Course
Ostomy Management
Course Highlights
- In this Ostomy Management course, we will learn about the different types of ostomies and their care techniques.
- You’ll also learn the process of site selection and identify complications of ostomies.
- You’ll leave this course with a broader understanding of the importance of patient education prior to and following the ostomy procedure.
About
Contact Hours Awarded: 1
Course By:
Abbie Schmitt
MSN, RN
Begin Now
Read Course | Complete Survey | Claim Credit
➀ Read and Learn
The following course content
Introduction
Newton's law of gravity states: what goes up, must come down; similarly, the normal human gastrointestinal system has a law that what goes in, must come out. When disease inhibits the normal process, ostomy procedures are a life-saving intervention.
There are around one million people living with an ostomy or continent diversion in the US, and approximately 100,000 ostomy surgeries are performed annually in the US (1). We will build a stronger understanding of various types of ostomies, indication for the need, site selection, stoma care, complications, and patient education.
Types of Ostomies
An ostomy is a surgically created opening that reroutes stool or urine from the abdomen to the outside of the body through an opening called a stoma (9). The term stoma refers to the portion of the bowel that is sutured into the abdomen (9).
When you look at a stoma, you are looking at the lining (the mucosa) of the intestine. The color is similar to the mucosa inside your mouth and cheek. Throughout various healthcare environments, you may hear the terms ostomy or stoma interchangeably. The purpose of an ostomy is to bypass a diseased portion of the gastrointestinal tract that is not functioning properly or has been removed (2).
Ostomies are placed proximal to the diseased area, comparable to building a dam in a river to stop the flow of fluid and divert it somewhere else. An ostomy can be temporary or permanent.
There are three most common types of ostomies: ileostomy, colostomy, and urostomy (9). We will discuss these types, but it is important to recognize that gastrostomy, jejunostomy, duodenostomy, and cecostomy procedures are also done.
- Ileostomy: A stoma is attached at the end of the small intestine (ileum) to bypass the colon, rectum, and anus.
- Colostomy: A stoma is attached to a portion of the colon to bypass the rectum and anus.
- Urostomy: A stoma is attached to the ureters (the tubes that carry urine from the kidney to the bladder) to bypass the bladder.
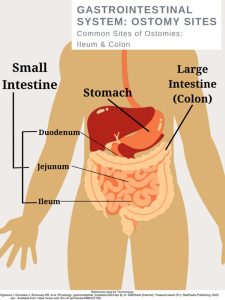
Ileostomy
The small intestine has three parts that are compact and folds over itself: the duodenum, jejunum, and the ileum. An ileostomy has a stoma attached and created from the ilium. The ileum is the final and longest segment of the small intestine (9).
The ileum terminates at the ileocecal valve, which controls the flow of digested material from the ileum into the large intestine and prevents the backup of bacteria into the small intestine (9). If a patient has this type of ostomy, the colon distal to the ostomy has a form of disease or disorder such as cancer. There are two main types of ileostomies, loop, and end ileostomy.
Loop ileostomy
In a loop ileostomy, a loop of the small bowel is lifted and held in place with a rod due to resection or repair to the distal bowel (Will). This ostomy is technically two stomas joined together (4). Loop ileostomies are typically temporary and will be closed or reversed through an operation in the future.
End ileostomy
In an end ileostomy, the ileum is surgically separated from the colon, the colon is removed or left to rest, and the end of the ileum is brought to the surface through the abdomen to form a stoma. Although end ileostomies are sometimes temporary and later rejoined, they are usually permanent (9).
Colostomy
A colostomy may be formed as an ascending, transverse, descending, or sigmoid colostomy (9). It is named according to the location of placement. An end colostomy is constructed from the ascending, transverse, descending, or sigmoid colon and has one opening for fecal elimination.
Loop Colostomy
The creation of a loop stoma takes a loop of the colon (usually the transverse colon) and pulls it to the outside of the abdominal wall (9). In this type of ostomy, the entire bowel is not dissected but left mostly intact.
End Colostomy
In end colostomies, the proximal end of the colon is dissected and pulled out of the abdominal cavity, which becomes the stoma (9). Additional procedures may involve repairing or removing portions of the distal colon or rectum.
