Course
Overview of Peritoneal Dialysis
Course Highlights
- In this Overview of Peritoneal Dialysis course, we will learn about the types of peritoneal dialysis that are currently available.
- You’ll also learn the complications of peritoneal dialysis.
- You’ll leave this course with a broader understanding of the indications for peritoneal dialysis.
About
Contact Hours Awarded: 2
Course By:
Tabo Mwikisa-Kelly
DNP, MSN, RN, CNEcl
Begin Now
Read Course | Complete Survey | Claim Credit
➀ Read and Learn
The following course content
Case Study
A 32-year-old patient, presented to the hospital with acute abdominal pain around their peritoneal dialysis catheter site, vomiting, and fevers lasting for 5 days. The patient has no known allergies. They reported having difficulty draining their abdomen and noticed the dialysate output was cloudy effluent for a week. Their vital signs on admission: BP 158/99, temperature 38.6, respiration 22 breaths per minute, heart rate 95 beats per minute.
The patient has a medical history of chronic kidney disease (CKD) related to Focal Segmental Glomerulosclerosis (FSGS) and Diabetes Mellitus 2 (DM2). The patient is currently on Continuous Ambulatory Peritoneal Dialysis (CAPD) and is actively listed for a kidney transplant. The patient has been on CAPD for 2.5 years and recently started using the Automated Peritoneal Dialysis (APD) and alternates with CAPD exchanges, 3 times a week. Their Peritoneal Dialysis (PD) regimen involves the use of a cycler with 4 cycles of 2 Liter exchanges over 8 hours with intervening dry days.
Their current medications are insulin, phosphate binders, lisinopril, and gentamicin every other day for the exit-site of the catheter. The patient lives with their spouse and two children at home. They perform both CAPD and CCPD independently to help achieve better renal clearance. When asked about the PD cleaning techniques, they occasionally state using a dialysis solution to clean the port. On days that they are tired they forget to clean the transfer set.

Introduction
Chronic Kidney Disease is becoming more common in the United States. There are approximately 37 million Americans who are affected by chronic kidney disease (CKD) [9]. Chronic kidney disease (CKD) is known as a “silent disease” because the symptoms usually manifest when the disease has progressed into the advanced stages. When left untreated, CKD can advance into End Stage Renal Disease (ESRD). ESRD affects approximately 808,000 adults in the United States [9].
When the kidneys are no longer able to support the body’s needs of filtering toxins and maintaining the right balance of water, electrolytes, and minerals in the body, a life-sustaining renal replacement therapy is necessary to survive. This life-sustaining treatment therapy is achieved by what is known as dialysis until one can receive a kidney transplant [22]. The two major forms of dialysis that are currently available worldwide are hemodialysis (HD) and peritoneal dialysis (PD) [11].
The main factors that determine what type of dialysis a person can receive are dependent on patient preferences that fit their lifestyle, resources within their health system, and health needs. Although the utilization of PD is low in the United States (US), more people are opting for home dialysis because it offers more flexibility and is known to produce better patient outcomes. In this course, we take a more in-depth view of PD.
Peritoneal Dialysis: The Basics
What is Peritoneal Dialysis?
Peritoneal dialysis (PD) is a type of renal replacement therapy used to treat a person with kidney failure. PD does not cure kidney failure. Rather, PD replaces the function of normal working kidneys by removing toxins and excess fluids from the blood using the peritoneal membrane that performs as a natural filter in the body. The peritoneal membrane is a semi-permeable lining found in the abdomen cavity.
To perform PD requires access to the peritoneal membrane which is achieved surgically by placing a hollow tube also known as a (catheter) under the skin and into the peritoneal cavity of the abdomen. The catheter is a soft tube that is usually made from silicone that allows for the transfer of fluid in and out of the peritoneal cavity [5]. It is recommended to start PD 10 to 14 days after the catheter has been surgically placed to allow for the catheter site to heal [4][21][20].
When the PD catheter is initially inserted, it contains cuffs made from Dacron (like velcro). As the catheter site starts to heal, the skin tissue in the abdomen starts to grow into the cuffs. The cuffs help to anchor the PD catheter in place by restricting back-and-forth movement and preventing trauma at the PD exit site. The area of the abdomen where the catheter comes outside of the body is known as the “exit site.” The exit site is usually located on the right or left side of the umbilicus [5][6].
PD is a self-management therapy that can be performed in a home setting or space that is conducive for the procedure, for example a patient room in a hospital [9]. After the PD catheter is placed, the person who will perform PD and their family members are required to go through training on how to safely perform the procedure. The training lasts for at least 1 – 2 weeks. Training with return demonstrations on how to perform PD is usually provided by a dialysis nurse at a dialysis center [5].
This training allows one to perform PD independently using a machine known as a cycler or manually. Once training is complete and the PD supplies are ordered for the patient, a home visit by a dialysis nurse is required to ensure that the patient’s home environment is conducive to performing PD [5].
How does Peritoneal Dialysis work?
