Course
Simulation Based Learning in Clinical Settings
Course Highlights
- In this Simulation Based Learning in Clinical Settings course, we will learn about examples of high, mid, and low fidelity types of simulation in clinical learning environments.
- You’ll also learn how the concepts of pre-briefing and debriefing can be used to enhance learning and application of knowledge.
- You’ll leave this course with a broader understanding of the relationship between knowledge development, competency, and skill performance.
About
Contact Hours Awarded: 2
Course By:
Abbie Schmitt
RN, MSN-Ed
Begin Now
Read Course | Complete Survey | Claim Credit
➀ Read and Learn
The following course content
Introduction
Within the ever-evolving realm of nursing education, simulation-based learning has become increasingly recognized as an essential part of nursing education programs. Simulation-based learning is characterized by realistic scenarios and interactive technologies.
Simulation is designed to bridge the gap between theoretical knowledge and real-world clinical experiences. It is important to explore existing literature on types of simulation, models for pre-briefing and debriefing, competency assessments, and feedback, and relay these findings to educators, researchers, and policymakers in an effort to advance nursing education and ultimately improve patient outcomes.
Definition
Clinical simulation is simply defined as an attempt to mimic real life situations to apply knowledge and theory to practice. It is a teaching method in which, following a strategic scenario, students experience the actual dimensions of their future professional roles, which can help them to act more quickly and appropriately (6).
Effective simulation can enrich the critical thinking skills of students. Students are able to put the information they have been taught into practice within a controlled environment, cope with any hurdles, and make mistakes without causing harm to patients. This technique can help to minimize errors and enhances students’ self-confidence, self-esteem, and comfort in skill performance.
Evidence supports the importance of simulation and has been demonstrated in aviation, aerospace, and surgery (3). There is overwhelming evidence that student clinical experiences in nursing curriculum results in improved understanding of nursing practice.

Self Quiz
Ask yourself...
- Are you familiar with the various types of learning, such as visual, auditory, and psychomotor?
- Can you think of reasons a controlled environment can have better outcomes for safety?
- What are some basic nursing skills that could be taught using simulation learning?
- Are there other fields, such as aviation, that benefit from simulation-based learning?
Types of Simulation
There are three types of simulation-based activities: low-fidelity simulation (LFS), mid-fidelity simulation (MFS), and high-fidelity simulation (HFS). Fidelity can be defined as “adherence to fact or detail”; if the likeness of an experience to real-life is greater, the fidelity will be higher. Fidelity is the route of the Latin word fidelitas, which means the degree to which something is copied or reproduced.
Clinical Simulation Terms
There are several key simulation terms and definitions that are used among the clinical simulation community and educators. Important terms include manikin, patient simulator, virtual patient, standardized patient, remote simulation, artificial intelligence (AI), augmented reality, and serious gaming.
- Manikin – A life-sized human-like simulator representing a patient for health care simulation and education
- Full or partial body representation of a patient for practice.
- Full or partial body simulators that can have varying levels of physiologic function and fidelity.
- Patient Simulator – Life-like, anatomically correct manikin with physiologic responses that mimic real patients.
- High- or low-fidelity full-body manikins controlled by instructors to create a structured learning environment in a realistic setting
- Learning can take precedence over patient care
- Virtual Patient – A representation of an actual patient such as software-based physiological simulators, simulated patients, physical manikins, and simulators
- The computer program simulates real-life clinical scenarios in which the learner acts as a health care provider
- Standardized Patient (SP) - An individual who has been carefully coached to simulate an actual patient.
- SPs can be used for teaching and assessment of learners, including but not limited to history/consultation, physical examination, and other clinical skills in simulated clinical environments.
- SPs can also be used to give feedback and evaluate learner performance
- An individual who is trained to portray a real patient in order to simulate a set of symptoms or problems used for healthcare education, evaluation, and research
- The Association of Standardized Patient Educators (ASPE) is a terrific resource for educators.
- Remote Simulation - Simulation performed with either the facilitator, learners, or both in an offsite location separate from other members
- Can be synchronously or asynchronously utilizing video or web conferencing tools.
- Artificial Intelligence (AI) – A system of computerized data-gathering and predictions that simulates human behavior and decision-making independently of humans. In healthcare simulation, AI often refers to programming that provides physiological or system-based algorithm changes based on inputs from users and learners. (2)
- Augmented Reality – A type of virtual reality in which synthetic stimuli and visuals are superimposed on real-world objects.
- Helpful in delivering information that is otherwise imperceptible to human senses.
- Forms of virtual reality include head-mounted displays, overlays of computer screens, wearable computers, or displays projected onto humans and manikins. (2)
- Serious Games – Games designed for learning purposes and engagement rather than pure entertainment.
