbursts, physical threats, uncooperative attitudes, and cooperation refusal (i.e., not taking pages or answering calls). Other behaviors include condescending language and refusing to complete tasks (9).
Disruptive behaviors often go unreported and, therefore, unaddressed for several reasons. Whether that is fear of retaliation, the stigma associated with "blowing the whistle" on a colleague, or a general reluctance to confront an intimidator, it all contributes to underreporting intimidating and disruptive behavior (9).
Part of the sentinel event has given guidance on what defines behaviors and required resolutions. Organizations are needed within this mandate to develop a specific ‘Code of Conduct’ that outlines acceptable and disruptive behaviors and the processes managing these behaviors. Additionally, organizations should establish policies and procedures that clearly state zero tolerance and provide training and education for physicians.
Regarding nurse-to-nurse (horizontal) disruptive behavior, the American Nurses Association (ANA) Code of Ethics for Nurses includes interpretive statements outlining that nurses are required to "create an ethical environment and culture of civility and kindness, treating colleagues, coworkers, employees, students, and others with dignity and respect" (10).
Similarly, nurses must be afforded the same respect and dignity as others; thus, the nursing profession should no longer tolerate violence from any source. As someone fulfilling a nurse leader role, you must refer to the ANA Code of Ethics for Nurses when managing conflict within the workplace.
Negative Behaviors
Familiar sources of conflict can include passive-aggressive communication, clique behaviors, lateral or vertical aggression, and other types of incivility. These sources can cause unprofessionalism and disruptive actions that can compromise patient safety, increase turnover and absenteeism, and reduce the overall joy of work (7). Let's look at the following negative behaviors often seen in conflict and how to deal with them potentially (7).
- Defensiveness (7)
- It is human nature to deflect when we hear something negative about ourselves, our interests, or our friends. Critical conversations will be redirected to focus on someone else's flaws instead.
- Redirect behavior and state facts.
- Victim mentality
- Individuals feel mistreated, singled out, or held to a higher standard.
- Remind people that personal conversations are confidential and held to the same standard as everyone else.
- Restate all expectations are clear
- Passive aggressiveness
- Confront and be direct
- Encourage open communication and concerns
- Vertical aggression
- Bullying of new leadership
- Address head-on and state expectations
- Bullying
- Identify and address immediately
- Provide clear examples of actions
- The informer
- Performance information given by peers and not leadership
- Hold team members accountable
- Address behaviors expressed by other team members

Self Quiz
Ask yourself...
- Can you recall a time when you witnessed negative behaviors of conflict?
- Do you have any behaviors among team members? If so, how does it affect productivity and patient care?
- Think about how you would manage these negative behaviors.
How to Manage Conflict (1)
Nursing requires a teamwork approach to provide safe, quality care; therefore, everyone must work together to solve conflicts. How you and your team respond to conflict will vary based on the situation and the individual personalities involved. Conflict resolution is defined in various ways. Thomas and Kilmann formulated a matrix with five distinct responses (methods, modes, or styles) to conflict resolution or management. Here are five different conflict management styles (Thomas-Kilman Conflict Modes) to try within your team when resolving conflicts.
Accommodation (11)
- Using this style results in a win-lose situation. The resolution to the conflict will only benefit one person and will not satisfy all involved. This style of conflict management can cause resentment. It is a strategy often used to maintain peace by smoothing over differences. It can be appropriate to escalate the issue if it results in a severe disruption.
Collaboration (11)
- In this particular style, all team members are brought together to resolve. It allows for solving the conflict by objectively evaluating different views. This style encourages open and respectful communication, active listening, and open-mindedness. Everyone involved will have a say in what caused the conflict and how to achieve a resolution. Collaboration often leads to new ideas and creativity and is the best outcome for all team members.
Compromise (11)
- No team members will be satisfied with the solution during this management style. The resolution to the conflict will cause resentment between all individuals involved because those involved will have to sacrifice a part of their solution. It is a bargaining strategy that protects the relationship's importance and can provide a temporary solution.
Avoidance (11)
- When using this conflict management style, some or all people involved will avoid or ignore the situation. This ends up being a losing situation, and the conflict remains unresolved. It will continue to build up disputes among team members. No cooperativeness exists between the parties involved, and no one’s concerns are met. The purpose is to delay or walk away, often due to immense anger. This is considered a short-term resolution to de-escalate an agitated, non-emergent situation.
Competition (11)
- This style creates another win-lose situation. It is a short-term solution strategy to resolve the problem. It can involve aggressively resolving the conflict when one individual has more decision-making power. It will not promote a team approach to problem-solving or resolving future disputes.
Steps for Conflict Management (11)
- Set rules on how to communicate effectively and respectfully
- Ask all team members to set aside previous judgments about one another
- Encourage active listening without interruption to ensure all are heard equally
- Have everyone involved write down the problem and then state the problem out loud. This will help to provide understanding and agreement about what is causing the conflict.
- Ask everyone involved to devise a solution to the problem or conflict.
- Set time aside to discuss each solution along with the positives and negatives of each solution.
Nurse Leader Role: Conflict Strategy Resolution
As one involved in a nurse leader role, it must be addressed to eliminate or manage conflict effectively. Ignoring the conflict or problem can result in your team developing resentment towards one another, making the work environment uncomfortable (1). Rushing to fix conflicts without determining the source of the issue can often lead to other future problems (1).
You must take the time to analyze the situation and identify the source of the conflict before proceeding to resolution. Conflict resolution requires patience, active listening skills, and commitment to finding a solution that benefits both parties (1). The goal is to address conflicts within your team and promote a safe and harmonious work environment that provides quality patient care (1). Engagement must be an ongoing process. To be successful, one must learn to not only engage in conflict but also remain engaged to promote collaboration and effective care coordination (1). The earlier conflict is identified, the better, as dysfunctional patterns can take place and potentially define the department's culture. Conflict resolution in nursing requires communication, collaboration, and listening skills. Here are some tips for handling conflicts:
Common Strategies (1):
- Safe Space: Create a safe place or mutual ground for all parties involved. It is essential that staff feel they are meeting in a safe space and that there is privacy and support.
- Guidance and Coaching: Develop effective communication and conflict-resolution skills and support suggestions for productive and creative solutions. Coaching can be in either group or individual settings. Coaching sessions are confidential (unless otherwise agreed upon), must follow a consistent format, and include a written summary of the session.
- Facilitation: There is usually a defined agenda. You will need someone neutral who can see past the fireworks or walls of silence and assist the group in identifying the core problems or issues.
- Foster Open Communication: Create a supportive environment that encourages active listening and honest communication. Be sure to understand the situation entirely. It is essential to have a discussion that addresses the issue and clears the air; avoid saying “always” and “never.” Nursing leaders and direct care nurses must engage in dialogues that address conflict and conflict management behavior as a first step in creating a healthy work environment.
- Collaborative: Collaborative works with the group problem-solving together.
- Storytelling: Storytelling uses traditional stories to help people move from personal experiences to broader ones and negotiate group conflict.
- Mediation: This can be formal or informal.
- Education and training: Nurses need to be educated on conflict and conflict management strategies that address and effectively resolve conflict. Providing team members with strategies to resolve disputes early before impacting patient care is essential. Learning conflict management strategies empowers nurses to resolve conflict early and influences the work environment in which they deliver patient care. Training should include all strategies one would encounter in the healthcare setting, not just those limited to coworkers. Education and training should also include communication skills.
- Mediate and negotiate: Approach the conflict objectively and seek additional perspectives from human resources or another nurse leader if necessary. Facilitate constructive dialogue to reach a mutually agreeable solution.
- Identify underlying issues: Identifying the conflict's root cause is crucial. Work on finding solutions that aren’t quick fixes and address the core problem. This is also an opportunity for growth and development, including developing policies and procedures to help identify future conflicts.
- Encourage empathy: Ask questions that promote different perspectives and creative solutions. Identify and discuss underlying interests that can often interfere with views.
- Seek a compromise: Find common ground and work together toward a mutual agreement. Stress the importance of collaboration.
- Encourage professional behavior: Rule out and quickly address bullying and rude, discourteous, or disrespectful behaviors. Identify, admit, and apologize if you have contributed to the conflict.
- Follow established policies and procedures: Be consistent with standards and potential consequences while handling conflicts fairly and openly.
- Document the issue and provide follow-up: Document the situation, steps taken, and the resolution. Continue to monitor to ensure the problem is resolved and does not reoccur
"Leaders can change the climate in the workplace and promote better collaboration among workers by interrupting a group's dysfunctional behavior patterns (12)." Adding self-awareness and emotional skills helps bring a team together. Relational ethics emphasizes the importance of mutually respectful relationships. People work to improve their awareness of how their choices and actions help shape their conversations and social interactions. The relational approach addresses conflict as it unfolds – just as a relationship evolves and unfolds over time. It incorporates the essential qualities that form the core of human relationships. It is hard to imagine an approach to conflict that excludes consideration of integrity, respect, identity, compassion, humility, shame, trust, fear, hope, pride, and acceptance. Love, joy, and other human dynamics are at the heart of most conflicts (12).
Emotional and social intelligence is defined as "skills that enable an individual to understand the impact of emotions on behavior and thinking, to regulate emotions and behavior, to understand the importance of emotions in others, and to understand social interactions and engage in adaptive ways with others in social situations" (12).
Nursing Interventions for Acute Pain Management
Introduction
Pain is one of the most common reasons people seek care in a hospital and one of the most distressing symptoms of hospitalized patients. It is also directly linked to a patient’s satisfaction with their care: people are more likely to report being unhappy with their care if they had unrelieved pain during their stay [24].
Most importantly, it is our job as nurses and healthcare providers to help relieve the pain and suffering of the people in our care. There are legitimate concerns about the overuse and addictive nature of opioid pain relievers, and thankfully there are many alternative options. These non-opioid nursing interventions for acute pain management include non-opioid pain relievers, complementary techniques, and non-medication strategies [17].
Nurses must regularly assess pain and collaborate with both the patient and provider to ensure that timely access to adequate pain relief is a priority of their care.
Prevalence of Acute Pain
Acute pain is a major problem for hospitalized patients and has been identified as a priority in the provision of quality and effective care. In addition, pain management has been identified by the Quality and Safety Education for Nurses (QSEN) project for nurses as a core competency under Patient-Centered Care [28]. This is important because if not properly treated, pain can cause anxiety, depression, reduced healing, fatigue, non-compliance with treatment, and longer hospital stays [12, 20]. Pain is also costly in other ways: causing decreased productivity, income, and quality of life [11].
Despite knowing the potential consequences of poor pain relief and having multiple modalities available as nursing interventions for acute pain, many patients are still inadequately managed for pain during hospitalization.
A 2019 study reviewing pain management in patients with chronic pain in an outpatient setting found that 77% of patients reported a negative pain management index [16]. Another study found that patients over-report pain to increase provider responsiveness to their pain relief [4].
This is because many barriers still exist that prevent patients from being treated appropriately for their pain. These potential barriers include [1, 22].
- Lack of knowledge or skills about nursing interventions for acute pain management
- Heavy nursing workload or lack of time
- Provider concerns about causing tolerance or addiction
- Patient fears of side effects or addiction
- Insufficient provider orders or time to pre-medicate patients before painful procedures
- Providers focus on treating pathophysiology, rather than managing pain or other symptoms
While all healthcare providers should aim to reduce a patient's pain, nurses are in the unique position to make a difference with individual patients, as well as system-wide pain management protocols.

