Course
Transitioning to the Nurse Educator Role
Course Highlights
- In this Transitioning to the Nurse Educator Role course, we will learn about the role of the Nurse Educator in academic and clinical settings.
- You’ll also learn how the Nurse Educator role is important in healthcare.
- You’ll leave this course with a broader understanding of at least three qualifications Nurse Educators must have to work in the academic setting.
About
Contact Hours Awarded: 3
Course By:
Kayla M. Cavicchio
MSN, RN, CEN
Begin Now
Read Course | Complete Survey | Claim Credit
➀ Read and Learn
The following course content
Introduction
The Nurse Educator role is one of great importance in both the academic and clinical settings. Nurse Educators are responsible for teaching the next generation of nursing, facilitating learning experiences for the bedside nurse, leading initiatives, and a lot more. The nurses coming into these roles may only have minimal training if they do not possess a master’s degree in nursing education. This course is designed for the nurse with a bachelor’s degree in nursing that is interested in becoming a nurse educator or improving their current skillset and knowledge base.
What is a Nurse Educator?
The Nurse Educator, in its simplest form, is a registered nurse that educates in a variety of settings. However, that definition is not all encompassing (8).
To understand the complex role of the Nurse Educator or the Nursing Professional Development Practitioner—abbreviated NPDP or NPD Practitioner—we must first understand the scope of practice and what it defines. The questions answered within the scope of practice are who, what, when, where, why, and how. The answers guide the Nurse Educator through their daily tasks. Since many stakeholders have a say in nursing practice, the scope of the Nurse Educator role is continuously changing, and it is important for Nurse Educators to be aware of their scope of practice (8).
The Association for Nursing Professional Development’s NPD Practice Model is guided by the work of Katz and Khan’s 1978 characteristics of Open Systems Theory. The characteristics include input, throughput, and output that repeat in a cyclic pattern. Input consists of items from the external environment, like resources or people. Throughputs are the actions or processes within the system created to change the inputs. Lastly, the outputs are the results of the throughput actions and are sent out into the environment. They provide feedback and subsequentially start the cycle over again (8). Figure 1 (below) reflects this continuous cycle.
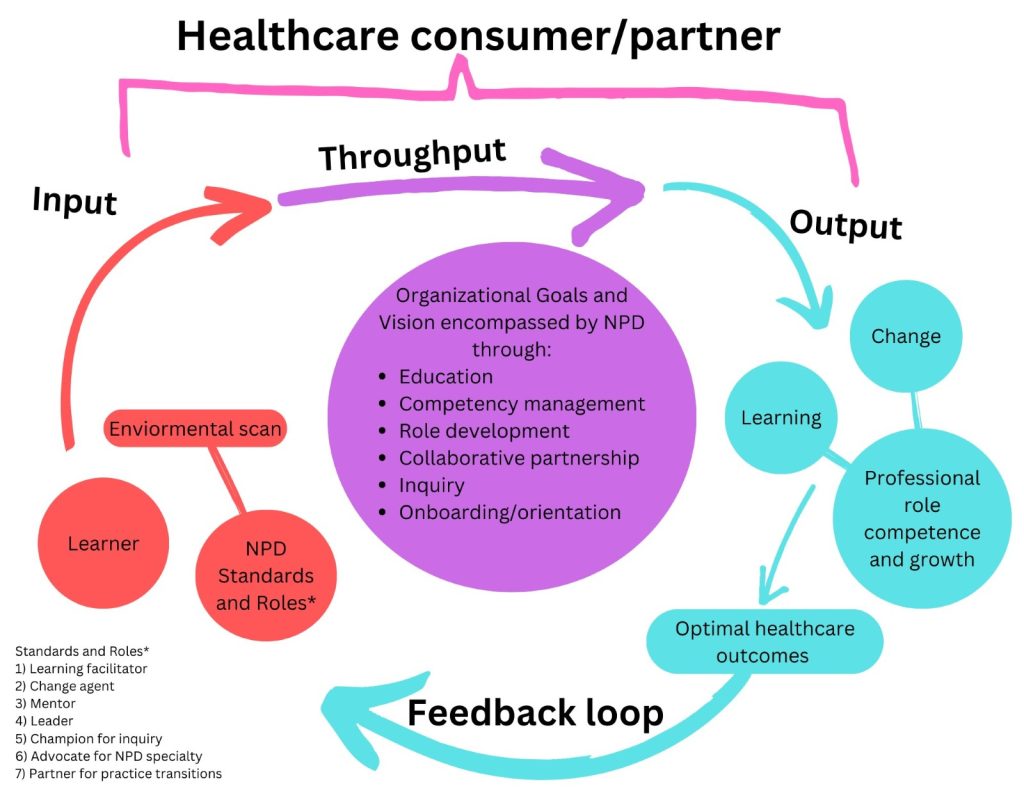
Figure 1: Open Systems Theory
As you may have noticed, the very top of the diagram mentions “healthcare consumer/partner.” The healthcare consumer/partner is the patient, client, individual, family, community, group, or population that partners with the healthcare providers to partake in decision-making about care, activities, treatment, or therapies that promote health. This is the focus of everything the Nurse Educator does. If nursing practice is not aligned with the standards set by the patient, family, community, or governing agencies, then there are consequences such as a loss of funding or accreditation, loss of patients, and loss of jobs. That is why it is important for the Nurse Educator to be aware of the inputs and guide education appropriately to ensure optimal care for the populations served (8).
Input
Within the input section of this model, the questions of “when,” “who,” and “how” are answered (8).
When: This is a continuous process done by the Nurse Educator through internally scanning the environment to make determinations if there is a professional practice gap. These environmental scans consist of data collection from a variety of sources within and outside of the organization. If the data shows a gap exists, the Nurse Educator can determine if the gap can be rectified by education, or if the gap needs to be addressed by other Nurse Educators in other roles or the organization itself (8).
Scanning the environment also helps the Nurse Educator plan for change. Healthcare is constantly advancing in legislation, policies and procedures, technology, and practice. If Nurse Educators are unaware of these changes, they will not be prepared to educate themselves and their target audience appropriately. Their actions become reactive instead of proactive to the needs of their audience and the organization’s strategic goals (8).
Who: The learner and the Nurse Educator impact the nursing professional development model and the success of measurable outcomes. The learner and the Nurse Educator are two separate entities that connect and interact closely with one another, moving towards change in the form of learning, growth, and professional role competence to achieve optimal population health (8).
Before moving on, it is important to define what a learner and Nurse Educator is. For the purpose of this course, learner(s) will be defined as an individual or group of individuals that have a gap of knowledge, practice, and/or skill, and who actively participate in professional development activities. These learners assume accountability and responsibility for learning, change, growth, and professional role competence. These individuals can include anyone within the organization and those who partner with the organization (8).
NPD Practitioners, or Nurse Educators, are registered nurses that have nursing professional development expertise and judgement that influences growth and professional role competence of learners in a variety of settings, for the betterment of population health. However, Nurse Educators are not just teachers. The following are seven roles that encompass the Nurse Educator: (8)
- Learning Facilitator: Utilizing adult learning principles and the educational design process, the Nurse Educator bridges the knowledge gaps in practice to ensure optimal patient outcomes.
- Change Agent: The Nurse Educator is an active participant in the change process on a micro, meso, and macro system level. They use change management strategies and theories to reach desired outcomes.
- Mentor: Nurse Educators form supportive relationships with those that they oversee. They use role-modeling, feedback, and guidance to support the learner’s growth. At a long-term level, mentoring is different than precepting or coaching. Mentoring is used to support the professional development of others and continuous professional learning.
- Leader: Leadership for the Nurse Educator is not always recognized since it is usually peer collaboration leadership. This is opposed to traditional leadership in which the change/information comes from the higher ups with no input from bedside staff.
- Champion for Inquiry: “Why” is a powerful question that can lead to important advancements within healthcare. Through dissemination of new knowledge, Nurse Educators encourage the spirit of inquiry in themselves and others. They may even seek to generate new knowledge through research or contribute to the pool of knowledge by performing quality improvement projects based on evidence-based practice.
- Advocate for NPD Specialty: Nurse Educators have a responsibility to each other to continuously advocate for the NPD specialty. True nursing professional development is more than handing someone an online module and hoping a change is made. Some do not realize how valuable Nurse Educators are, so it is the duty of Nurse Educators to support, promote, and demonstrate NPD as a specialty.
- Partner for Practice Transitions: Nurse Educators encourage nurses and other unlicensed assistive personnel to advance clinically within their profession through education, certification, and clinical role advancement.
Nurse Educators may utilize staff on their team to assist with education. The Association for Nursing Professional Development reflects on other roles that are vital to professional development that do not have the experience, credentials, or desire to be a formal Nurse Educator (8).
