Course
Skin Cancer Prevention and Early Detection
Course Highlights
- In this Skin Cancer Prevention and Early Detection course, we will learn about why skin cancer develops and correlate this to the skin changes that may be noted.
- You’ll also learn the risk factors for skin cancer and corresponding preventative measures.
- You’ll leave this course with a broader understanding of the methods used for the early detection of skin cancer.
About
Contact Hours Awarded: 2
Course By:
Brittane L. Strahan MSN, RN, CCRP
Begin Now
Read Course | Complete Survey | Claim Credit
➀ Read and Learn
The following course content
Introduction
Skin cancer is the most common malignancy in the United States [5]. There are two distinct classes of skin cancer (melanoma and non-melanoma), and these will be detailed in this course. Usually, skin cancer is diagnosed when a suspicious visible lesion on the skin is evaluated and biopsied; however, this is not always the case. As with all malignancies, the earlier diagnosis and treatment occur, the better.
Overview of Skin Cancer
According to the Skin Cancer Foundation, skin cancer is an “out-of-control growth of abnormal cells in the epidermis, the outermost skin layer, caused by unrepaired DNA damage that triggers mutations”. [14] This overgrowth of abnormal cells leads to the development of a mass that can be visualized on the topmost layer of skin. While there is not necessarily a standard appearance of one specific type of cancer, any unusual, new, evolving skin lesion should be considered a possible malignancy and evaluated.
Importance of Prevention
Prevention is the most important factor in the fight to reduce the incidence of skin cancer. There are several reasons why prevention is so important. These include eliminating the need for harsh cancer treatments such as chemotherapy and radiation, which can cure skin cancer but come with potential risks. The second reason prevention is so important is that surgery can be very disfiguring depending on the type and size of malignancy that must be excised. [4] Skin cancer is also expensive to treat and can be burdensome for both the affected person and their family or friends.
Importance of Early Detection
Similar to the reasons for the importance of prevention, early detection is also critical to reduce the risks associated with cancer treatments. More importantly, early detection plays a huge part in reducing the risk of metastasis. Although melanoma is more likely than the other types of skin to spread to other locations, basal and squamous cell cancers can spread as well. Early-stage skin cancers typically do not require systemic chemotherapy or radiation, and this reduces the overall morbidity and mortality associated with a skin cancer diagnosis. [14]

Self Quiz
Ask yourself...
- What is the simple explanation of how skin cancer develops?
- Why is skin cancer prevention important?
- What are three risks that can be minimized with early detection?
Types of Skin Cancer
In-situ skin cancers
In-situ skin cancers can be categorized into melanoma and non-melanoma types. These cancers are classified as stage 0 (on the 0-4 staging scale used for cancer) and they have not spread from the original clump of cells that have mutated and overgrown. The outlook is most favorable when a diagnosis is made at the stage 0 or carcinoma-in-situ stage. [23]
Basal cell carcinoma (BCC)
Basal cell carcinoma is a cancer specifically originating in the basal cells of the epidermis and usually occurs in sun-exposed areas of the face, neck, head, back, and shoulders. These typically appear as open, red sores, raised pink or flesh-colored bumps, or scar-like with a lighter periphery and darker central region. [1]
While BCC typically does not spread beyond the initial site, the growth can become large, unsightly, and disfiguring. Treatment of the growth can further exacerbate this issue. Also, while BCC rarely metastasizes it can become invasive and destroy the tissues directly underneath the tumor including soft tissue, muscle, and bone. BCC is the most common type of skin cancer with one of three newly diagnosed skin cancers being diagnosed as BCC. [1]
Squamous cell carcinoma (SCC)
