Course
West Virginia RN Renewal Bundle
Course Highlights
- In this West Virginia RN Renewal Bundle course, we will learn about best practices for managing patients who display drug seeking behaviors and diversion.
- You’ll also learn how to implement patient education taking into consideration different learning styles and individual preferences.
- You’ll leave this course with a broader understanding of how to identify and analyze quality improvement opportunities.
About
Contact Hours Awarded: 12
Course By:
Various Authors
Begin Now
Read Course | Complete Survey | Claim Credit
➀ Read and Learn
The following course content
Patient Education Strategies
Introduction
As nurses, we wear many hats and take on numerous roles in our careers. The main part of our job is to educate our patients.
Have you ever walked into your patient’s room after the physician leaves, and are bombarded with questions from your patient? They are confused and scared, and this is when you come in.
Patient education is important in every type of nursing: inpatient, outpatient, acute care, long-term care, adults, or pediatrics. No matter the specialty of nursing, at some point in time you must educate your patients and their families.
This course’s goal is to provide resources to improve education for your patients, give strategies to prevent barriers to education and evaluate the effectiveness of the education we provide.
Definition- Patient Education
What does patient education mean exactly?
Education is knowledge that results from the process of being educated [10]. No matter what type of nursing you are in, you are constantly giving patients instruction on a topic.
Whether it is regarding medications, diagnostic testing, or diagnoses we are the patient’s main point of contact. A physician or provider is with a patient for a short amount of time, and it is our job to explain the information that was given to them.
Currently, there is information everywhere. We are almost overloaded with information. With the use of smartphones, we can search for almost anything.
Our patients, for the most part, want to feel in control of their health, and this can come in the form of knowledge. As soon as they hear something, they want to search for information on the subject.
This should not substitute our teaching. A lot of the information published may not be accurate or not pertain to their situation. We must be aware of this and make sure we are providing our patients with resources so they can find accurate information [2].
Who are we educating?
The Healthcare Education Association has shared guidelines on patient education [8]. In some instances, we are educating family members, caregivers, friends, and sometimes an entire family [8].
You might be caring for an elderly patient in an acute care setting and will be discharging this patient home to their adult child. They will now be the caregivers and they will require education. Or you are caring for a five-year-old, just diagnosed with type I diabetes in which multiple members of the family will need to be educated on carbohydrate counting and insulin administration.
During this course, the term patient education may be used but it is meant to encompass anyone that we are providing teaching to.
Importance
At the end of the day, patient safety is our main goal. Patient education is a vital way to promote patient safety.
After a new medication is prescribed, we must educate the patient on why they need to take this medication, how to take the medication appropriately, and the side effects of the medication. Our education can also push the importance of lifestyle changes after a diagnosis.
It is easy to go through the motions of your job and forget why we became nurses. Our patients need their healthcare team to take the time to explain the importance of their treatment plan. Education helps patients be the center of their healthcare [12].
What is health literacy?
Health literacy is described as the knowledge of health information and the ability to understand and find resources related to health information, to make decisions for their healthcare based on this information [1].
This definition was changed in 2020 [1]. The change included being able to use health information and apply it to their life, not just having the ability to understand the information. This new definition also states that organizations need to include health literacy in their mission statement [1].
A study conducted by the National Assessment of Adult Literacy showed that only 12% of adult Americans have the appropriate health literacy to understand their care and make informed decisions [7]. With the average population, there is an extreme deficit of the ability to have the information to make autonomous decisions for their healthcare.
How does health literacy play a role in education?
With understanding what health literacy means, we want to give our patients the most accurate information, so they can make the most informed decisions about their healthcare. As nurses, we should be aware of our patients’ health literacy and want them to have the highest level of information available.
Our goal should be that the patient understands and utilizes the information provided in their healthcare choices. Studies have shown that there is a correlation between low education and poor health status [4].