PD involves the use of a sterile solution known as dialysate that is instilled and drained from the body’s peritoneum through the PD catheter. Dialysate contains a balanced concentration of electrolytes and varying concentrations of glucose. Dialysate is made up of a hypertonic solution that contains dextrose which is an osmotic agent or that exerts osmotic pressure and leads to ultrafiltration that occurs through the peritoneal membrane [2][3][22]. The waste products and excess fluids in the blood are filtered through the blood vessels in the peritoneum into the dialysate (effluent) by diffusion and osmosis [22].
The concentration of glucose in the dialysate helps to regulate the amount of excess fluid removed from the blood. The higher the glucose concentration, the more fluid is pulled off from the body. The process of draining and refilling dialysate in the body is referred to as an “Exchange.” The time in which the dialysate remains in the body between exchanges is referred to as the dwell time.
Advantages/Disadvantages
Studies have shown that peritoneal dialysis has several advantages compared to hemodialysis (HD). These advantages are patient independence, increased freedom of perception, improved quality of life, preservation of residual kidney function, patient satisfaction, and cost-effectiveness [7][13].
Advantages of Peritoneal Dialysis over Hemodialysis
- Generally associated with better patient outcomes as PD is known to preserve residual kidney function
- Fewer side effects with treatment (i.e. low blood pressure, fatigue, nausea)
- Convenience to be performed in a home setting
- Technical simplicity which requires lesser need for trained staff
- Decreased vascular complications
- Effective and gentler treatment
- Less restrictive on diet compared to HD
- No needles used compared to HD
- Allows for easier travel arrangements compared to HD
Disadvantages of Peritoneal Dialysis
- Poor blood pressure control due to fluid overload from PD fluid
- Risk of peritonitis
- Patient compliance with consistency in performing PD
- Weight gain especially around the waistline
- Storage space in the home for PD supplies
- PD sessions need to be incorporated into the daily routine as it is performed daily
- Requires more personal responsibility to remain adherent to treatment
Indications/Contraindications
Indications of Peritoneal Dialysis
PD is indicated in any patient who has acute renal failure or ESRD with an intact peritoneum. There are several indications for PD as a treatment option [2][6]. These include:
- Failure to have vascular access
- Congestive Heart Failure (CHF)
- Intolerance to Hemodialysis
- Prosthetic vascular disease
- Children 0 to 5 years old
- Patient preference
- No close access to a HD center
Contraindications of Peritoneal Dialysis
- Uncorrected abdominal wall hernia (collapsed muscle in the abdominal area)
- Pleuroperitoneal shunt
- Severe vascular disease
- Abdominal adhesions
- Inability to care for oneself
- Digestive tract diseases such as ulcerative colitis or diverticulitis

Self Quiz
Ask yourself...
- Describe how Peritoneal Dialysis (PD) works.
- What are the advantages of PD compared to hemodialysis?
- List at least 6 indications of PD.
- What are the types of PD?
Types of Peritoneal Dialysis
The two types of peritoneal dialysis are Continuous Ambulatory Peritoneal Dialysis (CAPD) and Automated Peritoneal Dialysis (APD) which is sometimes referred to as Continuous Cyclic Peritoneal Dialysis (CCPD) [1][9]. APD is known to be more effective because its dialysis adequacy and ultrafiltration targets are more optimized compared to CAPD. APD has improved patient compliance and lowered the risk of peritonitis [9]. Patients need to learn both CAPD and APD in case one must travel without the machine or in the event of a power outage or the machine does not work [3].
Continuous Ambulatory Peritoneal Dialysis (CAPD)
Continuous Ambulatory Peritoneal Dialysis (CAPD) does not require the use of a machine as it uses gravity. Patients manually infuse and drain 2 to 3 liters of dialysate approximately 4 times a day. The procedure generally takes 30 minutes to complete. During this process, patients have to allow the PD fluid to dwell in their peritoneum between four to six hours between cycles [9][12]. Patients typically have dialysate in their peritoneum 24 hours a day except for times when they are permitted to have dry periods for convenience and comfort. Dry days are suitable for patients who still have residual kidney function.