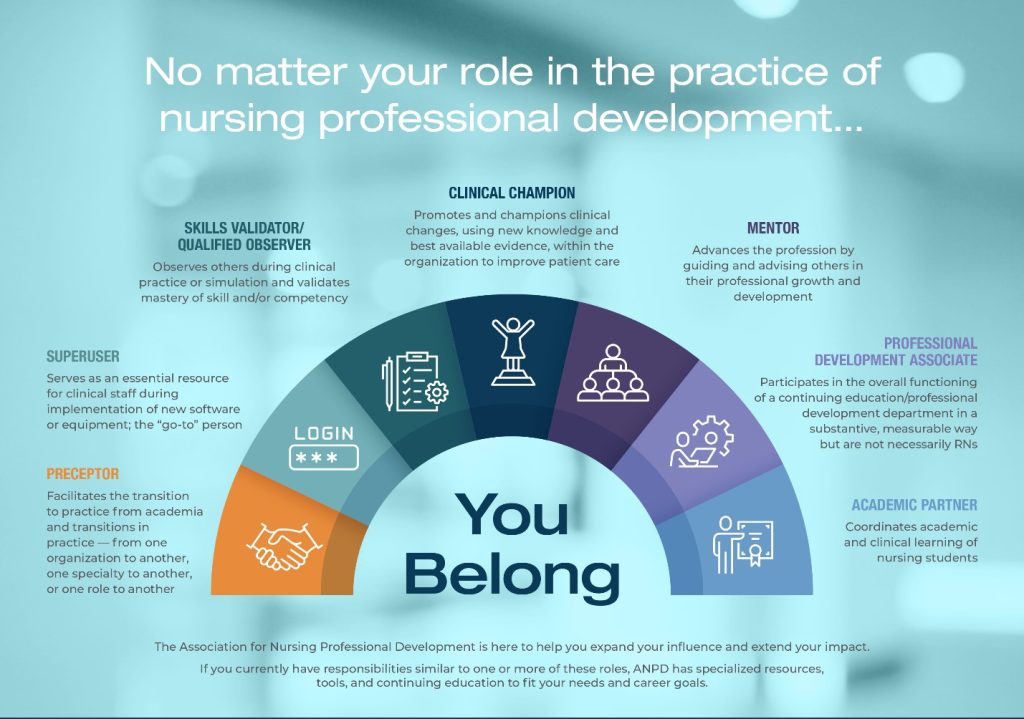
Figure 2: in Nursing Professional Development Roles (2)
As you can see in Figure 2, there are many ways to influence nursing professional development. If you are interested in a future career as a Nurse Educator, see what you can do now to gain experience through opportunities your Nurse Educator might have available (8).
How: The way the Nurse Educator functions is guided by the standards of NPD practice. Standards are used to define the expected minimal level the Nurse Educator must be able to meet. Nurse Educators should also be aware of scope and standards of practice for the specialty of the learners. For example, the Emergency Nurses Association has created scope and standards of practice for nurses working in the emergency department while the American Psychiatric Nurses Association created standards for psychiatric-mental health nursing (8).

Self Quiz
Ask yourself...
- Think through your nursing career, prior to being a Nurse Educator (if you are currently one), what roles did you perform during your time as a bedside nurse?
- Did some of these roles come naturally to you? What ones were your favorite and least favorite?
- If you are not a Nurse Educator, what roles would you like to explore more prior to becoming a Nurse Educator?
- If you could add one role to the list of Nurse Educator roles, what would it be? Why do you think that role is important in nursing education?
- What question in the input process—when, who, how—do you think is the most important? Why?
Throughput
The throughput processes of the Nursing Professional Development Practice Model transform the inputs through different methods to create the outputs via the experience. These throughputs represent the “what” question of the Nurse Educator’s scope of practice while the “why” is based on organizational goals and strategic plans (8).
Why: As already mentioned, the answer to “why” is based on the organization’s mission, vision, goals, and strategic plans. These are used to guide the Nurse Educator with decision-making and setting priorities related to the inputs (8).
What: The “what” is the responsibility of the Nurse Educator. Categorized into six major topics, the Nurse Educator focuses on onboarding/orientation, competency management, education, role development, collaborative partnership, and inquiry (8).
- Onboarding is an overall concept of hiring, orienting, and integrating new employees or students into the organization while orienting is a process within onboarding. Orientation is when the process of changing roles, practice, and responsibilities within those new roles occurs. Prior to a job, an employee may have worked in the fast-food industry. They might have some customer service skills but may not have a full understanding of the expectations based on their new role within the new organization. The Nurse Educator’s job with onboarding and orientation may vary based on their role. Expectations can range from conducting the entire onboarding process or individual parts within (8).
- Competency management involves ensuring that staff meet the minimum level of practice standards within their role through knowledge, ability, judgement, and skills. This is measured by using various tools to collect subjective and objective data on performance. Nurse Educators accept responsibility for verifying, measuring, documenting competence, and supporting the continued process of ensuring competency. They must also be ready to address gaps in competency (8).
- Education starts during the learner’s academia period and continues throughout their careers. Nursing is a profession of life-long learning. Nurse Educators must be able to meet the learners where they are in knowledge, skill, judgement, and ability and successfully ensure they meet and maintain competence. Continuing education is more than a requirement for re-licensure. This type of education stems from foundational knowledge and helps the learner expand their understanding and practice on certain topics (8).
- Role development is the growth through ongoing professional learning. This can be done through role transition and integration, acquisition of skills, and the mastery of their specialty. Specific examples include development of preceptors and/or leaders as well as transition to practice programs. Some organizations have internship programs for those entering specialty areas: critical care, emergency department, progressive care, labor and delivery, oncology, and behavioral health (8).
- Collaborative partnerships focus on a mutual partnership between two or more people or entities working towards a common goal. An example is interdisciplinary care. Providers from various specialties come together to provide care for patients in order to ensure optimal patient outcomes. Nurse Educators can be in collaboration with academic institutions to train nursing students, emergency medical services for disaster management, or public health for primary care promotion (8).
- The spirit of inquiry is the continued, internal professional curiosity that is vital to the modern Nurse Educator role. This can encompass research (generation, synthesis, translation, application, and dissemination of new knowledge into the profession to improve patient care) and scholarship (discovery, teaching, practice, and integration into the profession). Research can be part of the scholarship process for Nurse Educators as well as evidenced-based practice and quality improvement projects (8).

Self Quiz
Ask yourself...
- What are some other ways the Nurse Educator can encourage role development?
- How can Nurse Educators collaborate with others outside of their primary work setting?
- Who do you think should be responsible for the orientation process? The Nurse Educator, the manager, the preceptor? What is your reasoning?
- Why do you think the organization’s vision and strategic goal are so important when designing education?
- What other responsibilities of the Nurse Educator do you think should be included in the above list? What makes them important to you?
Outputs
Now, we will discuss the outputs of the Nursing Professional Development Practice Model. Outputs are directed by the “why” of the Nurse Educator’s role: “Why do we do what we do?” The answer is “optimal health for all patients through best practice.” The Nurse Educator supports this by leading and engaging learners into the process (8).
As covered previously, the outputs are learning, change, and professional competence and growth (8).
Learning is the gaining of skills, knowledge, judgment, and abilities that providers base their practice on. Learning is the foundation and prerequisite for change and must be based on a variety of factors: individual or group characteristics, educations methodology, and perceived needs (8).
Change is the intentional altering of a current state of things and becomes a cornerstone for future changes. For change to be successful, those undergoing the change must accept and adopt the change. This leads to professional role competence and growth (8).
Professional role competence focuses on the ability to meet a set of practice standards or criteria based on specialty area, model of practice, and context in which an individual participates. One way nurses can demonstrate professional role competence is through specialty certification. This validates and demonstrates the nurse’s knowledge to employers and patients. While certification is a fantastic way to display professional role competence, the total number of nurses certified varies by specialty and certification (8). An example of those certified is from the Board of Certification for Emergency Nursing (BCEN). From January 1, 2022, to December 31, 2022, the BCEN reported the following numbers for certification [Figure 3]:
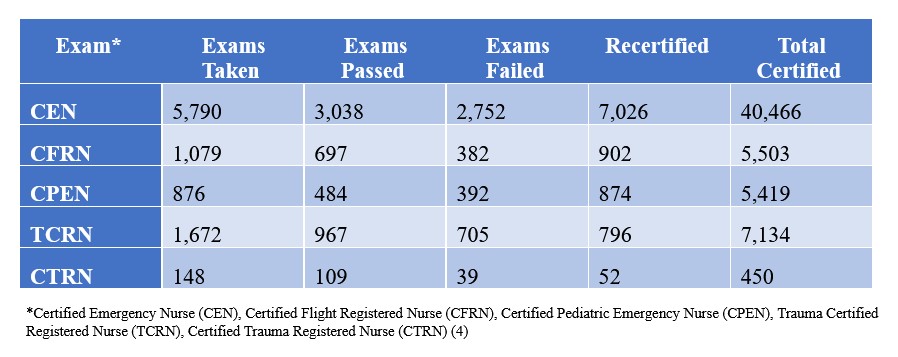
Figure 3: Board of Certification for Emergency Nursing 2022 Certification Numbers (4)
Certification examinations are often difficult to pass as they are geared towards a certain specialty and expect the examinee to have a foundation within nursing. This is opposed to the NCLEX which focuses on entry-level nursing.
As nurses progress through Benner’s Stages of Clinical Competence—a subject that will be covered in more detail further in this course—they display growth within their profession which can also be displayed through certification. A novice nurse in the emergency department will not have the knowledge and skillset needed to answer the questions in the exam correctly as they are a novice in that specialty. Nurse Educators can become certified in nursing professional development (more certifications will be discussed later) (8).
Figure 4 (below) is a depiction of the output process. Remember, learning must come before change. Both learning and change influence and lead to professional role competence and growth.
