Course
Pancreatic Cancer Updates
Course Highlights
- In this Pancreatic Cancer Updates
course, we will learn about the etiology and pathophysiology of Pancreatic Ductal Adenocarcinoma (PDAC). - You’ll also learn the impact of both modifiable and non-modifiable risk factors in PDAC.
- You’ll leave this course with a broader understanding of the latest advancements in immunotherapy, targeted therapies, genetic research, and the role of innovative diagnostic tools like circulating tumor DNA (ctDNA).
About
Contact Hours Awarded: 1
Course By:
R.E. Hengsterman MSN, RN
Begin Now
Read Course | Complete Survey | Claim Credit
➀ Read and Learn
The following course content
Introduction
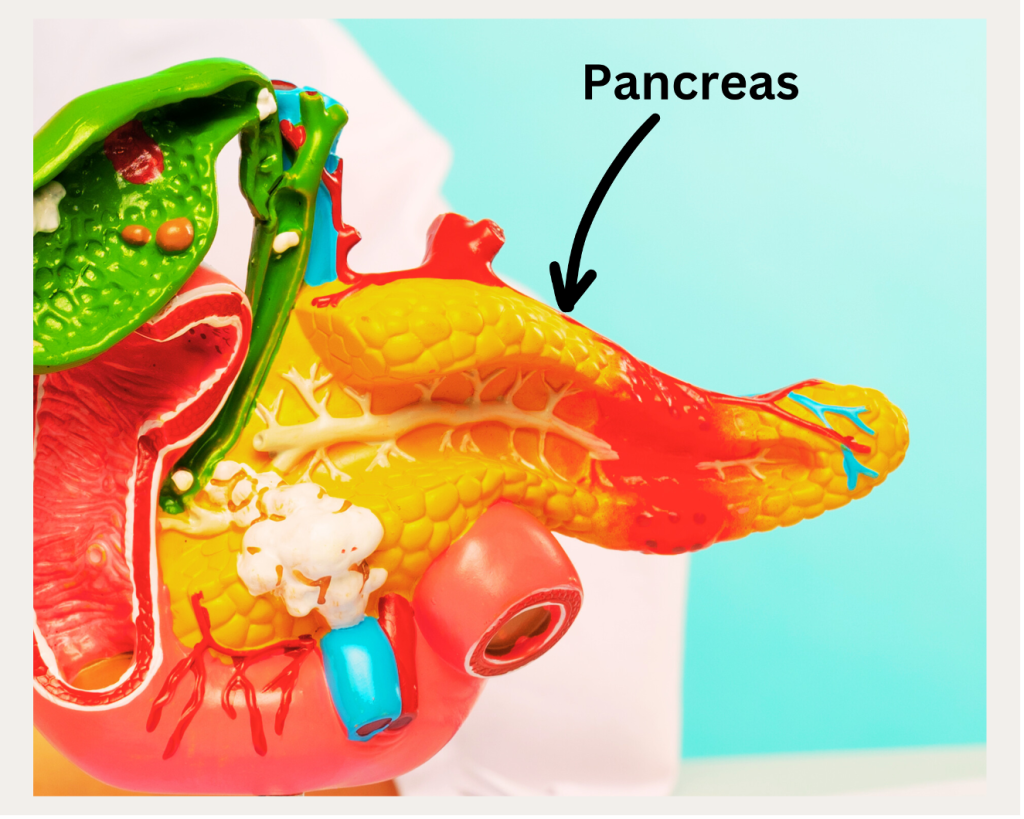
Pancreatic cancer presents formidable challenges in treatment, stemming from its affinity to spread, along with the unique biological properties of its tumors. Pancreatic ductal adenocarcinoma (PDAC), originating from pancreatic epithelial cells, stands as the predominant type of pancreatic cancer [1].
Pancreatic ductal adenocarcinoma (PDAC) ranks as the fourth leading cause of cancer-related fatalities across the globe, characterized by a low five-year overall survival rate of under 8% [1]. This increased mortality of pancreatic cancer, with its distinctive tumor microenvironment (TME), is characterized by a significant desmoplastic stromal microenvironment, a dense extracellular matrix, a range of activated cell types, hypoxic conditions, and an acidic extracellular pH make pancreatic cancer one of the most complex [2]. This active desmoplastic stroma poses challenges to effective treatment [2].
To combat pancreatic cancer, it is imperative to achieve total elimination of all cancer cells from the body [3]. This involves addressing both the primary tumor in the pancreas and any microscopic cancer cells that may have dispersed elsewhere. The most effective treatment for pancreatic cancer occurs through early detection [41].