Self Quiz
Ask yourself...
- How can nurses determine their patient’s health literacy?
- Can patient education cut healthcare spending costs?
- Who is responsible for funding patient education?
Role of Nursing
Whose role is it to provide patient education?
Sometimes education can be thought to fall under the physician’s scope of practice. However, every member of the healthcare team can play a part in educating our patients [8].
As said earlier, nurses usually spend the bulk of their time with patients. It is our duty to reinforce and expand upon the teaching provided by other members of the healthcare team. We also must collaborate with other members of the healthcare team to not leave gaps in the education that is provided [12].
Opportunities for Teaching
How should education be prioritized?
In nursing, we are expected to perform a variety of tasks. It can get overwhelming at times trying to prioritize and complete each task. Adding any other task to that list can be daunting.
Education should be incorporated into our work to place patient safety as the goal. Education should be prioritized over other tasks [13]. Many factors such as time and adequate staffing can result in insufficient education [13]. Simple tasks should be delegated if possible, so that you can focus on educating your patients.
Learning Styles
What are the main learning styles?
- Visual- A visual learner requires seeing what they are learning right in front of them [9]. They benefit from graphs and examples for them to look at. Not only going over the education but also providing them with a copy of the teaching is useful.
- Auditory- An auditory learner thrives on hearing the information [9]. This type of learner would not benefit from just receiving a pamphlet.
- Reading- This example of a learning style would be providing material for the learner to read on their own [9].
- Kinesthetic- This type of learner would be described as a “hands-on” learner [9]. This learner would benefit by tangibly holding material. When providing education about
changing an ostomy bag and giving them an ostomy bag to hold would be useful during the teaching.

How do we as nurses identify a patient’s learning style?
A barrier to education can be that we sometimes treat each patient the same. We build standardized educational pamphlets to provide to our patients, teach group classes, and provide similar, if not identical, resources.
While this can be helpful and save time, it can also be a barrier. Not all people learn the same way. Completing a learning assessment for each patient could help identify their preferred learning style to in turn make the teaching more effective [8].
How can we use learning styles in our teaching?
Each person may not be a single type of learner and may be responsive to a variety of learning styles. Prior to providing the actual education, it is important to determine which learning style the patient would be most receptive to.
Also factoring the subject matter into which style you use can be beneficial in teaching [9]. If you need to educate on how to change a dressing on a wound, a demonstration would be appropriate.
If you need to educate on dietary modifications for a low-cholesterol diet, a handout that can be referenced makes sense. The subject matter should be considered when determining which type of learning style should be used.
Case Study:
A patient is being discharged home with a diagnosis of asthma and a new prescription for an albuterol MDI as needed for wheezing. You are the nurse providing discharge teaching.
Prior to providing education you ask if the patient has a preferred learning style. The patient states they are a hands-on learner and are receptive to reading material.
When providing the teaching you give them a spacer with the inhaler to hold and demonstrate how to attach them together. You demonstrate how to administer the ordered number of puffs. You review and provide them with a printout of triggers that could exacerbate their asthma.

Self Quiz
Ask yourself...
- Can multiple learning styles be utilized in your patient’s education?
- Does age play a role in learning styles?
- Can the patient’s education level be a factor in their learning style?
- What if the patient does not have a preferred learning style?
Teaching Strategies
What to include in your education plan?
Before beginning your education with the patient or family member you must set a plan. In your plan, you should include realistic information [2]. Stick to the need to know and not all the information you would like your patient to know [2].
Information overload can be a barrier to helping the patient understand what you are teaching them. In some specialties, nurses have multiple interactions with their patients, where they can build a rapport with them [12].
Use this to your advantage. It might take several visits with your patients to help them understand a certain topic. While other specialties such as acute care, the emergency department, or outpatient surgery centers need to provide concise information and additional resources so the patient can review the information at a later time [2].
Set an attainable goal for yourself and your patient. If you have a short amount of time, it is not realistic to expect to educate on an entire topic such as COPD and expect the patient to verbalize understanding. With specific attainable goals, this will help in your planning and execution of the teaching.
What to ask patients at the beginning of the teaching?
At the start of your teaching, it is crucial to ask the patient about their concerns [8]. A patient might be more receptive to the education if they feel like they are heard. Patient education should be patient-centered, which means focusing on their needs [8].
This can be useful information so you can include what they are most concerned about in the teaching. The patient will then feel valued and will be open to learning.
How does a learner’s demographic become a factor in their understanding of information?
A review was conducted regarding older adults and their preferred style of information [3]. This review concluded that older adults benefit more from written articles presented by healthcare professionals and were not as receptive to group classes, online apps, or videos [3].
Statistics from the CDC states that by 2030, 71.5 million people will be over the age of 65 living in the United States [6]. Which means, in order for them to lead healthy lives, it is our responsibility as healthcare workers to play our part in providing accurate information for them to implement in their lives [6].
On the other end of the spectrum, you might be educating a patient on the other end of the spectrum, a child. Pediatric nursing requires lots of education for the families and the patients themselves.
Children can learn and understand topics when they are presented with developmentally appropriate material. With pediatric patients props and hands-on learning can be beneficial. Age should be considered when planning education materials for patients or their families.
Language can also be a barrier to communication. It is important to ask a patient their preferred language for healthcare information. A patient may speak English however they might be more comfortable in their first language if it is something other than language.
Prior to teaching, a learning assessment is beneficial for you and the patient [8]. Asking the learner their preferred language should take place first.
A patient’s culture can also impact their learning abilities [5][8]. As health care providers we must not shy away from cultural differences but rather incorporate this in our practice [8]. The information we provide should be standardized with our patients, however the way we communicate can vary.