Figure 4: Output Process of the Nursing Professional Development Practice Model
Outputs also have outcomes (the differences made by outputs). These outcomes include:
- Optimal care – interprofessional, collaborative, evidence-based practice-guided care that is safe, high-quality, and equitable for all that seek it.
- Population health – positive outcomes of health for a group of individuals that includes equitable distribution of care to reduce health disparities.
Feedback
Feedback is the final stage of the Nursing Professional Development Practice Model. Nurse Educators are expected to evaluate the process implemented to determine if outcomes have been met. If so, reinforcement and encouragement is given at certain intervals to ensure the behaviors are permanently adopted. If the outcomes are not met, then the Nurse Educator must determine why they have not been met and make appropriate changes to the process to ensure that the proper outcomes are met.

Self Quiz
Ask yourself...
- Are there other answers to the “why do we (as educators) do what we do” besides patient outcomes? If so, what are they?
- Have you looked up the pass/fail rate of the certification examination for your specialty? What information surprised you the most?
- Would you ever consider obtaining certification in your specialty area? Why or why not?
- If you would consider certification, what would you need to do in order to test for that certification? If you would not consider certification, what would need to happen for you to change your mind?
- Feedback allows Nurse Educators to see how the learners are progressing. What else could we use feedback for?
Nursing Professional Development Practice Model: Example
Below is an example of the Nursing Professional Development Practice Model in a real-life situation.
Input (why, when, where, and how): Through environmental scanning, the Nurse Educator notes that the catheter acquired urinary tract infection (CAUTI) infection rates at their facility are above the national average. The Nurse educator identifies this as a practice gap and knows there is an opportunity to improve the care of the healthcare consumer/partner. By performing a gap analysis, the Nurse Educator can make the determination of what is leading to the increased CAUTI infection rates: improper insertion, improper placement of the drainage bag, keeping catheters for longer than needed, initial need for catheter, improper cleaning, etc. The Nurse Educator can use laboratory data, direct observation, and testimony of others to assist in determining the cause.
After observation, it has been noted that the unlicensed assistive personnel are not keeping the catheter drainage bags in the proper position when walking patients. An evaluation of electronic medical record data shows that catheters are left in for extended periods of time when they are not needed. The catheter policy does not have any process in place to determine if a catheter needs to remain or can be removed.
Throughput (what and why): The Nurse Educator formulates and leads implementation of the plan that is aligned with the organization’s goals to ensure optimal population health.
- The Nurse Educator reviews the latest prevention data from reliable sources within the medical community to determine what needs to be changed and how to best implement the change based on evidence-based practice. (champion for inquiry, responsibility – inquiry)
- Collaborate with other departments as needed to create changes to the policy that includes criteria for catheter insertion and removal. (leader, change agent, responsibility – collaborative partnerships)
- Provide education on changes made to the policy and how to hold catheter bags during ambulation. (learning facilitator, responsibility – education)
- Change orientation content to ensure that the policy changes are discussed. (change agent, partner for practice transitions, responsibility – onboarding/orientation)
- Add catheter maintenance to competency assessment for unlicensed assistive personnel. (Responsibility – competency management)
Outputs (why): The Nurse Educator evaluates the effectiveness of the changes made.
- Verification of learning through discussion, post-test, and direct observation/return demonstration.
- Evaluation of change is done through electronic medical record data.
- Professional role competence is done through observation of daily work.
Feedback loop: The results of the evaluation are used to determine if adjustments need to be made to the changes that occurred.
Where do Nurse Educators Work?
As mentioned earlier, nursing and healthcare in general is ever-changing. Therefore, education is needed across the profession at all stages of nursing.
Academic Setting
Nursing education starts in the classroom, with nursing students eager to pursue a career in healthcare. Nurse Educators can teach in the classroom, providing lectures and traditional classwork, or they can teach clinicals, providing guidance and supervision during the students’ time in the clinical setting. Some educators may perform both roles. Table 1 (below) compares the two roles.
|
|
Academic Clinical Nurse Educator
|
Academic Nurse Educator
|
|
Definition |
Registered nurse that facilitates the clinical learning process of nursing students as required and trained by academic preparation.
|
Registered nurse that facilitates classroom learning and success in the academic setting. |
|
Requirements |
Graduate degree: Master of Science in Nursing (MSN), Doctor of Nursing Practice (DNP), or Doctor of Philosophy (PhD)
|
Advanced nursing degree: Master of Science in Nursing, Doctoral degree preferred, Current in nursing specialty |
|
Certification/Secondary Licensure |
Certified Clinical Nurse Educator (CNEcl)
|
Certified Nurse Educator (CNE) |
|
Roles/Responsibilities |
Direct supervision and evaluation of performance for students while they are in the clinical setting. |
Teaching, scholarship, and service (to students, university, community, and profession)
|
|
Assessment of educational needs/requirements |
Confers and collaborates with the Academic Nurse Educator to determine proper outcomes for clinical experiences. |
Analyzes the standards set forth by accrediting bodies to ensure that content taught in the classroom setting is in compliance with regulations.
|
|
Populations served |
Nursing students
|
Nursing students |
|
Short-term goals |
Success of students in the clinical setting through achievement of learning outcomes set by the Academic Nurse Educator and the Academic Clinical Nurse Educator.
|
Success of students within the classroom setting by meeting learning outcomes. |
|
Long-term goals |
Safe clinical practice |
Students obtaining degrees, successful licensure obtainment, and success of employment
|
|
Setting |
Varies depending on clinical setting
|
College or university |
Table 1: Comparison of Academic Clinical Nurse Educator and Academic Nurse Educator Roles (8)
Clinical Setting
Nurse Educators within the clinical setting focus their attention on staff, patients, or both depending on their role and expectations. Table 2 (below) compares the roles of the NPD Practitioner and Clinical Nurse Specialist (CNS).
|
|
NPD Practitioner |
Clinical Nurse Specialist (CNS)
|
|
Definition |
Registered nurse that influences professional role competence and growth in the target learner population in a variety of settings. |
Advanced practice registered nurse (APRN) that integrates care with the goal of continued improvements to nursing care, resulting in desired outcomes. |
|
Requirements |
|
|
|
Certification/Secondary Licensure |
|
|
|
Roles/Responsibilities |
Seven roles:
Six responsibilities:
|
|
|
Assessment of educational needs/requirements |
|
Assesses nursing practice for improvement opportunities. |
|
Populations served |
Practicing healthcare staff |
|
|
Short-term goals |
|
Improving care and outcomes |
|
Long-term goals |
|
Improving patient outcomes |
|
Setting |
Varies based on role, organization, and collaborative partnerships
|
Varies based on practice setting |
Table 2: Comparison of the Nursing Professional Development Practitioner and Clinical Nurse Specialist Roles (8)
Importance of the Nurse Educator Role
Since being recognized as a unique disciple in the 1800s, nursing has been tasked with the responsibility of education. Overall, education focused on the patient or community in which the nurses served, but Florence Nightingale advocated for education of the nurse. She created the first nursing school and educated nurses, physicians, and other health officials about the importance of proper hospital conditions to improve patient outcomes. Many organizations over the years have recognized how educating the nurse from the beginning to the end of their career can be beneficial for both patients and individuals who work with the nurse (3).
Regulatory bodies require education for a variety of skills and specialties. They ensure staff know policies and procedures, proper ways to dispose of hazardous waste, and how to activate emergency systems such as a “code blue” for a patient in cardiopulmonary arrest. Re-licensure requires continuing education, and those that obtain certification can complete a set number of continuing education hours for recertification. Completing these hours proves that the nurse is aware of relevant changes or updates to practice (8).
These are a few of the reasons why Nurse Educators are important. They come with expertise in areas of nursing that require constant adaptability and innovation to ensure optimal patient outcomes. The Nurse Educator must know all aspects of their role and the requirements of those who they oversee. Without Nurse Educators, regulatory education requirements might be missed, orientation and onboarding may not be consistent with each new staff member, staff may not be updated on the newest changes, and staff may not know how to operate equipment. Nurse Educators are a vital part of the healthcare setting.

Self Quiz
Ask yourself...
- Between the two roles, which are you more interested in, academic nurse educator or clinical nurse educator? Why?
- Do you have any experience in either role as an adjunct instructor or superuser for a new piece of equipment on your unit? Was it what you expected?
- Do you think education requirements from regulatory agencies are becoming extensive? Why or why not?
- Were there any Nurse Educators in your life that stand out in your mind, good or bad, and why do they stand out in your mind?
- What are some other reasons why Nurse Educators are important?
Basics of Nurse Education
As discussed, nursing education encompasses much more than teaching a class or a new skill. Nurse Educators must understand the process of performing a needs assessment. They must also know how to ensure the most up-to-date content is being used, determine learning styles, appeal to the adult learner, create learning objectives, communicate, manage conflict, and evaluate the process.
Needs Assessment
The needs assessment is the process of determining where gaps in knowledge lie and how to properly address it. But how do educators know what the goal is? How do they know what they need to do? A quote by author Steven Covey sums up the answer quite well: “Being with the end in mind.” If your goal is to ensure emergency department nurses are able to place ultrasound guided intravenous lines (IV), then you need to ensure your education program gives them proper pre-work, practice, and validation methods to ensure competence. If you simply want unlicensed assistive personnel to be aware of a new physician paging process, you may give them an educational flyer with the steps on how to properly page providers with in-person support during the first few days of the process changing (12).