Self Quiz
Ask yourself...
- Given that the unique tumor microenvironment (TME) of Pancreatic Ductal Adenocarcinoma (PDAC), including its desmoplastic stroma, contributes to treatment challenges, how might our understanding of this specific microenvironment inform the development of more effective treatment strategies?
- Considering the imperative of achieving total elimination of all cancer cells for effective treatment of pancreatic cancer, what implications does this have for the current methods of early detection and diagnosis, and how might advancements in these areas alter the course of treatment and survival rates?
The higher mortality rate associated with pancreatic cancer is due to two factors:
- Early Metastasis: Pancreatic cancer tends to metastasize at an early stage. In 85% of cases, the cancer has already spread beyond the pancreas at diagnosis [4].
- Genetic Reprogramming During Migration: As pancreatic cancer cells migrate to other organs including the liver, they undergo genetic changes that strengthen the underlying cell [4].
Effective pancreatic cancer treatment targets two primary aspects:
- Local Disease Management: Focused on the primary, or Stage 1, tumor in the pancreas. 10% of patients diagnosed early with pancreatic cancer achieve a disease-free status following treatment. The average survival time for pancreatic cancer is 3 to 3.5 years for patients diagnosed before the tumor grows or spreads [5].
- Systemic Disease Management: Cells from the pancreatic tumor can detach, enter the bloodstream, and circulate to distant organs, forming new tumors. Cancer cells tend to break away from the primary tumor, influenced by paracrine and autocrine signaling mechanisms [6]. These signals coordinate a multi-step process for the cancer cells, concluding in their establishment and colonization within distant tissues [6].
Case Study: Pancreatic Cancer Treatment and Staging
Patient Profile:
Name: John Doe
Age: 58 years
Medical History: Non-smoking, moderate alcohol use, no significant family history of cancer.
Presenting Complaint: The patient presents with a 2-month history of upper abdominal pain, unexplained weight loss, and jaundice.
Initial Assessment and Diagnosis:
Physical Examination: Noticeable jaundice, and mild abdominal tenderness.
Blood Tests: Elevated liver enzymes, CA 19-9 tumor marker levels.
Imaging: Abdominal CT scan reveals a mass in the head of the pancreas, no apparent liver metastases.
Diagnosis:
Based on clinical presentation and investigations, the patient receives a preliminary diagnosis of pancreatic cancer.
Staging:
MRI and endoscopic ultrasound (EUS) to assess local invasion and lymph node involvement.
PET scan to rule out distant metastasis.
Findings:
There is no evidence of distant spread with localized lymph node involvement noted.
Stage Determination:
Stage IIB (T3, N1, M0) – The tumor is advanced but without distant metastasis.
Treatment Plan:
Multidisciplinary Team (MDT) Consultation: Involves oncologists, surgeons, radiologists, and gastroenterologists.
Neoadjuvant Therapy: Given the local advancement, the treatment team opts for neoadjuvant chemotherapy to shrink the tumor and improve surgical outcomes.
Surgical Intervention: After reassessment, the patient undergoes a Whipple procedure (pancreaticoduodenectomy) to remove the tumor.
Adjuvant Therapy: Post-surgical chemotherapy combined with radiation therapy, to address any residual microscopic disease.
Follow-Up and Monitoring:
Regular follow-up visits, imaging, and CA 19-9 levels monitoring for early detection of recurrence.
Prognosis and Patient Education:
With vigilant monitoring, the patient’s prognosis is optimistic, considering the early stage and response to treatment.
Education: Patient education on post-surgical care, lifestyle modifications, and importance of follow-up assist the patient with coping after the diagnosis.
Conclusion:
This case study illustrates the importance of early detection and a comprehensive, multidisciplinary approach in the management of pancreatic cancer, considering current treatment and staging guidelines.

Self Quiz
Ask yourself...
- How does the early metastasis of pancreatic cancer, occurring in 85% of cases before diagnosis, challenge the current methodologies in early detection, and what innovations or changes might be necessary to detect and address metastasis at a more manageable stage?
- Given the role of genetic reprogramming during the migration of pancreatic cancer cells, how could a deeper understanding of these genetic changes inform the development of targeted therapies, particularly for systemic disease management?