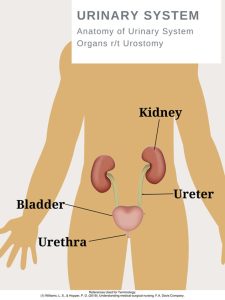
Urostomy
Kidneys have an important job of filtering waste and excess fluid from your blood. This process creates urine, which then travels from the kidneys to the bladder through tubes called ureters (8). If the bladder is damaged or diseased, ostomies are a life-saving method of creating safe passage for the urine.
A urostomy is a surgical opening in the abdominal wall that redirects urine away from a bladder that’s diseased, has been injured, or isn't working properly (8). The bladder is either bypassed or removed (called a cystectomy) during surgery. Following the surgery, urine exits the body through a stoma.

Self Quiz
Ask yourself...
- Have you ever witnessed a GI or Urinary Surgery?
- Do you have experience with GI / Urinary procedures like a colonoscopy?
Indication for Ostomy Placement
Gastrointestinal Tract Ostomy
- Cancer
- Colorectal
- Rectal
- Trauma/ Injury
- Significant Disorders
- Crohn’s disease
- Ulcerative Colitis
- Diverticulitis
- Bowel perforation from a ruptured diverticulum or abscess
- Bowel obstruction
- Infection (9)
Urinary Tract Ostomy
- Bladder Cancer
- Neurogenic bladder disease (damage to the nerves that control the bladder)
- Birth defects
- Chronic inflammation of the bladder (9)

Self Quiz
Ask yourself...
- Have you cared for a patient with a new ostomy?
- Can you list reasons a patient is a candidate for an ostomy?
Site Selection
Wound, ostomy, and continence nurses (WOCN) play a vital role in site selection. Patients should have a pre-operative consultation prior to surgery. During this consultation, the nurse acts as an advocate and educator to prepare these patients for the physical and emotional path ahead of them. A significant amount of time should be spent with the patient before surgery to determine a stoma incision site (exit of ostomy).
It is important to make the presence of the ostomy (and collection bag) as comfortable as possible, striving to reduce the hindrance to ease movements and ability to wear their typical clothing (9). Studies show that preoperative education and stoma site marking has been directly responsible for improving quality of life and decreasing peristomal skin and pouching complications (4).
Site Assessment:
Locate positions for a site within the rectus muscle (4).
Observe the abdomen in various positions sitting, standing, or lying down.
Ask the patient about the types of clothing they wear most often. Examples: Level of pants (low, high), use of belts, dresses, etc. (9)
Determine a location that is visible to the patient, as they will need to see the site well for stoma care.
Avoid skin or fat folds (folds increase chances of leakage)
Avoid scars, bony prominences, and the umbilicus (4).

Self Quiz
Ask yourself...
- Locate places on yourself that would be appropriate for an ostomy site
- Can you think of reasons patients need to be able to see the site?
- Do you have a wound care nurse at your past or present workplace?
Post-operative Care
Post-operative care following ostomy placement is vital. The post-operative nurse assigned to this patient should read the surgery documentation to determine the type of procedure performed, intraoperative findings, type of stoma created, any advanced diseases, and unexpected events during surgery (2).
The nurse should be aware of the level of invasiveness; was this a laparoscopic, robotic, or open surgery? This type of surgery can have an impact on the post-op care plan and length of stay (2). Teaching can begin as soon as they are able to comprehend and focus on understanding new skills.
The stoma will gradually decrease in size over the weeks following the surgery. For a patient with a new ostomy, postoperative assessments should be done per facility protocol and the stoma should be inspected at least every 8 hours (9).
Note the type of closure (staples, sutures, liquid bonding agent), presence of abdominal drains, and presence of urinary catheter (C2). Assess for pain and address accordingly with repositioning, cold/heat therapy, and ordered pain medications. Assess for bowel sounds. Palpate the abdomen and note firmness and tenderness levels. Document strict Intake and Output for these patients.
Stoma Assessment:
Note the Appearance/ Color: The stoma should be pink to red in color, moist, and firmly attached to the surrounding skin (9). If the stoma appears bluish, it indicates inadequate blood supply; if the stoma appears black, necrosis has occurred. Immediate notification is needed from the provider, as the need to return to surgery will be assessed.