Ways to identify the goal can involve looking at current problems or anticipating future problems within the department, facility, organization, or nursing profession as a whole. Proactive action is better than reactive action. It allows those responsible for addressing the problem to be more prepared (12).
An example is safety rounding on behavioral health units. Facility A and Facility B have the same rounding checks time frame; every 15 minutes they are to visualize the patients to ensure they are alive and safe. Both facilities have had past instances where patients have attempted to harm themselves during the 15 minutes when they are not being observed. Facility A makes the decision to change the round time to ten minutes, meaning the patients are observed more frequently. Facility B does not make this change. A few months later, Facility B has a patient successfully harm themself and the team is now reacting to the situation and rushing to implement a new change.

Self Quiz
Ask yourself...
- Regarding these two facilities, which do you think was able to carry out a proper needs assessment and why?
- Was a facility wrong in their approach to the “near misses” that were occurring on their units? Why or why not?
- If you were the educator at Facility B and you heard what Facility A was doing, what could you do to implement the same changes before the patient had harmed themselves?
- If you were the educator at Facility B and you heard what Facility A was doing, what could you do to encourage implementation of the same changes after the patient had harmed themselves?
- If Facility A and Facility B were within the same organization, and you were the educator for Facility B, would you be willing to reach out to get information from the educator from Facility A? Vice versa?
The needs assessment can also be used when there are changes to role descriptions that require training. Refer back to the ultrasound IV insertion example. Some facilities are now requiring nurses in specialty areas to become trained to perform skills that may have been once performed by a physician or a nurse on an “IV Team.” The emergency department and intensive care units are areas where these skills would be beneficial as nurses in these areas encounter critically ill patients with limited vascular access. Sometimes the provider is not immediately available to insert a centrally inserted venous catheter line.
In this case, a peripherally inserted line can be a temporary solution. However, if not properly trained, nurses can accidentally access arteries or poke nerves, leading to pain and possible nerve damage. Need assessments can also be conducted due to the general needs of the industry, thematic or programmatic areas, or social, political, or economical needs (12).
How does a Nurse Educator conduct a needs assessment? The tools involved in a needs assessment vary depending on the Nurse Educator. Multiple tools and methods should be utilized in order to ensure that the needs assessment is thoroughly completed. Observations, questionnaires, consultations, data, and self-assessment/tests are a few ways that a needs assessment can be completed. The strengths, weaknesses, opportunities, and threats (SWOT) method can be used with committees or focus groups. Each component is addressed separately, and topics are separated into the categories as depicted in Figure 5 (below) (12).

Figure 5: SWOT Model (Educational Needs Assessment Tool) (12)
Nurse and education activist Donna Wright created her own model similar to the SWOT model; however, her topics are listed under the following categories: New, Changes, High-risk, and Problematic. The following is a table (Table 3) based on Wright’s Competency Assessment Model (21).
| Potential Competency Needs |
Priority (High, Medium, Low)
|
| What are the NEW procedures, policies, equipment, etc. that are affecting the job? |
High: STAT paging on-call providers Medium: New infant warmer for neonates born in the emergency department. Low: New Foley catheter brand
|
| What are the CHANGES in procedures, policies, equipment, etc. that are affecting the job? |
High: STAT paging on-call providers Medium: New infant warmer for neonates born in the emergency department.
|
| What are the HIGH-RISK aspects of the job that can cause harm, death, or legal action? |
High: Increase in delivery of neonates in an emergency department that does not have a dedicated labor and delivery unit at facility but has on-call obstetric providers.
|
| What are the PROBLEMATIC aspects of the job that can be identified through patient or staff surveys, quality monitoring, and incident reports? |
Low: Long waits to be seen by a provider. Low: Increased door-to-urine collection time Low: Lack of completed duties from unlicensed assistive personnel.
|
Table 4: Implementation of Donna Wright’s Competency Assessment Model (Example) (21)

Self Quiz
Ask yourself...
- Based on Table 4 above what do you think would be the most important topics to address as an educator?
- With the few topics listed, what other topics could you anticipate being of concern for this particular emergency department?
- What resources might be useful for educating on the topics listed?
- Do any of these topics seem to be a management issue as opposed to an education issue?
- How many of these topics do you think you should address at a time? Why?
As you can see in the above example, there are a few topics that could be considered a manager concern, not an education one. A good question to ask is “if we [fill in the blank], would we still have this problem?” Sometimes the answer to that question is not clear and requires more investigation (12).
Going back to Table 4, “lack of competing duties by unlicensed assistive personnel” is listed. If we educate, would we still have the problem of unlicensed assistive personnel not competing their assigned duties?” The answer could be yes or no, depending on what else you know about the staff. If you knew the staff was new, inexperienced, or had their role description changed, then yes, education could very well help with the problem.
However, if the staff was seasoned, experienced, and had not undergone any role changes, the answer would lean towards no. In this case, the lack of competing assigned duties from unlicensed assistive personnel is something the manager would need to investigate and address appropriately. Nurse Educators can emphasize roles and expectations in onboarding and orientation, educate new-hire staff, and provide refresher education to current staff. However, if a staff member is not performing their job correctly, the manager needs to have a discussion with that individual. The Nurse Educator should be available to assist the manager if needed during this process, offering any education that was used in onboarding/orienting the new hire.
Evidence-Based Practice
Once the education needs have been identified, the Nurse Educator needs to go to the literature to ensure that policies and procedures are following best practice. Best practice is pulled from random controlled trials that are synthesized into systematic reviews. If 50 out of 52 random controlled trials say central line catheter dressing changes should be done twice a week due to a significant change in bacteria growth, it is in the best interest of the patient for organizations to start performing dressing changes twice a week. However, if 50 out of 52 trials stated there was no significant change, then the facility should evaluate time, supplies used, costs, staff needed to perform changes, and other factors before implementing the change. This is why evaluation of best practices should be done prior to implementing a project (3).
There are many ways to obtain evidence-based practice articles, some of which may be provided by your facility.
- Most healthcare organizations have some form of a medical library with access to journal articles though various databases (6):
- Cumulative Index to Nursing and Allied Health Literature (CINAHL)
- Medline with Full Text
- PubMed
- Nursing Reference Center Plus
- Cochrane Library
- JBI EBP Database
- ProQuest
- Your academic institutions may offer the same databases but have access to different journals or sources. Even if you are not a Nurse Educator in academia, or you are no longer in school, some institutions allow you to maintain access to these databases by simply having your login for that institution.
- Evidence-based practice specialists or committees can be valuable resources when performing a needs assessment. Not every organization has these options, however, Nurse Educators with access to these resources should utilize them whenever possible.
- Nursing organizations often produce journals containing research articles. These articles are often geared towards the overall topic of the organization. For example, the Emergency Nurses Association has the Journal of Emergency Nursing that publishes research articles regarding all things emergency nursing.
- Google Scholar can be used. Some articles can be accessed for free.
- Reliable medical institutions within healthcare may be used such as Johns Hopkins, Cleveland Clinic, Mayo Clinic, Centers for Disease Control and Prevention, World Health Organization, American Heart Association, and universities like the University of Michigan.
Tips:
- The process of finding evidence-based articles that fit the topic can be challenging. Ensure you try all variations of the topic—cardiopulmonary resuscitation, CPR, resuscitation, code blue, etc.—to broaden your reach. Authors do not always use the same terms when discussing topics as many databases hold articles from all over the world.
- Ensure that you expand the year range as much as you reasonably can. For example, CPR algorithms have changed over the years, so you do not want to pull content from 1980. However, if you are having a challenging time finding research, go further back in time. It is possible that there have not been significant changes or research conducted on your topic recently.
- Ask for help if you are having trouble, especially if you have someone who oversees the medical library like evidence-based practice specialists or an evidence-based practice committee.
Learning Theories
This section will cover several learning theories, including the Adult Learning Theory, Bloom’s Taxonomy, Behaviorist Theory, Neuropsychological Theory, and the Theory of Social Learning.
Terms to Know:
- Andragogy – education of adults
- Pedagogy – education of children
- Cybergogy – combination of pedagogy and andragogy to teach adults via online learning
Adult Learning Theory: Malcolm Knowles
To understand and successfully teach adult learners, we must first discuss the Adult Learning Theory. Malcolm Knowles – an educator that pioneered the theory – proposed that adults learn best when (Teaching in Nursing):
- They understand the “why” behind the subject.
- “Why is it important to me?”
- “What’s in it for me?”
- “Where is the evidence to support this?”
- They are given the ability to learn the subject in their own way. Adults want to be in control as much as possible when it comes to learning. Many adults are in control of various aspects of their lives. Therefore, not being able to have a say in how they learn can lead to feelings of negativity surrounding learning. The more learners are able to assist with the process from planning to completion, the more buy-in educators are likely to have.
- Learning is based on experience to solve real problems. Experiences help learners grow, so encouraging learners to share those experiences can allow others to benefit from that story. If a nurse made a medication error that resulted in a negative patient outcome, then the experience may teach others to always use proper patient and medication verification methods when administering any medication.