- In light of the case study of John Doe, who received an early-stage diagnosis and a multidisciplinary treatment approach, what factors might contribute to replicating such successful early diagnoses in a broader patient population, considering the challenges posed by pancreatic cancer’s asymptomatic onset and rapid progression?
Statistical Evidence/Epidemiology
The global incidence of pancreatic cancer shows significant variation across different regions and populations [7]. Pancreatic cancer ranks as the twelfth most common cancer in men, the eleventh in women, and is the seventh leading cause of cancer-related deaths worldwide [8]. The risk of developing pancreatic cancer increases with age with most people who develop pancreatic cancer older than 45 [9]. 90% are older than 55 and 70% are older than 65 [9].
According to the International Agency for Research on Cancer’s (IARC) GLOBOCAN data, in 2018, there were 458,918 new cases and 432,242 deaths from pancreatic cancer across the globe, representing 2.5% of all new cancer cases and 4.5% of all cancer deaths [8].
There has been an increasing trend in pancreatic cancer incidence observed in recent decades, with projections suggesting a continued rise [10]. This increase factors in modifiable variables including tobacco use, obesity, diabetes, physical inactivity, and high calorie/fat diets in certain regions, alongside advancements in clinical diagnosis and an aging global population [9].
A 2023 review in the Journal Cell reports that pancreatic cancer has become the third leading cause of cancer-related deaths in the US, surpassing breast cancer in mortality rates [10]. Projections indicate that by 2040, pancreatic cancer will overtake colorectal cancer, becoming the second leading cause of cancer-related deaths in the US [10].
Pancreatic cancer incidence is three to four times higher in developed countries compared to developing ones. Europe and North America report the highest rates, while the lowest are in Africa and South-Central Asia [7]. In 2019, an estimated 56,770 new cases, and 45,750 deaths occurred [12]. Higher rates appear in Black populations compared to White, although the rate of increase is faster among Whites [13].
Researchers have discovered that pancreatic cancer rates are rising in both men and women [13]. In women under 55, the increase in rates was 2.4% higher compared to men in the same age group [13]. Similar trends of increased rates occur in older men and women. The rates in young Black women are 2.23% higher than those in young Black men [13].
In 2021, there was a slight gender difference in the incidence rates of pancreatic cancer, with the condition being more common in men at a rate of 5.5 per 100,000, representing 243,033 cases, compared to women, who had a rate of 4.0 per 100,000, amounting to 215,885 cases. [14].

Self Quiz
Ask yourself...
- What underlying factors might explain the significant regional and population variations in the incidence of pancreatic cancer and the higher rates in developed countries compared to developing ones?
- Considering the increase in pancreatic cancer incidence among younger populations and across genders, what implications does this have for current public health strategies and cancer screening protocols?
- Given the rising trend in pancreatic cancer incidence and its correlation with modifiable lifestyle factors such as diet, obesity, and physical inactivity, how might public health policies be adapted to address these risk factors?
- With the projection that pancreatic cancer will become the second leading cause of cancer-related deaths in the US by 2040, what strategic shifts in research funding and healthcare resource allocation might be necessary to meet the challenges posed by this anticipated increase?
Etiology/Pathophysiology
Extensive research, including various meta-analyses and pooled studies, has identified a spectrum of risk factors associated with pancreatic cancer. These factors fall into two categories: those that are modifiable and those that are non-modifiable.
Modifiable Risk Factors:
Smoking: A leading environmental factor for pancreatic cancer, with the risk increasing with the duration and intensity of smoking. Smokers have twice the risk of developing pancreatic cancer compared to non-smokers [15]. Smoking is responsible for up to 25% of pancreatic cancer cases [15].
Alcohol: High alcohol consumption (more than three drinks per day) increases the risk of pancreatic cancer, in combination with smoking [16].
Obesity: Linked to an increased risk of various cancers, including pancreatic cancer, with studies showing higher incidence and mortality rates among obese individuals [17].
Dietary Factors: The consumption of red and processed meats, fried foods, and foods high in cholesterol and nitrosamines elevates the risk of pancreatic cancer [18]. A diet rich in fruits and vegetables may offer protective benefits [19].
Occupational Exposures: Patients with occupational and environmental contact with cadmium, arsenic, lead, selenium, nickel, and chromium have a heightened risk of exocrine pancreatic cancer (EPC) [20].
Non-modifiable Risk Factors:
Gender: Pancreatic cancer is more prevalent in men than women [8].
Age: Most common among individuals over 50 years of age [9].
Ethnicity: Incidence rates vary among different ethnic groups, with African Americans showing higher rates than Caucasians [13].