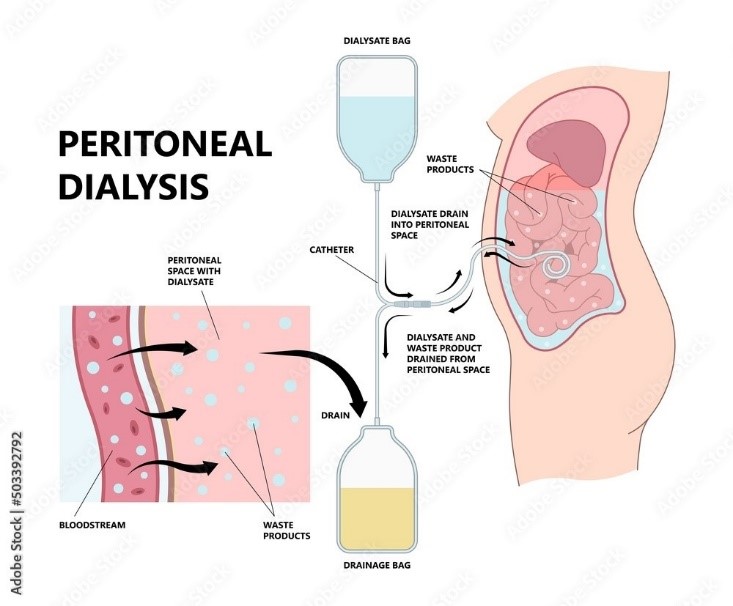
Figure 1. Peritoneal Dialysis [23]
Automated Peritoneal Dialysis (APD)
Automated peritoneal dialysis (APD) is a popular method of PD that is performed with the use of a machine often referred to as a cycler. The machine automates the process of filling and draining dialysate in the peritoneum of the abdomen. The machine performs several dialysis exchanges mostly when the patient is sleeping at night or sometimes during the day. The cycler is programmed to deliver specified amounts of dialysate as scheduled by the patient/caregiver. Also, the cycler maintains 3 to 5 exchanges over 8 – 10 hours [1] [9]. There are three types of APD which include the following.
- Continuous Cyclic Peritoneal Dialysis (CCPD) – Three to six nighttime exchanges are performed using a cycler with a daytime dwell of up to 12 to 15 hours.
- Nocturnal Intermittent Peritoneal Dialysis (NIPD) -nighttime exchanges using the cycler are performed and patients can go without dialysate in their peritoneal cavity during the day.
- Tidal peritoneal dialysis (TPD) – involves leaving some dialysate in the peritoneum between exchanges for patient comfort.
To be able to achieve adequate clearances, some patients are prescribed both CAPD and APD [22].
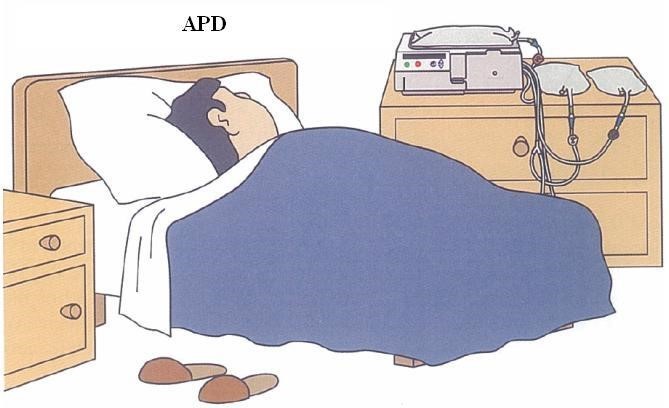
Figure 2. Automated Peritoneal Dialysis [17]
Things to Consider
Below are some important precautions and contraindications to pay attention to for any person who performs peritoneal dialysis [2][4]. Training is required to be able to successfully perform peritoneal dialysis independently. Here are things to consider:
Allergies
When using dialysate made with icodextrin, consider allergies to corn or corn-based products with cornstarch.
Diabetes
Patients with diabetes require close monitoring of insulin requirements. It is important to ensure that the correct testing of glucose is used as patients may present with false glucose readings as a result of the dialysate use (this could result in administering insulin unnecessarily)
Dialysate
Dialysate is intended for intraperitoneal administration only and is contraindicated in patients with severe lactic acidosis. Dialysate should not be used intravenously or intraarterial [2]. The most commonly used dialysate in the United States contains dextrose with the following concentrations: 1.5 %, 2.5%, and 4.5%. The higher the concentration of dextrose, the more that fluid is pulled from the body [15]
The lesser-used dialysate in the United States is Extraneal (icodextrin) which is the only FDA-approved non-glucose solution that contains a 7.5% icodextrin. Icodextrin has a longer dwell time in the peritoneum of up to 8 to16 hours and minimizes the number of exchanges performed by patients (Baxter). Extraneal is indicated for single daily exchange and has been found to have better ultrafiltration compared to 4.5% dextrose [15].
Other
Monitoring patient’s volume should be implemented carefully to avoid volemic complications hypervolemia or hypovolemia. Choosing an osmotic agent for the patient must be individualized.