- Note the Presence of edema.
- Note the Surrounding skin
- Note any Ostomy Discharge
- Amount
- Color / Consistency
- Note any Bleeding
- Monitor for rupture or leakage.
Diet
Once bowel sounds and activity return, the patient’s diet may resume (2). Typically, patients are offered clear liquids to determine their ability to tolerate fluids. Nurses should encourage the patient to chew thoroughly, eat small frequent meals, and ambulate frequently to assist in gas movement and peristalsis (2).

Self Quiz
Ask yourself...
- Do you have experience with post-operative abdominal surgery?
- Explain possible respiratory or cardiovascular assessments that would be helpful for these patients
Stoma Care
Nursing Consideration / Reminders
Ostomy pouching system needs to be changed every 4 to 7 days, depending on the patient and type of pouch.
Patients should be encouraged to participate in stoma care. Instruct the patient to empty the pouch when it is one-third to one-half full as they become heavy and more prone to spilling or leaks.
Table 1. Ostomy Change Procedure SAMPLE (Always check with your agency policy)
| Steps | PURPOSE |
| 1. Perform hand hygiene. | This prevents the spread of germs and microorganisms. |
| 2. Gather supplies. |
Supplies:
|
| 3 Create privacy. Lift bed to comfortable height. |
Attention to psychosocial needs is imperative. Proper body mechanics is important for nurse. |
| 4. Place waterproof pad under pouch. | The pad prevents the spilling of effluent on patient and bed sheets. |
|
5. Remove ostomy bag. Apply non-sterile gloves. Support / hold the skin firmly with your other hand, apply adhesive remover if needed. Measure and empty contents. Place old pouching system in a garbage bag.
|
The pouch and flange can be removed separately or as one. Gentle removal helps prevent skin tears. Remove flange by gently pulling it toward the stoma. |
| 6. Clean stoma gently by wiping with warm water. Do not use soap. |
Aggressive cleaning can cause bleeding. If removing stoma adhesive paste from skin, use a dry cloth first. Soaps can irritate the stoma. Clean stoma and peristomal skin |
| 7. Assess stoma and peristomal skin. |
Stoma skin should be pink or red in color, raised above skin level, and moist (2). Skin surrounding the stoma should be intact and free from wounds, rashes, or skin breakdown. |
|
8. Measure the stoma diameter using the pre-cut measuring tool (or tracing template). Trace diameter of the measuring guide onto the flange and cut the outside of the pen marking. |
The opening should match the size of stoma. If there is skin exposed between the stoma and edge of the flange with an ileostomy, the drainage contains enzymes that will break down the skin (9). Cut out size to fit stoma, assess fit once cut. |
|
9. Prepare skin.
|
Paste can be applied directly to the skin or flange. |
|
10. Apply Flange
|
Press gently around the periphery of the stoma to create a seal |
|
11. Apply the ostomy bag Close the end of the bag with clip (follow the manufacturer’s instructions) |
Involve patient with this process, understanding instructions. |
| 12. Apply pressure to ostomy pouch to help with adhering to skin. | Heat/ warmth from hand can activate some flanges. |
| 13. Clean us supplies, perform hand hygiene. | Remove trash as quickly as possible to reduce odor. |
| 14. Document Procedure |
Example: Date/time: flange change complete. Stoma pink, moist, warm. Peristomal skin intact. Patient instructed in cutting flange to correct size, verbalized understanding of frequency of change. See ostomy flowsheet. (Abbie S., RN) |
| Data Source: Carmel, Colwell, J., & Goldberg, M. (2021). Wound, ostomy and continence nurse’s society core curriculum: ostomy management (Second Edition). Wolters Kluwer Health. | |

Self Quiz
Ask yourself...
- Are you familiar with your facility's ostomy care protocol (if appropriate)?
- How can the nurse implement safety measures with ostomy care?
- Do you feel comfortable with ostomy care documentation?
Complications
Ostomy Leakage
One of the most common and troublesome complications is leakage (4). Proper preoperative site selection (away from skin folds) is important. Patient education on proper techniques and supplies can aid in the prevention of leakage.