Like basal cell carcinoma, squamous cell carcinoma originates in a specific type of epidermal cell (squamous cells). Like BCC they tend to develop in highly sun-exposed areas such as the face, ears, neck, and hands. [14] Similarly, SCC can appear as non-healing lesions, but these are typically a thicker, scaly, crusted lesion. They can also appear wart-like. Unlike BCC, SCC can multiply and spread rapidly leading to an increased risk for metastasis. SCC is the second most commonly diagnosed skin cancer type. [22]
Melanoma
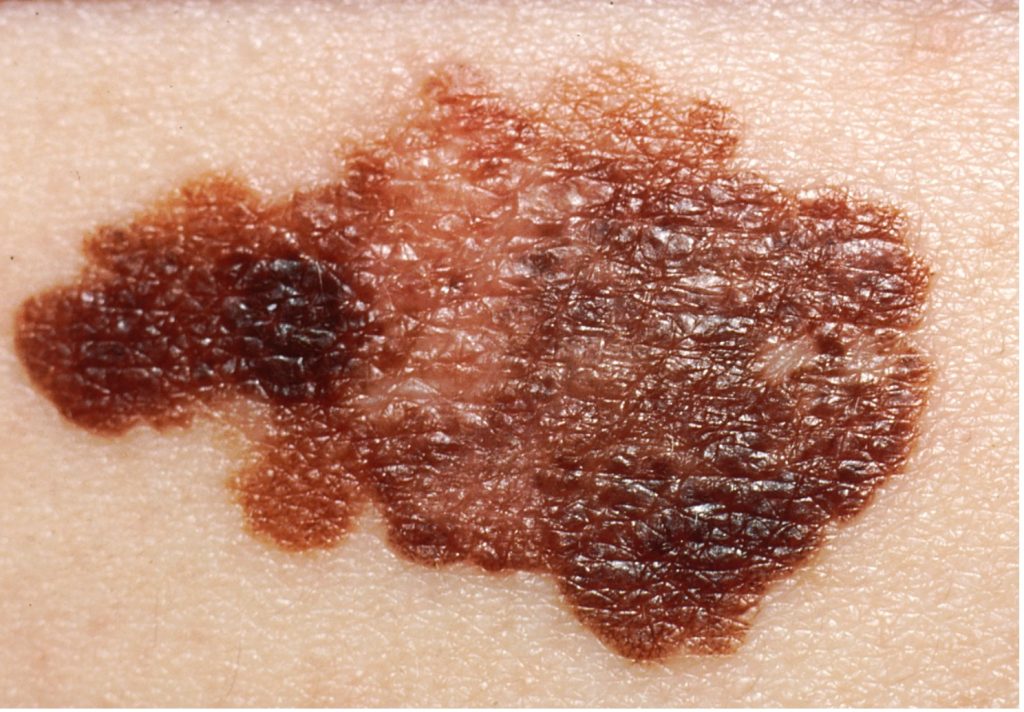
Melanoma is the most commonly diagnosed type of skin cancer and the most aggressive of the three mentioned above. [14] The most common causes of melanoma are tanning bed use and sun exposure resulting in sunburn. In 2023, it was estimated that approximately 52% of melanoma were advanced at diagnosis and had at least invaded the dermis.
Contrary to BCC and SCC, melanoma can develop on any skin surface, even one not routinely exposed to the sun. The self-screening for melanoma is more defined than for other skin cancers and will be discussed in further detail in the appropriate section. Melanoma can arise from moles so it may be brown to black. However, they can also be skin-colored, red, pink, clear, or white which can make some melanoma difficult to spot. The key is to watch for any new or changing skin lesions. [9]
 (27)
(27)
Merkel cell carcinoma (MCC)
Merkel cell carcinoma is a rare type of skin cancer and is known to be very aggressive. One especially notable point about the detection of MCC is that the lesions often appear as painless, firm nodules on the face or head (typically in areas receiving high sun exposure). [14] These lesions are sometimes mistaken for inflamed hair follicles or cysts. Unlike BCC, SCC, and melanoma which are caused almost exclusively by excess sun exposure, MCC is also associated with a virus (Merkel cell polyomavirus). While MCC is treatable, especially if caught in the early stages, it is also highly likely to recur, and the site must be monitored with great vigilance. [10] The self-screening method for MCC is slightly different than for melanoma and will be discussed more below.

Self Quiz
Ask yourself...
- What is in-situ skin cancer?
- What is the common denominator root cause for BCC, SCC, and melanoma?
- What are the differences in appearance between the four malignancies mentioned above?
- What makes Merkel Cell carcinoma difficult to diagnose and easy to misdiagnose?
Epidemiology
This section will give a very brief overview of the statistics of skin cancer including the stage at diagnosis and the prevalence of skin cancer among different demographic/ racial groups.
Population statistics
In the United States, there are approximately 9,500 new cases of skin cancer diagnosed every day and it is estimated that 20% of Americans will develop skin cancer during their lifetime. [20] Women are diagnosed with non-melanoma skin cancer more often than men. Regarding melanoma, which is expected to be the fifth most common cancer in the United States in 2024, women younger than 50 are more likely to be diagnosed with melanoma than men of the same demographic. However, the opposite becomes true after the age of 50. Lighter-skinned populations are more likely to develop melanoma; however, when it is diagnosed in a darker-skinned individual it is usually diagnosed at a later stage portending a worse prognosis. [20]
Incidence
The global incidence of skin cancer has grown by almost 75% between the years 1990-2017. [25] Skin cancer is a disease that affects individuals of all races. However, because sun exposure is the biggest risk factor, white or fair-skinned people are disproportionately affected. [14] Interestingly, the type of skin cancer being diagnosed varies between global regions with countries with a higher percentage of members of white European ancestry having higher rates of melanoma. Conversely, countries with historically darker-skinned populations such as Africa, the Middle East, southern Asia, and South and Central America record more diagnoses of non-melanoma type skin cancers (BCC or SCC). This is due to the protective effect of melanin on darker skin. However, the takeaway message is that the overall number of cases is rising and that is concerning.

Self Quiz
Ask yourself...
- What is the recent trend in the incidence of skin cancer diagnoses?
- What is the interesting demographic shift seen with skin cancer diagnoses, especially melanoma?