Self Quiz
Ask yourself...
- Think about the last time you were in pain. In addition to the physiological pain sensation, what other feelings did it invoke?
- What are some potential barriers to adequate pain relief that you've observed in your practice?
- How many nursing interventions for acute pain are you aware of?
- How many nursing interventions for acute pain have you used in your practice?
Pathophysiology of Pain
There is no set definition of pain, but it is commonly defined as an unpleasant experience, usually related to underlying tissue damage or injury. Pain is a subjective experience and one that very much depends on the person experiencing it. What one person experiences as pain, another person may experience as a minor discomfort, and another may be considered [19].
It is a complex sensation, the experience of which involves the interaction of three different systems [6, 19, 25]:
Sensory/Discriminative System
The actual sensation of and reaction to pain are sent through sensory and afferent nerves, the spinal cord, and the brain stem. This system causes the body to try to remove itself from the source of the pain.
Motivational/Affective System
A person's learned approach/avoidance behavior concerning pain occurs through the interaction of the brain stem, the reticular formation, and the limbic system.
Cognitive/Evaluative System
A person's learned behavior towards the pain experience, including appropriate (and inappropriate) pain behaviors. This learned behavior can block or increase a person's perception of their pain.
Anatomy and Physiology of Pain
The nervous system is the primary body system responsible for the experience and interpretation of pain. The four main steps involved in this process are transduction, transmission, perception, and modulation [5, 8 15].
Step 1: Transduction
The process of transduction begins with the afferent pathway, which is responsible for the actual detection of pain. Nociceptors are pain receptors found at the end of small afferent neurons that detect noxious stimuli, which include changes in temperature, pressure, and other mechanical or chemical stimuli. These nociceptors are found deep in the skin, muscles, tendons, and subcutaneous tissue and produce a large variety of different – and not all unpleasant – sensations. These can range from a cool breeze to a pleasant massage to cutting, crushing, and burning sensations.
When these receptors are activated, they release chemical mediators, such as prostaglandins, substance P, serotonin, histamine, bradykinin, and potassium. Among other functions, these mediators generate an action potential by exchanging sodium and potassium at the cell membrane and activating and sensitizing the nociceptors to further stimulation by the stimuli.
Step 2: Transmission
The sensation travels along A- and C-nerve fibers to the dorsal horn of the spinal cord. A-nerve fibers are lightly myelinated (insulated in a protein and fatty acid substance known as myelin, which allows nerve impulses to travel faster), while C-nerve fibers are unmyelinated. The thicker the nerve fiber (and myelin coating), the quicker that nerve impulses will travel. The table below shows the different types of these fibers and the sensations they detect. Nerve impulses travel the fastest among the A-alpha and A-beta fibers and slowest along the A-delta and C-nerve fibers [32].
|
Characteristics of Afferent Nerve Pathways |
||
|
Afferent Nerve Fibers |
Sensation |
Conduction Velocity (m/s) |
|
A-alpha |
Proprioception (the body’s position in its environment) and motor strength |
13-22 |
|
A-beta |
Light touch |
16-100 |
|
A-delta |
Pickling pain and temperature (cold) |
5-30 |
|
C |
Pain, temperature (warmth), itch, autonomic function |
0.2-2 |
Once these nerve signals reach the spinal cord, excitatory neurotransmitters cross the synaptic cleft with the nociceptive dorsal horn neurons (NDHN). The neurotransmitters involved in this process include [33]:
- Substance P
- Nitric oxide
- Bradykinin
- Glutamate
- Adenosine triphosphate
From here, the nerve impulse travels up the spinal cord to the thalamus, where they are sent to different areas in the brain for processing.
Step 3: Perception
Pain perception translates all this nerve activity into a conscious and actual experience for the patient. This is facilitated by several different areas of the brain and central nervous system.
Reticular Formation Tracts
Reticular formation tracts are responsible for the recognition of and response to pain. For example, if you step on a tack, the reticular formation track recognizes the painful stimulation and causes you to move your foot quickly. This area is also responsible for the alert and attentive feeling that comes with pain.
Limbic System
The limbic system also plays a key role in the unpleasant emotional and behavioral response to pain and actions taken to reduce it.
Thalamus
The thalamus acts as a switchboard of sorts, helping to direct the pain signal to the different locations in the brain. Some parts of the thalamus also direct the motor, behavioral, and emotional responses that occur when painful stimuli are present.
Somatosensory Cortex
The somatosensory cortex comprises two distinct regions in the parietal lobe of the brain that are responsible for receiving and processing sensory information from all over the body. This region receives information about painful stimuli and identifies the location, intensity, and type of pain. It also connects the current pain sensation with previous experiences with pain.
Step 4: Modulation
Modulation is the final step in the pain pathway. This process changes the pain impulse transmission in the spinal cord due to the descending modulatory pain pathways (DMPP). Endogenous hormones and substances are found within this pathway and help to either block pain signal transmission or increase it. Inhibitory neurotransmitters help to block the transmission of pain nerve impulses to relieve pain and include [31]:
- Acetylcholine
- Oxytocin
- Serotonin
- Gamma-aminobutyric acid (GABA)
- Norepinephrine (noradrenalin)
- Neurotensin
- Endogenous opioids, such as enkephalins and endorphins
Excitatory neurotransmitters increase the transmission of pain to the brain and are usually responsible for the increased mental alertness and cognition associated with a painful event.
The Gate Control Theory is one of the most familiar theories of pain modulation. Under this theory, a series of gates are found throughout the spinal cord. When these gates are open, pain messages can get through to the central nervous system, making the pain feel worse. Factors like stress, tension, anxiety, boredom, and lack of physical activity can all help open those gates and worsen pain sensations [27].
On the other hand, when those gates are closed, fewer pain messages get through to the central nervous system, reducing the pain experience. Factors that help to close the gates include feeling relaxed, regular exercise, distraction, certain medications, and other types of stimulation (such as massage, heat, ice, or acupuncture). This theory is often used to explain why non-medication nursing interventions for acute pain can be so effective [27].


Self Quiz
Ask yourself...
- Why might distraction be an effective form of pain management for some people?
- How can anxiety and fear worsen a person's experience of pain?
- Does understanding the pathophysiology of pain help you to understand the rationale behind different nursing interventions for acute pain?
- How does the Gate Control Theory explain why non-medication nursing interventions for acute pain are effective?
Classification of Pain
Pain can be classified based on its duration, location, quality, and intensity. Understanding these different types of pain can help the medical and nursing team plan appropriate nursing interventions for acute pain management. The figure below shows the organization and classification of these different types of pain.
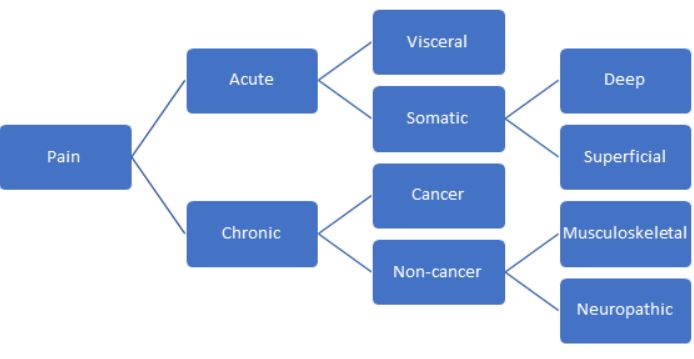
Flowchart describing the different types of pain based on location and duration.
Duration of Pain
One of the most common and important distinctions of pain is its duration. There are two classifications of pain based on duration: acute and chronic.
Acute
Acute pain is short-term pain that lasts less than three months. It is usually associated with a specific insult or injury, such as a broken leg, a ruptured appendix, or even childbirth. In most cases, once the cause is addressed and treated, the pain subsides. Acute pain is often described as sharp, stabbing, or burning. There are many effective nursing interventions for acute pain [19].
Chronic
Chronic pain, however, is far more complex. Chronic pain is pain that has lasted longer than three months or past the expected healing time from an injury or illness. Headaches, fibromyalgia, and arthritis are all examples of this type of pain. Chronic pain can be described as sharp or intense, but it can also be described as dull, aching, or burning.
In addition, chronic pain often has a psychological or emotional component, causing anxiety, insomnia, depression, and a decrease in a person's ability to perform everyday tasks. This type of pain is much more difficult to treat and can severely interfere with a patient's quality of life [19].
Location
Pain can also be classified based on the location where the pain is occurring. Both acute and chronic pain can be classified by any of these categories.
Visceral Pain
Visceral pain arises from the internal organs in the abdomen and pelvis, such as the intestines, female reproductive organs, kidneys, and liver. This type of pain is often described as diffuse, and it is often difficult to isolate where it is coming from. One reason for this is the phenomenon of referred pain, where the pain is experienced in a location different from the actual injury. Think about having left arm and shoulder pain during a heart attack.
While the internal organs are mostly immune from injuries like lacerations or burning (short of a catastrophic injury), they are more likely to cause pain by inflammation, ischemia (death of tissue), and stretch (like overdistended intestines). Visceral pain is often described as pressure, dull, throbbing, or aching [3]
Somatic Pain
Somatic pain, on the other hand, is pain that is experienced in the skin, muscles, bones, and joints. While visceral pain is diffuse, somatic pain is usually well-localized, and it is easy to determine where it is coming from. It is usually described as sharp, stabbing, aching, or burning. Somatic pain can result from an injury, such as a paper cut, or an illness, such as arthritis or bone cancer.
Somatic pain can be further categorized as deep or superficial, depending on where the injury occurs [3]
Deep Pain
Deep somatic pain comes from structures deep within the body, such as bones, muscles, tendons, and joints.
Superficial Pain
Superficial somatic pain comes from structures closer to the surface of the body, like the skin and mucus membranes.
Location
Pain can also be classified based upon the location where the pain is occurring. Both acute and chronic pain can be classified by any of these categories.
Visceral Pain
Visceral pain arises from the internal organs in the abdomen and pelvis, such as the intestines, female reproductive organs, kidneys, and liver. This type of pain is often described as diffuse, and it is often difficult to isolate where it is actually coming from. One reason for this is the phenomenon of referred pain, where the pain is actually experienced in a location different from the actual injury. Think about having left arm and shoulder pain during a heart attack.
While the internal organs are mostly immune from injuries like lacerations or burning (short of a catastrophic injury), they are more likely to cause pain by inflammation, ischemia (death of tissue), and stretch (like overdistended intestines). Visceral pain is often described as pressure, dull, throbbing, or aching.
Somatic Pain
Somatic pain, on the other hand, is pain that is experienced in the skin, muscles, bones, and joints. While visceral pain is diffuse, somatic pain is usually well-localized and easy to determine where it is coming from. It is usually described as sharp, stabbing, aching, or burning. Somatic pain can result from an injury, such as a papercut, or an illness, such as arthritis or bone cancer.
Somatic pain can be further categorized as deep or superficial, depending on where the injury occurs.
Deep Pain
Deep somatic pain comes from structures deep within the body. Think of bones, muscles, tendons, and joints.
Superficial Pain
Superficial somatic pain comes from structures closer to the surface of the body, like the skin and mucus membranes.
Pathophysiology
The last main way to classify pain is based on its cause or pathophysiology. There are three types of pain in this category: nociceptive, neuropathic, and psychogenic [19].
Nociceptive Pain
Nociceptive pain comes from an injury to the body tissues and is the type of pain that most people are familiar with. It can be acute, chronic, visceral, or deep pain. It covers many kinds of injuries or illnesses, from simple paper cuts or stubbing a toe to arthritis or cancer pain [19].
Nociceptive pain is usually responsive to changes in the environment: shifting position, applying ice or a heat pack, or elevating the injured site.
Neuropathic Pain
Neuropathic pain arises from damage to the neurons in the peripheral or central nervous system. Are you familiar with the tingling associated with hitting your funny bone? That's neuropathy: you've hit and temporarily injured the large nerve that runs through the elbow. Other common causes of neuropathies include multiple sclerosis, diabetic neuropathy, and even phantom limb pain [19].
Unfortunately, neuropathic pain doesn't respond well to changes in the environment and is more likely to develop into chronic pain. Damaged neurons or nervous tissue don't heal quickly or easily.
Nociplastic Pain
Nociplastic pain is a pain for which no readily identifiable underlying cause can be found and is attributed to psychological factors. Common conditions contributing to nociplastic pain include fibromyalgia, tension headaches, and irritable bowel syndrome [19].
This definition of pain has drastically changed over the past several years. Despite this changing definition, we do know that depression, anxiety, and other psychological problems can interact with pain, particularly chronic pain. Depression, anxiety, and other factors can worsen pain, and ongoing pain can significantly worsen associated psychological symptoms. As nurses, we should be mindful of and sensitive to these types of issues.