Self Quiz
Ask yourself...
- How can your own culture become a barrier to patient communication?
- What is the best way to ask about a patient’s culture?
- When providing education to a patient who speaks a different language than your own, can information be lost when utilizing an interpreter?
When is the appropriate time to educate your patient?
The patient may be in the middle of a life-changing event or managing a chronic disease and they may have a hard time focusing. When planning to educate a patient it is important to factor in the time of the education.
Did the patient just get out of surgery? Was the patient up all night? Involving the patient in the education will help the patient be more receptive and give them some control [2].
If the patient is being discharged and requires education set a time with them to go over the information. This can prevent barriers that might occur.
How can technology influence education?
In this day in age, technology has influenced all aspects of our lives. Technology can be incorporated into our education as well [2]. Many hospitals are using programs on patient televisions to provide education.
When planning to teach our patients we should explore these methods to help the patient and ourselves as the educator. Some videos can be used that explain procedures, skills, and medications to our patients [8]. It is also important to know our patients and see how receptive they are to this means of education.
An elderly patient may not be interested in a link for more education regarding dietary changes [3]. A person in their 30s may like education they can look at on their computer at home.

Self Quiz
Ask yourself...
- When is providing a patient with a video for teaching appropriate?
- Can technology inhibit a patient from understanding the education provided?
Evaluating Effectiveness
What does it mean to evaluate your teaching?
Teaching is not complete until it is evaluated. As healthcare professionals, we must gauge if our teaching was understood or if further teaching is indicated [8].
If further teaching is needed, it does not mean we failed at our job. It means that we have our patient’s best interest, and we want them to succeed and need to change our education to fit their needs.
Studies in the past have shown that 40-80% of medical teaching done at an outpatient visit was not remembered by the patient and almost half of the information that was retained was not accurate [11].
What are some strategies to evaluate the patient’s understanding of the education provided?
- Demonstration- Often nurses must teach a patient to perform a skill, for example, check blood pressure with a blood pressure cuff, perform a blood glucose check, and administer a subcutaneous injection.
In this type of instruction, the nurse should begin by stating the objective to the patient, which is the skill that needs to be performed, and explain that the patient should return to demonstrate that skill to the nurse [8]. By stating this at the beginning, the patient will know they need to perform the skill at the end of teaching and not be caught off guard. This is also a way to evaluate the teaching [8].
When the patient returns and demonstrates this skill, the nurse can discuss ways they can improve the skill [8].
- Teach-back method- This is a strategy that includes teaching and then allows the learner/patient to demonstrate what they learned back to you [11].
This is an example of how to evaluate the level of the patient’s understanding [11]. Giving the patient time to verbalize what you are educating is a measurable way to evaluate the education that was provided.
A strategy to use the teach-back method is to teach in sections and then allow the patient to state in their own words what they learned in that section [11]. This helps break up the teaching and allows the patient to process the information [11].
Case Study
You are set to discharge a patient home that was hospitalized due to anaphylactic shock from a food allergy. They are overwhelmed by the amount of information they are receiving.
They are prescribed an Epi-pen in case of future reactions. To implement the teach-back method you can use a training Epi-pen to demonstrate how it works.
Then give the practice Epi-pen to the patient so they can hold the Epi-pen and apply the Epi-pen to themselves. Now the patient can feel more comfortable after practice, and you can evaluate if the teaching was understood.