- Why is the protective effect of melanin both a positive and negative factor in the screening and diagnosis of skin cancer?
- Why is there a difference in the cancer types diagnosed in different global regions?
Etiology
Ultraviolet radiation (natural and artificial)
The most important modifiable risk factor for the reduction of skin cancer is to minimize exposure to ultraviolet (UV) radiation. UV radiation is divided into three distinct forms (UV-A, UV-B, and UV-C) but not all are equally linked to the development of skin cancer. UV-A is thought to be the most dangerous of the three because it causes the formation of free radicals under the skin. However, the general mechanism of action for both UV-A and UV-B is that the DNA becomes damaged, the cell dies, and cellular repair cannot happen normally leading to mutated cells and eventually malignancy.
Both sunlight and tanning beds cause cellular damage by this mechanism so more unprotected exposure equals more risk. [14] [12].
Having a history of more than five blistering sunburns in childhood and adolescence increases the risk for the development of melanoma by 80% and non-melanoma skin cancer by almost 70%. [12]
Chemical exposure
Exposure to certain chemicals has been linked to the development of skin cancer. Several chemicals are known to cause changes in skin cells through various mechanisms. These include paraffin, coal, industrial tar, and arsenic. [26]
Human Papillomavirus
Human papillomavirus (HPV) is a family of viruses that cause several notable diseases such as genital warts and HPV-mediated cancers (notably head and neck and anogenital cancers). It is thought that HPV transforms two proteins from their normal shape and function which causes a subsequent disruption of the cell cycle and malignant changes in cells. [2] Certain strains of the virus are thought to be more likely to cause these malignant changes and there is also a strong link between sun exposure in addition to having the HPV present.


Self Quiz
Ask yourself...
- How does UV exposure increase the risk of developing skin cancer?
- At what level of UV exposure does the risk steeply increase for developing melanoma?
- What chemicals have been correlated with an increased risk for skin cancer?
- How does the human papillomavirus increase the risk for skin cancers?
Pathophysiology
Sunlight is the main risk factor for the development of skin cancer as highlighted above. [14] Through exposure to both types of UV-A and UV-B rays, cell damage is caused at the level of the DNA. To reiterate what has already been mentioned, when the DNA is damaged, the cell cannot function properly and undergoes apoptosis (cell death). At the same time, because the DNA is damaged, the cell cannot repair itself nor can new cells be formed appropriately or function as they should.
One specific gene that is affected is p53, which is responsible for the proliferation of keratinocytes. In a p53 mutated cell, keratinocytes are multiplied, and this out-of-control cellular growth leads to SCC. Another gene commonly mutated, though this time in BCC, is PCTH in addition to p53.
There is another common group of mutated genes in melanoma. These include CDKN2A, MCR1, and B-RAF. Regardless of the mutation or the specific malignancy, the main underlying pathophysiology revolves around DNA damage and subsequent cell damage. The dysfunctional cells then proliferate and are noted as skin lesions.
[5]

Self Quiz
Ask yourself...
- How does the alteration in the p53 pathway lead to the development of squamous cell carcinoma?
- What is the underlying mechanism for developing skin cancer, regardless of type?
Risk Factors
- Sun exposure – Sun exposure and the impact of UV rays on the development of cancer have already been discussed and reiterated. The damaging effect of the UV rays on the DNA leads to irreparable cellular damage, defective cells, increased cell death, and the development of a population of abnormal cells (tumor). This population of cells can then become invasive or metastatic depending on its histology.
- Skin type – The Fitzpatrick skin type scale is a simplified scale to correlate skin tone with the ability to tan or burn. Hair and eye color are factored into this scale as well as skin color because all of these characteristics are related to the number of melanocytes present in an individual. This scale is useful in determining if someone is more prone to developing skin cancer. [21]
- Family history – As with many medical conditions, family history plays a large part in predisposing an individual to skin cancer. If there is a strong family history, the risk is higher. Of course, much of this family history could be related to sun exposure and skin type. [8] Genetic changes in the family line, especially those directly linked to a higher likelihood of developing skin cancers cannot be overlooked either. Likely, family history is multifactorial when it comes to an increased risk for skin cancer.
- Previous medical history – An individual’s previous medical history also plays a large part in determining their risk for skin cancer. Of course, if they have a history of previous skin cancer, they are more likely to have another skin cancer diagnosed or a recurrence of their previous cancer. In patients with a previous history of skin cancer (usually melanoma), genetic testing may be ordered once a patient has multiple instances of melanoma being diagnosed.
- Medications – Several classes of medication have been linked with an increased occurrence of skin cancer. [11] These include tumor necrosis factor-alpha inhibitors, angiotensin-receptor blockers, phosphodiesterase type 5 inhibitors, and HMG-CoA-reductase inhibitors. The indications for these medications include inflammatory conditions such as rheumatoid arthritis, ulcerative colitis, Crohn’s disease, psoriasis (TNF-alpha inhibitors), hypertension (ARB), erectile dysfunction, and pulmonary hypertension (PD5 inhibitors), and hyperlipidemia (HMG-CoA-reductase inhibitors).