- Serious games have carefully thought-out simulations of real-world events or processes designed for the purpose of solving a problem.
- Gaming is used as an effective education tool in industries like scientific exploration, emergency management, city planning, and engineering. (2)
Educator Tip: Do not be afraid to be imaginative, silly, and dramatic. Imagine each student as an impressionable learner who will one day be a pilot of nursing practice. Use all creative and technological tools available to encourage learning and critical thinking skills.

Types of Fidelity
- Conceptual fidelity - Does this scenario make sense and actually depicts situations in the real world.
- Lab work, diagnostics, and medications should be consistent with the signs and symptoms the patients are exhibiting.
- Example: The patient simulator that exhibits rapid heart rate and hypotension during a simulation experience on caring for a patient with septicemia (sepsis) and responds appropriately to ordered medications.
- Physical fidelity - The degree to which the simulator duplicates the appearance and feel of the anatomy of real patients.
- Emotional or Psychological fidelity – The extent in which a simulation can mimic the real task and make the learner feel as if it is real.

Self Quiz
Ask yourself...
- Can you think of examples of low and high-fidelity manikins?
- Do you have experience working in simulated events within your workplace?
- What are some ways educators can enhance emotional fidelity within scenarios?
- Have you noticed that artificial intelligence (AI) has been a topic of discussion within our society recently?
Low Fidelity Simulation (LFS)
The simulations in this category will feel less real to the learner. Equipment can include stationary models, two-dimensional displays, and unrealistic synthetic body parts. These simulations can be designed for specific task or procedures such as IV arms or CPR manikins.
Low-fidelity simulation experiences are relatively easier to implement, less expensive, and often less time consuming (4).
A major misconception is that low-fidelity simulation is not as important as the simulations with more realistic features. This is misleading because a foundation of knowledge and comprehension is essential to learning success in high-fidelity simulations.
In 1990, George Miller outlined a model for the assessment of clinical competency, referred to as “Miller Pyramid” (13). Miller argued that clinical competency among students should not be strictly knowledge-based assessments through examinations but should incorporate how they would react in a real-life situation (13).
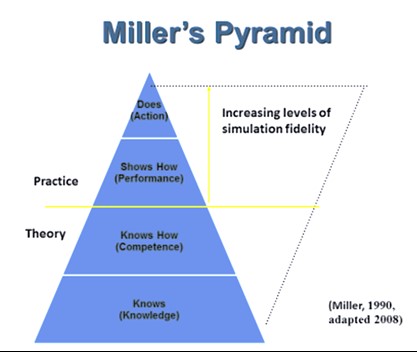
Figure 1. Miller’s Pyramid: Model for Assessment of Clinical Competency (14)
Low-fidelity simulations are critical in the theoretical portion of learning and obtaining basic knowledge. Some LFS may incorporate real-life equipment, but the experience does not feel as real to the students.
For example, models or two-dimensional displays showing the anatomy of the heart can build understanding of the heart chambers, valves, and directionality of blood flow. Diagrams showing signs and symptoms of heart failure can further enhance the learner’s knowledge of the disease process. This foundation of knowledge is critical for building complex understanding and critical thinking skills.
Another example of a LFS is a simulation to enhance the understanding of EKG interpretation and discussion. The EKG equipment could be authentic, but the simulation excludes the other real-life environmental factors.
The removal of high stressors, such as an unconscious simulated patient or loud alarms, can allow students to interpret the rhythm and comprehend the correlating factors. Later in the learning process, a high-fidelity simulation can incorporate these skills and further enhance understanding.

Self Quiz
Ask yourself...
- Can you name examples of low-fidelity equipment and simulators?
- Do you consider it difficult to comprehend information during a stressful situation?
- What is typically less expensive to simulate- a low or high-fidelity situation?
- Are you familiar with various theoretical learning models?
High Fidelity (HFS)
Have you ever visited a planetarium? One that you go into a large room with dark lighting and projected images of planets, stars, and nebula all around you. The goal is to imitate traveling to the outer universe to create that meaningful experience. It is extremely different than hearing a description or looking at a poster image.
Nursing instructors attempt to do this same thing in HFS with nursing students. The sights, sounds, and reactions are created as an attempt to transport each nursing student to a situation they could experience in their future career.
When you hear high fidelity in simulated health care, think replication. This involves getting as close as possible to the real-life scenario. In HFS, nursing students work with manikins that have features that are similar to real patients; their voices, body structure, anatomical landmarks, skin color, along with many other features based on the manufacturer. A Simulated Patient (SP) can also be used. SP is essentially a real person who is an actor in the created experience. These can be professional actors, students, faculty, or volunteers that receive training to simulate symptoms or problems that a real patient might have or act as a family member of simulated patient.