Diabetes Mellitus: Both types I and II diabetes are associated with an increased risk of pancreatic cancer [15].
Family History and Genetic Factors: Familial history and genetic mutations account for a significant percentage of pancreatic cancer cases [15].
Infections: Certain chronic infections, such as H. pylori, have been associated with an increased risk of pancreatic cancer [22].
ABO Blood Group: Researchers evaluated the data and when compared to type O those individuals with type A blood had a 32% increased risk of developing pancreatic cancer, those with type AB had a 51% higher risk, and those with type B faced a 72% greater risk [23].
Genetic Cause: Ten percent of patients have genetic mutations or associations with syndromes such as Lynch syndrome, Peutz-Jeghers syndrome, Von Hippel-Lindau Syndrome, and MEN1 (multiple endocrine neoplasia type 1) [24].
Pancreatic adenocarcinoma and its variants represent about 90% of all pancreatic cancer types. 60%-70% of pancreatic adenocarcinomas originate in the pancreas’s head, while the body and tail each account for about 15% of cases [29].
Pancreatic cancer may originate as adenocarcinoma, serous, seromucinous, or mucinous types and its development is a complex process that involves intricate interactions between tumor cells and their surrounding environment, accompanied by a range of molecular changes [21]. These dynamic interactions and modifications play a vital role in both the initiation and advancement of the disease.
PDAC (Pancreatic Ductal Adenocarcinoma) develops from curable noninvasive precancerous lesions if detected and treated early [25]. The classification of these lesions is based on size and involvement with the pancreatic ductal system. Most PDACs originate from PanIN (pancreatic intraepithelial neoplasia), microscopic neoplasms affecting pancreatic ducts smaller than 5 mm [25]. A smaller proportion (<10%) of PDACs come from IPMNs (intraductal papillary mucinous neoplasms), which are macrocystic lesions involving the ductal system [25].
The tumor microenvironment (TME) plays a critical role in the development of pancreatic cancer (PC) and the failure of treatments [26]. Pancreatic tumors consist not just of tumor cells but also of various cell types like fibroblasts, immune cells, and endothelial cells [27]. Pancreatic tumor cells can induce epigenetic modifications in cancer-associated fibroblasts (CAFs), such as DNA methylation of the SOCS1 gene, which in turn promotes tumor growth [28].

Self Quiz
Ask yourself...
- How might the identification and modification of modifiable risk factors, such as smoking and diet, impact the overall incidence and prognosis of pancreatic cancer, and what strategies could be employed to reduce these risks in the general population?
- Considering the significant role of non-modifiable risk factors like age, gender, and ethnicity in pancreatic cancer, how could this knowledge influence targeted screening and prevention strategies to identify high-risk individuals?
- Given the complexity of pancreatic cancer’s etiology, involving interactions between tumor cells and the tumor microenvironment, what implications does this have for the development of new therapeutic approaches that target not just the tumor cells but also the microenvironment?
- What advancements in early detection and diagnostic methods help identify these lesions, thereby increasing the rate of successful treatment outcomes?
Diagnostic and Screening tools
Ongoing research focuses on developing and utilizing innovative blood tests, diagnostic imaging techniques, and other methods to identify pancreatic cancer in its initial stages before it can spread [30]. This effort includes detecting precancerous stages, such as pancreatic intraepithelial neoplasia (PanIN lesions) [29].
These screening methods are employed for individuals at elevated risk of developing pancreatic cancer including those with a significant family history or known genetic predispositions to the disease. There are no established screening tests that can detect pancreatic cancer in its initial stages, before the onset of symptoms [30].

Self Quiz
Ask yourself...
- Considering the current limitations in detecting pancreatic cancer in its initial stages and the focus on developing new screening methods for high-risk individuals, how might advancements in blood tests and imaging techniques improve the early detection of asymptomatic pancreatic cancer, thereby altering the course and prognosis of the disease?
Medication Management
Cancer researchers are exploring several types of immunotherapies as potential treatments for pancreatic cancer, including cancer vaccines made from various sources like pancreatic cancer cells, bacteria, or a person’s specific tumor cells, administered during various stages of treatment [31]. Immune checkpoint inhibitors, such as anti-PD-1 antibodies, already approved for other cancers, are under investigation for pancreatic cancer in patients with high microsatellite instability [32]. Targeted therapies approved for pancreatic cancer include erlotinib, olaparib, larotrectinib, and entrectinib, with ongoing research into drugs that block tumor growth in those targeting the KRAS gene and its mutations, and strategies to inhibit autophagy and break down tumor-associated stroma to enhance chemotherapy effectiveness [33].