Self Quiz
Ask yourself...
- How can nurses use the return demonstration method in their practice?
- Is the return demonstration method appropriate for every patient?
- What are the next steps if a patient does not accurately demonstrate the skill you were teaching?
Case Study
A patient is diagnosed with hypertension and high cholesterol. As the nurse at an outpatient clinic, you are responsible for going over some lifestyle changes with the patient. You have listed some changes they should make in their diet.
In the middle of the teaching, you ask, “What are 3 dietary modifications you can implement into your daily life?” This helps the patient process the information and turn it into their own words.

Self Quiz
Ask yourself...
- How can nurses use the teach-back method in their practice?
- What settings can the teach-back method be useful in?
When to allow questions during teaching?
Sometimes it might feel easier for us to instruct the learner to save their questions till the end of the instruction. However, allowing the learner to ask questions throughout the education can help prevent information overload and be helpful for you to evaluate your teaching [8].
Questions can allow you to tailor your education to focus on areas that the patient might need more information on [8]. The patient can emphasize their concerns by asking to hear more information on a certain aspect of what you have taught.
When preparing for education make sure that you insert breaks so the patient or family member can ask questions. This will help with their learning and can help you determine the effectiveness.

Self Quiz
Ask yourself...
- What are signs that the patient is not understanding our education?
- If our patient is not grasping the teaching, does it mean our educational techniques fail?
- What is the next step if the patient does not understand our teaching?
Conclusion
To summarize the content of this course: Patient education should be specific, concise, tailored to your patient’s needs, and measurable.
You should present your patients with objectives at the beginning of your education so they will know what to expect to understand by the end of the teaching. Address any questions that the patient might have and allow the patient to provide you with feedback.
By providing intentional patient-centered education we can give our patients the tools they need to make informed decisions about their healthcare.
Nurse Burnout
Introduction
In May 2022, during Mental Health Awareness Month, the United States Surgeon General Dr. Vivek Murthy issued a new Surgeon General’s Advisory highlighting the urgent need to address the health worker burnout crisis nationwide. Citing existing challenges in the healthcare system and the long-term effects of the coronavirus pandemic, Dr. Murthy prioritized our healthcare workers' mental health to strengthen our nation’s public health infrastructure.
This report stated that “…. up to 54% of nurses and physicians, and up to 60% of medical students and residents, suffering from burnout”. Symptoms of burnout have indeed impacted the current workplace, and ongoing employee mental and physical exhaustion results in a vulnerable, compromised workforce (2).
The lingering effects of post-pandemic burnout have affected every element of our current healthcare system. Healthcare professionals are leaving the profession at an alarming rate (due to illness and scheduled retirement), which translates to increasing shortages of providers. Coupled with additional vacancies due to ongoing mental health conditions (depression, anxiety, post-traumatic stress disorder), our healthcare system is experiencing significant gaps in its ability to provide quality care across the healthcare spectrum.
While the legislature addresses healthcare burnout on a larger scale, nurse professionals owe it to themselves to recognize the signs and symptoms of nurse burnout and take appropriate action to protect themselves, their families, colleagues, and patients.

Self Quiz
Ask yourself...
- Why do you think the coronavirus pandemic caused such large numbers of healthcare worker burnout?
- How do you think the coronavirus pandemic affected your place of employment?
- What difference did the pandemic make in your specific job responsibilities?
Nurse Burnout vs. Compassion Fatigue
Although the terms “nurse burnout” and “compassion fatigue” are often used interchangeably, they do refer to two separate conditions (4). Nurse burnout is the term used to describe emotional and physical exhaustion related to ongoing stressful working environments and associated responsibilities. Burnout has a gradual onset and usually occurs in behaviors such as decreased workplace productivity and persistent feelings of hopelessness, helplessness, and overwhelming exhaustion.
Compassion fatigue, on the other hand, often emerges from some prolonged emotional stress or strain. It may occur after exposure to a traumatized individual more so than a workplace trauma. Signs and symptoms of compassion fatigue may manifest in such behaviors as anger, irritability, increased anxiety, and physical exhaustion. In comparing burnout to compassion fatigue, burnout appears to gradually rise to the surface, while compassion fatigue occurs more suddenly (5).