Educate patients on the risks of changing the ostomy too often. Frequent appliance changes lead to pain and frustration, as well as financial expenses on supplies (4). Leakage is more common in the early postoperative period but can also develop with weight changes later.
Interventions involve thickening the stool with antidiarrheals to form more solid excretion and pouching techniques to bolster the height of the stoma off of the peristomal skin (4). Helpful tips also include heating the appliance with a hair dryer before application, lying flat for several minutes following application, making sure the peristomal skin is dry before application, and the possible use of a fine dusting of stomal powder and skin sealant prior to application (4). Leakage is frustrating for patients, so support and encouragement is vital.
Mucocutaneous Separation
The stoma is sutured to the skin of the abdomen with absorbable sutures during surgery (4). Mucocutaneous separation is a complication that can occur if the sutures securing the stoma become too tight or if blood flow to the area is restricted (9). This complication requires appropriate treatment because the pouch leakage will occur from the open pocket.
The goal of treatment is to keep this open pocket covered properly until the wound heals on its own and closes. Appropriate covering of the opening can include an absorbent product such as an alginate, followed by a cover dressing such as a hydrocolloid, which is covered with the ostomy pouch (4).
Early High Ostomy Output
Early high ostomy output (HOO) is defined as ostomy output greater than fluid intake occurring within 3 weeks of stoma placement, which results in dehydration (4). This is more common with ileostomies (4). Strict Input and Output records are a vital nursing intervention. The most important treatment for this complication is hydration to prevent renal failure, which is typically done intravenously (4).
The site of a patient’s colostomy will impact the consistency and characteristics of the excretion. The natural digestive process of the colon involves the absorption of water, which causes waste from the descending colon to be more formed. Waste from an ileostomy or a colostomy placed in the anterior ascending colon will be a bit more loose or watery (2).
Peristomal Skin Issues
Irritant Contact Dermatitis (ICD) is the most common peristomal skin complication following ostomy placement (9). ICD is characterized by redness; loss of epidermal tissue; pain; and open, moist areas.
Newer and inexperienced patients and caregivers will increase the size of the pouching system opening to get a better seal and stop leakage (2) However, this only contributes to more skin breakdown and irritation. Patients may also develop a fungal rash, have allergic rashes to the ostomy appliance, or folliculitis (4).

Self Quiz
Ask yourself...
- Can you name measures to prevent leakage?
- Have you cared for a patient with Irritant Contact Dermatitis?
- Are you familiar with bulking agents for stool?
Patient Education
Patient education is a key aspect is caring for a patient with an ostomy, this process begins prior to surgery and remains constant throughout encounters. If you have not received specialized training on wound and ostomy care, you should reach out to the Wound, Ostomy and Continence Nurse (WON) within your healthcare setting to become involved if they are not already.
However, each nurse has a meaningful impact on discussing and managing expectations for life with an ostomy, including stoma care, complications, managing ostomy output, maintaining pouching appliances, and resources. Patients may feel inadequate and uneasy about caring for their stoma.
Nurses need to meet the unique learning needs of each patient and caregiver, providing education in verbal information, written pamphlets, online resources, videos, and demonstrations. The United Ostomy Associations of America, Inc. (UOAA), is a nonprofit organization that serves as an excellent resource for information, support, advocacy, and collaboration for those living with ostomies.
Nurses should be aware there is an “Ostomy and Continent Diversion Patient Bill of Rights” (PBOR) that outlines the best practices for providing high-quality ostomy care during all phases of the surgical experience (1). There are numerous national resources for patients, as well as community-based and online ostomy support groups.

Self Quiz
Ask yourself...
- Can you think of methods to assess patient knowledge on ostomy care?
- What are creative ways to involve an ostomy patient in care?
- Not all patients are savvy with online supply ordering, can you think of other ways to order supplies if they are not?
Promotion of Body Image and Self-Esteem
Ostomy surgery can have a major impact on how patients perceive themselves. A person’s body image is how they see themselves when they look in the mirror or how they picture themselves in their mind.
There are stigmas surrounding ostomies, such as being odorous, unhygienic, and unattractive due to the stoma, but the truth is that ostomies save lives and make life possible. Positivity should surround the conversation. Confirmations such as beauty, strength, celebration, and hope are meaningful.