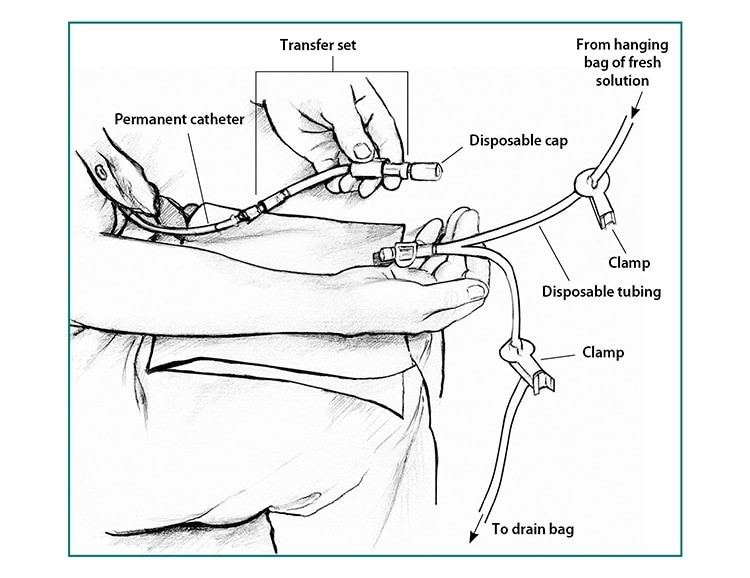
Performing Peritoneal Dialysis
To perform CAPD it is important to have a functioning catheter and compatible transfer set. A transfer set is an extension of the PD catheter tube with a twist or lock clamp that is used to connect the catheter to the dialysate bag. The transfer set helps to minimize trauma to the PD catheter [11]. Depending on the manufacturer of the catheter, there are instances when a patient’s transfer set is not compatible with the PD delivery system. This requires adaptation of the PD catheter delivery system through the patient’s transfer set. For example, when a patient who has a Fresenius transfer set is admitted to a hospital that uses the Baxter PD system. An adapter is used to ensure that PD can be performed successfully on the patient with a non-compatible transfer set. The adapter can be left in place until the patient is discharged from the hospital [23].
Peritoneal Dialysis Procedure [9]
Procedure
It is important to gather all the necessary supplies needed to perform PD. PD is a 3-step procedure that is referred to as an “Exchange.” Step 1 involves draining the PD effluent (waste and excess fluid from the body). Step 2 is the filling of dialysate into the peritoneum and step 3 is the dwelling of the dialysate solution in the peritoneum for a given period. The three steps are repeated in a continuous cycle [1].
The PD procedure is usually performed in a home setting or an enclosed environment such as a patient’s hospital room.
You will need the following supplies to perform PD [4]:
- Correct ordered dialysate solution
- CAPD warmer/electric blanket
- Zero spring weighing scale if performing PD manually
- Supplies to clean the exit site (PD cleaning solution, gauze)
- Mask for everyone present in the room where the PD is taking place
- Designated table or clean surface for the PD supplies
- 2 ultra-clean clamps (for manual PD)
- Sterile disposable mini cap
- Hand sanitizer
- Clean gloves or sterile gloves
- IV pole to hang the bags when performing manually
- Cycler when performing APD
Preparation for Peritoneal Dialysis Therapy
- It is important to work in an area that is clean and dry, for the prevention of infections [1][3].
- It is recommended to work or set up PD equipment in an area that is well lit and free from clutter.
- No pets must be in the room during the PD procedure.
- Turn off any fans if present.
- PD must be performed away from open windows or drafts.
- Before starting PD, it is recommended to warm the dialysate to body temperature to help- prevent abdominal discomfort such as cramping. A special warmer is used to warm the dialysate or overwrap in a heating pad. The recommended temperature is 37 °C (98.6F). Do not warm the PD fluid in the microwave. When performing PD through APD, the machine automatically warms the solution.
- It is important to inform others that the PD procedure will be taking place by putting a sign by the door.
Steps Before Connecting the Peritoneal Dialysis System
The most important key in performing PD is to maintain an aseptic technique [3][10].
- Before connecting the transfer set to the dialysate bag, perform thorough hand hygiene and flush out air from the tubing before opening the PD transfer set.
- Everyone present in the room must wear a clean surgical mask.
- Don some gloves.
- For manual CAPD exchanges, open the ultra-bag packaging that contains the dialysate solution and uncoil the tubing and drainage bag. Inspect the PD solution bag, tubing, and frangible to ensure the pull ring is intact. DO NOT use the PD solution if the pull-out cap is off or the frangible is broken as this may have impeded sterility.
- An important acronym to remember when inspecting the bag is SEAL [3][9]. You would check for the following:
- S: Solution strength
- E: Expiration date
- A: Amount contained in bag (e.g. 2 L)
- L: Leaks
- Once the packaging is open, hang the PD solution bag on the IV pole for the manual CAPD exchange.
- Hang the solution bag above the patient’s abdomen and the drainage bag below the patient’s abdomen. The solution bag is the inflow, and the drainage bag (empty bag) is the outflow.
Connecting the Tubing
- Before connecting the transfer set to the PD tubing, clean the transfer set of the PD catheter using a recommended cleansing solution to prevent peritonitis – follow manufacturer instructions.
- Perform hand hygiene and wear some clean gloves.
- Using an aseptic technique (without touching the inside of the tubing), quickly pull the ring from the ultra-bag and remove the mini cap from the transfer set.
- Using an aseptic technique (without touching the rim of the catheter), connect the Y-tube of the fresh dialysate bag to the patient’s transfer set whilst keeping the transfer set closed.
- While keeping the patient connector end closed, the tubing needs to be primed to remove any air. This can be done by allowing a small amount of solution from the fresh dialysate bag. This is followed by clamping the tubing that runs from the dialysate bag and emptying the dialysate from the peritoneal cavity.