Self Quiz
Ask yourself...
- How could an untreated neuropathy develop into a chronic pain condition?
- How does understanding the classification of pain lead to more effective and patient-centered nursing interventions for acute pain?
- How could the nurse support a patient with a psychogenic pain disorder?
Performing a Pain Assessment
One of the most important nursing interventions for acute pain management is regular assessment of the patient's pain and the effectiveness of their pain management plan.
There are two main components of a pain assessment: a health history/interview and a physical exam.
Health History and Interview
Assuming that you are working with an established patient, you don't need to complete a full history or patient interview, but you should touch upon the relevant clinical factors about their pain. If this is a new admission or a new patient, you will need to perform a comprehensive initial history and assessment first.
The PQRSTU mnemonic can help you remember all the different points you should hit during the interview to assess the characteristics of their pain. The table below shows the important questions that you should ask about a patient's pain [9,21].
| PQRSTU Pain Assessment Questions | |
| Factor | Questions to Ask |
| Provoking/palliating factors |
|
| Quality/quantity |
|
| Radiating |
|
| Severity |
|
| Timing/treatment |
|
| Understanding/you |
|
Pain Scales
Pain scales are useful tools for nurses to assess and rate patients' pain. Several different scales can be used in different clinical situations, and it is up to the nurse's judgment to determine which is the most appropriate one to use [30].
Number Rating Scale
This is the most common pain scale and the one that most people are familiar with. It is appropriate for adults (or older children) who are alert, oriented, and responsive. Ask the patient to rate their pain on a scale from one to ten, with one being no pain and ten being the worst pain they've ever had.
Wong-Baker FACES
This pain scale is very commonly used for children aged three and older. It uses six pictures of faces, ranging from a face without pain to a face with a lot of pain. To use it, the child is asked to pick which face represents how they are feeling.
FLACC
The FLACC scale is used for young children from ages 0-2 years of age. It stands for Face, Legs, Activity, Cry, and Consolability. The nurse assesses each of these characteristics and assigns a score from zero to two. These scores are added together for a total score between zero and ten. The higher the number, the higher the patient's pain is assumed to be.
CRIES
The CRIES scale is also used for young infants who are greater than or equal to 38 weeks of gestational age. This scale is similar to the FLACC scale in that the nurse evaluates the infant based on five characteristics, assigning a score of zero to ten. The scores are totaled, where a score greater than 6 indicates the need for analgesia. The characteristics used by this scale are the presence of a high-pitched cry, the requirement of oxygen to maintain oxygen saturation above 95%, increased blood pressure and pulse, facial expression, and sleeplessness.
CPOT
The CPOT (Critical Care Pain Observation Tool) was developed to be used in critically ill patients who may not be able to verbalize their pain. It is similar to the CRIES and FLACC scales: four different criteria are assessed on a scale from zero to two, with a maximum score (indicating the most pain) of eight. The domains used in this scale include facial expression, body movements, muscle tension, and compliance with mechanical ventilation (in intubated patients) or vocalization (in non-intubated patients).
Please note that this is not a comprehensive list of all available pain scales. You should defer to your institutional policies when appropriate.
The patient should be assessed frequently, especially if they are having pain or receiving pain medication. The nurse should also ask about the presence of associated signs and symptoms: insomnia, nausea, vomiting, shortness of breath, itching, etc. Make sure to evaluate the effectiveness of the nursing interventions for acute pain by reassessing the pain level after administering analgesia or other non-pharmacological interventions.
The nurse must always remember that pain is what the patient says it is, regardless of their body language. If the patient states that their pain is a level 7, but is laughing and hanging out with family members, the nurse must document and act as if the pain level is a 7.

Self Quiz
Ask yourself...
- Which tools does your institution use for pain assessment? What are the policies surrounding pain assessment?
- What would you do if the pain scale recommended by your institution does not apply to your current patient?
- Which questions would the nurse ask a patient to get more information about the quality of their pain?
- Why is it important to reassess pain after administering any nursing interventions for acute pain?
Physical Exam
If appropriate, the physical exam should also be abbreviated and limited to what is relevant to the patient's pain. Make sure to get a set of vital signs and then examine the area that is causing pain.
- Look for redness/swelling/warmth of the skin.
- If the pain is related to a recent surgical procedure, check out the surgical wound and surrounding tissue.
- Palpate gently, if safe and appropriate, to determine where the pain might be coming from.
- If the pain is in a joint or muscle, perform a gentle range of motion exercises to see what movements trigger the pain.
If the pain is new, notify the provider in case it signals a change in status.

Self Quiz
Ask yourself...
- What questions would you ask, and which exam techniques would you use if a 12-year-old child presents to the emergency department after falling off a bicycle?
- How should you document a patient's pain level if their stated pain score is different from their behavior or appearance?
Non-Pharmacological Nursing Interventions for Acute Pain
For patients with mild pain, non-pharmacological nursing interventions for acute pain can sometimes be very effective. They can also work well in conjunction with pain medications and other nursing interventions for acute pain [18, 19].
Acupressure
Acupressure is a traditional Chinese modality that has been used for generations. By applying pressure to certain points on the body, it is believed that you can help restore the flow of energy and balance throughout the body. Though acupressure is mostly considered safe, some points should not be stimulated in pregnant women as they might stimulate labor. Press firmly and use an up-and-down or circular movement for several minutes. Make sure to stop or ease up pressure if the motion causes worsening pain or discomfort [18, 19].
Acupuncture
Acupuncture is also a traditional Chinese modality that has recently gained popularity in the United States and other Western countries. It is believed that the insertion of small needles into the skin at specific points helps to stimulate endorphin release and trigger other pain-relieving changes in the brain. The needles are left in place for 10 to 30 minutes at a time so the patient can rest. The needles are then removed, and the treatment is repeated several times. Acupuncture is quite safe but should only be performed by a licensed practitioner. Research about effectiveness is mixed, but it may be worth a try for patients with complicated or chronic pain [18, 19].
Aromatherapy
The use of essential oils is an ancient therapeutic modality that dates back hundreds of years and has gained popularity in recent years. It involves the absorption of essential oils through the skin or olfactory system to reduce pain, nausea, muscle tension, anxiety, and depression [18, 19].
Distraction
Distraction is an effective and simple nursing intervention for acute pain. Remember the gate theory of pain? Distraction is one of those factors that can help close the pain gates, reducing the experience of pain. The presence of strong sensory input can help a person be unaware of their pain [18, 19].
Music
Music therapy works similarly to distraction. It gives the person something else to focus on apart from their discomfort. When using this nursing intervention for acute pain, the nurse must remember to let the patient select the type of music that they prefer to listen to [18, 19].
Heat
The application of a heating pad or hot water bottle may stimulate the closure of the pain gates, reducing pain and discomfort. It may also stimulate the release of endorphins, which also reduce pain. The patient should be reminded to not lie directly on the heat source due to the risk of burns. If the nurse applies the heating pad, the site should be reassessed frequently to reduce the possibility of injury [18, 19].
Cold
Applying a cold or ice pack works similarly. Cold can relieve inflammation and pain and promote healing. It works best over inflamed joints. Like applying heat, the nurse must carefully and frequently assess the patient's skin to ensure that injury does not occur and remove the ice if the patient feels numbness, aching, or burning. Ice can be particularly effective before a needle puncture or injection [18, 19].
Guided Imagery
This nursing intervention for acute pain involves the nurse sitting close to the patient and helping them to create a calming and relaxing image in their mind. The nurse speaks quietly, helping the patient to concentrate on the image and relax [18, 19].
Massage
Massage is a great technique to soothe tense muscles and promote relaxation and sleep. This touch stimulation may trigger the release of endorphins or help to close the pain gates responsible for pain transmission [18, 19].
Biofeedback
Biofeedback is a type of behavioral therapy that is taught to the patient over several weeks. It allows the patient to visualize physiological responses and eventually learn to control them. This technique is particularly beneficial for people with headaches or muscle tension [18, 19].
Transcutaneous Electrical Nerve Stimulation (TENS)
This technique uses a special device that produces a mild electrical current through the skin via external electrodes. The machine produces a buzzing or tingling sensation, the intensity of which can be controlled by the patient in response to the pain they are feeling. This treatment does require a physician's order, and the nurse should help the patient with hair removal if needed before applying the electrodes [18, 19].