Targeted therapies for pancreatic cancer focus on various approaches including Ras-Directed Therapies that alter RAS genes, are pivotal in cell growth signaling, and exist in over 90% of pancreatic cancers [30].
Pancreatic cancer can evade the immune system through several strategies, such as its immunosuppressive, dense fibrotic tumor microenvironment, and low tumor mutational burden [34]. Immunotherapy holds promise in eradicating cancer cells by reactivating the body’s cancer-fighting immune response with Pembrolizumab (Keytruda), an immune checkpoint inhibitor targeting pancreatic cancer patients with high microsatellite instability (MSI) [34].

Self Quiz
Ask yourself...
- How might the development of immunotherapies including those utilizing cancer vaccines and immune checkpoint inhibitors, transform the treatment landscape for pancreatic cancer considering its ability to evade the immune system?
- Given the prevalence of RAS gene mutations in pancreatic cancer, how could the advancement of Ras-Directed Therapies target and change the prognosis for the majority of pancreatic cancer patients?
- In light of the challenges posed by pancreatic cancer’s immunosuppressive tumor microenvironment and low tumor mutational burden, what strategies could enhance the effectiveness of immunotherapies in overcoming these barriers to treat pancreatic cancer?
Common Misconceptions
There are several misconceptions about pancreatic cancer, some of which include the common idiom that pancreatic cancer is a death sentence. While pancreatic cancer can be aggressive and difficult to treat if diagnosed late, advances in treatment and early detection are improving outcomes for some patients [25].
There is the misconception that only individuals with a family history get pancreatic cancer. Though a family history of pancreatic cancer can increase risk, most cases occur in people without a known family history [38].
Many believe pancreatic cancer is symptomless. In truth, early-stage pancreatic cancer often does not cause symptoms, which makes diagnosis difficult. Symptoms such as jaundice, abdominal pain, pancreatitis, new onset unexplained weight loss, and changes in stool can be indicative of pancreatic cancer [39].
You cannot reduce your risk of Pancreatic Cancer: Certain lifestyle factors, including smoking, obesity, and a diet high in processed and red meats, can increase the risk of developing pancreatic cancer. Reducing these risk factors can lower the risk [19].
Pancreatic Cancer Only Affects Older Adults: While the risk of pancreatic cancer increases with age, it can affect younger adults as well [9].
All Pancreatic Tumors are the Same: There are diverse types of pancreatic cancer, such as adenocarcinoma and neuroendocrine tumors, which behave differently and may require different treatment approaches [21].

Self Quiz
Ask yourself...
- Considering the misconception that pancreatic cancer is often symptomless in the initial stages, how can healthcare professionals and public health initiatives better educate the public about the subtle signs and symptoms of pancreatic cancer to improve early detection rates?
- Given the variety of pancreatic tumors and their distinct behaviors, how might we develop personalized treatment approaches and communicate to patients and healthcare providers to address the specific characteristics of each type of pancreatic tumor?
Upcoming Research
Genetic and molecular studies in cancer focus on identifying and modifying damaged genes and proteins to control uncontrolled cell growth. Recent progress in tumor genetics has led to the identification of circulating tumor DNA (ctDNA) [36]. There is an increasing amount of evidence that highlights the effectiveness of these sensitive biomarkers in identifying residual disease, diagnosing recurrence, and facilitating the use of targeted and tumor-specific adjuvant treatments [37].
Through a simple blood draw or urine sample providers can analyze circulating tumor DNA (ctDNA), which is cancer cell-derived DNA found in the bloodstream [35] [36]. The study of ctDNA is gaining traction as a means to monitor tumor response to treatment, detect early signs of disease recurrence, and understand the disease’s resistance to current treatments.
Researchers have subjected pancreatic tumor samples to various molecular techniques including DNA sequencing and mutational analysis to detect genetic alterations [35]. The insights gained from these studies are crucial for developing new drugs targeting these genetic changes.

Self Quiz
Ask yourself...
- How might the growing use of circulating tumor DNA (ctDNA) in monitoring treatment response and detecting early recurrence transform the management of cancer in terms of personalized treatment plans and the early intervention of disease recurrence?
- Given the insights from molecular techniques like DNA sequencing and mutational analysis in understanding pancreatic cancer, what are the potential implications for the development of new targeted therapies, and how might these therapies address the unique genetic alterations found in the distinct types of pancreatic cancer?