Setting Up with the Peritoneal Dialysis Cycler:
- Perform hand hygiene.
- Hook the machine by following instructions and the procedure manual on the machine or as instructed by the PD nurse.
- Connect 3 to five bags to the machine which will automatically do the PD cycling overnight which is typically between 8 to 10 hours.
- Disconnecting tubing when the cycle is complete.
- Disposal of PD fluid is usually done in a sink or tub closest to where the PD is performed.
The Process for Peritoneal Dialysis
For Continuous Ambulatory Peritoneal Dialysis (CAPD):
a) Drain – The process of removing the saturated dialysate (effluent) from the body which contains excess fluids and waste outside of the body into a drainage bag that is connected to the catheter. You may notice the color is brown at the beginning of a drain. The drainage bag must be below the abdomen to aid in the flow of gravity of the effluent.
This is usually at the end of a 4 to 6 hours period after the dialysate has been absorbed by the body. The draining process takes between 20 – 30 minutes when performed manually. It is necessary to weigh the bag containing the effluent and record the amount at the end of each draining procedure. It’s desirable to have more effluent than the amount of inflow Inspect for any fibrin and cloudiness as this may indicate peritonitis.
b) Fill – This is the process of instilling the new dialysate solution after the old dialysate solution has been drained from the abdomen. To fill, you will need to open the transfer set and unclamp the new solution bag and let it drain by gravity into the abdomen. When complete, clamp the tubing at the fill line.
c) Dwell – During this process, the dialysate stays in the peritoneal cavity for the prescribed amount of time. Complete the process by disconnecting the ultra from the transfer set. Immediately connect a sterile mini cap to the end of the transfer set. Ensure the mini cap has iodine and is wet before use.
*Disposal of PD effluent can be done in the toilet or bathroom drain.

Self Quiz
Ask yourself...
- What does the acronym SEAL stand for and when is it helpful to use?
- List the important supplies that should be gathered before performing PD.
- What is the aseptic technique and why is it important in PD?
After Care
After care includes:
- Use non-occlusive dressing to help decrease microtrauma to the exit site.
- Routinely clean the exit site twice a week or as needed if it becomes soiled.
- Wear breathable and freshly laundered clothing when exercising to help reduce sweat around the exit site [4].
Complications
The two most common causes of peritoneal dialysis complications are mechanical and infectious.
Mechanical Complications
Mechanical complications are categorized as flow dysfunction and leak issues.
Flow dysfunction is manifested as pain when draining the effluent solution which results in incomplete draining of PD effluent resulting in irritation against the parietal peritoneum [14]. Four types of flow dysfunction will be discussed below.
- Extrinsic compression of the catheter tip: This is caused by distention of the bladder and constipation which makes draining the effluent difficult due to blockage to the holes in the PD catheter. Treatment of the underlying cause can help resolve the issue. For example, constipation can be treated using laxatives, eating a healthy diet, and regular exercise.
- Internal luminal obstruction – This is caused when there is kinking or too much fibrin/blood clots inside of the catheter which makes it difficult to perform and exchange either through draining or filling of the dialysate. Begin by ensuring that the tubing is straightened out [14]. When there is too much fibrin – one can squeeze the tubing gently or bend the closest frangible at the Y-tube connection to help pass the fibrin. Have a trained professional like a dialysis nurse irrigate the catheter with saline. Then call the provider as soon as possible after completing the exchange. One can anticipate receiving heparin which is instilled in the dialysate.
- Poor positioning and migration – This can affect the performance of PD exchanges. This can be minimized during the initial catheter insertion when the right shape is used for a particular patient.
- Tissue attachment and entrapment can cause difficulty in performing an exchange and may require a surgical release or exchange of the catheter. Often requires surgical intervention.
Leaking from PD catheter: Recurring leaks may require the PD catheter to be exchanged or to completely switch to hemodialysis depending on severity of the problem [6][7][14].
- Peri-catheter leaks: These can be avoided by delaying the start of PD by at least 2 weeks through what is known as the “break-in period.” The break-in period is the time interval between the PD catheter insertion and initial PD use. If PD needs to be performed urgently, it is recommended to use low volume of fluid exchanges which must be performed when the patient is in a supine position [7].
- Abdominal hernias: Develop due to increased abdominal pressure from the continual use of PD dialysate. The contributing risk factors are weight gain and prolonged use of steroids. Surgical procedures may be required to fix hernias that are problematic to the patient [14].
- Hydrothorax: Rare and emergent complication that occurs on the right side of the chest. Results in a fistula known as the pleuroperitoneal connection. The PD fluid moves into the peritoneum and eventually into the pleural space which leads to clinical sequelae. The hydrothorax increases the risk of developing a pleural effusion and requires surgical repair [7] [14].