These drugs are widely used and the exact mechanisms of action that increase the risk of skin cancer are diverse. They include immunosuppression and alteration in the functioning of normal cellular pathways. Therefore, patients on these medications should be properly cautioned and educated to take extra preventative measures.
- Immunocompromised status – The most likely way in which an immunocompromised status increases one’s risk for cancer is related to the ability of aberrant cells to multiply and escape detection by the immune system until the cells have already undergone numerous proliferations and have grown beyond what the immune system can eradicate. [18] This is especially concerning for someone receiving immunosuppressive drugs such as in the case of an organ recipient. However, since these immunosuppressive drugs cannot be stopped for the patient’s overall well-being, they must be cautioned on the increased need for prevention and screening. Of course, there are other causes for immunosuppression, including autoimmune diseases, age, poor nutritional status, and other coexisting immunodeficiencies. The treatment for each of these is different and should be addressed.


Self Quiz
Ask yourself...
- How does the Fitzpatrick scale provide valuable information about an individual’s risk for skin cancer?
- In what ways does family history affect the risk for skin cancer development?
- What is the correlation between previous skin cancer and future risk?
- What medications are known to increase the risk for skin cancer and why?
- How does an immunocompromised status increase the risk for skin cancers?
Assessment
This section will detail skin assessments at both a self-care level and a more thorough medical examination.
Self-assessment
Self-assessment should be conducted on a routine basis. This ensures that concerning lesions are identified promptly. Symptoms that can be noted and should prompt a careful self-screening and medical evaluation include changes in sensation (itching), changes in size, shape, color, or surface texture (including the development of bleeding, crusting, or a scaly texture), and changes in the skin surrounding the suspicious mole. The surrounding skin may become erythematous, edematous, or start to develop other pigmented lesions including those which are red, white, or even blue. [9] [13]
Frequency
According to the University of California at San Francisco, the recommended frequency for a self-assessment is at least once a month. This provides a recurring reminder to take a thorough evaluation of the skin and allows for early recognition of changes in existing moles or the development of new moles. [16] It is recommended that a trusted partner or friend be enlisted to check any harder-to-assess areas, but a small mirror can also be used if doing a self-check. It can be useful to develop a “body map” or “mole map” to keep track of current moles and facilitate better identification of new or changing moles. [16]
Dermatology appointments should occur at least once a year especially if one falls into a higher risk category such as those with a strong family history of skin cancer, especially melanoma, personal history of skin cancer, previous blistering sunburns, previous radiation treatments, exposure to toxic metals (such as arsenic) or certain medications, or a history of an organ transplant. [16] These examinations are supplementary to the self-check and any change in existing moles or development of new moles should be evaluated sooner than the yearly dermatology check.
Techniques
Several techniques can be used to evaluate mole characteristics. The key criteria to look at are related to color, shape, borders, and overall changes. These characteristics are covered by acronyms ABCDE for melanoma and AEIOU for Merkel Cell Carcinoma. Non-melanoma lesions can be identified by the characteristics listed above in the relevant sections on BCC and SCC. The biggest thing to note though is that not all malignant lesions will necessarily fit the acronyms below, so any mole or lesion that is changing should be professionally evaluated. [16]
ABCDE Method [16]
The ABCDE method to identify possible melanomatous lesions consists of looking at the borders, color, and size.
- “A” is for asymmetry. Usually, non-cancerous moles are round or oval and fairly symmetric. Melanoma moles are asymmetric and can appear more oddly shaped.
- “B” is for border irregularity. Somewhat similar to symmetry, looking at the borders of a non-cancerous mole would reveal a relatively smooth border whereas a melanoma may have a ragged or notched border.
- “C” is for color. Melanoma lesions are usually various shades of black or brown. Benign moles are almost always uniform in color.
- “D” is for diameter. The cut-off between a benign mole and a malignant melanoma is 6 millimeters. A benign mole is smaller than 6mm, but a melanoma is almost always larger even in the early stages.
- “E” is for evolution. This simply refers to a change in the mole over time and should be applied in terms of the “ABCD” characteristics. Evolving could also be applied to moles that are now bleeding, crusting, or itching.
AEIOU Method
The AEIOU method is used to identify potential Merkel Cell Carcinoma. Like melanoma, these characteristics are identified in comparison to a benign lesion. Also, MCC can develop, change, and spread rapidly, so any change in a mole needs prompt evaluation. [10]
- “A” stands for asymptomatic. MCC lesions do not have any associated pain or tenderness.
- “E” is for expansion. Similarly to “D” in melanoma, expansion refers to the size and increase in size which usually is rapid.
- “I” is immunosuppression. While this is not directly related to the lesion itself, immunosuppression is one of the biggest risk factors for developing MCC in tandem with previous sun exposure.
- “O” is for people older than 50. Statistically, MCC does not occur in individuals younger than 50.