- The time is right for them to learn. If overwhelmed with tasks, and a new education module is expected to be done correctly, learners most likely will not prioritize the learning and instead focus on work-related tasks. If the subject being taught does not impact their daily workflow, learners are less inclined to care about the subject. For example, if the oncology floor is starting a new process for medication administration and all nurses—regardless of if they work in oncology or not—must complete the training, there may be many nurses that will become frustrated with the training. On the other hand, other nurses impacted by the change may be more willing to learn due to the impact on their daily workflow.
- The process is engaging and positive. If learners are disengaged from the learning process, the Educator may have a challenging time meeting learning needs. Some team members may scan through the course because it is unengaging.
Intrinsic and extrinsic feedback and factors also affect the learning process. Intrinsic feedback is an internal response to give learners a feel or sense of how they are or have performed. Extrinsic feedback, on the other hand, is the response generated by the Educator or other individual through verbal or nonverbal cues on how the learner performed (3). The Nurse Educator should be aware of the following factors which can greatly impact the learning experience, and make changes where feasible:

Figure 6: Intrinsic and Extrinsic Feedback of the Learning Process (3)
Case Study: The behavioral health unit has received grant funding from their organization’s foundation. The money will be used to purchase special medical beds that are safe for behavioral health and will allow the unit to expand their patient criteria. The team is required to go through additional training to ensure they are able to provide proper care for these new patients. During training, the team members are frustrated with the process, and vocalize their frustrations to the Nurse Educator. They say they were not made aware of the change until the beds had been purchased, nor did anyone ask about their thoughts. They state that they are not getting paid more for the extra work they are required to do for the patients.

Self Quiz
Ask yourself...
- From the case study, what are the intrinsic and extrinsic factors that the team members are experiencing?
- If you were the Nurse Educator in the case study, what could you say to the team members that are expressing frustration with these changes?
- What are some ways you can address intrinsic and extrinsic factors?
- Who else could you involve in the process to help you with these concerns?
- If you were involved in the planning process, what could you have suggested to alleviate some of these factors before they became issues?
Bloom’s Taxonomy: Benjamin Bloom
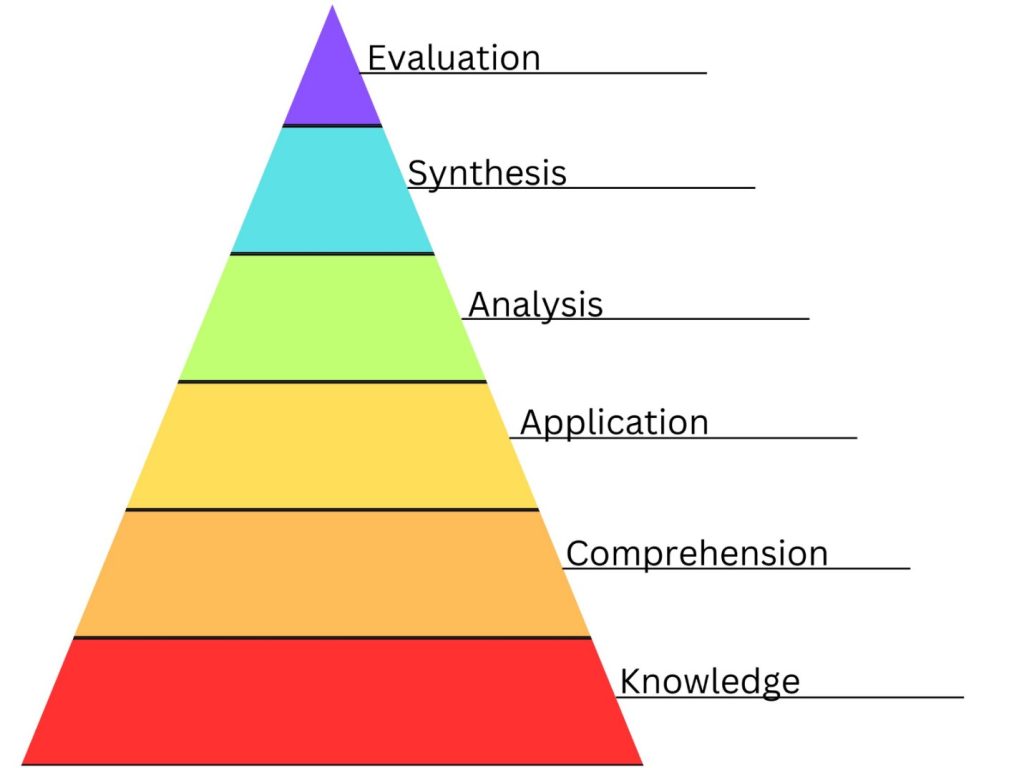
Bloom’s Taxonomy, developed by Benjamin Bloom and other collaborators, highlighted categories of educational goals that have been utilized by educators to guide their teaching and ensure learners have met outcomes in a meaningful way. The initial Taxonomy was created in 1956 with revisions made in 2001. Figure 7 and 8 (below) are both Taxonomies with associated categories.
Bloom’s Initial Taxonomy
Categories:
- Knowledge – the recall of processes, patterns, specifics, setting, or structure
- Comprehension – understanding that verifies the individual knows what is being communicated to them and they can utilize the material.
- Application – using abstracts in certain or concrete situations.
- Analysis – breaking down communication into elements so the hierarchy of thoughts is understood and/or relation between thoughts/ideas is explicit.
- Synthesis – combining elements of a subject or thoughts and making them whole.
- Evaluation – forming judgement about the value of the topic or materials for variety of purposes.
Figure 7: Bloom’s Initial Taxonomy (1)
Bloom’s Revised Taxonomy
Categories:
- Knowledge is at the foundation and includes: (1)
-
- Factual – terminology, specific details
-
- Conceptual – classifications, categories, theories, models, principles, generalizations
-
- Procedural – algorithms, techniques, skills, methods, criteria on when to use certain procedures
-
- Metacognitive – strategic, self-knowledge, cognitive task
- Remember – recognizing or recalling information
- Understand – classifying, explaining, summarizing, interpreting
- Apply – executing or implementing skills or information to make decisions
- Analyze – organizing, attributing, differentiating thoughts or information
- Evaluation – checking or critiquing information
- Create – planning, producing, generating new information
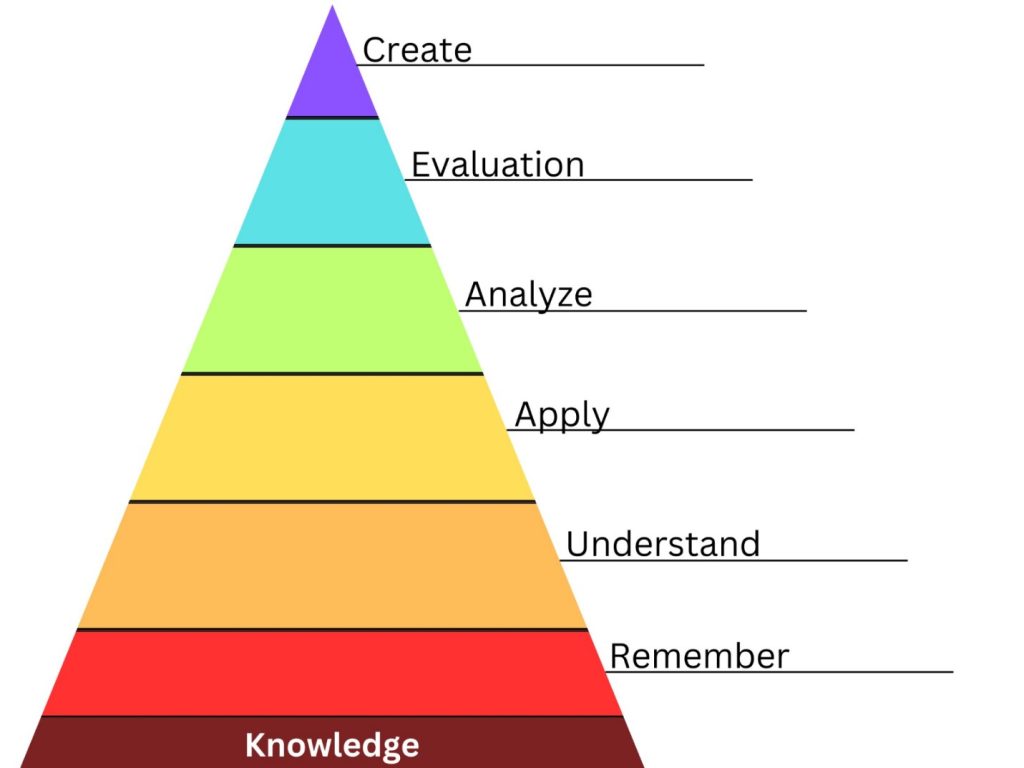
Figure 8: Bloom’s Revised Taxonomy (1)
Creating Learning Objectives
Bloom’s Taxonomy assists Nurse Educators in enhancing learning through the development of skills and knowledge. Nurse Educators can use this tool to assist in creating appropriately leveled, observable objectives. Questions that should be considered when writing objectives include what is expected of the learner that can be observed in some way, to what degree the learner must be able to perform it, and under what conditions the learning must take place. Remember ABCD:
- Audience – who is being taught?
- Behavior – what would you like them to do?
- Conditions – what circumstances does the learner have to meet in order to complete requirements?