Ways to become involved in celebrating ostomies:
- Become familiar with the United Ostomy Associations of America (UOAA) and their initiatives.
https://www.ostomy.org/ostomy-awareness-day/
National Ostomy Awareness Day on October 7, 2023
Worldwide Virtual Run for Resilience Ostomy 5k
- Social Media Sites
Celebrate Body Positivity for those with ostomies
Intimacy Encouragement
Conclusion
Ostomy care is an essential nursing skill. If you are caring for a patient with an ostomy, remember that this is a major life-altering event and condition. Reflect on ways to provide individualized care by understanding various types of ostomies, site selection, stoma care, complications, and patient education. Empower and encourage these ostomy patients’ confidence in themselves.
References + Disclaimer
- Burgess-Stocks, Gleba, J., Lawrence, K., & Mueller, S. (2022). ostomy and continent diversion patient bill of rights. Journal of WOCN : Wound, Ostomy, and Continence Nursing., 49(3), 251–260. https://doi.org/10.1097/WON.0000000000000876
- Carmel, Colwell, J., & Goldberg, M. (2021). Wound, ostomy and continence nurse’s society core curriculum: ostomy management (Second edition.). Wolters Kluwer Health.
- Estrada, D. M. L., Benghi, L. M., & Kotze, P. G. (2021). Practical insights into stomas in inflammatory bowel disease: what every healthcare provider needs to know. Current Opinion in Gastroenterology, 37(4), 320–327. https://doi.org/10.1097/MOG.0000000000000737
- Hedrick, T. L., Sherman, A., Cohen-Mekelburg, S., & Gaidos, J. K. J. (2023). AGA Clinical Practice Update on Management of Ostomies: Commentary. Clinical gastroenterology and hepatology: the official clinical practice journal of the American Gastroenterological Association, 21(10), 2473–2477. https://doi.org/10.1016/j.cgh.2023.04.035
- Hill, B. (2020). Stoma care: procedures, appliances and nursing considerations. British Journal of Nursing, 29(22), S14–S19. https://doi.org/10.12968/bjon.2020.29.22.s14
- Ogobuiro I, Gonzales J, Shumway KR, et al. Physiology, gastrointestinal. [Updated 2023 Apr 8]. In: StatPearls [Internet]. Treasure Island (FL): StatPearls Publishing; 2023 Jan-. Available from: https://www.ncbi.nlm.nih.gov/books/NBK537103/
- United Ostomy Associations of America, Inc. (2018). Know your ostomy pouching system & supplies. https://www.ostomy.org/know-your-ostomy-pouching-system-supplies/
- Urostomy and continent urinary diversion. (2006). U.S. Dept. of Health and Human Services, National Institutes of Health, National Institute of Diabetes and Digestive and Kidney Diseases.
- Williams, L. S., & Hopper, P. D. (2019). Understanding medical-surgical nursing. F.A. Davis Company.
Disclaimer:
Use of Course Content. The courses provided by NCC are based on industry knowledge and input from professional nurses, experts, practitioners, and other individuals and institutions. The information presented in this course is intended solely for the use of healthcare professionals taking this course, for credit, from NCC. The information is designed to assist healthcare professionals, including nurses, in addressing issues associated with healthcare. The information provided in this course is general in nature and is not designed to address any specific situation. This publication in no way absolves facilities of their responsibility for the appropriate orientation of healthcare professionals. Hospitals or other organizations using this publication as a part of their own orientation processes should review the contents of this publication to ensure accuracy and compliance before using this publication. Knowledge, procedures or insight gained from the Student in the course of taking classes provided by NCC may be used at the Student’s discretion during their course of work or otherwise in a professional capacity. The Student understands and agrees that NCC shall not be held liable for any acts, errors, advice or omissions provided by the Student based on knowledge or advice acquired by NCC. The Student is solely responsible for his/her own actions, even if information and/or education was acquired from a NCC course pertaining to that action or actions. By clicking “complete” you are agreeing to these terms of use.
➁ Complete Survey
Give us your thoughts and feedback
➂ Click the Green MARK COMPLETE Button Below
To receive your certificate