Infectious Complications
Peritonitis is a serious and the most common type of infection found in patients on PD. Peritonitis is mostly caused by Staphylococcus aureus. Peritonitis can be prevented by maintaining proper hand hygiene and PD technique which could include proper clamping and priming of fluid, performing good exit site care, and avoiding constipation. The signs of peritonitis include fever, pain at the exit site, cloudy PD effluent, nausea, vomiting and abdominal distention. Patient education is key to preventing peritonitis [5][6].
Exit site infections and Tunnel infections: Tunnel infections occur in the presence of exit site infections and are more serious as they occur in the deep cuff of the catheter which spreads in the peritoneal cavity. Exit site and tunnel infections are the leading causes of peritonitis and loss of PD catheters. These infections are caused by poor exit site location or poor exit site care, usually related to a “touch contamination” due to a break in aseptic technique and contamination of the connection on the catheter when performing PD [5][6][14].
Clinical manifestations: fever, chills, abdominal pain, redness at the exit site, changes in PD fluid color and purulent effluent. Diagnosis: cultures and treatments are usually with corresponding antibiotics [8].
Superficial extrusion: rare complication associated with an infection or PD catheter malfunction [5][14].
Other Complications
- Overinfusion – It is important to look out for signs and symptoms of hypervolemia such as shortness of breath, abdominal distention or fullness, and edema. This can be resolved by draining [2][3].
- Encapsulating peritoneal sclerosis – This is a rare complication that is due to failure in ultrafiltration in the peritoneum which can cause acute bowel obstruction and malnutrition. EPS occurs when the intraperitoneal cavity becomes inflamed and fibrosis which results in encasement of the bowels loops. EPS often occurs due to prolonged use of PD dialysate which contains glucose degradation products that induce inflammation in the peritoneum which leads to fibrin deposits. EPS is associated with high morbidity and mortality rates in patients on PD [2,14,16].
Case Study Continued
Reminder: the patient is 32 years old and presented to the hospital with acute abdominal pain around their peritoneal dialysis catheter site, vomiting, and fevers lasting for 5 days. The patient is now found to have greater than 100 WBCs, with staphylococcus aureus in the peritoneal fluid sample (cell count and gram stain). The patient also reported that sometimes they forget to clean the catheter site with the recommended solution.


Self Quiz
Ask yourself...
- What are the signs and symptoms related to peritonitis infection in PD?
- A patient who is on PD complains about having severe right-sided chest pain. What emergent complication could the patient be experiencing?
Patient Education
Proper training during the initial phase, when patients start PD, is essential to achieving successful techniques and prevention of peritonitis. Prevention of peritonitis is the most important topic when educating patients on how to perform PD. Also, patients need to be alert and aware of the signs and symptoms of peritonitis [1][2][3][5][11].
Important topics to cover are listed below.
Teaching Topic 1: Peritoneal Dialysis Techniques
This section covers hand hygiene, masks, aseptic technique, warming of dialysate [3][4].
- Initial training must have an emphasis on hand washing and proper drying of hands.
- Wearing masks during PD exchanges or setup.
- Exchange techniques i.e. how to use aseptic techniques to prevent contamination (both manual and or with cycler). The sequence on how to prime dialysate bags and proper clamping of tubing during the PD procedure.
- The setting where PD takes place should be in a clean and dry space, with windows and doors closed, and no pets whilst performing PD.
- Inspect dialysate bags before each use. Remember to use the acronym SEAL when inspecting.
- Dialysate must be warmed up to 37 ℃ (97 ℉) using dry heat (i.e. no microwave or soaking dialysate in hot water)
Teaching Topic 2: Living with Peritoneal Dialysis
Patients will have to adjust to some lifestyle changes when they are on PD (i.e. work, traveling, sexual activities, and body image). Discuss with the patient that body image may change when on PD. The abdomen could enlarge slightly and the feeling of being bloated can occur from extended use of dialysate. Provide information on support groups [1][4].
- Patients can continue going to work even if they are on PD.
- It’s ok to travel although it is important to bring all the supplies necessary to perform PD, patients must be encouraged to bring medical information, and contact the care team about shipping supplies for further destinations, for air travel – contact airline on allowed PD items to bring.
- Provide sexual education and use options that support patients (APD or CAPD). Sexual activity can cause leaks mostly during the first few weeks of having the PD catheter inserted.
Teaching Topic 3: Storing Supplies
Store dialysate bags in a cool area as heat can degrade glucose and increase glucose concentration of glucose degradation products [9].
Teaching Topic 4: Site Care/ Assessment
Daily care of the exit site and assessment of infection must be encouraged – No redness, pain or purulence [4].
- Cleanse with a washcloth and gentle use of soap and water.
- Apply antibacterial cream and cover it with a bandage to immobilize the catheter to prevent trauma.
- Presentation with new tenderness at the catheter exit site or notice of new drainage must be reported to the dialysis team as soon as noticed.
- Exit site cleaning twice a week after showering or vigorous exercise.
- Application of mupirocin at the exit site can help reduce infections by using topical antibacterial prophylactic agents such as gentamicin.
Teaching Topic 5: Exercise
Exercise for patients on PD must be performed with caution such as limiting physical activity with a full peritoneal cavity [3][4].