Self Quiz
Ask yourself...
- How should the nurse respond to a patient who refuses pharmacological pain medication in favor of alternative nursing interventions for acute pain?
- What is the best response by the nurse if a patient's family is encouraging him or her to only use non-pharmacological nursing interventions for acute pain?
- What method should the nurse suggest for a patient with frequent tension headaches?
- How does guided imagery help to relieve pain and promote comfort and relaxation?
- How many of these nursing interventions for acute pain have you used on patients or yourself in the past?
Analgesics as Nursing Interventions for Acute Pain
For patients with pain that does not respond to non-pharmacological measures, analgesics may be more effective. There are three types of pain medication:
- Non-steroidal anti-inflammatory drugs (NSAIDs) and non-opioids
- Opioids or narcotics
- Adjuvants
Non-Opioid Analgesics
Non-opioid analgesics can be used to treat mild to moderate pain and are often combined with opioid pain relievers to enhance their effectiveness. The two common types of drugs in this category are cyclooxygenase inhibitors and acetaminophen.
Cyclooxygenase Inhibitors
Cyclooxygenase inhibitors are mainly subdivided into nonsteroidal anti-inflammatory drugs and aspirin. Cyclooxygenase, or COX, is an enzyme in the pathway to synthesize prostaglandin, a key inflammatory hormone-like substance, from arachidonic acid. When produced, prostaglandins have several different effects on their target organs and are known to contribute to nociceptive pain.
There are two types of COX enzymes: COX-1 and COX-2. COX-1 is found primarily in the gastric mucosa, kidneys, and blood vessels. Inhibition of this enzyme is believed to contribute to renal toxicity and gastrointestinal effects. COX-2 enzymes are activated by the processes causing pain, fever, and inflammation [29].
Selective COX-2 inhibitors were introduced as an alternative to non-selective COX-1/COX-2 inhibitors to reduce the gastric side effects linked to COX-1 inhibition. However, the drugs were quickly linked with some potentially serious cardiovascular safety concerns, including myocardial infarction, cerebrovascular accident, and other thromboembolic diseases. Most of these medications were removed from the market, and the FDA recommended limiting the use of celecoxib (Celebrex), the remaining selective COX-2 inhibitor [29].
Salicylates, like aspirin, are non-selective COX inhibitors, and they also inhibit platelet aggregation, block pain impulses, and may act on the hypothalamus to reduce fever and pain. The table below shows selected medications belonging to the COX inhibitor class of drugs [29].
Non-Opioid Analgesics
Non-opioid analgesics can be used to treat mild to moderate pain and are often combined with opioid pain relievers to enhance their effectiveness. The two main types of drugs in this category are cyclooxygenase inhibitors and acetaminophen.
Cyclooxygenase Inhibitors
Cyclooxygenase inhibitors are mostly made up of nonsteroidal anti-inflammatory drugs and aspirin. Cyclooxygenase, or COX, is an enzyme in the pathway to synthesize prostaglandin, a key inflammatory hormone-like substance, from arachidonic acid. When produced, prostaglandins have several different effects on their target organs and are known to contribute to nociceptic pain.
There are two types of COX enzymes: COX-1 and COX-2. COX-1 is found primarily on the gastric mucosa, kidneys, and blood vessels. Inhibition of this enzyme is believed to contribute to renal toxicity and gastrointestinal effects. COX-2 enzymes are activated by the processes causing pain, fever, and inflammation.
Selective COX-2 inhibitors were introduced as an alternative to non-selective COX-1/COX-2 inhibitors with the goal of reducing the gastric side effects linked to COX-1 inhibition. However, the drugs were quickly linked with some potentially serious cardiovascular safety concerns, including myocardial infarction, cerebrovascular accident, and other thromboembolic diseases (14). Most of these medications were removed from the market, and the FDA recommended limiting the use of celecoxib (Celebrex), the remaining selective COX-2 inhibitor.
Salicylates, like aspirin, are non-selective COX inhibitors, and they also inhibit platelet aggregation, block pain impulses, and may act on the hypothalamus to reduce fever and pain. The table below shows selected medications belonging to the COX inhibitor class of drugs.
| Properties of Selected Cyclooxygenase Inhibitor Drugs | ||||
| Drug | Class | Adult Dosage | Indications | Adverse Effects |
| Acetylsalicylic Acid (Aspirin) |
Salicylates | 650mg q4-6h |
|
|
| Ibuprofen (Motrin, Advil) |
Propionic Acid Inhibitor and Non-selective inhibitor of COX-1 and COX-2 | 400-800mg q6-8h |
|
|
| Celecoxib (Celebrex) |
Selective COX-2 inhibitor | 100-200mg once or twice daily |
|
|
| Diclofenac (Voltaren, Cataflam) |
Acetic acid derivative | 50mg 3-4 times a day |
|
|
| Ketorolac (Toradol) |
Acetic acid derivative |
15-30mg IV/IM q6h 10mg PO q4-6h |
|
|
| Naproxen (Naprosyn, Aleve) |
Propionic Acid Inhibitor and Non-selective inhibitor of COX-1 and COX-2 | 250-500mg PO twice daily |
|
|
[29]
Acetaminophen
Acetaminophen is thought to inhibit prostaglandin synthesis in the central nervous system. It also reduces fever and inflammation, though less effectively than the COX inhibitors. It is used to treat mild to moderate pain and can also be used as a fever reducer. Dosing in children depends on their age and weight, but in adults, the dose is typically 650mg q4 hours or 1,000mg q6 hours, with the maximum daily dose not exceeding 4g per day. Patients with a history of liver failure should not exceed 2g per day [13].
Acetaminophen is metabolized in the liver, but larger doses can cause the accumulation of a hepatotoxic metabolite that can build up and cause liver damage. Hepatotoxicity is the primary adverse effect of acetaminophen, and the nurse should carefully counsel patients to be aware of hidden sources of the drug in cold medicine and other combination products [13].
Acetaminophen overdose is a medical emergency and is often fatal secondary to hepatotoxicity. There are four phases of acetaminophen overdose:
- Phase 1 – Occurs within the first 2 to 24 hours after ingestion.
-
- The patient experiences symptoms such as nausea, vomiting, sweating, abdominal pain, and diarrhea.
- Phase 2 – Occurs 24 to 72 hours after ingestion.
-
- The patient may be feeling better, though right upper abdominal pain often persists. Serum liver enzymes, bilirubin, and prothrombin time begin to rise.
- Phase 3 – Occurs 72 to 96 hours after ingestion.
-
- Symptoms begin to reappear, including nausea/vomiting, jaundice, confusion, and coma. Even more dramatic rises in liver enzymes and other markers will be present.
- Phase 4 – Occurs 6 to 7 days after ingestion.
-
- Liver enzymes begin to trend back towards normal and hepatic damage may begin to resolve. However, depending on the amount of acetaminophen ingested, the treatment, and the extent of liver damage that occurs, full hepatic failure and death are possible.
The treatment for acetaminophen overdose includes gastric lavage, administration of activated charcoal, and acetylcysteine every 4 hours (started within the first 8 hours after ingestion) for 18 doses. Acetylcysteine interferes with the formation of hepatotoxic metabolites. In addition to administering medication and providing supportive care, the nurse will need to follow plasma acetaminophen levels [13].