Self Quiz
Ask yourself...
- Regarding compassion fatigue, what situations could make a healthcare professional “angry, irritable, and exhausted” while on duty?
- Regarding nurse burnout, what situations could make a healthcare professional feel “hopeless and helpless” while on duty?
Life As a Nurse
An average day in the life of a nurse will include varying degrees of stress and long work hours. Both factors are known to affect one’s mental health, yet it is considered “a normal day’s work” when describing a day in the life of a nurse.
In any workplace setting, a nurse's role includes a very demanding set of acceptable stressors (“part of the job”). Upon completing a highly stressful workday, nurses may head home to face additional demands on their time and energy levels (child/elder care, various household responsibilities, and community and church obligations, to name a few). This routine leaves little time for rest and recovery, both mind and body.
All those demands on their time and attention can lead to compassion fatigue. The pandemic is a convincing example of both nurse burnout and compassion fatigue. Nursing professionals were repeatedly exposed to critically ill patients, many of whom did not survive. Staffing patterns were suboptimal, critical care beds and equipment were sorely lacking in some areas, and the daily stressors felt during a single shift seemed to repeat themselves. There was no quality “downtime” for nurses to take a well-deserved break, much less debriefing and regrouping/refocus efforts.
This pandemic, a universal “once in a lifetime” event by any standard, affected everyone at some level. Nurse professionals were witnessing traumatic losses of life every day. Compassion fatigue, understandably so, began to surface. The healthcare community experienced anger, irritability, and increasing levels of anxiety. They took to the news media, voicing feelings of isolation, despair, anger, and devastation. They publicly spoke of sleep difficulties, increased workloads, and lack of appropriate lifesaving supplies, thus becoming more exhausted and cynical with each passing shift. When the pandemic crisis finally came under control, the landscape of nursing looked quite different (6).
Nurses had resigned, transferred, or walked off their shifts. Early retirements and medical leaves of absence were increasing in number. Enrollments in nursing schools were down. The healthcare arena continues to suffer years later, looking for solutions to “heal thyself.”
So, the question remains…. What can we do to reduce the risk of nurse burnout moving forward?

Self Quiz
Ask yourself...
- How would you describe your current workplace?
- Do you feel appreciated for your efforts while at work?
- What is one “major stressor” you wish to change at your workplace?
Burnout Risk Factors
While no single factor causes nurse burnout, there are undoubtedly identifiable risk factors and patterns that heighten the risk. Early identification and intervention of such risk factors lower the chances of nurse professionals suffering personally and professionally.
Increased workloads (due to staff call-ins, lack of patient care equipment, and lack of ancillary help) are a leading causative factor in nurse burnout. In addition, lack of support from senior leadership, unit managers, worksite colleagues, and other members of the organizational healthcare team impacts feelings of helplessness and hopelessness.
Again, there is no single factor to point blame at, but there are often patterns of behavior that warrant further investigation at the workplace. In addition, nurse burnout is very individualized. What is harmful and hurtful to one nurse may not be seen as such to another nurse.
The goal is to make the workplace environment supportive for all employees by creating (and nurturing) a culture that welcomes nursing input. By recognizing the bigger picture of individual and organizational safety, the nurse in crisis feels safe in stepping forward and seeking professional help in a supportive environment.
While nurse burnout can occur in any area of nursing, from hospitals to clinics to home health settings and beyond, some areas are at higher risk for burnout. Nursing professionals in the intensive care and emergency care units are at higher risk for symptoms of burnout.
Studies have shown that many specialty nurses experience anxiety, increasing exhaustion, and mounting frustration while on duty. Combined with a patient population often experiencing high rates of trauma-related mortality and complex illnesses, it is understandable that “typical workdays” may be filled with extremely high levels of workplace stress.

Self Quiz
Ask yourself...
- Think about your current workplace. Are there any factors that could contribute to burnout?
- Have you witnessed anyone in your workplace display signs of being “burned” out?
Causes of Burnout
An article published in the Journal of the American Medical Association identified some causes that directly impact nurse burnout (7). The authors found that nurses who routinely worked longer shifts (extra shifts, mandated overtime shifts) and experienced sleep deprivation exhibited symptoms of burnout. The combination of excessive work hours and inadequate sleep (as often occurred with shortened turnaround times and back-to-back shifts) resulted in increased patient care errors. These occurrences often compounded the feelings of helplessness and hopelessness (8).