- Degree – to what degree/how good do they have to perform in order to pass?
Here are two examples of learning objectives:
- By the end of the cardiac rhythm assessment computer-based learning, learners will be able to identify lethal cardiac rhythms 100% of the time on a post-test.
- During simulation validations, learners will be able to prioritize treatment in order of most important to least important when managing a child with a severe asthma exacerbation 100% of the time.
Behaviorist Theory: John B. Watson & B.F. Skinner
The Behaviorist Theory emphasizes that learning comes from reinforcement, whether it be good or bad. Think of Ivan Pavlov’s dog and classical conditioning.
Pavlov was a Russian psychologist that stumbled upon the classical conditioning theory by accident. He was studying digestion in dogs and noticed that the dog’s reaction to food began to change over time. Initially the dog would only salivate when food was placed in front of it, but eventually began salivating before the food arrived. To test this theory even further, Pavlov would ring a bell before bringing the food. The process was similar. Initially the dog began salivating when the food was present to it, but eventually began salivating when it heard the sound of the bell and before food arrived (14).
The Behaviorist Theory, also known as operant condition, is of the same idea. If learners are presented with positive reinforcement for their achievements, they are likely to continue learning or acting the same way. If the reinforcement is negative, the learner will learn to avoid whatever is resulting in negative feedback.
Neuropsychological Theory: Donald Hebb
Hebb’s theory on neuropsychological changes stemmed from Pavlov. The theory can be summarized into this simple phrase: “cells that fire together wire together.” What this means is that learning is enriched when cells throughout the brain are stimulated. Some individuals say that listening to music, chewing gum, or smelling a certain scent can assist them in memory recall during tests. This is because multiple areas of the brain are working at the same time, causing more cells to fire and develop (9).
Theory of Social Learning: Albert Bandura
The Theory of Social Learning is another theory that builds off of the previously mentioned Pavlov’s classical conditioning as well as operant conditioning. Bandura adds two crucial factors: (10)
- Behavior is learned through the environment through the act of observational learning.
- Facilitating processes occur between responses and the stimuli they originated from.
The phrase “see one, do one, teach one” comes to mind with this theory as the learner first observes, imitates, then models the behavior.
There are many other learning theories available for educators across various professions. Some focus on the learner, while others draw attention to the environment around the learner. It is important that the Nurse Educator focuses on all aspects of the learning theories to ensure they can successfully address the learning needs of those they teach.
Learning Styles and Considerations
This section will cover various learning styles and considerations, including the VARK and VAK tests, Dunn and Dunn Model, Myers-Briggs Type Indicator Assessment, generational learning, and the Novice to Expert Model.
VARK and VAK Tests
The most common learning style assessments are the visual-auditory, reading/writing, kinesthetic (VARK), or the visual, auditory, kinesthetic (VAK) tests. These tests are designed to discover the best method of learning for the learner. Questions are presented about a variety of topics. The tests list the way a learner taking the test would learn about the topic best (18).
Example question:
If I want to learn how to crochet, I would:
- Watch a video.
- Write down the instructions.
- Discuss methods with someone who crochets.
- Use photos showing the steps.
Learners answer the questions and total the number of As, Bs, Cs, and Ds they selected. This will reveal their learning style (or the online version will score the test for them). Some sites that offer these types of tests will also provide the best ways to learn based on that learning style (18).
Dunn and Dunn Model: Rita and Kenneth Dunn
As highlighted earlier, some individuals can learn better under different circumstances. Some learners must study in complete silence by themselves while others enjoy group studying and discussion. Learning advocates Rita and Kenneth Dunn proposed six characteristics that affect the learning process: (17)
- Environment – pertains to where the learners like to learn. As mentioned, some individuals prefer silent environments while others might need a loud environment to learn. Temperature, lighting, seating, other learners, and instructors can all affect how learning occurs.
- Emotional – emotional state can affect learners in a variety of ways. If a learner is not motivated to learn, they may not be successful in any attempts made. If a learner was given shocking news prior to the start of class, they may be preoccupied with the news instead of the topic.
- Sociological – some learners work better alone while others enjoy learning in a group. Some can learn in either environment. Patterns or routines for learning can improve how well the learner retains and remembers content. They may also need little to no support from the educator, or they might need step-by-step support.
- Physiological – by using the VARK/VAK or other assessments, learners can determine their preferred learning method. Any physical interaction learners use when learning can help educators solidify content in the learner’s mind.
- Psychological – this focuses on how learners respond to information and ideas present in the learning material.
Reading through this list created by Rita and Kenneth Dunn, we can see how this content can affect the learning process and meet any learning objectives (17).
Myers-Briggs Type Indicator Assessment
Some Nurse Educators may utilize the Myers-Briggs Type Indicator® (MBTI®) assessment to determine the personality types of their learners: extrovert/introvert, sensing/intuition, thinking/feeling, and judging/perceiving. Learners can fall into one of 16 personality types. Nurse Educators can use the learner’s personality types to help plan, create, and implement positive education. Working to the strengths of others can alleviate negativity surrounding the learning process (16).
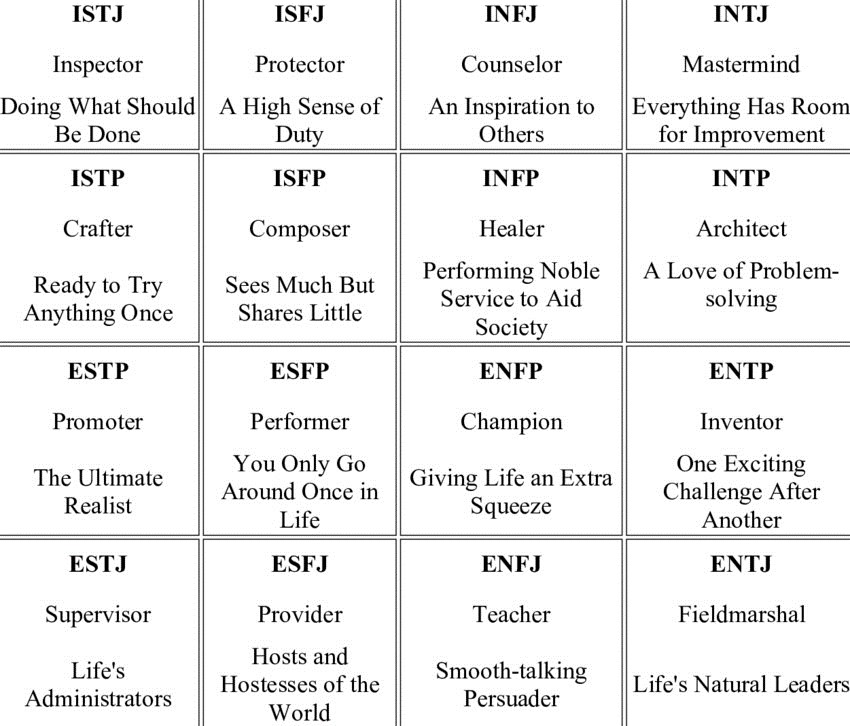
Figure 9: Myers-Briggs Type Indicator® (MBTI®) Assessment (19)
Generational Learning
Table 5 (below) addresses the learning style of past to current generations and outlines learning needs Educators should consider.
|
Generation and Year Range
|
Description | Learning Considerations |
|
Silent/Greatest Generation (1928 – 1943) |
Prefer formal learning methods Need clear instruction, especially with new technology and learning methods Educators are seen as being in authority
|
Clear directions/instructions Classroom or other traditional education methods |
|
Baby Boomers (1946 – 1964) |
Prefers teamwork Values lifelong learning and wants experiences to be valuable |
Want to know why something must be done Group experiences to facilitate learning
|
|
Generation X (1965 – 1980) |
Self-guided learning Wants clear information and expectations Value the outcomes more than the process
|
Wants to know the relevance Wants to be in a good mood while learning |
|
Generation Y/Millennials (1981 – 1996) |
Independent and active learners Wants immediate feedback Wants on-demand access to material
|
Offer 24/7 education options Give a variety of outcomes with immediate feedback |
|
Generation Z (1997 – 2012) |
Technology Motivation to learn: intrinsic and extrinsic factors
|
eLearning Variety of options Feedback |
Table 5: Generational Learning (5, 11, 15)
Novice to Expert Model: Patricia Benner
Nurse Educators should also be aware of the level of experience that learners have. Patricia Benner’s Novice to Expert Model shows how learners grow within their role and the criteria they meet and display at each stage [See Table 6] (below). It is important to note that a team member may have gained many years of experience in their profession, but they may not be an expert in a particular field. Experience does not equal expertise (13).