Self Quiz
Ask yourself...
- Why is there an increased risk of gastric ulcer in people taking COX inhibitors?
- What side effects are associated with the use of acetylsalicylic acid?
- What NSAID would be most appropriate for a patient with rheumatoid arthritis pain?
- What medication would the nurse recommend for a patient with menstrual cramps?
- What provider orders would the nurse anticipate for a patient with a suspected acetaminophen overdose?
Opioid Pain Management
Opioid pain relievers are a nursing intervention for acute pain that is usually reserved for cases of severe pain, such as cancer or post-surgical pain, or moderate pain that is not well-controlled with other types of drugs. This class of medication acts directly on receptors in the central nervous system in a few different ways: they block transmission of nociception from the peripheral nerves to the spinal cord, change the activity of the limbic system in the brain, and modulate the descending inhibitory pathways in the spinal column to prevent transmission of pain signals.
There are three types of opioid receptors: mu, kappa, and delta, and drugs are classified based on their response to these receptors.
- Pure Agonists bind directly to mu receptors to relieve pain
- Partial Agonists work similarly to pure agonists but don't produce the same full response as pure agonists. As the dosage gets higher, the analgesic effect will not increase, but the potential for side effects does.
- Mixed Agonists- Antagonists act as an agonist to produce analgesia at the kappa receptors but as an antagonist at the mu receptors.
- Antagonists bind to receptors and competitively block other opioids from binding there.
Morphine sulfate is the prototype opioid prescribed for pain and the drug against which the other opioids are compared. It is the drug of choice for cancer patients and is often used for other types of moderate to severe pain. In addition to producing analgesia, morphine has several other clinically useful effects, including reduction of the emotional response to pain, suppression of the cough reflex, reduction of cardiac workload, and reduction of anxiety. Because of this, morphine is an effective nursing intervention for acute pain management [7, 14].
In addition to morphine, there are many other options for opioid pain relievers. The table below shows some common drugs in this class of medication.
| Properties of Selected Opioid Pain Relievers | |||
| Pure Opioid Agonists | |||
| Drug | Indication | Administration | Nursing Considerations |
| Morphine (Roxanol, MS Contin, Astromorph, Kadian, Avinza) |
Moderate to severe pain Chronic cancer pain Used for its analgesic, anxiolytic and hemodynamic functions during a myocardial infarction Used in palliative care to treat pulmonary edema |
Can be administered IV, IM, SC, or PO Exhibits a first-pass effect with oral administration, meaning that this route requires a higher dose When administered IV, onset of action is 5-10 minutes IV dose: 2.5-10mg q2-3h PO dose: 10-30mg q3h |
Use cautiously with older adults Can accumulate with repeated dosing in patients with renal failure. Can cause itching and respiratory depression in some patients. |
| Codeine (Tylenol #2, #3, or #4) |
Mild to moderate pain Also effective as an antitussive (cough suppressant) and anti-diarrheal
|
Available in parenteral form, but most commonly given orally as: Tylenol #2 (15mg of codeine + 300mg acetaminophen) Tylenol #3 (30mg of codeine + 300mg acetaminophen) Tylenol #4 (60mg of codeine + 300mg acetaminophen) |
Associated with a higher incidence of constipation than other opioids. Nurse must counsel patients taking combination products to watch their daily total acetaminophen intake. |
|
Hydrocordone
|
Treats moderate to severe pain |
Not available in intravenous form. Most commonly administered as a combination product with either acetaminophen or ibuprofen. Dose ranges between 2.5-10mg q6h |
Nurse must counsel patients taking combination products to watch their daily total acetaminophen intake.
|
|
Oxycodone
|
Used to treat moderate to severe pain |
Oxycodone is only available as an oral medication. Pure oxycodone (oxycontin) is available as an extended-release drug and should be given every 12 hours. More commonly administered in combination with acetaminophen, aspirin, or ibuprofen. |
Higher risk of abuse due to increased euphoria associated with the crushed form of this drug. Nurse must counsel patients taking combination products to watch their daily total acetaminophen intake. |
| Hydromorphone (Dilaudid) |
Moderate to severe pain Also has antitussive effects |
Can be given PO, IV, IM, SC, and PR. Has a faster onset but a shorter duration of action than morphine. |
Adverse effects are similar to morphine but with a shorter duration of activity. |
| Fentanyl (Sublimaze, Duragesic) |
The parenteral form is used in the pre-operative or immediate post-operative setting. Transdermal system used to treat chronic pain. |
Patches are available as 25, 50, 75 or 100mcg/hr dosing. Patches are usually changed every 3 days. Very potent drug with a quick onset of action when used parenterally. |
Patients using the transdermal patches may require breakthrough pain relief until the medication becomes effective. High potential for abuse; nurse must check the patch at least once per shift to ensure that it is in place and intact. Clean the skin with soap and water before applying the patch. Do not apply the patch over lotion, alcohol, hair, or oils on the skin. Wear gloves when applying or removing a patch. Site should be changed each time that it is applied |
| Meperidine (Demerol) |
Used short-term for acute pain in younger patients
|
Available with both oral and parenteral dosing. PO dose: 150-300mg PV dose: 25-100mg |
Should not be used in patients taking MAOI's due to risk of life-threatening hypertension.
|
| Levorphanol (Levo-Dromoran) |
Used for moderate to severe pain |
Available as PO, IV, IM and SC dosing. Has a long half-life of 11-16 hours, which can increase the risk of drug accumulation if dosing is set too high or too frequently. |
Not frequently used due to risk of drug accumulation and overdose. |
| Methadone (Dolophine, Methadose) |
Primarily used for detoxification of patients with opioid addiction. Occasionally used for chronic pain management |
Can be administered orally or intramuscularly. Long half-life leads to an increased risk of accumulation, adverse effects, and overdose. |
Adverse effects are similar to morphine. When used for opioid detoxification or maintenance, access is limited to licensed methadone clinics. |
| Partial Agonists | |||
| Drug | Indication | Administration | Nursing Considerations |
| Buprenorphine (Buprenex) |
Rarely used, but can be prescribed to treat moderate to severe pain |
Available in parenteral and sublingual forms Extensive first pass metabolism with oral dosing |
Not appropriate for patients with opioid dependence or who have been treated for chronic pain. Overdose is not readily treated with naloxone; treatment is respiratory support as needed. |
| Buprenorphine + Naloxone (Suboxone) |
Can be used for withdrawal or as maintenance during opioid detoxification | Film that can be administered sublingually or buccally. |
Can precipitate opioid withdrawal
|
| Mixed Agonists-Antagonists | |||
| Drug | Indication | Administration | Nursing Considerations |
| Butorphanol (Stadol) |
Used for moderate to severe pain Can be used as an adjunct to anesthesia |
Available for parenteral dosing or as a nasal spray. |
Can worsen hypertension in patients with pre-existing high blood pressure
|
| Antagonists | |||
| Drug | Indication | Administration | Nursing Considerations |
| Naloxone (Narcan) |
Used to reverse the respiratory and central nervous system effects of acute opioid intoxication or overdose |
Parenteral dosing (IV or IM) only Rapid onset of action 0.4-2mg mas a single injectable dose |
Repeated injections or continuous infusion may be needed to reverse the full effects of opioids due to short half-life |
[7, 14]
Opioid medications do carry the risk of some serious side effects, which the nurse must monitor for. Potential side effects include [7]:
- Constipation
- Itching
- Respiratory depression
- Vertigo/lightheadedness
- Confusion
- Nausea/vomiting
- Hypotension
Due to their similar nature, many of the opioids produce similar effects to varying degrees. However, opioid antagonists are the exception and cause very different side effects, which can include [26].
- Nausea/vomiting
- Hypertension
- Dizziness
- Abdominal pain
- Insomnia
- Weakness
- Headache
- Muscle pain
There is also a risk of allergy, which can occur with any of the major opioid drugs, including morphine. The nurse must be especially careful of this risk and other adverse effects when administering opioids to an opioid-naïve patient.


Self Quiz
Ask yourself...
- Which action would the nurse take if respiratory depression secondary to morphine is suspected?
- What signs and symptoms might suggest a morphine allergy?
- Why would Buprenex not be a good option for a patient with an opioid addiction?
- Meperidine should not be given to patients taking which medication due to the risk of hypertension?
- When considering opioids as one of the nursing interventions for acute pain, what factors should you consider?
Adjunct Analgesics
Adjunct or adjuvant drugs are the final type of medications that are used for analgesia. These drugs are often combined with analgesics to enhance pain relief. Sometimes, these drugs are used on their own to manage specific types of pain. There are many different types of adjuvants, depending on the patient's needs and clinical situation [2].
Corticosteroids
Corticosteroids are primarily used to manage acute and chronic cancer pain, pain due to spinal compression, and pain affecting the musculoskeletal system. Though the exact mechanism is unknown, corticosteroids are known to reduce swelling, inflammation, and edema. However, corticosteroids do cause some serious side effects, including hyperglycemia, increased susceptibility to infection, reduced immune system function, and suppression of adrenal function. Dexamethasone, prednisone, and methylprednisolone are the three most prescribed corticosteroids. Corticosteroid injections are one of the most common nursing interventions for acute pain management of arthritis and joint pain.
Antidepressants
A class of antidepressants, known as tricyclic antidepressants (TCAs) can be used with opioid or non-opioid pain relievers to help relieve pain. They are most effective for neuropathic pain and may work by increasing the levels of serotonin and norepinephrine in the synaptic cleft, preventing the transmission of pain signals. Doses for TCAs tend to be lower when used to treat pain than the dose used to manage depression. The most common side effects are weight gain, loss of sexual desire, dry mouth, orthostatic hypotension, and urinary retention.
Antiepileptic Drugs
Antiepileptic or antiseizure drugs affect the central nervous system in several different ways that can reduce neuropathic pain. They modulate amino acids and neurotransmitters in a way that reduces the transmission of pain signals between the periphery and central nervous system. These drugs tend to be used for chronic pain disorders, such as diabetic neuropathy and fibromyalgia.
Antihistamines
Some antihistamines, particularly hydroxyzine, have been found to have analgesic, anxiolytic, and sedative properties that can be useful in patients with acute or chronic pain.
Local Anesthetics
Local anesthetics are a great option for well-localized pain, usually in the skin or superficial structures. Topical EMLA creams work well to minimize the pain due to venipuncture, intravenous line insertion, or other simple procedures. Lidocaine or prilocaine can be injected into the tissue to help with pain associated with invasive procedures, while patches can be used to manage post-herpetic lesions and neuropathies.
Alpha-2 Adrenergic Agonists
Alpha-2 adrenergic agonists may decrease the release of peripheral norepinephrine and work on the central alpha-2 adrenergic receptors, both of which may help to reduce chronic headache and neuropathic pain. The drugs from this class that are most commonly prescribed for pain are clonidine and zanidine. Side effects are mild, but may include dry mouth, orthostatic hypotension, and sedation.
GABA Receptor Agonists
More commonly known as muscle relaxants, GABA receptor agonists work best on neuropathic pain and muscle spasms. These drugs block the transmission of pain impulses and can decrease spasticity.
It may take time and trial and error to find a regimen that works. The nurse's role in the assessment and evaluation of different nursing interventions for acute pain plays a crucial role in helping patients be as comfortable as possible. Most importantly, the nurse must advocate for patients who are struggling with pain management in the acute care setting.