- How might the integration of both modifiable and non-modifiable risk factor identification into public health initiatives and individual healthcare practices contribute to more effective prevention and early detection strategies for Pancreatic Ductal Adenocarcinoma (PDAC)?
- Considering the challenges of PDAC’s aggressive tumor microenvironment and genetic complexity, what multidisciplinary approaches could enhance the efficacy of current treatments, such as immunotherapy and targeted therapies, and how might these advancements change the prognosis for patients with PDAC?
Conclusion
Pancreatic Ductal Adenocarcinoma (PDAC), characterized by early metastasis, aggressive tumor microenvironment, and a propensity for genetic reprogramming during migration, is one of the deadliest cancer types [40]. The case study of John Doe exemplifies the crucial role of early detection and a multidisciplinary treatment approach, emphasizing the importance of both local and systemic disease management to achieve optimal outcomes.
The identification of both modifiable and non-modifiable risk factors provides avenues for preventive strategies and targeted interventions. In terms of treatment, advancements in immunotherapy, targeted therapies, and genetic research hold promise [36]. However, the challenges posed by the tumor’s microenvironment and genetic complexity continue to hinder effective treatment modalities. The exploration of innovative diagnostic tools like circulating tumor DNA (ctDNA) and molecular techniques in tumor analysis are pivotal in the early detection and personalized treatment of pancreatic cancer [36].
The fight against pancreatic cancer necessitates a concerted effort in research, early detection, comprehensive treatment strategies, and public education.
References + Disclaimer
- Siegel RL, Miller KD, Jemal A. Cancer statistics, 2018. CA Cancer J Clin. 2018;68(1):7–30.
- Carvalho, T. M. A., Di Molfetta, D., Greco, M. R., Koltai, T., Al Farouk, K. O., Reshkin, S. J., & Cardone, R. A. (2021). Tumor Microenvironment Features and Chemoresistance in Pancreatic Ductal Adenocarcinoma: Insights into Targeting Physicochemical Barriers and Metabolism as Therapeutic Approaches. Cancers, 13(23), 6135. https://doi.org/10.3390/cancers13236135
- Potential new therapies help outsmart pancreatic cancer. (2023, October 25). Johns Hopkins Medicine. https://www.hopkinsmedicine.org/health/conditions-and-diseases/pancreatic-cancer/potential-new-therapies-help-outsmart-pancreatic-cancer
- Pancreatic cancer discovery opens the door for new clinical trial at Wilmot. (2023, November 15). URMC Newsroom. https://www.urmc.rochester.edu/news/story/pancreatic-cancer-discovery-opens-the-door-for-new-clinical-trial-at-wilmot
- Pancreatic cancer prognosis. (2022, November 1). Johns Hopkins Medicine. https://www.hopkinsmedicine.org/health/conditions-and-diseases/pancreatic-cancer/pancreatic-cancer-prognosis
- Thomas, S. M., Lee, V., & Beatty, G. L. (2020). Paracrine and cell autonomous signaling in pancreatic cancer progression and metastasis. EBioMedicine, 53, 102662. https://doi.org/10.1016/j.ebiom.2020.102662
- Rawla, P., Sunkara, T., & Gaduputi, V. (2019). Epidemiology of Pancreatic Cancer: global trends, etiology, and risk factors. World Journal of Oncology, 10(1), 10–27. https://doi.org/10.14740/wjon1166
- Khalaf, N., El–Serag, H. B., Abrams, H. R., & Thrift, A. P. (2021). Burden of pancreatic Cancer: From Epidemiology to practice. Clinical Gastroenterology and Hepatology, 19(5), 876–884. https://doi.org/10.1016/j.cgh.2020.02.054
- Pancreatic cancer – risk factors. (2023, December 14). Cancer. Net. https://www.cancer.net/cancer-types/pancreatic-cancer/risk-factors
- Luo, W., Tao, J., Zheng, L., & Zhang, T. (2020). Current epidemiology of pancreatic cancer: Challenges and opportunities. Chinese Journal of Cancer Research, 32(6), 705–719. https://doi.org/10.21147/j.issn.1000-9604.2020.06.04
- LifeSciencesIntelligence. (2023, November 14). Advancements in pancreatic cancer screenings. LifeSciencesIntelligence. https://lifesciencesintelligence.com/features/advancements-in-pancreatic-cancer-screenings