Self Quiz
Ask yourself...
- Have you ever picked up extra shifts only to regret it afterward?
- How did you feel after working those extra shifts?
Impact on (Individual) Health
In the early stages of burnout, the nurse professional may feel overworked, underappreciated, and physically tired. While such symptoms may appear benign when occurring sporadically and “chalked up” to “just having a bad day,” repeated shifts like this may manifest into a more profound feeling of despair.
It soon becomes challenging to continue working under such circumstances, further escalating the situation. To distance oneself from these feelings, the nurse professional may become cynical and jaded about their workplace, mentally distancing themselves from colleagues. These efforts only serve to isolate the individual further and exacerbate feelings of hopelessness and isolation while negatively impacting workplace efficacy (9).
Impact on Workplace/Organization Health
The stressed out, overworked, and exhausted nurse professional may unknowingly / unintentionally compromise the quality of care. Feelings of helplessness and hopelessness can negatively affect the nurse’s judgment and critical thinking skills. Critical steps/tasks may be skipped when the nurse is tired and overworked.
Nurse burnout negatively impacts job satisfaction and, in doing so, also negatively impacts patient care. The effect will be poor patient care, increased patient and family complaints, and poorer patient outcomes. Nurse burnout affects not only the individual but the organization. (10)

Self Quiz
Ask yourself...
- How does a nurse unintentionally compromise the care being delivered to a patient?
- How do you think being sleep-deprived could affect your abilities while on duty?
Self-Care Strategies
“I have come to believe that caring for myself is not self-indulgent. Caring for myself is an act of survival.”
— Audre Lorde (3).
What is self-care? (12)
In the most basic definition, self-care refers to doing things that will improve your physical and mental health. It is very subjective, and self-care strategies must focus on your needs, wants, and desires. As stated, nurse burnout is very individualized: what profoundly affects one nurse may not even bother the next nurse.
The strategies discussed here are generic; they must be personalized to fit your specific needs and healing process.
- A good night’s sleep: Limit caffeine intake before bedtime, no electronics 1-2 hours before sleep, lower room temperature to facilitate comfortable sleep, and blackout curtains.
- Physical activity: Light-impact activities such as swimming, yoga, walking, bike riding, and other activities will be physically and mentally beneficial.
- Diet: Maintain a balanced diet. Monitor hydration levels and limit caffeine products. The goal is to nourish your body to offset the adverse effects of stress. Cut down on processed food intake and “junk foods.”
- Mental health: Journaling, podcasts, music, and joyful hobbies and activities (knitting, crafts, painting).
- Homefront Maintenance: Calm surroundings foster the healing process. Keep the environment clean, uncluttered, and welcoming. Empty the sinks and dishwashers, fold the laundry, and make your bed. Aromatherapy, lighted candles, and essential oils are all ways to make your home a place to rest and relax.
The list of “self-care “strategies is endless. Be sure to find an appropriate diet, activity, and behaviors that enable you to focus on building a balanced lifestyle.


Self Quiz
Ask yourself...
- What are some self-care strategies that have worked in your personal life?
- How could you encourage a nursing colleague to “take better care of themselves” through self-care practices?
Organizational Strategies
Healthcare organizations must provide structured support for their nurse professionals to ensure quality patient care. Facility-wide strategies work best to identify and treat nurse stress and burnout early.
- Nursing rounds- routinely meet with nursing staff and listen to their feedback. Ask the difficult questions (staffing patterns, scheduling issues) and be receptive to working on viable solutions.
- Support staff in utilizing earned days off, vacation time/ paid time off.
- Open lines of communication with staff experiencing signs of nurse burnout or compassion fatigue. Offer alternate job duties and work assignments if possible.
- Acknowledge employee organizational loyalty (through retention bonuses, additional days off, gift cards, personalized thank-you letters, and personal development endeavors).
- Encourage critical debriefings for staff members involved in essential/traumatic patient care encounters.
- Openly promote facility resources available to staff, including all Employee Assistance Programs.