Self Quiz
Ask yourself...
- Which adjuvant would the nurse anticipate for a patient with chronic headaches?
- How do corticosteroids help to reduce pain?
- How would a nurse counsel a patient in pain about a new prescription for an antidepressant?
- Were you aware that antidepressants are used as one of the nursing interventions for acute pain?
Nursing Care of Patients Receiving Analgesia
The nursing care plan is an invaluable tool when caring for a patient with acute pain.
Assessment
The nurse should start with an assessment, as described earlier in this module. For a new complaint of pain, the nurse should perform a more comprehensive assessment: determine if there are other symptoms, ask about the characteristics of their pain (PQRSTU questions), and perform a physical examination as needed [9,21].
When caring for someone with known or expected pain, such as a post-surgical patient or after a broken ankle, the assessment could be more focused on the patient's current pain level. Even in these situations, you should continue to perform a complete assessment at least once per shift or according to your institutional policies.
Report any new or unexpected complaints of pain or abnormal assessment findings to the provider and document them in the patient's chart.
Identifying Goals and Planning
Based on the data identified during the assessment, the nurse will formulate goals and objectives to meet the patient's needs. The primary goal for someone with acute pain is relief from that pain, but there may be other goals that are also appropriate. They may include [9,21]:
- Improved physical mobility
- Improved self-care
- Decreased anxiety
- Improved rest and sleep
- Relief from analgesic side effects
Creating a concept map can be a useful tool for identifying potential problem statements and their relationships, as pain is often interrelated with other health problems.
Once goals are set, it is important to establish criteria against which the goals are measured. For example, you may identify that your patient will have a tolerable amount of pain upon discharge from the hospital. Your expected outcome may be that their pain level is consistently reported to be at a 4 or below.
A comprehensive pain management plan must consider the entire interdisciplinary care team. Did the medical provider enter orders for pain management medications? Are they appropriate? (For example, a simple acetaminophen order after a surgical procedure may not be sufficient to deal with post-surgical pain). Is the physical therapist planning to start mobility exercises to get the patient back on their feet? Does the patient want to speak with a clergy member to help focus on spiritual health? Is a pain management specialist needed? Having the appropriate team members in place makes it more likely that the patient will achieve the planned outcomes.
Implementation
Depending on the extent of the patient's pain, you'll use your nursing judgment to select and implement nursing interventions for acute pain to address it. For mild pain, non-pharmacological measures may suffice; for severe pain, regular administration of opioid pain relievers (as ordered) may be the best course of action. For these patients, it is important to stick with the scheduled doses as closely as possible because the pain becomes much harder to treat once it becomes severe.
Once the patient's pain is under control, it is important to begin teaching and involving the patient in their care. The nurse should teach the patient non-pharmacological comfort measures, wellness strategies, and what to expect during the healing period. This information helps the patient become more capable of caring for themselves and promotes both physical and emotional healing.
Evaluation
Remember those expected outcome statements you created earlier in the planning stage? Well, now is when you'll put them to use by comparing those expected outcomes to the actual outcomes experienced by the patient. The best way to evaluate patient outcomes is to ask the patient themself. Key questions could include:
- Are you still having pain?
- What is your current pain level?
- Have you experienced any side effects from your treatment?
- How is your pain limiting your ability to function or perform your activities of daily living?
- How is the treatment affecting your ability to perform activities of daily living?
- Are you able to rest?
- Are you able to eat comfortably?
- And any other questions that could apply to the patient's specific problem statement.
If the patient is unable to communicate, the family could also be a useful source of information. It is important for the nurse to explicitly ask these questions: some patients may not readily volunteer this information or be afraid to mention that they are still in pain or having side effects.
In addition to speaking with the patient (or family) directly, objective data can also provide useful information, particularly about potential side effects, such as oversedation or respiratory depression. The nurse should collect data, such as [9,21]:
- Vital signs
- Level of consciousness
- Sedation
- Oxygen saturation
If the data suggests that the patient's pain is under control and there are no bothersome side effects, then great! In this situation, you'll continue to care for the patient according to the care plan and periodically evaluate the patient to ensure continued success.
If, however, the patient is still experiencing unacceptable amounts of pain or having side effects (whether they are dangerous or just uncomfortable), then the nurse will need to immediately make changes to the plan. This may include administering a second dose of medication, speaking to the provider about adding additional pain medication, adding alternative methods of pain management, discontinuing a medication that is causing side effects, and obtaining an order for a different option.
The nurse must continue to check in with the patient and provide reassurance and education about pain management. For example, if the patient complains that intravenous pain medication is not working 5 minutes after administration, the nurse should reassure the patient that the medication will have peak effectiveness at about 15 to 30 minutes, and they'll check back then.


Self Quiz
Ask yourself...
- How would the nurse document the pain assessment and evaluation for a patient receiving pain medication?
- What would the nurse do first when a patient complains that the IV morphine administered for post-operative pain control is not effective 45 minutes after administration?
- What action would the nurse take first if a patient is found to have a respiratory rate of 6 bpm at 1 hour after IVPB morphine administration?
- Which information would the nurse include when teaching a patient about their pain medication?
Nursing Interventions for Acute Pain in Special Populations
Pain management strategies may need to be adjusted when caring for certain populations. Three populations that will always need special consideration are infants and children, older adults, and people with a history of addiction.
Infants and Children
While the process is the same as with adult patients, assessment tools and treatments must be modified to work for the developmental ages of the young kids they are caring for. Pain scales like the FACES, FLACC, and other scales specifically designed for use in pediatric patients should be used when assessing for pain, and the nurse can also rely on input from the parents [9, 21, 30]. As discussed earlier, these scales rely on the nurse's observations of the child to determine pain level, rather than asking the child to describe their pain, which they may not be able to do.
Older children and adolescents are more likely to be able to verbalize their pain, making it more appropriate for the nurse to ask these kids directly.
When administering pain medication to children, especially infants or very young children, the nurse must be extremely careful when drawing up and administering intravenous medications. Some institutions may even require that a second nurse be present to review the order, medication label, prepared medication, and patient ID band before a narcotic is administered. Frequent assessments should be performed to reduce the risk of serious adverse reactions.
Older Adults
Age-related changes can influence not only a patient's experience of pain but also how they metabolize pain medication. Older adults are more likely to have multiple health conditions, which can make the assessment process a bit more confusing. This would require the nurse to perform a more in-depth or comprehensive assessment to determine the source and type of pain that a patient is experiencing. In addition, the nurse must take a careful medication history, as they are at higher risk for side effects and drug interactions. Other factors that could increase a person's risk for adverse effects include [10.:
- Slowing of gastrointestinal function that slows the absorption rate of medications
- Decreased renal or hepatic function
- Decreased muscle, fat, and bone mass, which can lead to a higher risk of overdose
- Poor nutrition causes decreased albumin levels, which may be an issue with protein-bound drugs
- Thinner skin, which can impact the absorption of topical medications
The nurse must be careful to take these factors into account when administering narcotics or other pain medications to an older adult and monitor them closely for side effects, adverse reactions, or drug interactions.
In addition, older adults may be more likely to have cognitive impairments, like Alzheimer's disease or dementia, which could impact their ability to accurately communicate or report their pain. Again, the nurse must be aware of these limitations and use the appropriate tools when working with this patient population [10].
Safety is a major concern for this population as well, particularly when administering medications that can increase drowsiness, dizziness, or the risk of falling. The nurse must be careful to check on the patient frequently, assist with ambulation, and place the call bell or other needed items within easy reach of the patient.
People with a History of Addiction or Substance/Opioid Use Disorder
People with a history of addiction pose a unique challenge to the implementation of pain management strategies. Patients in recovery are often concerned about the risk of relapse, whether they are addicted to opioids, alcohol, or other substances. And patients who are actively using it may be concerned about withdrawal while being in the hospital, or even whether their pain will be taken seriously given their history.
Healthcare providers may also struggle with providing opioids for patients with a history of substance abuse: they may be worried about the diversion or overtreatment of pain or be distrustful of a patient's report of pain [23].
When treating opioid-dependent patients with narcotics for pain, they will likely need higher doses to achieve pain relief. The nurse must carefully monitor patients in this situation due to the risk of toxicity. The addition of adjuvants may also be particularly useful in this population.
Patients who refuse opioid treatment due to the risk of relapse should be respected; this may mean finding other viable alternatives, such as non-opioid adjuvants, local or regional medications (like an epidural or spinal block), and non-pharmacological methods of pain relief.


Self Quiz
Ask yourself...
- Which pain assessment tool would the nurse use for a newborn infant?
- What measures would the nurse implement for an older adult who is at high risk of falling due to the use of opioid narcotics?
- What tool(s) would the nurse use to assess pain in an elderly adult with dementia?
- Which opioid(s) are contraindicated in patients with a history of substance abuse?
- Can you think of any other patient population who might need special considerations when determining appropriate nursing interventions for acute pain?
Conclusion
Nurses should be knowledgeable about pain management techniques. left untreated, pain can lead to depression, anxiety, reduced healing, non-compliance with medical treatment, longer hospital stays, poor quality of life, and even reduced patient satisfaction with the healthcare facility. However, treating pain is not simple. It is a complex phenomenon that is experienced differently by everyone and influenced by many different factors.
The nurse plays a vital role in identifying patients with unrelieved pain and advocating for better pain management strategies.
A-fib and Stroke Risk
Introduction
In 2023, stroke was the third leading cause of death in the United States after heart disease and cancer (1). As the life expectancy of the average American is approximately 76 years (2), an increasing number of people will live with comorbid health conditions compared with prior generations. One risk factor for stroke, apart from high blood pressure, is atrial fibrillation (also known as AFib or AF), which causes approximately 15% of strokes (3). Furthermore, people living with AFib are up to five times more likely to have a stroke than those without this condition (4). Nurses are critical providers of education and information to patients about their risk of AFib and stroke. They can elucidate a deadly subject to help patients reduce their risk of morbidity and mortality.
Pathophysiology of A-Fib and Stroke
Atrial fibrillation, the most common arrhythmia, is due to rapid or disordered electrical signals in the heart's upper chambers (the atria). These impaired signals cause the atria to contract too chaotically and quickly, termed fibrillation. AFib causes blood to pool in the atria and increases the risk of blood clots, stroke, and heart disease (15).
Since AFib can exist in asymptomatic patients, estimates of its prevalence vary between 3 to 6 million Americans, with 12 million patients affected by the year 2030 (15). Worldwide, that number is estimated at over 33 million, or approximately 0.5% of the planet’s population, though numbers are likely far higher due to the underdiagnosing of the condition (15). Within the United States, AFib is directly linked to nearly 160,000 deaths per year (15, 16). Part of the reason AFib is so deadly is that 1 in 7 strokes are caused by this condition (16).
Strokes occur when blood vessels in the brain rupture (hemorrhagic) or are blocked by a clot (ischemic). These incidents reduce blood flow to the brain, affecting the transport of essential elements like oxygen and nutrients for cell survival. Ischemic strokes occur in approximately 87% of cases (5).
Strokes originating from cardiac factors like AFib are known as cardioembolic; AFib is one of the major causes of cardioembolic strokes (6). Approximately 20-25% of ischemic strokes are cardioembolic in nature, their incidence increasing with age (6,8). A cardioembolic stroke occurs when blood clots or emboli travel from the heart or aorta and lodge in the cerebral circulation, causing ischemia. The risks of both AFib and stroke grow with age, and when the two conditions occur together, the results of the stroke are usually more severe and deadly (7, 8, 15).
While AFib is the highest contributor to cardioembolic stroke, other causes include sick sinus syndrome, structural diseases (like patent foramen ovale), valvular heart disease (such as infective endocarditis and valvular calcifications), septal or ventricular aneurysms, heart failure with reduced ejection fraction (HFREF), and myocardial infarction (MI) (6).
The course of illness depends on the severity of the stroke, pre-existing conditions, age, and any other complications present. Stroke generally presents rapidly and is a medical emergency. Most hospitals require patient education regarding stroke signs, symptoms, and management, such as when to call for EMS promptly.