- Goyal, S., Vojnic, M., Yang, J., Jose, J., Newman, E., & Saif, M. W. (2021). Neoadjuvant therapy (NAT) in localized pancreatic cancer: Should we do it and what should we do? Journal of Cellular Signaling, 2(1). https://doi.org/10.33696/signaling.2.037
- Thomson, F. (2023, February 13). Pancreatic cancer rates rising faster in women than men. Open Access Government. https://www.openaccessgovernment.org/pancreatic-cancer-rates-rising-faster-women-men/153015/
- Hu, J., Zhao, C., WenBiao, C., Liu, Q., Li, Q., Lin, Y., & Gao, F. (2021). Pancreatic cancer: A review of epidemiology, trend, and risk factors. World Journal of Gastroenterology, 27(27), 4298–4321. https://doi.org/10.3748/wjg.v27.i27.4298
- Pancreatic cancer risk factors. (2024). American Cancer Society. https://www.cancer.org/cancer/types/pancreatic-cancer/causes-risks-prevention/risk-factors.html
- Alcohol and Cancer risk fact sheet. (2021, July 14). National Cancer Institute. https://www.cancer.gov/about-cancer/causes-prevention/risk/alcohol/alcohol-fact-sheet
- Pati, S., Irfan, W., Jameel, A. T., Ahmed, S., & Shahid, R. (2023). Obesity and Cancer: A Current overview of epidemiology, pathogenesis, outcomes, and management. Cancers, 15(2), 485. https://doi.org/10.3390/cancers15020485
- Sun, Y., He, X. T., & Sun, Y. (2023). Red and processed meat and pancreatic cancer risk: a meta-analysis. Frontiers in Nutrition, 10. https://doi.org/10.3389/fnut.2023.1249407
- Ibrahim, M. O., Abuhijleh, H., & Tayyem, R. (2023). What Dietary Patterns and Nutrients are Associated with Pancreatic Cancer? Literature Review. Cancer Management and Research, Volume 15, 17–30. https://doi.org/10.2147/cmar.s390228
- Camargo, J., Pumarega, J., Alguacil, J., Sanz-Gallén, P., Gasull, M., Delclos, G. L., Amaral, A., & Porta, M. (2019). Toenail concentrations of trace elements and occupational history in pancreatic cancer. Environment International, 127, 216–225. https://doi.org/10.1016/j.envint.2019.03.037
- Puckett, Y. (2022, September 26). Pancreatic cancer. StatPearls – NCBI Bookshelf. https://www.ncbi.nlm.nih.gov/books/NBK518996/
- Zhou, B., Mei, Y., Wang, J., Xia, J., Jiang, X., Ju, S., & Ding, Y. (2023). Is Helicobacter pylori infection associated with pancreatic cancer? A systematic review and meta-analysis of observational studies. Therapeutic Advances in Chronic Disease, 14, 204062232311551. https://doi.org/10.1177/20406223231155119
- Weaver, C., MD. (2023, November 7). Blood type linked to risk of pancreatic cancer. CancerConnect. https://news.cancerconnect.com/pancreatic-cancer/blood-type-linked-to-risk-of-pancreatic-cancer
- Carrera, S., Sancho, A., Azkona, E., Azkuna, J., & López-Vivanco, G. (2017). Hereditary pancreatic cancer: related syndromes and clinical perspective. Hereditary Cancer in Clinical Practice, 15(1). https://doi.org/10.1186/s13053-017-0069-6
- Wood, L. D., Canto, M. I., Jaffee, E. M., & Simeone, D. M. (2022). Pancreatic cancer: pathogenesis, screening, diagnosis, and treatment. Gastroenterology, 163(2), 386-402.1. https://doi.org/10.1053/j.gastro.2022.03.056
- Khan, M. A., Azim, S., Zubair, H., Bhardwaj, A., Patel, G. K., Khushman, M., Singh, S., & Singh, A. P. (2017). Molecular Drivers of Pancreatic Cancer Pathogenesis: Looking inward to move forward. International Journal of Molecular Sciences, 18(4), 779. https://doi.org/10.3390/ijms18040779
- Murakami, T., Hiroshima, Y., Matsuyama, R., Homma, Y., Hoffman, R. M., & Endo, I. (2019). Role of the tumor microenvironment in pancreatic cancer. Annals of Gastroenterological Surgery, 3(2), 130–137. https://doi.org/10.1002/ags3.12225
- Cellular & Molecular immunology. (2023, March 22). Nature. https://www.nature.com/cmi/
- McGuigan, A., Kelly, P., Turkington, R., Jones, C., Coleman, H., & McCain, R. S. (2018). Pancreatic cancer: A review of clinical diagnosis, epidemiology, treatment, and outcomes. World Journal of Gastroenterology, 24(43), 4846–4861. https://doi.org/10.3748/wjg.v24.i43.4846