High-fidelity simulations extend beyond the simulator manikin and includes the surroundings, equipment, and modes of communication, to help learners become fully immersed in the experience.
These experiences are highly impacted by technology, but not dependent on it.
Instructors often communicate and interact with the learners throughout the experience and often utilize unfolding case studies. Students are coached to take everything as seriously and realistically as possible when working with a simulator patient during a simulation (9).
Instructors often control the mannequins and observe from a nearby area or act as a fellow health care team member or patient family member.
Within a faculty-created scenario, students are able to practice skills, including tracheostomy care, wound care, urinary catheterization care, CPR, injections, chest tube insertion, and shocking of the heart to name a few. More importantly, they learn to assess, plan care, react to changes in their patients and the environment, problem solve, and think critically.
High-fidelity Manikins
Learners can perform physical examinations to determine their condition, recognize deterioration, or monitor their improvement. These manikins have assessable vital signs and various unique humanistic features, making it possible to complete physical examination components like vital signs (heart rate, respiratory rate, and blood pressure) and assessment of the patient’s head, neck, abdomen, limbs, heart, and lungs. Manikin operators can manipulate all of these parameters to learn the differences between normal and abnormal findings, various health conditions, and disease states.
The manikins are sometimes equipped with a wireless microphone and programmed with select sounds and phrases enabling them to communicate during a scenario, including life-like breath sounds, heart sounds, and lung sounds. Many of these manikins have palpable pulses, visual capillary refill, and responsive pupils.
The results of simulation studies have found that HFS is an impactful teaching-learning tool to augment nursing students’ clinical competence, confidence, critical thinking, knowledge, clinical reasoning, communication skills, motivation, and clinical judgment (8).
Empirical evidence has identified HFS as an effective teaching strategy to compliment foundational competencies and translate theoretical nursing into practice (8).
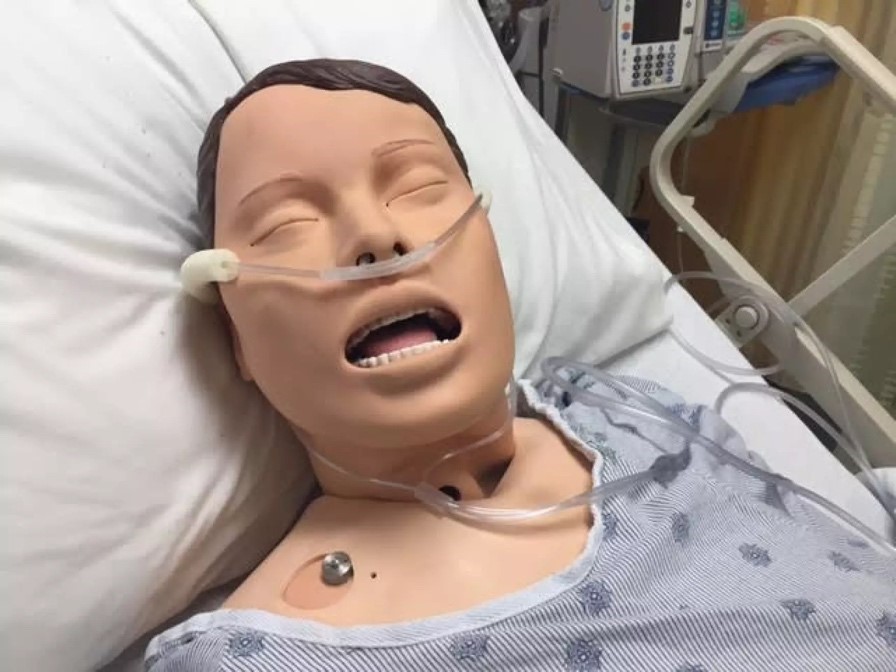
Image 1. Simulation Manikin (9)

Self Quiz
Ask yourself...
- Can you name parts of the physical assessment that can be completed on a simulator manikin?
- How is technology incorporated into high-fidelity simulations?
- Should students be encouraged to act as if the simulation is real or pretend?
- What are ways educators can make the clinical environment seem more real in HFS?
Advantages/ Benefits
Major benefits of simulation-based learning in clinical settings is enrichment of learning, increased safety for patients, stronger confidence in students, and support for educators facing barriers to clinical site experiences.