- “U” is for a lesion that appears in an area that has had significant UV exposure. This includes the face, scalp, neck, shoulders, and back.
Ugly Duckling Method
The “ugly duckling” method views lesions in how they appear compared to other lesions. Typically, this method relies on color, size, or even isolation of moles. If the suspicious lesion is noticeably darker or lighter than its neighbors, this should be further evaluated. Amelanotic melanoma, or those which are very light in color or even white, skin tone, or colorless are especially difficult to identify. Finally, if there is a single mole without any surrounding moles, this is another characteristic of “ugly duckling” and should be evaluated. [9]

Self Quiz
Ask yourself...
- What is the frequency of self-assessment and why is the recommendation specific to that frequency?
- What does the acronym represent in the evaluation of possible melanomatous moles?
- What does the acronym represent in the evaluation of possible Merkel Cell Carcinoma lesions?
- How does the “Ugly Duckling” method of self-assessment help to identify potentially malignant lesions?
Medical Assessment
A thorough medical evaluation should be done every year for any individual having an increased risk for skin cancer, especially melanoma. Of course, a dermatologist is the best option for a medical evaluation of the skin since they receive lengthy and specialized training in conditions of the skin, diagnosis, and treatment. However, there is also usually a lengthy waiting period for a specialist such as a dermatologist and this may present a delay in evaluation if a lesion has changed or developed. [3] In this case, a primary care physician can also conduct a more thorough examination than what an individual can typically do for himself and can put in a referral to dermatology which may receive a quicker response than if the individual tried to schedule immediately with dermatology.
Though the primary care physician may not be as skilled in identifying the specific type of skin lesion and will likely be unable to biopsy or remove the lesion on their own, they can provide an initial contact for the individual. [6]
Primary care practitioner
As briefly mentioned above, the primary care physician (PCP) may not be able to conduct the extent of examination or intervention that a dermatologist may be able to, but their capability should not be overlooked when an individual discovers a new or changing skin lesion. In the United Kingdom, data has shown that patients who have first presented to their primary care physician to be evaluated only to be diagnosed with a benign lesion have helped to lessen the burden on dermatologists. This also provides a quicker evaluation for the individual which can facilitate a faster diagnosis, and treatment plan if needed, as well as reducing anxiety caused by long wait times. [6]
The strategy used by the PCP will include identification of risk factors, a thorough patient history, and a comprehensive examination. PCPs can also provide education related to the prevention of skin cancer. However, it may not be to the depth covered by a dermatologist given the overall load of patients seen in primary care. In primary care, the examination will probably be done without any special tools, so a thorough exam will provide the information needed for an urgent, or slightly less urgent, referral to dermatology.
Electronic medical records and video or photo sharing capability can enable PCPs to share visual representations of the individual’s lesions directly with the dermatologist.
Dermatologist
The dermatologist will have better access to specialized tools and a more robust knowledge of skin lesions. Some of the tools that a dermatologist will have at their disposal include a dermatoscope and other higher-level imaging services including ultrasound and specialized forms of microscopy. In addition to the assessment completed by a PCP, the dermatologist can use the dermatoscope to visualize sub-surface structures of the suspicious skin lesion including the dermis and vasculature. [6] Dermatologists are also able to remove suspicious lesions in-office and can order the appropriate pathology screening assessments.
Other signs of skin cancer
Though the skin changes identifying BCC and SCC were not detailed in this screening section, the identifying characteristics are listed above. The biggest notable factor in identifying non-melanomatous lesions is a change in a pre-existing skin lesion or the development of a new lesion. Changes may include color, texture, size, or changes in the margins. All of these can be observed in a self-assessment, and all should prompt a timely medical evaluation.

Self Quiz
Ask yourself...
- How would a dermatologic evaluation differ between a primary care evaluation and one done by dermatology?
- What are some of the other characteristics that can be noted on a thorough skin screening that would lead one to be suspicious of malignancy?
Clinical signs and symptoms
While the previous sections have detailed specific characteristics for the different types of skin cancer, this section will provide a more general overview.
The signs and symptoms of a malignant skin lesion in the early stages may include the following: [19]
- A new mole or skin lesion
- Noted changes in an existing mole or skin lesion including changes in the color, shape, size, border, or texture
- A painful or itchy skin lesion
- A lesion that is crusted, bleeding, or that will not heal
- A shiny, raised lesion on the skin which is red or skin-toned in color
- A palpable rough and red lesion that may feel scaly
- A lesion that is crusted, scaly, or bleeding in the middle and has raised borders
- A growth that appears wart-like but is not a wart
- A lesion that appears like a scar but has a poorly defined border

Self Quiz
Ask yourself...
- What are five defining characteristics that should be considered as clinical signs and symptoms of early-stage skin cancer?
Prevention
The prevention of skin cancer can be viewed straightforwardly. While certain elements of risk cannot be mitigated, such as family history or even past medical history such as sun exposure and sunburns in childhood, one can always implement risk-mitigation strategies at any time to decrease their risk of developing skin cancer.