- Advances in pancreatic cancer research. (2023, August 31). National Cancer Institute. https://www.cancer.gov/types/pancreatic/research
- Pancreatic cancer – latest research. (2023, December 18). Cancer. Net. https://www.cancer.net/cancer-types/pancreatic-cancer/latest-research
- Eso, Y., & Seno, H. (2020). Current status of treatment with immune checkpoint inhibitors for gastrointestinal, hepatobiliary, and pancreatic cancers. Therapeutic Advances in Gastroenterology, 13, 175628482094877. https://doi.org/10.1177/1756284820948773
- Luo, J. (2021). KRAS mutation in pancreatic cancer. Seminars in Oncology, 48(1), 10–18. https://doi.org/10.1053/j.seminoncol.2021.02.003
- Yoon, J., Jung, Y., & Moon, S. (2021). Immunotherapy for pancreatic cancer. World Journal of Clinical Cases, 9(13), 2969–2982. https://doi.org/10.12998/wjcc.v9.i13.2969
- Takano, S., Fukasawa, M., Shindo, H., Takahashi, E., Fukasawa, Y., Kawakami, S., Hayakawa, H., Kuratomi, N., Kadokura, M., Maekawa, S., & Enomoto, N. (2021). Digital next‐generation sequencing of cell‐free DNA for pancreatic cancer. JGH Open, 5(4), 508–516. https://doi.org/10.1002/jgh3.12530
- What is circulating tumor DNA and how is it used to diagnose and manage cancer? MedlinePlus Genetics. (2024). https://medlineplus.gov/genetics/understanding/testing/circulatingtumordna/
- Reece, M., Saluja, H., Hollington, P., Karapetis, C. S., Vatandoust, S., Young, G. P., & Symonds, E. L. (2019). The use of circulating tumor DNA to monitor and predict response to treatment in colorectal cancer. Frontiers in Genetics, 10. https://doi.org/10.3389/fgene.2019.01118
- Pancreatic cancer risk factors. (2023, October 30). Johns Hopkins Medicine. https://www.hopkinsmedicine.org/health/conditions-and-diseases/pancreatic-cancer/pancreatic-cancer-risk-factors
- Pancreatic Cancer Action Network. (2023, November 29). Signs and symptoms of pancreatic cancer – Pancreatic Cancer Action Network. https://pancan.org/facing-pancreatic-cancer/symptoms/
- Palamaris, K., Felekouras, E., & Sakellariou, S. (2021). Epithelial to mesenchymal transition: key regulator of pancreatic ductal adenocarcinoma progression and chemoresistance. Cancers, 13(21), 5532. https://doi.org/10.3390/cancers13215532
- Pancreatic Cancer Action Network. (2023, November 29). Early Detection – Pancreatic Cancer Action Network. https://pancan.org/facing-pancreatic-cancer/diagnosis/early-detection/
Disclaimer:
Use of Course Content. The courses provided by NCC are based on industry knowledge and input from professional nurses, experts, practitioners, and other individuals and institutions. The information presented in this course is intended solely for the use of healthcare professionals taking this course, for credit, from NCC. The information is designed to assist healthcare professionals, including nurses, in addressing issues associated with healthcare. The information provided in this course is general in nature and is not designed to address any specific situation. This publication in no way absolves facilities of their responsibility for the appropriate orientation of healthcare professionals. Hospitals or other organizations using this publication as a part of their own orientation processes should review the contents of this publication to ensure accuracy and compliance before using this publication. Knowledge, procedures or insight gained from the Student in the course of taking classes provided by NCC may be used at the Student’s discretion during their course of work or otherwise in a professional capacity. The Student understands and agrees that NCC shall not be held liable for any acts, errors, advice or omissions provided by the Student based on knowledge or advice acquired by NCC. The Student is solely responsible for his/her own actions, even if information and/or education was acquired from a NCC course pertaining to that action or actions. By clicking “complete” you are agreeing to these terms of use.
➁ Complete Survey
Give us your thoughts and feedback
➂ Click the Green MARK COMPLETE Button Below
To receive your certificate