Enrichment of Learning
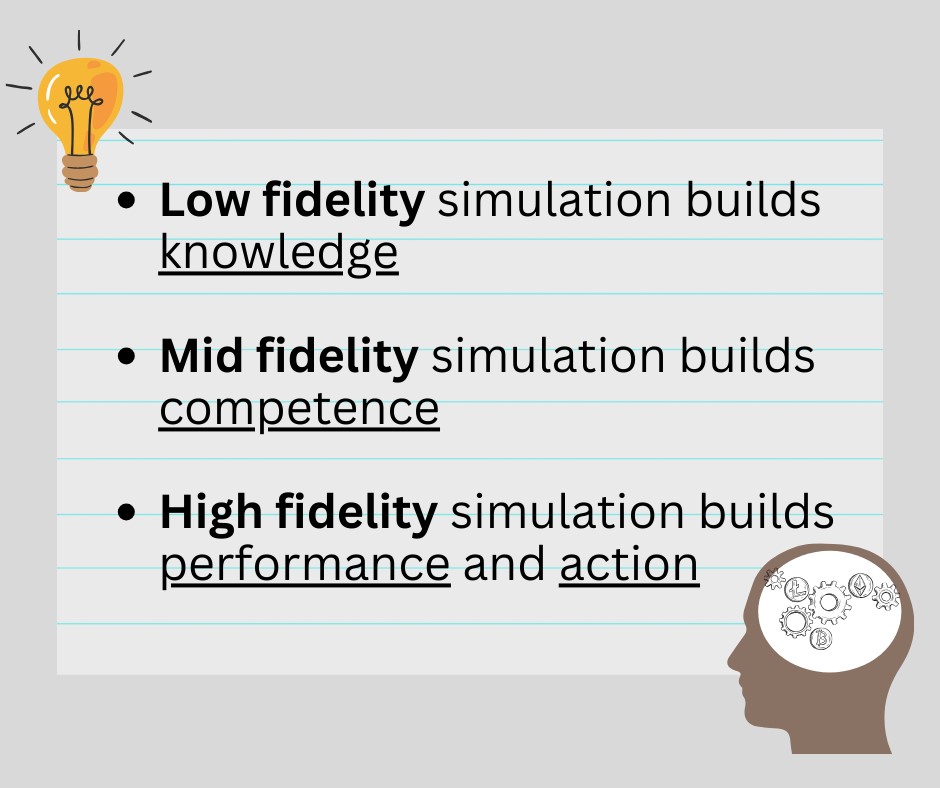
The goal of enhanced learning is a huge benefit of simulation-based learning. Each type of fidelity is important to the development of students.
Low fidelity simulation helps to build foundational knowledge. Although the learner may not feel as they are in the actual clinical setting, they will be able to focus on gaining knowledge.
Mid fidelity simulation builds the essential component of competence. These simulations allow more opportunities for learning and applying knowledge. This can include a manikin that mimics breath sounds, bowel sounds and heart sounds and allow students to perform procedures such as IV insertions, injections, NG tube insertion, tracheostomy suctioning and Foley catheter insertions. The structure of the manikin is similar to real patients, but they do not function and respond to interventions, and likely the students always feel like it is just a manikin.
High fidelity simulation builds performance and action. These simulations maximize the realness of a clinical experience. These are full body computerized manikins with the anatomy and physiology of a real patient, have the ability to communicate, and allow educators to run pre-programmed scenarios.
Some educators may feel the low-fidelity simulations have less meaning, however, there are many benefits. In low-fidelity experiences, many physical elements from the scenario are removed, and the focus is shifted to critical thinking in the clinical decision-making process. Essentially, the educator would use LFS experiences to reduce the learners’ cognitive load to provide clarity on the desired outcomes of the scenario. An example would be a scenario with a patient
Building Patient Safety Culture and Prevention of Adverse Events
Patient safety is a major benefit. If a nursing student makes a mistake within the field, it can result in serious harm to patients. If the mistake is initially made in the simulated environment, then discussed and evaluated, a similar mistake can hopefully be avoided in the future.
Simulation experiences can be used to build a mindset to focus on patient safety and the evidence-based research topics that build a patient safety culture.
Research has determined the following seven subcultures of patient safety culture: (1) leadership, (2) just, (3) teamwork, (4) evidence-based, (5) communication, (6) patient-centered, and (7) learning (4).
- Leadership – The learners will gain insight on how leadership can impact patient safety. Leaders that are dedicated to patient safety can create an attitude that permeates through all levels of an organization (4).
Simulation Topic Example: Assign leadership and administrative roles among the students to encourage the development and implementation of a safety protocol (safety checks or patient identification protocols).
- Just – A just culture describes an error prevention method that includes personal accountability and system effectiveness (4).
Simulation Topic Example: A major topic of safety among educators is instilling the importance of patient identification. It can seem like a simple step, but possibly one of the most crucial. This is the process of “correctly matching a patient to appropriately intended interventions and communicating information about the patient’s identity accurately and reliably throughout the continuum of care” (11).