These strategies include the use of sunscreen, UV-protective clothing, and timed sun exposure to mitigate UV exposure which leads to DNA changes, aberrant cells, and eventual cancer. [17] [16] According to the National Cancer Institute, while there have not been enough research studies to say that sunscreen and UV-protective clothing prevent both non-melanoma and melanoma skin cancers, there is enough data to show that sunscreen reduces the risk of sunburn and subsequent cellular damage. [17] [16]
Since UV radiation from tanning beds and devices can increase the risk of skin cancer due to the same mechanism as natural UV exposure, abstinence from these devices is also a good preventative measure.
It cannot be stressed enough how much routine self-skin examinations can facilitate the identification of early-stage skin cancers. While this may not directly prevent a non-melanoma or melanoma skin cancer, it can prevent a later-stage diagnosis requiring more treatment and is usually predictive of a worse outcome.
Finally, there have been other medications and supplements tried to see if the risk of skin cancer could be lowered. However, the data did not show a strong correlation between the medications or supplements and a lower risk. Some supplements even appeared to raise the risk of some malignancies. These included topical chemotherapy (fluorouracil), beta-carotene, retinoids, selenium, celecoxib, vitamin B3, and alpha-difluoromethylornithine (DFMO) which is being studied as a possible form of chemoprevention. [17]

Self Quiz
Ask yourself...
- What is the biggest preventative measure one can take to lessen the risk of skin cancer?
- How does sunscreen lower the risk of developing skin cancer?
- Have there been other methods tried to reduce the risk of skin cancer and have they been effective?
Treatment
As has been extensively reviewed already, the early detection and prevention of skin cancer is paramount because skin cancer diagnosed in a later stage requires more treatment, and more aggressive treatment, and portends a worse outcome overall. Treatment in the earlier stages is much less invasive and does not affect the quality of life to quite the same extent. Early detection has been shown to increase overall survival. [3] Three key outcomes have been noted in cases of early detection and treatment. These include an improved response to treatment, a decreased risk of complication, and better overall outcomes. [5] [14]
An improved treatment response simply means that the malignancy will respond better to the treatment in the early stage compared to a later stage. This could mean that the removal process of the lesion is more straightforward and not as disfiguring, chemotherapy can be given in a topical form, or there is a very low likelihood of a recurrence, relapse, or metastasis. [5] [14]
If skin cancer is diagnosed and treated in the early stages, the risk of complications is much lower. The rationale for this is similar to the reasons for an improved treatment response. These include using the least invasive (but still effective) surgeries, topical chemotherapy versus a systemic formulation, and a very low likelihood that radiation would be necessary. [5] [14]
As with any malignancy, the earlier it is found and treated, the lower the risk that it will recur or spread either locally or through metastasis. This means that life expectancy should not be shortened solely because of cancer or cancer-directed treatments. There is also a lower risk of disfigurement or complications for the reasons stated above. [12]
While treatment varies between early and later-staged skin cancer diagnoses, there are three mainstays of treatment. These include surgery, chemotherapy, or radiation. Sometimes one modality is enough as is typically the case in the early stage setting where a surgical option is adequate for treatment. Typically, in the later settings, more than one method is used to attempt to provide the best outcomes.
Surgery
In the early-stage setting, surgery or some surgery alternatives are typically adequate therapy for a lesion. These surgeries may include a skin shave or a slightly larger incisional or excisional technique, or a surgical alternative might include cryotherapy in which the lesion is frozen off with liquid nitrogen. [5] MOHS micrographic surgery may be necessary for a more invasive lesion.
Chemotherapy
Chemotherapy can be used but in a topical formulation. This is typically used in cases of multiple lesions which are identified as BCC or SCC. The best treatment in the case of either lesion is definitive removal, but in the case of multiple lesions, the better option may be topical chemotherapy. [5]
Radiation
Radiation is typically used in later-stage settings given its destructive nature and the damage that can be done to surrounding tissues. It is typically used in tandem with systemic chemotherapy and more usually in an advanced or metastatic setting or the case of a fairly aggressive malignancy or one with a higher risk of recurrence.


Self Quiz
Ask yourself...
- Why is early detection and treatment of skin cancer important?
- What three outcomes are improved by an early response to a skin cancer diagnosis?
- Why would surgery typically be sufficient treatment for an early-stage skin malignancy?
- What circumstance might prompt the use of topical chemotherapy instead of surgery?
- What specific situations may indicate the use of radiation for skin malignancy?
Self-Management
The biggest key to self-management is to initiate and regularly do self-screening every month. [20] Routine self-screenings are the earliest method for the identification of suspicious lesions which then prompt a medical evaluation.