- Walking and stationary bikes are safe for exercise.
- Light weightlifting, shoveling snow and jumping must be done after one has drained the abdomen which helps to reduce higher abdominal pressure.
- Swimming: preferably in the sea or well-maintained swimming pool. Patients must use clear waterproof dressing or a colostomy bag to secure the site.
- Contact sports can lead to increased risk for trauma and are not recommended.
- Core strength exercises are recommended to help support the back and manage low back pain.
Teaching Topic 6: Diet
Maintaining adequate nutrients and a balance in protein and electrolytes by limiting intake of foods high in sodium, potassium, and phosphorus. A registered dietician on the dialysis team can assist with making dietary recommendations [4,10,19].
- It is important to monitor caloric intake to help prevent excessive weight gain that can result from the body absorbing some of the high dextrose found in the dialysate.
- Patients must incorporate fiber in their diet to avoid being constipated.
- Eating star fruit is not recommended for patients on PD. Star fruit contains oxalate which is nephrotoxic and can lead to acute kidney injury (AKI). The adverse effects manifest as edema, oliguria, hiccups, confusion, agitation, and seizures.
Teaching Topic 7: When to Call for Help
Report any changes in the appearance of the effluent immediately to the dialysis team so they can assess [4].
- Patients should go to the nearest emergency department (ED) when there is no one available to help promptly as this allows for early intervention in case there is an infection or other underlying problem.
- Patients can be instructed to bring in specimens of the effluent in a specimen collection container.

Self Quiz
Ask yourself...
- Name the most important topic that must be covered when educating patients about PD.
- Name the life-threatening complication that EPS can cause.
Conclusion
Peritoneal dialysis is an effective form of renal replacement therapy that works as well as hemodialysis. Providing the proper training on how to perform PD is very important in preventing peritonitis, a common infection in PD, and other complications. PD provides more flexibility and is cost-effective for patients as they can independently perform the procedure from home or other appropriate spaces.

Self Quiz
Ask yourself...
Final Reflection Questions
- List the contraindications of PD.
- How does the concentration of dextrose in dialysate affect PD?
- Explain what the term exchange means in PD.
- Explain what dwell time means in PD.
- Name at least 3 types of mechanical complications in PD.
- What would be some indications that a patient has peritonitis?
- Identify two ways in which you can troubleshoot a problem related to poor draining of a PD catheter before calling the doctor.
- Name the most important technique that can assist in preventing infections such as peritonitis related to PD.
- What is the proper way to warm PD fluid? List two.
- Why is it important to weigh the effluent after draining PD fluid?
- List some of the benefits of PD.
- Why is the peritoneum a suitable medium for performing PD?
- List two ways that can help prevent peri-catheter leaks.
- Explain why it is important to drain the peritoneum before exercising.
- Name a serious complication that can happen when a patient eats excessive amounts of star fruit when on PD.
- What concerns would you have when a patient reports having right-sided chest pain after two PD exchanges?
- Name a common PD complication that is non-infectious and is caused by repeated exposure to dialysate.
- A float nurse from the maternal and child unit asks which tubing she needs to use to hang a PD dialysate bag. What would be the best response to give the nurse?
- How long should one wait before exercising after a Catheter is inserted?
- Name some types of exercises that are safe for patients on PD?
- What can a patient on PD do prior to doing a jumping exercise?
- A patient notices their PD effluent is cloudy and smells purulent when draining. They call the dialysis care center, and they are closed for Thanksgiving holiday. What should the patient do next?
References + Disclaimer
- American Kidney Fund. (2023). Peritoneal Dialysis. https://www.kidneyfund.org/treatments/dialysis/peritoneal-dialysis#how-can-i-do-pd-safely
- Baxter Healthcare Corporation. (2019). Highlights of prescribing information. https://dailymed.nlm.nih.gov/dailymed/fda/fdaDrugXsl.cfm?setid=aa268d3f-7389-4f25-801f-5d4825495f08&type=display
- Bexter Empowers (2018, March). PD education. Steps for safe treatment. https://www.pdempowers.com/sites/g/files/ebysai3381/files/2020-06/pd-lesson4-steps.pdf
- Bennett, P. N., Bohm, C., Harasemiw, O., Brown, L., Gabrys, I., Jegatheesan, D., & Thompson, S. (2022). Physical activity and exercise in peritoneal dialysis: International Society for Peritoneal Dialysis and the Global Renal Exercise Network practice recommendations. Peritoneal Dialysis International, 42(1), 8-24.