| NOVICE | ADVANCED BEGINNER | COMPETENT | PROFICIENT | EXPERT | |
|
Estimated time required in one area (not always important) |
0-1 YEAR | 1-2 YEARS | 2-3 YEARS | 3-5 YEARS | 5-7 YEARS |
| FUNCTIONS BY | Rules, principles (exceptions are difficult) | Supervision, guidance, imitation |
Guidelines (e.g., care plans) |
Situational (paradigms, maxims) |
Discretionary judgment, unconscious/ automatic |
| USING…. | Objective, observable data | Mastery of the nursing process | Unconscious application of the nursing process | Confident in own assessments, some second opinions |
Uses data more to validate own “intuition”/knowing (experience helps) |
| DECISION-MAKING | With assistance | Recognizes global & some recurring aspects, begins to interpret some. Weak in pattern identification & cause/effect, especially related to own role/actions. | Discriminates; Correctly ignores some data & steps. Incorporates cause > effect, pathology etc. | Compares causes of same problem & intervenes differently. Anticipates typical & deduces atypical | Zeroes in on subtle cues, changes, and differences others may miss. Knows what to ask and what’s significant |
| ORGANIZATION | Task-oriented, works in “pieces” | Needs help with priorities (Sets same for all, tries to do all; or is crisis-driven) | Organized, efficient. Mastery of procedures & routines | Greater speed & efficiency, especially in problem solving | Quick, automatic judgments; eliminates many options. Less trial & error |
| FOCUS | Procedures, immediate needs. One thing at a time | All data viewed as about equally relevant | Outcome-oriented. Takes responsibility for long-range plans | Holistic; broad perspective & current needs. Revises to reduce consequences. | Envisions possibilities. Anticipates changes & makes contingency plans |
| APPROPRIATE ASSIGNMENTS | Routine patients and care | Uncomplicated situations (not necessarily routine) | Complex care- any patient on unit | Handling multiple demands & tasks simultaneously | Unprecedented situations or roles requiring expertise, leadership, masterful problem-solving, coaching or directing others. Independent functioning. |
Table 6: Patricia Benner’s Novice to Expert Model (13)
As we have seen in this section, learning is more involved than simply giving the learner material and having them understand it completely. Learning is an ongoing, complex process that needs to be addressed so learning can be successful.

Self Quiz
Ask yourself...
- Referring to Table 6 above, from which generation are you? Is the description of your generation accurate?
- Do you find yourself a combination of two generations? Are you at the end of one and the start of another?
- Which generation do you think is the most difficult to teach? Why?
- In your current role, what stage of Benner’s Novice to Expert Model are you? What traits do you recognize in yourself?
- How do you think that will change as you advance in your Nurse Educator role or when you become a Nurse Educator?
Effective Communication and Conflict Management
Nurse Educators need to be able to convey material in an effective manner. If learners do not understand what is being taught due to poor communication, they may become frustrated, disengaged, or perform skills incorrectly. Research shows that this can lead to a risk in patient safety.
Skills for effective communication: (20)
- Personal connections
- Active listening
- Verbal and nonverbal communication
- Compassion
- Respect
- Classroom management (ensuring that order is maintained in the classroom)
Nurse Educators must also be aware that some learners will expect the Nurse Educator to keep their word, meaning, if the Nurse Educator says “We will have class on Tuesday” some learners may expect to have a class on Tuesday. The learner may assume that class will be all day, or that they can arrive whenever they want. An example of clear communication in this case is the Nurse Educator stating:
“Class will be on Tuesday, will start at 8am, and there will be another class at 1pm. You must enroll in the course on our online learning center by the Friday before so we can get a head count for each class since space is limited.”
In this case, there is no room for confusion. Clear communication also limits the risk for learner frustration should they miss class due to unclear instructions from the Educator. Poor communication can lead to conflict. Conflict management is an important skill the Nurse Educator should possess.
Individuals have many methods of dealing with conflict:
- Avoidance – not dealing with the conflict by ignoring it.
- Accommodation – allowing the other individual to get what they want regardless of how you feel about the topic. Win/lose situation.
- Competitive – another form of win/lose resolution that does not create teamwork due to one individual or group fighting to get their way.
- Compromise – making adjustments to what they want on both sides of the conflict to create a resolution that all can agree on. Win/win solution.
- Collaboration – coming together as a group to create a solution to the problem through active listening, open mindedness, and respect.
Nurse Educators can encounter conflict from leadership above them or the learners they are responsible for. Reasons for conflict include conflicting personalities or individuals having different expectations on how a problem should be solved.
Those experiencing conflict should seek to resolve it. As mentioned earlier, there are many ways to come to a reasonable conclusion. Before going into the situation where conflict has occurred, Nurse Educators should ensure that reasonable limits are set for the conversation. These include all participants communicating respectfully, setting aside preconceived notions, engaging in active listening, and coming up with at least one solution with discussion of the positive and negative parts of each solution (7).
There are many books available to help with conflict management. Nurse Educators who may not feel confident in managing conflict should consider reading books or attending classes to help them develop these skills.
Evaluation
Determining if the education provided was successful depends on the learning objectives as well as how the Nurse Educator verifies success. An example is IV insertion. A Nurse Educator could determine training was successful by having learners do a post-test, but direct observation would be a better choice. Knowing how to insert an IV and being able to demonstrate the insertion are two different things.
World renown nurse author and leadership development expert, Donna Wright designed a model for competency assessment that lists 11 methods of verification that can be used throughout healthcare [See Table 7] (below).
|
Verification |
Definition |
Pros |
Cons |
Examples |
|
Test |
Used to measure cognitive skills and knowledge |
Great to measure comprehension of basic knowledge Answers the question “Is retention of information what we want to measure?” If the answer “yes,” then the test will work |
Does not reflect behavioral, psychomotor, performance skills
Must be aware of acceptable score and what is okay for testers to miss |
EKG rhythm recognition Understanding of legal holds when it comes to behavioral health patients Crossword puzzles
|
|
Return Demos |
The learner demonstrates a skill or set of skills in a simulated or real-world environment |
Can be done in simulation or in the real-world (only if patient safety is not affected) |
Must use a standard set of criteria or guidelines |
IV starting Cardiopulmonary resuscitation (CPR) Holding an individual who is violent |
|
Evidence of Daily Work |
The learners bring the evidence of their work to the educator (observing the finished product) |
Reduces some of the legwork the educator must do |
Those that are unable to perform the task may struggle without direction/guidance Those that procrastinate may have issues with completion without setting time limits |
Submitting an Excel spreadsheet showing the number of team members overdue on education Setting up a sterile field or other equipment |
|
Case Studies |
Discusses a scenario and the learner must explain their responses or reactions with a rationale |
Measures critical thinking skills Can be used in a group or individually
|
Not applicable |
“A patient presents to the emergency department with severe shortness of breath and chest pain. He says that he drove two hours to get there. What would be your priorities?” |
|
Exemplars |
A story that is told or written by the learner |
Used to measure interpersonal and critical thinking skills Can also assess actions not taken in a situation |
Usually does not focus on actual skills of the event
|
Charge nurse dealing with a problem or difficult team member New nurse calling a physician in the middle of the night
|
|
Peer Reviews |
Active support practice to enhance and acknowledge a team member’s actions |
Feedback is coming from peers as opposed to leadership
|
Some may be concerned about retaliation depending on feedback Does not measure all aspects of the job, only measures what can be observed |
Communication Documentation Patient care Inserting IVs |
|
Self-Assessments |
Team member’s evaluation of themselves |
Gives team members the opportunity to self-reflect on actions and behaviors |
Honesty or lack thereof
|
Coping with change Confidence with skill performance Confidence in managing particular patient populations |
|
Discussion Groups |
Written or verbal communication between team members to measure critical thinking skills |
Allows for others to have discussion and see other points of view |
If not managed appropriately, may be difficult to control the dynamics |
Debriefing after a code Mock event or disaster Hypothetical situation Analyzing a sentinel event |
|
Presentations |
Used to assess competencies that address knowledge and understanding |
Teaching a subject is a great way to deem competence with many skills in healthcare – “see one, do one, teach one” |
Attending a presentation does not classify as a competency. If so, another validation method paired with it would be most appropriate. |
Cardiac arrythmias Chest pain Psychosis Labor and delivery process
|
|
Mock Events |
Simulations of real-life events |
Shows team members how they would react in a real event, especially if it is an unannounced event |
May distract from real events if the event happens in the hospital or facility
|
Mock inspection for accrediting agencies Hazardous material cleanup Financial audits Pediatric patient abduction
|
|
Quality Monitors |
Used to monitor the environment and outcomes related to care or other actions |
Can be used to verify competency of an organization, facility, unit or individual – the data must be filtered down to appropriate information Can provide a variety of data points
|
Does not reflect everyone’s performance – additional verification may need to be completed
|
Hand hygiene Falls Stroke or cardiac alerts Callback time for on-call providers |
Table 7: Donna Wright Competency Assessment Model with Examples (21)
As noted in Table 7 above, not every evaluation and verification process have to be the same. Nurse Educators need to collaborate and determine the best method for the learners as well as themselves.

Self Quiz
Ask yourself...
- The list of evaluation/verification methods can be daunting, which methods have you seen used?
- Which ones did you like and dislike? Why?
- Are there any other methods that you have seen used to validate or evaluate education success in the nursing profession?
- Are there any methods that you prefer over others? What makes those appealing to you as a Nurse Educator (or future Nurse Educator)?
- Which methods do you think are harder to create? Which ones do you think take the most time? What about team member satisfaction?
Adjusting to Your New Role
Being a Nurse Educator is vastly different from bedside nursing. Roles and expectations change, and you are seen as a leader within your organization. Always be willing to learn and stay open to innovative ideas or suggestions. As the educator you must be a cheerleader for changes within the department and organization, even if everyone else is vocalizing frustration.