During a simulated experience, if a student forgets to appropriately identify the patient, the educator can let the case unfold as if this were the incorrect patient. For example, the student has an order to administer a cardiac medication, the instructor could let this unfold into simulation of abnormal findings in vital signs or EKG rhythms, the frustration among the family members and healthcare team, and ultimately serious harm to the patient.
During the debriefing, the instructor should ask the learner, “what actions would you do differently in the future” and “what organizational policy or procedure could be implemented to help avoid situation”?
- Teamwork and Communication – Involves open and respectful collaboration among the healthcare team members.
Simulation Topic Example: Practice for nursing handoff reports, delegation, closed-loop communication, etc.
- Evidence-Based – This includes application of protocols and checklists to standardized care. Learners must gain understanding that evidence and research is a major factor in the development of protocols within an organization and they must follow these to ensure the most therapeutic care.
Simulation Topic Example: Educators could do a simulation for learners to perform a peripherally inserted central catheter (PICC) dressing change on a simulation manikin using a sample protocol. The educator could explain the outcome if any of these evidence-based practice steps were missed and simulate an infection or thrombosis in an effort to inspire protocol adherence.
- Patient-Centered Approach – Patient care should always include input and participation from patients. This can be encouraged through simulation through simulation on patient education and informed consent.
Simulation Topic Example: The learners have an experience of orders for blood administration based on a critical need in the simulation; however, this particular patient has specific cultural or religious beliefs that are extremely important to them, and they do not ever want to accept blood transfusion or blood products. The instructor should let this simulation unfold and allow the learners to provide patient education while also gaining a deep understanding of the patient’s right to autonomy.
- Learning – Evidence shows the significant benefits from learning from mistakes in the development of a patient safety culture (4).
Fostering Confidence and Self- Reflection in Learner
In the simulated experience, the students can be the nurse rather than the nursing student. Learners need to practice the role of the bedside nurse, to include making decisions, communicating with healthcare providers, documenting without a co-signer, and administering medications independently.
Simulation can be a powerful self-reflection tool for students.
The simulated environment should reduce stress and cognitive overstimulation in learners. Stress and pressure can serve as both a positive and negative motivator. Studies have found that clinical simulation typically reduces stress and anxiety among nursing students (7).
Support for Educators Facing Clinical Site Challenges
The use of simulation has also expanded as a solution to a lack of clinical opportunities for student training and shortage of clinical instructors in some nursing programs (6). If certain criteria are met, and specific regulations are adhered to, it is possible for students to meet clinical competency requirements through simulated clinical experiences. Educators are able to devote time and effort into many meaningful experiences, rather than hoping the students are able to observe and participate in a wide variety of situations within the real-life healthcare environment.

Self Quiz
Ask yourself...
- Can you name some benefits of simulation-based learning on patient safety?
- How can clinical setting simulation help educators who have a shortage of clinical sites and clinical instructors?
- What are the subcultures of a patient safety culture?
- Do you recognize the value in all types of fidelity in clinical simulation?
Pre-Briefing
Conducting a discussion before the simulation training has become a foundational part of the simulation experience (3). A briefing before the simulation serves to prepare and orient learners to the simulation experience.
If learners are given an adequate orientation and a psychologically safe environment, it lowers their fear and anxiety (3). Establishing expectations is a critical part of education and competency assessment. It is important to establish ground rules during the pre-brief period so that students understand expectations. They need to know it is okay to make mistakes, and that those mistakes will be discussed during debriefing, providing the opportunity to learn from the mistakes and explore ways to improve.
The pre-briefing before simulation has four key components:
- Provide Goals and Objectives
- Establish a fiction contract
- Explain logistic details about the experience to the learners
- Pledge to respect each learner
The first step of the pre-briefing is reviewing the goals and objectives. Instructors should review learning objectives, outline the sequence of events, familiarizing the learners with the simulation equipment and environment, and explaining the roles of the educators (3).
The second component is establishing a fiction contract with the learners. The educator is responsible for creating a scenario that is as real as possible to encourage engagement, the learners are responsible for fully engaging in the simulation and acting as if everything is real. Attitudes of silliness or disbelief should be firmly discouraged, as engagement in the realness is a key component.
The third step is providing logistic details about the session to the learners. These details include the length of the session, breaks, and how to manage telephone calls, texts, pages, and emails throughout the session.
The last component of pre-briefing is pledging to respect each learner’s experience. Actions during simulation should not be focused on correct or incorrect, but educators should inquire about the learner’s decision-making process and rationale behind their choices. This approach allows the educator to identify knowledge gaps and give meaningful feedback. Mutual respect and encouragement are key.