- Burkart, J. M., & Bansal, S. (n.d.). Patient education: Peritoneal dialysis (beyond the basics). Updated 2023, October 2023. Retrieved from https://www.uptodate.com/contents/peritoneal-dialysis-beyond-the-basics?search=peritoneal%20dialysis%20patient%20education&source=search_result&selectedTitle=1~150&usage_type=default&display_rank=1
- Ganapathy, A. S., Powell, M. S., & Pirkle, J. L. (2021). Extrusion of both Superficial and Deep Cuffs of a Functional Double-Cuff Peritoneal Dialysis Catheter after Significant Weight Loss. Case reports in nephrology and dialysis, 11(2), 190–194. https://doi.org/10.1159/000515049
- Ellsworth.P.I., (2021). Peritoneal Dialysis catheter insertion. https://emedicine.medscape.com/article/1829737-overview?form=fpf#showall
- Li, P. K. T., Chow, K. M., Cho, Y., Fan, S., Figueiredo, A. E., Harris, T., & Johnson, D. W. (2022). ISPD peritonitis guideline recommendations: 2022 update on prevention and treatment. Peritoneal Dialysis International, 42(2), 110-153.
- Khan, S. F. (2023). Updates on Infectious and Other Complications in Peritoneal Dialysis: Core Curriculum 2023. American Journal of Kidney Diseases.
- National Institute of Diabetes and Digestive and Kidney Disease. (2023). Kidney disease statistics for the United States. https://www.niddk.nih.gov/health-information/health-statistics/kidney-disease
- National Institute of Diabetes and Digestive and Kidney Disease., (2018, August). Peritoneal Dialysis. https://www.niddk.nih.gov/health-information/kidney-disease/kidney-failure/peritoneal-dialysis
- National Kidney Foundation., (2022). Kidney disease: the basics. Retrieved from https://www.kidney.org/news/newsroom/fsindex
- Gursu, M., Shehaj, L., Elcioglu, O. C., & Kazancioglu, R. (2023). The optimization of peritoneal dialysis training in the long-term. Frontiers in Nephrology, 3, 1108030.
- Fresenius Kidney Care., (n.d.) What is Continuous Ambulatory Peritoneal Dialysis? https://www.freseniuskidneycare.com/thrive-central/continuous-ambulatory-peritoneal-dialysishttps://www.ncbi.nlm.nih.gov/books/NBK532979/
- Baxter Healthcare Corporation (2023). Start with Extraneal. https://renalcareus.baxter.com/pd-hcp/extraneal
- Oza-Gajera, B. P., Abdel-Aal, A. K., & Almehmi, A. (2022). Complications of Percutaneous Peritoneal Dialysis Catheter. Seminars in interventional radiology, 39(1), 40–46. https://doi.org/10.1055/s-0041-1741484
- Sachdeva, B., Zulfiqar, H., & Aeddula, N. R. (2023). Peritoneal Dialysis. In StatPearls. StatPearls Publishing.
- Waknin, R., Cassani, F. A., & Kucera, J. N. (2022). Calcified encapsulating peritoneal sclerosis associated with peritoneal dialysis: A case report. Radiology Case Reports, 17(8), 2742-2746.
- Yaoking 2008, June 28th) Illustration of APD Dialysis [digital image]. Retrieved from https://commons.wikimedia.org/wiki/File:Illustration_of_APD_dialysis.jpg
- Herath, N., Kodithuwakku, G., Dissanayake, T., Rathnathunga, N., & Weerakoon, K. (2020). Acute kidney injury following star fruit ingestion: a case series. Wilderness & Environmental Medicine, 32(1), 98-101.
- Kidney Campus (n.d.). What is Peritoneal Dialysis? https://kidneycampus.ca/what-is-peritoneal-dialysis/
- Slaond. J., (2019). Nephrology secrets. Peritoneal Dialysis. Edition 4th. Chapter 53., pp. 368-386. Elsevier, Inc.
- Permpron., (n.d.). Shutterstock. Peritoneal Dialysis. https://www.shutterstock.com/image-vector/dialysate-cleansing-home-care-tube-fluid-2151913017
- Fresenius Medical Care. (2021). Adapting PD catheter connections to alternate PD delivery systems. https://rtg-education.fmcna.com/wp-content/uploads/2021/11/101419-01_Adapting-PD-Catheter-Connections.pdf
Disclaimer:
Use of Course Content. The courses provided by NCC are based on industry knowledge and input from professional nurses, experts, practitioners, and other individuals and institutions. The information presented in this course is intended solely for the use of healthcare professionals taking this course, for credit, from NCC. The information is designed to assist healthcare professionals, including nurses, in addressing issues associated with healthcare. The information provided in this course is general in nature and is not designed to address any specific situation. This publication in no way absolves facilities of their responsibility for the appropriate orientation of healthcare professionals. Hospitals or other organizations using this publication as a part of their own orientation processes should review the contents of this publication to ensure accuracy and compliance before using this publication. Knowledge, procedures or insight gained from the Student in the course of taking classes provided by NCC may be used at the Student’s discretion during their course of work or otherwise in a professional capacity. The Student understands and agrees that NCC shall not be held liable for any acts, errors, advice or omissions provided by the Student based on knowledge or advice acquired by NCC. The Student is solely responsible for his/her own actions, even if information and/or education was acquired from a NCC course pertaining to that action or actions. By clicking “complete” you are agreeing to these terms of use.
➁ Complete Survey
Give us your thoughts and feedback
➂ Click Complete
To receive your certificate