In addition to self-screening and routine dermatology visits, if one is deemed to be at high risk or has a concerning lesion, sun protection is the next most important aspect of self-management. This includes the use of sunscreen, UV-protective clothing, and minimizing time outside in the peak UV hours. Of course, tanning beds and devices should be strictly avoided. While these methods are effective in preventing and identifying skin cancer in the early stages, what methods can be taken to care for oneself after a skin cancer diagnosis?
After a cancer diagnosis, the individual needs to care not only for the area specifically affected by the cancer diagnosis but they need to focus more on holistic care as well. This may include taking more time to pursue physical exercise or better nutrition, more time to focus on goals or hobbies, less time participating in activities that cause stress, changing the pace of their life routine and slowing down to focus on their recovery, and finally letting go of any guilt related to their cancer diagnosis. [9]

Self Quiz
Ask yourself...
- What are the most important self-management tips to prevent skin cancer or to facilitate early identification?
- Are there any ways in which one can better care for oneself after receiving a skin cancer diagnosis?
Research Findings
Risk assessment models can help to identify those who are more at risk of developing skin cancer. Since routine screening is not recommended for everyone, this may help identify individuals who should be routinely screened. [6]
Other devices and methods that have become available through clinical trials are the use of the dermatoscope and more fleshed-out guidelines for self-screening. However, there is still quite a bit of discord between PCPs and dermatologists on the ability of PCPs to make an accurate diagnosis in the case of early-stage malignancies. PCPs do reduce the burden on the dermatology specialty, so their value should not be downplayed.

Self Quiz
Ask yourself...
- What is one of the recent outcomes of research into early detection of skin malignancies?
Resources
There are numerous resources available for individuals in both a preventative and treatment setting. The Skin Cancer Foundation and CancerCare.org both provide detailed pages with potential resources whether that be related to financial support, psychosocial and emotional support, patient education, or organizations that can provide advocacy, connection, and caregiver support. These resources also help with health insurance questions, patient assistance, and workplace support. [15] [24]

Self Quiz
Ask yourself...
- What are two resources that may be useful for someone who has been recently diagnosed with early-stage skin cancer?
- Why might these resources be beneficial?
Conclusion
The prevention and early detection of skin cancer are critical to individuals around the world because skin cancer is quickly rising to be the most common malignancy. It is already the most common in the US. Both non-melanoma and melanoma skin cancers are caused by cellular damage caused when UV radiation damages the DNA and causes damage leading to cell death and the proliferation of aberrant cells.
Earlier detection and treatment are correlated to better outcomes. Of course, prevention is important because prevention of skin cancer means that there is no need for harsh anti-cancer treatments. This means less disfigurement and less toxicity associated with non-surgical treatments. Early detection is equally important because detection in an earlier stage means the treatment can be more localized and is typically curative. There is also a much lower risk for advanced disease, including invasion or metastasis.
Finally, the importance of receiving early and complete treatment cannot be overstated because with complete treatment in the early stage, it is unlikely that the individual will have a recurrence, relapse, or metastasis. In conclusion, the prevention of skin cancer through skin protection, minimized exposure to UV radiation, self-assessment, and routine medical examinations helps facilitate earlier detection of skin cancer. Likewise, earlier detection provides more options for definitive treatments and better outcomes for patients.
References + Disclaimer
- Basal cell carcinoma. (2022, April). The Skin Cancer Foundation. https://www.skincancer.org/skin-cancer-information/basal-cell-carcinoma/
- Chen, M., Wang, S., Wei, J. C., Yip, H., Hung, Y., & Chang, R. (2021). The impact of human papillomavirus infection on skin cancer: A population‐based cohort study. The Oncologist, 26(3), e473–e483. https://doi.org/10.1002/onco.13593
- Garrison, Z. R., Hall, C. M., Fey, R. M., Clister, T., Khan, N., Nichols, R., & Kulkarni, R. P. (2023). Advances in early detection of melanoma and the future of at-home testing. Life, 13(4), 974. https://doi.org/10.3390/life13040974
- General, O. of the S. (2014, July 23). Surgeon general call to action to prevent skin cancer: Exec summary [Text]. https://www.hhs.gov/surgeongeneral/reports-and-publications/skin-cancer/executive-summary/index.html
- Gruber, P., & Zito, P. M. (2024). Skin cancer. In StatPearls. StatPearls Publishing. http://www.ncbi.nlm.nih.gov/books/NBK441949/
- Jones, O. T., Ranmuthu, C. K. I., Hall, P. N., Funston, G., & Walter, F. M. (2020). Recognizing skin cancer in primary care. Advances in Therapy, 37(1), 603–616. https://doi.org/10.1007/s12325-019-01130-1