Self Quiz
Ask yourself...
- Can you discuss similarities between meetings prior to a simulated clinical environment and an actual clinical site?
- How can an orientation to the clinical setting reduce anxiety among learners?
- What are the four key components of the pre-briefing session?
- How can educators encourage learner engagement?
Tips for Increasing Fidelity and Realism in Simulation
- Choose the level and type of fidelity that is appropriate for the simulation as well as the appropriate scenario to maximize student learning.
- Remember, simulation is a learning exercise, not a punitive evaluation
- Instruct students to act exactly like a real-life setting
- Give a few minutes after report for the students to plan as a team before starting the scenario.
- Make it as real as possible. Use equipment used in the clinical setting.
- Apply sounds, smells, and visual components to make it real for the students when possible.
Competency Assessment
A major function and purpose of simulation is assessing student competency and performance. Although simulations encourage learning and comprehension, the ultimate goal for educators is to identify problems with student performance and to correct these issues before they impact patient care.
The American Association of Colleges of Nursing (AACN) defines competency-based education as “a system of instruction, assessment, feedback, self-reflection, and academic reporting that is based on students demonstrating that they have learned the knowledge, attitudes, motivations, self-perceptions, and skills expected of them as they progress through their education” (1).
Components and Benefits of Competency-Based Education (CBE) (1):
- Students are responsible for their learning and success.
- Mitigates bias using formative and focused feedback from multiple assessors using various methods.
- Clarifies faculty expectations regarding student performance and allows the faculty to hold students accountable for prior learning.
- Relates curriculum and course work to nursing practice.
- Provides an overall cohesive framework for clinical setting simulation design and development.
- Requires internal motivation, a collaborative culture, and the continuous cycle of using assessment findings and feedback to assure the competence of learners.
Mistakes made by students can be a powerful teaching tool, but an alarming amount of careless and repetitive mistakes should raise a red flag for educators.
Competency assessment requires a solid foundation of effective teaching methods and clearly communicated expectations.
Formative and Summative Evaluation
Competency assessments may be formative or summative.
Formative evaluation in provides feedback to learners about their progress in meeting the clinical competencies and outcomes of the simulated clinical course. With this type of evaluation, after identifying the learning needs, instruction is provided to move students forward in their learning. Formative evaluation, therefore, is diagnostic; it should not be graded (10).
Summative clinical evaluation, however, guides clinical grading because it summarizes competencies the student has developed in clinical practice. Summative evaluation is done at the end of a certain period of time. For much of clinical practice in a nursing education program, summative evaluation comes too late for students to have an opportunity to improve performance (10).
The goal of formative evaluation is to improve performance while simulation experiences are still available, but summative evaluations are designed to assign a grade level to performance.

Self Quiz
Ask yourself...
- What are some benefits to competency-based education (CBE)?
- What are some creative ways to use a mistake to create an opportunity for learning?
- Can you describe the difference between formative and summative evaluation?
- Should all competency assessments yield a “pass” or “fail” determination?
De-brief After Simulation
Debriefing is an essential component of simulation that follows the simulation experience. The facilitator should provide feedback on the students’ performance, all aspects of the simulation activities are discussed, and reflective thinking is encouraged.
Evidence supports that significant learning happens through discussion and reflection during debriefing. Theoretical frameworks and models are immensely helpful in making a debriefing meaningful.
Reflection, Reflection, Reflection! The debriefing should not be focused on what was done wrong, but meaningful reflection on what could be better.
Models for Meaningful Debriefing
Simulation facilitators can use theoretical models to make the most of the debriefing session. Models include the Gather – Analyze – Summarize (GAS) method, Debriefing for Meaningful Learning (DML), Plus Delta, along with many other meaningful models (4).
- Gather – Analyze – Summarize (GAS)
- Gather data by actively listening to participants to understand the reasons for actions from their perspective
- Analyze
- Encourage student reflection and analysis of their actions.
- Identify positive aspects of team or individual behaviors
- Identify behaviors that require change.
- Summarize
- Review process of decision-making and concepts that were learned.
- Debriefing for Meaningful Learning (DML)
- DML worksheets are used to guide the debriefing process and the instructor posting notes and ideas on a white board
- Colored markers are used to identify correct concepts versus concepts that need to be changed.
- The six iterative aspects of DML are:
- Engage - Learners reflect about the clinical situation and briefly telling the patient situation and events that unfolded
- Explore – Group discussion and reflection; concept maps can be used
- Explain – Faculty and learners discuss patient assessment, findings, orders, actions, and responses.
- Elaborate – Facilitator links these components along with worksheets to review knowledge, skills, and attitudes.