Self Quiz
Ask yourself...
- How do you feel your healthcare organization could improve the current workplace?
- What are some employee assistance programs currently offered at your workplace?
- What incentives/ acknowledgments from your nurse leaders would most benefit staff morale?
Case study
Marie is a 35-year-old Registered Nurse working full-time on a 16-bed ICU unit. She has been employed here for three years, beginning her employment at the start of the coronavirus pandemic. Marie works 12-hour shifts (7p-7a) with every other weekend off. Two of Marie’s nurses' coworkers recently resigned, leaving the unit chronically short-staffed.
Marie has been working additional shifts to help her coworkers and has just completed a 50-hour work week. She was once again called into work early and arrived on only 4 hours of sleep the night before. The unit is at total capacity with 2 “ICU holds” in the Emergency Department. Marie has fallen behind on her patient care while intercepting repeated calls from the ED staff.
Marie spent a long overdue break crying in the nurse's lounge. She confided to another staff member (Anne) that she is exhausted and overwhelmed by these work conditions and is considering resigning. Anne told Marie to take a few more minutes for her break and promised to discuss the situation with their charge nurse, Carol. Marie agreed.
Anne discussed the situation with Carol, stating Marie is a great nurse who has been working too many shifts lately. Anne offered to pick up some of Marie’s current patient assignments to lower Marie’s stress level, hopefully. Carol approved and also took some of Marie’s patients. Marie finished her break, apologized to her coworkers for her “moment of weakness,” and promised, “it wouldn’t happen again.”

Self Quiz
Ask yourself...
- What factors did you identify that put Marie at risk for nurse burnout?
- If Marie confided in you, as a colleague, that she was exhausted and overwhelmed, how would you respond?
- Marie apologized for her “moment of weakness” and promised “it wouldn’t happen again.” How would you respond to this employee if you oversaw this shift?
- What resources are available at your current workplace for employees who acknowledge they are “exhausted and stressed out”?
- If you were the Nurse Manager of this ICU, what would you do to support your staff during this time (* significant staffing shortages due to recent resignations)?
Resources
The following links are provided for additional information on nurse burnout surveys.
Conclusion
The healthcare workforce continues to be challenged by large numbers of scheduled retirements, an aging population, and medically complex patients. Nurse leaders must proactively hire and retain a healthy workforce (13). Healthcare organizations must invest in a workplace culture that supports workers' work/life balance. It is the key to ensuring the health and safety of our nation.
Bullying in Nursing
Introduction
In a time when bullying has become one of the most frowned upon behaviors, why is it thriving in the world of nursing? We’ve all heard the saying that “nurses eat their young”. It is a term that has been passed down the nursing ranks as each generation of nurses enters the workplace; unchanged and still true. We, as nurses, cannot permit such unhealthy and detrimental behavior to continue. In this course, we will discuss nurse bullying, why it happens and what we can do to break the curse.
Definitions
To fully understand nurse bullying and the issues that come with it, we must define some terms and phrases so that we are all on the same page.
Nurse Bully
A nurse bully is someone who repeatedly harasses and/or harms other nurses whom they believe they can dominate; they may also see them as less skilled or incompetent (5).
Incivility
Incivility is a type of lower-level bullying that entails more passive types of behavior. This is your mocking, gossiping, alienation, and general rudeness. The difference between incivility and actual bullying is that incivility may not actually harm the victim (6).
Harassment
Harassment is when someone torments or intimidates another person (4).


Self Quiz
Ask yourself...
- What is the difference between incivility and bullying?
- Who is the victim of the nurse bully?
Incidence Rate
The nursing profession has historically been known as the most trusted profession. Nursing is also synonymous with caring and compassion. From the outside looking in, it may be difficult to believe that bullying could exist in such a respected and revered profession. The prevalence of bullying in nursing is staggering. Both new and seasoned nurses; young and old; nurses of every gender; and nurses of every walk of life report that they have been bullied on the job. These instances represent a wide variety of bullying behaviors which include verbal abuse, threatening, scapegoating, sabotage, and physical abuse (5).
Incidence rates of bullying in nursing, as documented in a variety of studies, ranging from 17-85%. This includes incidents of verbal abuse, threatening, belittling, and even physical abuse. With the prevalence of bullying so high among nurses, it is safe to say that virtually every nurse has been touched by bullying, whether victim, perpetrator, or observer (5).