Self Quiz
Ask yourself...
- Have you ever had a patient/client who had difficulties maintaining anticoagulation regimens and lab follow-up? Did they ever present with clotting disorders such as DVT, PE, or Stroke?
- TEE and/or Echocardiogram exams are often ordered by practitioners for patients in A-Fib. If a thrombus was found within the heart's upper chambers, would this be a critical result to be reported immediately? What treatment can you anticipate?
Risk Factors for A-Fib and Stroke
In general, the risk factors of cardioembolic stroke overlap with the general risk factors for stroke and include hypertension, diabetes mellitus, hyperlipidemia, cardiac diseases, and lifestyle factors. When educating patients with AFib about their risk of developing a stroke, numerous risk factors may be considered for teaching opportunities.
The following chart shows modifiable versus non-modifiable risk factors for AFib that lead to stroke (9,10,11,15):
| Modifiable | Non-Modifiable |
| Hypertension | Age (older than 65 years) |
| Hypercholesterolemia | Race (higher risk of AFib for those of European descent; higher risk of stroke fr African Americans) |
| Rheumatic heart disease or pericarditis |
Sickle Cell Anemia |
| Metabolism Syndrome, Diabetes Mellitus, Hyperthyroidism | Prior stroke, TIA, or MI |
| Poor diet |
History of migraine headaches |
| Heart Disease (A-fib, valve disease, prosthetic valve, mitral stenosis) | Sex (men have a higher risk of AFib; women for stroke) |
| Excessive alcohol or caffeine consumption alcohol | Family History |
| Smoking or other tobacco use |
|
| Sleep apnea |
|
| Obesity | |
| Physical inactivity | |
| Carotid or peripheral artery disease |
|
| Athleticism (higher incidence of SVT, which can lead to AFib) | |
| Lung or Kidney Disease | |
| High-stress levels or mental health conditions |
The clinical team must work with the patients and families to identify the specific risk factors for each patient to reduce the risk of stroke.

Self Quiz
Ask yourself...
- Do any of these risk factors surprise you?
- Are patients always aware or forthright regarding their risk factors?
CHADs and Stroke Risk Scoring in A-Fib
Cardiologists and other clinicians use a scoring system to evaluate the stroke risk for those with atrial fibrillation. The CHADS2 score was first published in 2001 and stands for Congestive heart failure, Hypertension, Age ≥75 years, and Stroke [Double weight] (12). Its goal is to predict the risk of stroke in patients with nonrheumatic AFib, and the score assists practitioners in making anticoagulation decisions (12).
Patients with high scores (>2) are at significant risk for stroke: They have a 5.9% annual risk with a score of 3 and as high as an 18.2% yearly risk for those with a score of 6 (12). The CHADS2 did not include some additional risk factors for stroke. It was revised to the CHA2DS2-VASc, which contains three more risk factors: vascular diseases (e.g., coronary artery disease and aortic atherosclerosis), age (65-74 years old), and female sex (12). See tables below (12).
CHADS2 Score: Stroke Risk Assessment in Atrial Fibrillation: (4)
| Score | CHADS2 Risk Criteria |
| 1 point | Congestive heart failure |
| 1 point | Hypertension |
| 1 point | Age ≥ 75 years |
| 1 point | Diabetes mellitus |
| 2 points | Stroke/transient ischemic attack |
CHADS2 Score and Corresponding Annual Stroke Risk: (4)
| CHADS2 Score | Adjusted Stroke Risk (%) |
| 0 | 1.9 |
| 1 | 2.8 |
| 2 | 4 |
| 3 | 5.9 |
| 4 | 8.5 |
| 5 | 12.5 |
| 6 | 18.2 |
CHA2DS2-VASc Score and Risk Criteria: (4)
| Score | CHA2DS2-VASc Risk Criteria |
| 1 point | Congestive heart failure |
| 1 point | Hypertension |
| 2 points | Age ≥75 years |
| 1 point | Diabetes mellitus |
| 2 points | Stroke/Transient Ischemic Attack/Thromboembolic event |
| 1 point | Vascular disease (prior MI, PAD, or aortic plaque) |
| 1 point | Age 65 to 74 years |
| 1 point | Sex category (i.e., female sex) |
The American Heart Association/ American College of Cardiology/ Heart Rhythm Society (AHA/ACC/HRS) considers recommending oral anticoagulants to patients who have a CHA2DS2-VASc score of 1; at a score of 2 or higher; the recommendation is certain (14).

Self Quiz
Ask yourself...
- Would explaining the risk for stroke CHADS2 scoring system to patients and families assist them in making decisions about anticoagulants?
- What are the common concerns that patients and families have regarding taking "blood thinners"?
Case Study
John, a 76-year-old Caucasian male patient, presents to the ED with cellulitis, intermittent heart palpitations, and shortness of breath. He has a history of diabetes mellitus and peripheral arterial disease with right-toe amputation. John quit smoking two years ago after a 60-pack-year history. His vital signs upon presentation are Temp: 38.1°C, HR 130, BP 150/88, RR 16, SpO2 94% on room air. His ECG rhythm reads atrial fibrillation, and he states he had never been told he had this condition before.
He did not want to come to the hospital, but his wife Sally insisted since his cellulitis wounds started spreading and weeping. Sally states that John has seemed tired and irritable lately and has endorsed some new-onset lightheadedness and shortness of breath at rest. He is treated with broad-spectrum IV antibiotics and moderate-rate fluid replacement. Cardiology was called to evaluate the AFib.