- Evaluate – Incorporation of a series of questions to identify what did not go well, and to consider what students would do differently and why.
- Extend (Thinking-Beyond-Action): Learners are encouraged by the use of “what if” questions to explore different patient situations.
- Socratic Questioning – Used to clarify ideas, probe assumptions, provide reasoning for actions.
- Plus Delta
- Simple to use application of asking “what went well” (Plus) and “what would you change” (Delta)?

Self Quiz
Ask yourself...
- What are the meaningful benefits of debriefing?
- How can facilitators encourage participation and reflection during debriefing?
- Can you name theoretical methods that facilitators can apply during the debriefing session?
- Are you familiar with Socratic questions?
Feedback
Polls have found that students made positive comments and strongly argued that simulation and the clinical laboratory procedure have prepared them for what they will later face in the hospital (6).
For clinical evaluation to be effective, the instructor should provide continuous feedback to students about their performance and how they can improve it (10). This enables students to reflect on their performance, identify continued learning needs, and decide how to meet them.
Feedback can be given verbally, visually, by demonstrating correct performance, or written.
Feedback on performance throughout the clinical simulation should be specific and supported by evidence-based practice.
Learners must have a foundational knowledge base and be able to judge their own performance.
Educators may choose to video the simulation and allow students to review the experience and discuss certain positive or negative actions. This may have a meaningful impact on reflection.

Self Quiz
Ask yourself...
- Should instructors always provide feedback on performance?
- What are technological tools that can enhance feedback?
- Should students be encouraged to voice the reasoning behind their actions?
- Can you name different ways feedback can be provided?
Simulation Resources for Educators
The Society for Simulation in Healthcare is the world’s largest organization dedicated to medical simulation (12). The Society also publishes a peer-reviewed research journal, “Simulation in Healthcare Journal,” which is an interprofessional publication covering all domains within clinical simulation. The SSH also provides accreditation for certification to specialized simulation educators and operations specialists (12).
There is exponential opportunity for simulation and many organizations hope to foster the expansion of simulation-based technologies like virtual reality in medicine, video debriefing, augmented reality, standardized patients, specialized task training and more.
Clinical instructors using simulation-based learning should immerse themselves in literature on simulation in clinical settings. Clinical Simulations in Nursing Education: Advanced Concepts, Trends, and Opportunities, by Pamela Jeffries, is an excellent resource that innovative teaching and learning methods, new clinical models, and up-to-date best practices for providing high-quality simulation-based education (4). There are many other peer-reviewed articles being published that can have a huge impact on learning.

Self Quiz
Ask yourself...
- Can you name organizations that are dedicating to fostering the growth of simulation-based learning methods?
- How can facilitators apply theoretical frameworks and methods into their curriculum?
- Are you familiar with opportunities to become involved in the simulation community?
- Can you name organizations that allow nurses to join committees and become active in policymaking?
Sample Organizational Proposal: The Virtual Reality in Clinical Curriculum Project
Please note, this is not an actual proposal, figures do not accurately reflect a formal proposal.
Proposed Simulation Experience: Integration of VR technology and platform into simulation-based learning within clinical curriculum.
Purpose
The purpose of the Virtual Reality in Clinical Curriculum Project is to enhance the quality of student skill acquisition, critical thinking, and clinical decision-making through the use of simulation using VR devices and software programs. This is a high-fidelity simulator experience available to students for use during simulated clinical experiences.
Supporting Data
Empirical evidence has identified HFS such as virtual reality (VR) technology as an effective teaching strategy to compliment foundational competencies and translate theoretical nursing into practice (8).
Cost Projection and Budget
This budget projects the expenses for the Virtual Reality in Clinical Curriculum Project, including costs of equipment and necessary training costs.
|
Item |
Per Unit |
Total |
|
Sample VR-SIM |
$835.00 (5 total units proposed) **This is not an actual price projection** |
$4,175.00 |
|
Ongoing service / subscription to VR program support |
$99.00 / month |
$1,188.00 |
|
Additional Faculty Training |
|
$4,000.00 |
|
Total for Year 1: |
|
$9,363.00 |

Self Quiz
Ask yourself...
- Are there opportunities for faculty to submit proposals within the organization you work for?
- Are you familiar with new technology that could be designed to focus on healthcare clinical environments, such as VR headsets or gaming systems?
- Do you think that entertaining activities can also yield meaningful learning is designed appropriately?
- Can you name barriers for academic institutions to obtaining high-fidelity simulation equipment?
Conclusion
Traditional nursing education has predominantly relied on the apprenticeship model, where students learn through hands-on experiences in real patient care settings. However, challenges such as limited clinical opportunities, shortage in clinical staff, and safety considerations have prompted educators to explore alternative methods for skill acquisition. Simulation-based learning in the clinical setting is a meaningful endeavor that has great promise and growth.