Tips for Aspiring or New Nurse Educators
Keep in mind that Table 8 (below) is not all-encompassing. However, some of the tips may inspire you during contemplation or jumping headfirst into the role.
|
Aspiring |
New |
|
|
Find ways to get involved with education at the facility or organization where you work. Some education departments allow bedside staff to assist with training or the Nurse Educator on your unit may have projects that you can help with. Being a superuser or go-to person for new procedures, processes, or equipment is a fantastic way to get involved in education. |
Find a mentor that’s willing to help you through the transition. This person should be someone who is willing to be your biggest advocate and critic. |
|
|
Expand your knowledge base. Nursing is a career of lifelong learning. Use this to your advantage, especially if you are interested in being an educator in a department that is different than your own. |
Work on obtaining a higher degree for your current job or a job you desire. Some individuals are content with a unit-based role, but others may want to become managers, directors, chairs, or deans within the education world. |
|
|
With the tip above, if you want to become an educator in a specialty area, consider transferring to that area if you do not work there already. |
Nurse Educators should multitask and be flexible. They are responsible for training many team members and educating them on many topics. Have a method of keeping everything on one calendar or a place where you can keep track of duties. |
|
|
Obtain specialty certification. This helps to boost your knowledge, confidence, and can be the factor that makes you the better candidate. |
Obtain the appropriate certification for your role. It sets you apart from others and can help you with your work and resume if you plan to advance in your field. |
|
|
If you are interested in becoming a Nurse Educator for nursing students, consider becoming a clinical instructor with your community college or university. Many nursing schools have limited instructors, leading to small numbers of nursing cohorts graduating. This can help you get experience in academia. |
Start where you can and work towards your goal. Not everyone will be given their dream educator job. Sometimes you will need to take other opportunities to get the experience and knowledge needed to eventually get the job you want. Don’t give up and continue to work towards your goal. |
|
|
Find unique opportunities outside of your institution to continue your education, expand your resume, and gain experience. You may not be able to teach Basic Life Support (BLS) at your facility, but can you work at another business that offers BLS courses. |
Find unique opportunities outside of your institution to continue your education, expand your resume, and gain experience. Writing continuing education courses, doing live or recorded webinars, or presenting at conferences can all help you gain experience and confidence. |
|
Table 8: Tips for Aspiring or New Nurse Educators
Continuing Education and Development Resources
- For Professional Development:
-
- Association for Nursing Professional Development: https://www.anpd.org/
-
- National League for Nursing: https://www.nln.org/
-
- International Nursing Association of Clinical and Simulation Learning: https://www.inacsl.org/
-
- American Nurses Association: https://www.nursingworld.org/
- Nursing Specialty Nursing Associations:
-
- Emergency Nurses Association: https://www.ena.org/
-
- American Association of Critical Care Nurses: https://www.aacn.org/
-
- The Academy of Medical-Surgical Nurses: https://amsn.org/
-
- The Association of Women’s Health, Obstetric and Neonatal Nurses: https://www.awhonn.org/
- Certification Boards:
-
- Board of Certification for Emergency Nursing: https://bcen.org
-
- Pediatric Nursing Certification Board: https://www.pncb.org/

Self Quiz
Ask yourself...
- What other ways could you improve yourself as a Nurse Educator or a future Nurse Educator?
- Are there any of the above suggestions/tips (Table 8) that you have considered? Which ones?
- Are there any that you will consider doing, especially if you desire to become a Nurse Educator in the future?
- Think of your education department. Is there anyone you would feel comfortable asking to mentor you in your Nurse Educator role or help you prepare for an opening? What are some ways you can approach them and ask them to be your mentor?
- Does your facility have any resources for Nurse Educators outside of the ones mentioned? Do you know how to access them?
Conclusion
From ensuring education compliance set forth by regulatory bodies is maintained, providing role guidance for their team, to training the next generation of nurses, Nurse Educators go above and beyond for the organizations that they serve. They give the learners the tools to succeed in patient care, making education as easy as possible for the team while managing dozens of tasks. They provide support to the team members from the day they start to the day they leave the organization, utilizing adult learning principles, various learning styles, and evidence-based research to do so. Nurse Educators are, without a doubt, a vital part of the nursing world.
References + Disclaimer
- Armstrong, P. (2010). Bloom’s taxonomy. Vanderbilt University Center for Teaching. https://cft.vanderbilt.edu/guides-sub-pages/blooms-taxonomy/
- Association for Nursing Professional Development. (2023). Role of practice in nursing professional development. In www.anpd.org. https://www.anpd.org/About/About-Us
- Bastable, S. B. (2020). Nuse as educator: Principles of teaching and learning for nursing practice. Jones & Bartlett Learning.
- Board of Certification for Emergency Nursing. (2023). Certifications exam statistics. BCEN. https://bcen.org/about-us/certification-exam-statistics/
- Dimock, M. (2019, January 17). Defining generations: Where millennials end and generation Z begins. Pew Research Center. https://www.pewresearch.org/short-reads/2019/01/17/where-millennials-end-and-generation-z-begins/
- Eisner, P. J. (2023, September 8). LibGuides: Evidence-Based practice research in nursing: Finding EBP articles in the databases. Libguides.adelphi.edu. https://libguides.adelphi.edu/c.php?g=1129354&p=8242231
- Gossman, W., Ellis, V. L., & Toney-Butler, T. J. (2022). Conflict management. Nih.gov; StatPearls Publishing. https://www.ncbi.nlm.nih.gov/books/NBK470432/
- Harper, M. G., & Maloney, P. (Eds.). (2022). Nursing professional development : Scope and standards of practice (4th ed.). Association for Nursing Professional Development.
- Langille, J. J., & Brown, R. E. (2018). The synaptic theory of memory: A historical survey and reconciliation of recent opposition. Frontiers in Systems Neuroscience, 12(52). https://doi.org/10.3389/fnsys.2018.00052
- McLeod, S. (2023, July 25). Albert Bandura’s social learning theory. Simply Psychology. https://www.simplypsychology.org/bandura.html
- Montgomery College. (n.d.). Teaching multiple generations. https://www.montgomerycollege.edu/_documents/offices/elite/teaching-multiple-generations.pdf
- Nienaber, A., Sigma Theta Tau International, Longo, A., & Jeffery, A. D. (2016). Staff educator’s guide to professional development: Assessing and enhancing nurse competency. Sigma Theta Tau International.
- Petiprin, A. (2019). Benner’s from novice to expert – nursing theory. Nursing Theory. https://nursing-theory.org/theories-and-models/from-novice-to-expert.php
- Rehman, I., Mahabadi, N., & Rehman, C. I. (2022, August 22). Classical conditioning. Nih.gov; StatPearls Publishing. https://www.ncbi.nlm.nih.gov/books/NBK470326/
- Szymkowiak, A., Melović, B., Dabić, M., Jeganathan, K., & Kundi, G. S. (2021). Information technology and Gen Z: The role of teachers, the internet, and technology in the education of young people. Technology in Society, 65(65). https://doi.org/10.1016/j.techsoc.2021.101565
- The Myers-Briggs Company. (2017). Myers-Briggs Type Indicator® (MBTI®) | Official Myers Briggs Personality Test. Themyersbriggs.com. https://www.themyersbriggs.com/en-US/Products-and-Services/Myers-Briggs
- United Nations Institute for Training and Research. (2012, July 23). Learning Styles: Dunn and Dunn Model – Learning and training wiki. Learningwiki.unitar.org. https://learningwiki.unitar.org/index.php/Learning_Styles:_Dunn_and_Dunn_Model
- VARK. (2020). VARK – A guide to learning preferences. VARK – a Guide to Learning Preferences. https://vark-learn.com/
- Whitman, L. (2012). Myers-Briggs Types. In Research Gate. https://www.researchgate.net/figure/The-16-Myers-Briggs-Types-with-their-equivalent-Keirsey-Descriptions_tbl2_229429287
- Worcester State University. (2022, August 17). Top communication skills for nurse educators. Worcester. https://online.worcester.edu/programs/msn-educator/communication-skills-for-nurse-educators/
- Wright, D. (2021). The ultimate guide to competency assessment in healthcare (4th ed.). Creative Health Care Management.
Disclaimer:
Use of Course Content. The courses provided by NCC are based on industry knowledge and input from professional nurses, experts, practitioners, and other individuals and institutions. The information presented in this course is intended solely for the use of healthcare professionals taking this course, for credit, from NCC. The information is designed to assist healthcare professionals, including nurses, in addressing issues associated with healthcare. The information provided in this course is general in nature and is not designed to address any specific situation. This publication in no way absolves facilities of their responsibility for the appropriate orientation of healthcare professionals. Hospitals or other organizations using this publication as a part of their own orientation processes should review the contents of this publication to ensure accuracy and compliance before using this publication. Knowledge, procedures or insight gained from the Student in the course of taking classes provided by NCC may be used at the Student’s discretion during their course of work or otherwise in a professional capacity. The Student understands and agrees that NCC shall not be held liable for any acts, errors, advice or omissions provided by the Student based on knowledge or advice acquired by NCC. The Student is solely responsible for his/her own actions, even if information and/or education was acquired from a NCC course pertaining to that action or actions. By clicking “complete” you are agreeing to these terms of use.
➁ Complete Survey
Give us your thoughts and feedback
➂ Click the Green MARK COMPLETE Button Below
To receive your certificate