Self Quiz
Ask yourself...
- Using the CHA2DS2-VASc risk scoring system what would his score be?
- Would he qualify for oral anticoagulants?
- Would IV heparin infusion be considered in his case?
Oral Anticoagulants in A-Fib and Stroke Reduction
Patients with AFib-induced stroke will have an anticoagulation regimen prescribed, likely along with other treatments, whether newer or traditional; anticoagulants on the market can be confusing and difficult for patients to differentiate when evaluating risks and benefits.
There are many oral anticoagulants available now, each with its unique properties. If warfarin (Coumadin) is used, the INR goal is generally around 2.5. However, there are situations, especially in the over-75 age group, where a lower INR goal of 2.0 is acceptable (13). Warfarin has an onset of 36-48 hours and can last in the system for 2-5 days, delaying any surgical procedures. Other oral anticoagulants for atrial fibrillation include apixaban (Eliquis), dabigatran (Pradaxa), edoxaban (Savaysa), and rivaroxaban (Xarelto). Each has a unique drug profile, half-life, and reversal agent.
For those unable to take anticoagulants and at risk for atrial thrombus (which can form in the left atrial appendage due to reduced contractility during AFib), a device called the Watchman has been created. It is a tent-like device surgically placed in the left atrial appendage to seal it off. Since more than 90% of stroke-causing clots come from the left atrial appendage in nonvalvular AFib, the Watchman aims to significantly reduce the risk of clots at that site (13). The outpouching of the sac is seen protruding from the left atrium in the diagram below (13).
Other treatments for AFib include lifestyle changes, medicines, surgery, and other procedures that aim to slow and restore the heart's regular rhythm and help prevent blood clots (15). In addition to the oral anticoagulants listed above, other medications may include beta-blockers (e.g., atenolol and metoprolol), calcium channel blockers (e.g., diltiazem and verapamil), and digoxin (15). If those treatments fail to treat the AFib effectively, other medications like amiodarone, dofetilide (Tikosyn), flecainide, procainamide, and others may be given, but they all require careful monitoring and dosing (15). Surgical and procedural treatments generally include electrical cardioversion, AV node ablation, and implanted pacemakers (15).
Ways to prevent the risk of stroke in people with AFib include, but are not limited to (15):
- Controlling blood pressure, cholesterol and triglyceride levels, and weight
- Taking all medications as prescribed and informing the primary care provider of any other drugs or herbal supplements used
- Eating a diet low in saturated and trans fats and high in fruits, vegetables, and whole grains
- Getting daily exercise of at least 30 minutes
- Quitting smoking and reducing alcohol and caffeine consumption
- Maintaining overall health by scheduling regular physical examinations
- Monitoring and treating other comorbidities
- Reporting all instances of dyspnea or angina immediately to a physician
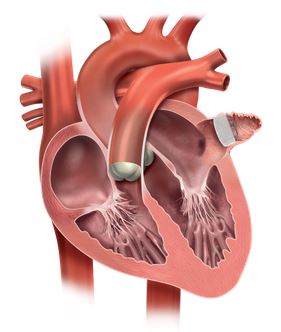
Conclusion
By the nature of atrial fibrillation, all patients with this condition have risk factors for stroke. The clinical team's responsibility is to assess each patient’s unique risk and then educate them in making decisions regarding stroke prevention. The risk of stroke from atrial fibrillation is a genuine concern as the population ages, and the number of patients diagnosed with these comorbid conditions is on the rise.
For patients presenting with ischemic stroke, the causal factors must be investigated to prevent stroke reoccurrence, which will likely include proper management of anticoagulants for atrial fibrillation. The nurse is responsible for providing information and resources for the patient to manage these conditions. As part of ongoing care, the nurse can also help reduce morbidity and mortality in patients who might otherwise succumb to AFib and stroke.
References + Disclaimer
Ethics for the Telehealth Nurse
- American Academy of Ambulatory Care Nursing (AAACN). (2018). Scope and standards of practice of professional telehealth nursing. Pitman NJ: Author.
- American Nurses Association, Code of Ethics for Nurses with Interpretive Statements (ANA, 2015). https://nurse.org/education/nursing-code-of-ethics/
- American Nurses Association, principles of connected health (ANA, 2019). https://www.nursingworld.org/~4a9307/globalassets/docs/ana/practice/ana-core-principles-on-connected-health.pdf
- Scope and Standards of Practice for Professional Telehealth Nursing – 6th Edition 2018
One Hour Sepsis Bundle
- McCulloh, R. J., & Opal, S. M. (2017). Sepsis, Septic Shock, and Multiple Organ Failure. In Lange Critical Care. Retrieved March 8, 2019, from https://accessmedicine.mhmedical.com/book.aspx?bookid=1944
- Marini, J. J., & Dries, D. J. (2019). Sepsis and Septic Shock. In Critical Care Medicine: The essentials and more(pp. 576-594). Philadelphia, PA: Lippincott Williams & Wilkins. Retrieved March 8, 2019, from http://ovidsp.dc1.ovid.com/
- Levy, M. M., Evans, L. E., & Rhodes, A. (2018). The Surviving Sepsis Campaign Bundle: 2018 update. Intensive Care Medicine,44(6), 925-928. doi:10.1007/s00134-018-5085-0
- Milano, P., Desai, S., Eiting, E., Hofmann, E., Lam, C., & Menchine, M. (2018). Sepsis Bundle Adherence Is Associated with Improved Survival in Severe Sepsis or Septic Shock. Western Journal of Emergency Medicine,19(5), 774-781. doi:10.5811/westjem.2018.7.37651
- Hour-1 Bundle. (n.d.). Retrieved March 11, 2019, from http://www.survivingsepsis.org/Bundles/Pages/default.aspx
- García-López, L., Grau-Cerrato, S., Frutos-Soto, A. D., Lamo, F. B., Cítores-Gónzalez, R., Diez-Gutierrez, F., . . . Andaluz-Ojeda, D. (2017). Impact of the implementation of a Sepsis Code hospital protocol in antibiotic prescription and clinical outcomes in an intensive care unit. Medicina Intensiva (English Edition),41(1), 12-20. doi:10.1016/j.medine.2017.02.001
Renal Failure Stages, Treatment, and Outcomes
- About Chronic Kidney Disease. (n.d.). Retrieved March 14, 2021, from https://www.kidney.org/
- Zhang, R., Liu, L., Yao, T., Shao, Y., Saredy, J., Sun, Y., . . . Saaoud, F. (2020). End-stage renal disease is different from chronic kidney disease in upregulating ROS-modulated proinflammatory secretome in PBMCs – A novel multiple-hit model for disease progression. Redox Biology, 34, 1-28. doi:DOI: 10.1016/j.redox.2020.101460
- Thrive-On Day 2 Facilitator Guide. (2021) v1.8 Retrieved March 19, 2021, from https://fmcna.sharpoint.com/sites/FKC-Education.
- NxStage Home Therapies (n.d.). Introducing the NxStage System One: An overview of a simple, flexible therapy option for home hemodialysis. Retrieved March 21, 2021, from https://ww3.nxstage.com.
- McAuslan, T. & Pask, T. (2019) Adopting palliative care in the dialysis unit…Canadian Association of Nephrology Nurses and Technicians Annual Conference , October 24-26, 2019, Edmonton, Alberta. CANNT Journal, 29(2). 30-31.
- Sauve, C., Vandyk, A., & Fothergill, B. (2016). The experience of individuals transitioning from incenter hemodialysis to home dialysis after a suboptimal start. CANNT Journal, 26(4). 11-17.
- National Institute of Diabetes and Digestive and Kidney Diseases (2021). Retrieved April 25, 2021, from https://www.niddk.nih.gov/health-information/health-statistics/kidney-disease.
Managing Conflict in a Nurse Leader Role
- Johansen, M. L. (2012, February). Keeping the peace: Conflict management strategies for nurse managers. Nursing Management, 43(2).
- Kahn, M.L. et al. (2013). The modes of conflicts and managerial leadership styles of managers. Global and Business Management: An International Journal, 7(2)
- Bell, J.A. (2013). Five generations in the nursing workforce. Journal for Nurses in Professional Development 29 (4) https://www.sgna.org/Portals/0/Bell_FiveGenerationsInTheNursingWorkforce_2013.pdf
- Andrea, S. (2018, December). Embracing generational diversity: Reducing and managing workplace conflict. ORNAC Journal, ().
- Gerardi, D. (2015). Perspectives on leadership. American Journal of Nursing, 115(3), 56-61.
- McKibben, L. (2017, January). Conflict management: Importance and implications. The British Journal of Nursing, 26(2), 100 -103. doi: 10.12968/bjon.2017.26.2.100
- Kiwanuka F, Nanyonga RC, SakDankosky N, Muwanguzi PA, Kvist T. Nursing leadership styles and their impact on intensive care unit quality measures: An integrative review. Journal of Nursing Management. 2021;29:133– 142. https://doi.org/10.1111/jonm.13151
- Sherman, R. O. (2017, February). Choosing your political battles. American Nurse Today, 12(2).
- Joint Commission Resources: 2011 Hospital Accreditation Standards. Oakbrook Terrace, Ill.: Joint Commission on Accreditation of Healthcare Organizations, 2011.
- American Nurses Association. Position Statement: Incivility, Bullying, and Workplace Violence. https://www.nursingworld.org/practice-policy/nursing-excellence/official-position-statements/id/incivility-bullying-and-workplace-violence/. Published July 22, 2015. Accessed March 2, 2019.
- Gerardi, D. (2015). Conflict Engagement. American Journal of Nursing, 115(5
- Gerardi, D. (2015, August). Conflict engagement: Emotional and social intelligence. American Journal of Nursing, 115(8), 60-65.
- Gerardi, D. (2015) Conflict engagement: Connection and cultivating curiosity. American Journal of Nursing. 115(9)
- Labrague LJ, Al Hamdan Z, McEnroe– Petitte D.M. An integrative review on conflict management styles among nursing professionals: implications for nursing management. Journal of Nursing Management. 2018;26:902–917. https://pubmed.ncbi.nlm.nih.gov/30155953/
Nursing Interventions for Acute Pain Management
- QSEN Institute. (n.d.). QSEN Competencies. Retrieved from https://qsen.org/competencies/pre-licensure-ksas/
- Germossa, G. N., Hellesø, R., & Sjetne, I. S. (2019). Hospitalized patients’ pain experiencee before and after the introduction of a nurse-based pain management programme: A separate sample pre and post study. BMC Nursing, 18(40). Doi: 10.1186/s12912-019-0362-y
- Gregory, J. & McGowan, L. (2016). An examination of the prevalence of acute pain for hospitalized adult patients: A systematic review. Journal of Clinical Nursing, 25(5-6). P. 583-598. https://doi.org/10.1111/jocn.13094.
- The Joint Commission. (2017). R3 Report: Pain assess and management standards for hospitals. Retrieved from https://www.jointcommission.org/-/media/tjc/documents/resources/patient-safety-topics/sentinel-event/r3_report_issue_11_pain_assessment_8_25_17_final.pdf?db=web&hash=938C24A464A5B8B5646C8E297C8936C1
- Al-Mahrezi, A. (2017). Towards effective pain management: Breaking the barriers. Oman Medical Journal, 32(5). 357- 358. Doi: 10.5001/omj.2017.69
- Huether, S. E., McCance, K. L. (2004). Understanding pathophysiology (3rd ed.). St. Louis, MO: Mosby. Pp. 330-335. ISBN 0-323-02368-1
- Hall, J. (2011). Guyton and Hall textbook of medical physiology (12th ed.). Philadelphia, PA: Saunders/Elsevier. P. 563-564. ISBN 978-1-4160-4574-8
- World Health Organization. (2016). International classification of diseases for mortality and morbidity statistics (10th Revision). Retrieved from https://icd.who.int/browse10/2016/en#/F45.4
- World Health Organization. (2018). International classification of diseases for mortality and morbidity statistics (11th Revision). Retrieved from https://icd.who.int/browse11/l-m/en#/http%3a%2f%2fid.who.int%2ficd%2fentity%2f767044268
- Merkel, S. I., Voepel-Lewis, T., Shayevitz, J. R., & Malviya, S. (1997). The FLACC: A behavioral scale for scoring postoperative pain in young children. Pediatric Nursing, 23(3). 293-297. Retrieved from https://pami.emergency.med.jax.ufl.edu/files/2015/03/Merkel-SI-et-al.-Practice-applications-of-research.-The-FLACC.-a-behavioral-scale-for-scoring-postoperative-pain-in-young-children.pdf
- Krechel, S. W., & Bildner, J. (1995). CRIES: A new neonatal postoperative pain measurement score. Initial testing of validity and reliability. Pediatric Anesthesia, 5(1). p 53-61. https://doi.org/10.1111/j.1460-9592.1995.tb00242.x
- Rijkenberg, S., & van der Voort, P. H. J. (2016). Can the critical-care pain observation tool (CPOT) be used to assess pain in delirious ICU patients? Journal of Thoracic Disease, 8(5). E285-E287. Doi: 10.21037/jtd.2016.03.32
- Dimitriou, V., Paraskevi, M., Manataki, A., & Damigo, D. (2017). Postoperative pain management: A systematic review of randomized controlled trials. Journal of PeriAnesthesia Nursing, 32(6). 530-541. https://doi.org/10.1016/j.jopan.2016.12.003
- McKenry, L., Tessier, E., & Hogan, M. (2006). Mosby’s Pharmacology in Nursing (22nd ed.). St. Louis: Mosby. Pp. 267-268. ISBN 0-323-030008-4
- Edwards, S. (2011). On the brain: The long life of early pain. The Harvard Mahoney Neuroscience Institute Letter, 17(1). Retrieved from https://hms.harvard.edu/sites/default/files/HMS_OTB_Winter11_Vol17_No1.pdf
- Hulla, R., Vanzzini, N., Salas, E., Bevers, K., Garner, T., & Gatchel, R. T. (2019). Pain management and the elderly. Practical Pain Management, 17(1). Retrieved from https://www.practicalpainmanagement.com/treatments/pain-management-elderly
- Potter, P. A., Perry, A. G., Stockert, P. A., & Hall, A. M. (2013). Fundamentals of Nursing (8th Ed.). St. Louis: Elsevier. Pp. 967. ISBN 978-0-323-07933-4.
- Quinlan, J., & Cox, F. (2017). Acute pain management in patients with drug dependence syndrome. Pain Reports, 2(4). P. e611. Doi: 10.1097/PR9.0000000000000611
A-Fib and Stroke Risk
- American Stroke Association. (2021, February 11) “About Stroke“. https://www.stroke.org/en/about-stroke
- Babkair, Linda (2017) “Cardioembolic stroke: A Case Study“ Critical Care Nurse (37) 1, 170-174
- American Heart Association. (2021, February 11) “Stroke Risk factors“. https://www.stroke.org/en/about-stroke/stroke-risk-factors
- Tarek, Aham MD Medscape update (2021, February 17) “CHADS2 and CHA2DS2-VASc Score for Stroke Risk Assessment in Atrial Fibrillation“. https://emedicine.com/article/2172597-overview
- Watchman.com (2021, February 15) “Physician Resources: About the Procedure.“ https://www.watchman.com/content/watchman-com1/hcp
Disclaimer:
Use of Course Content. The courses provided by NCC are based on industry knowledge and input from professional nurses, experts, practitioners, and other individuals and institutions. The information presented in this course is intended solely for the use of healthcare professionals taking this course, for credit, from NCC. The information is designed to assist healthcare professionals, including nurses, in addressing issues associated with healthcare. The information provided in this course is general in nature and is not designed to address any specific situation. This publication in no way absolves facilities of their responsibility for the appropriate orientation of healthcare professionals. Hospitals or other organizations using this publication as a part of their own orientation processes should review the contents of this publication to ensure accuracy and compliance before using this publication. Knowledge, procedures or insight gained from the Student in the course of taking classes provided by NCC may be used at the Student’s discretion during their course of work or otherwise in a professional capacity. The Student understands and agrees that NCC shall not be held liable for any acts, errors, advice or omissions provided by the Student based on knowledge or advice acquired by NCC. The Student is solely responsible for his/her own actions, even if information and/or education was acquired from a NCC course pertaining to that action or actions. By clicking “complete” you are agreeing to these terms of use.
➁ Complete Survey
Give us your thoughts and feedback
➂ Click the Green MARK COMPLETE Button Below
To receive your certificate