- Melanoma patients: Self-care & wellness tips. (n.d.). Melanoma Research Alliance. Retrieved June 16, 2024, from https://www.curemelanoma.org/patient-eng/ten-tips-for-people-just-diagnosed-with-melanoma/practicing-self-care/
- Melanoma skin cancer risk factors | melanoma risk factors. (n.d.). Retrieved June 14, 2024, from https://www.cancer.org/cancer/types/melanoma-skin-cancer/causes-risks-prevention/risk-factors.html
- Melanoma warning signs and images. (2021, January). The Skin Cancer Foundation. https://www.skincancer.org/skin-cancer-information/melanoma/melanoma-warning-signs-and-images/
- Merkel cell carcinoma warning signs and images. (n.d.). The Skin Cancer Foundation. Retrieved June 17, 2024, from https://www.skincancer.org/skin-cancer-information/merkel-cell-carcinoma/mcc-warning-signs/
- Nardone, B., Orrell, K. A., Vakharia, P. P., & West, D. P. (2018). Skin cancer associated with commonly prescribed drugs: Tumor necrosis factor alpha inhibitors (Tnf-αis), angiotensin-receptor blockers (Arbs), phosphodiesterase type 5 inhibitors (Pde5is) and statins -weighing the evidence. Expert Opinion on Drug Safety, 17(2), 139–147. https://doi.org/10.1080/14740338.2018.1400530
- Skin cancer. (2024, June 4). https://www.aad.org/media/stats-skin-cancer
- Skin cancer early detection. (2023, May 18). Fred Hutch. https://www.fredhutch.org/en/patient-care/prevention/skin-cancer-early-detection.html
- Skin cancer information. (2024, June). The Skin Cancer Foundation. https://www.skincancer.org/skin-cancer-information/
- Skin cancer, information, resources. (n.d.). CancerCare. Retrieved June 16, 2024, from http://www.cancercare.org/diagnosis/skin_cancer
- Skin cancer prevention. (n.d.). Ucsfhealth.Org. Retrieved June 14, 2024, from https://www.ucsfhealth.org/education/skin-cancer-prevention
- Skin cancer prevention—Nci. (2024, March 22). [pdqCancerInfoSummary]. https://www.cancer.gov/types/skin/patient/skin-prevention-pdq
- Skin cancer risk in immunosuppressed patients. (2023, November 30). Cleveland Clinic. https://consultqd.clevelandclinic.org/skin-cancer-risk-in-immunosuppressed-patients
- Skin cancer symptoms. (n.d.). MD Anderson Cancer Center. Retrieved June 16, 2024, from https://www.mdanderson.org/cancer-types/skin-cancer/skin-cancer-symptoms.html
- Skin cancer types: Melanoma Self-care after treatment. (n.d.). Retrieved June 16, 2024, from https://www.aad.org/public/diseases/skin-cancer/types/common/melanoma/self-care
- Skin phototype (Fitzpatrick skin type) | DermNet. (n.d.). Retrieved June 14, 2024, from https://dermnetnz.org/topics/skin-phototype
- Squamous cell carcinoma warning signs and images. (2023, March). The Skin Cancer Foundation. https://www.skincancer.org/skin-cancer-information/squamous-cell-carcinoma/scc-warning-signs-and-images/
- Stages and grades of skin cancer. (2023, January 24). https://www.cancerresearchuk.org/about-cancer/skin-cancer/stages-grades
- Support resources. (2024, April). The Skin Cancer Foundation. https://www.skincancer.org/treatment-resources/support-resources/
- Urban, K., Mehrmal, S., Uppal, P., Giesey, R. L., & Delost, G. R. (2021). The global burden of skin cancer: A longitudinal analysis from the Global Burden of Disease Study, 1990–2017. JAAD International, 2, 98–108. https://doi.org/10.1016/j.jdin.2020.10.013
- What causes skin cancer: Risk factors other than sun or uv rays. (2022, June 1). City of Hope. https://www.cancercenter.com/cancer-types/skin-cancer/risk-factors
- National Cancer Institute (AV Number: AV-8500-3850; Date Created: 1985; Date Entered: 1/1/2001), https://visualsonline.cancer.gov/details.cfm?imageid=9186
Disclaimer:
Use of Course Content. The courses provided by NCC are based on industry knowledge and input from professional nurses, experts, practitioners, and other individuals and institutions. The information presented in this course is intended solely for the use of healthcare professionals taking this course, for credit, from NCC. The information is designed to assist healthcare professionals, including nurses, in addressing issues associated with healthcare. The information provided in this course is general in nature and is not designed to address any specific situation. This publication in no way absolves facilities of their responsibility for the appropriate orientation of healthcare professionals. Hospitals or other organizations using this publication as a part of their own orientation processes should review the contents of this publication to ensure accuracy and compliance before using this publication. Knowledge, procedures or insight gained from the Student in the course of taking classes provided by NCC may be used at the Student’s discretion during their course of work or otherwise in a professional capacity. The Student understands and agrees that NCC shall not be held liable for any acts, errors, advice or omissions provided by the Student based on knowledge or advice acquired by NCC. The Student is solely responsible for his/her own actions, even if information and/or education was acquired from a NCC course pertaining to that action or actions. By clicking “complete” you are agreeing to these terms of use.
➁ Complete Survey
Give us your thoughts and feedback
➂ Click the Green MARK COMPLETE Button Below
To receive your certificate