References + Disclaimer
- American Association of Colleges of Nursing (AACN). (2021). What is competency-based education? Retrieved from https://www.aacnnursing.org/essentials/tool-kit/competency-based-education
- HealthySimulation.com. (2023). Healthcare simulation dictionary. Retrieved from https://www.healthysimulation.com/healthcare-simulation-dictionary/
- Hughes PG, Hughes KE. Briefing Prior to Simulation Activity. [Updated 2023 Jul 24]. In: StatPearls [Internet]. Treasure Island (FL): StatPearls Publishing; 2023 Jan-. Available from: https://www.ncbi.nlm.nih.gov/books/NBK545234/
- Jeffries, P. R. (2012). Simulation in nursing education: From conceptualization to evaluation. New York, NY: National League for Nursing.
- Kiernan, L. C., & Olsen, D. M. (2020). Improving clinical competency using simulation technology. Nursing, 50(7), 14–19. https://doi.org/10.1097/01.NURSE.0000668448.43535.4f
- Koukourikos, K., Tsaloglidou, A., Kourkouta, L., Papathanasiou, I. V., Iliadis, C., Fratzana, A., & Panagiotou, A. (2021). Simulation in Clinical Nursing Education. Acta informatica medica : AIM : journal of the Society for Medical Informatics of Bosnia & Herzegovina : casopis Drustva za medicinsku informatiku BiH, 29(1), 15–20. https://doi.org/10.5455/aim.2021.29.15-20
- Labrague LJ, McEnroe-Petitte DM, Bowling AM, Nwafor CE, Tsaras K. High-fidelity simulation and nursing students’ anxiety and self-confidence: A systematic review. Nurs Forum. 2019; 54: 358-368. https://doi.org/10.1111/nuf.12337
- McGaghie, W. C., Barsuk, J. H., & Wayne, D. B. (Eds.). (2020). Comprehensive Healthcare Simulation : Mastery Learning in Health Professions Education (1st ed. 2020.). Springer International Publishing. https://doi.org/10.1007/978-3-030-34811-3
- Michigan Radio. (2016). Life-like mannequins help nursing students train for real life. Retrieved from https://www.michiganradio.org/health/2016-06-06/life-like-mannequins-help-nursing-students-train-for-real-life
- Oermann, M. H., & Gaberson, K. B. (2017). Evaluation and testing in nursing education (Fifth edition.). Springer Publishing Company, LLC.
- Riplinger, L., Piera-Jiménez, J., & Dooling, J. P. (2020). Patient Identification Techniques – Approaches, Implications, and Findings. Yearbook of medical informatics, 29(1), 81–86. https://doi.org/10.1055/s-0040-1701984
- Society for Simulation in Healthcare (SSH). (2023). SSH Certification vision and mission. Retrieved from https://www.ssih.org/Credentialing/Certification.
- Witheridge, A., Ferns, G., & Scott-Smith, W. (2019). Revisiting Miller’s pyramid in medical education: the gap between traditional assessment and diagnostic reasoning. International journal of medical education, 10, 191–192. https://doi.org/10.5116/ijme.5d9b.0c37.
- Wolters Kluwer. (2018). Increasing fidelity and realism in simulation for nursing students. Retrieved from https://www.wolterskluwer.com/en/expert-insights/increasing-fidelity-and-realism-in-simulation
Disclaimer:
Use of Course Content. The courses provided by NCC are based on industry knowledge and input from professional nurses, experts, practitioners, and other individuals and institutions. The information presented in this course is intended solely for the use of healthcare professionals taking this course, for credit, from NCC. The information is designed to assist healthcare professionals, including nurses, in addressing issues associated with healthcare. The information provided in this course is general in nature and is not designed to address any specific situation. This publication in no way absolves facilities of their responsibility for the appropriate orientation of healthcare professionals. Hospitals or other organizations using this publication as a part of their own orientation processes should review the contents of this publication to ensure accuracy and compliance before using this publication. Knowledge, procedures or insight gained from the Student in the course of taking classes provided by NCC may be used at the Student’s discretion during their course of work or otherwise in a professional capacity. The Student understands and agrees that NCC shall not be held liable for any acts, errors, advice or omissions provided by the Student based on knowledge or advice acquired by NCC. The Student is solely responsible for his/her own actions, even if information and/or education was acquired from a NCC course pertaining to that action or actions. By clicking “complete” you are agreeing to these terms of use.
➁ Complete Survey
Give us your thoughts and feedback
➂ Click the Green MARK COMPLETE Button Below
To receive your certificate