Self Quiz
Ask yourself...
- Does the incident rate of nurse bullying surprise you?
- Have you ever witnessed or been involved in an incident of nurse bullying?
Why Does It Occur?
What drives bullying behaviors? What makes a bully? There are a myriad of factors that come into play when discussing why bullying occurs.
Anger and frustration are two strong emotions that can contribute to bullying behaviors. In today’s nursing work environment, anger and frustration are at the forefront of many nursing units. Nursing shortages have left many units understaffed and the nurses overworked. This frustration leads to anger when the nurses who have remained loyal, full-time staff see travelers come into their areas making higher pay. Lack of resources and the belief that they are unheard of also contribute to feelings of frustration (5).
The belief that another nurse is less competent or altogether incompetent can also lead to bullying. When it is perceived that another nurse can’t do their job and therefore may leave tasks for the oncoming shift, the above-mentioned frustration sets in and bullying may result. Just the feeling of superiority over another nurse can have bullying effects on the nursing environment (1).

Self Quiz
Ask yourself...
- Is there a key risk factor that promotes an environment of nurse bullying?
- Are nurse bullying risk factors real or perceived? Explain.
Risk Factors
There are some circumstances that contribute to the bullying climate. These are not excuses that give permission to the bullies, rather they are risk factors that have been identified as possible catalysts to bullying behaviors.
Seniority
Some nurses may feel that they have “paid their dues” and should have authority over their less-experienced peers. If this authority is not granted, the senior nurse may harbor feelings of underappreciation and lash out by being unhelpful or, to the extreme, harmful. The aim is to show how much this nurse is needed; they will refrain from helping the newer nurse or giving any advice (5).
Insecurity
When new nurses come into the workplace, the existing nurses may feel that they will be replaced. Nursing is an ever-evolving occupation with new technologies and treatments being developed all the time. A new nurse who was taught the most up-to-date trends in nursing may pose a threat to their job. This is when the nurse may start to bully the new nurse joining the team (1).
Protection
Some nurses become very attached to their patients. They may feel that no one else can give the same level of care that they can. As a result, they may see other nurses as incapable of providing care that is up to their standards. Only they can provide the care that their patients require. These perceived inadequacies can quickly turn into bullying behaviors (1).
Education
Differences in levels of education may also contribute to bullying. Nursing has many different levels of education and nurses from all these levels may work together on a single unit. Nurses with higher levels of education may feel superior and lash out at those with less education. RNs may treat LVNs differently than their RN peers (3).

Self Quiz
Ask yourself...
- Name 2 risk factors that contribute to nurse bullying.
- Have these risk factors led to a nurse bullying environment in your organization?
- Does one risk factor stand out to you as a prime contributor to nurse bullying?
- Which one?
Types of Bullying
It is important to note that not every bullying-type behavior can be construed as actual bullying. We all have bad days when things just don’t seem to be going right and we may react inappropriately. One of the key factors that differentiates bullying from a lapse in judgment is that bullying is a repeated or habitual behavior.
This does not excuse the one-time behavior however, we must realize that not all poor behaviors are bullying. Nurse bullying may manifest itself in a variety of different behaviors. Below, we will discuss a few of these types of bullying. This is by no means an exhaustive list of all possible bullying behaviors; they are some of the behaviors that you may commonly see in the healthcare environment (5).
Verbal abuse
This may include being rude, belittling, criticizing, and threatening. We’ve all heard “sticks and stones may break my bones, but words will never hurt me”. This is a false saying as constant verbal abuse plays with our psyche as we rerun the taunts in our heads over and over. If heard enough, we may start to believe the bully’s words.
Controlling
Constantly telling another nurse what to do and how to do it. This is unsolicited advice that if not taken may escalate bullying behaviors. Controlling behaviors may also include certain “looks” and intimidating posturing.
Ignoring/excluding
Ignoring requests for help. Ignoring any suggestions to better provide care to the patients. Excluding that one nurse from lunch plans, work-related activities, or any after-work gatherings.
Assigning heavy workloads
Repeatedly assigning a nurse a heavy workload while everyone else’s load is relatively light. All the other nurses have time to sit and document while the one nurse is overwhelmed.
Physical abuse
Unwanted physical contact is usually violent in nature.
Mobbing
This happens when a group of bullies band together to create an environment to force the victim to resign (2).


Self Quiz
Ask yourself...
- Have you witnessed any of these behaviors at your organization?
- Is there a behavior that is most indicative of nurse bullying?
- What is the key aspect that makes these behaviors acts of bullying?
Characteristics of a Nurse Bully
Nurse bullies come in all shapes and sizes and come from all walks of life. There isn’t necessarily a template for what a nurse bully will look like. However, there are some characteristics that may help identify a nurse bully.
You may encounter a nurse who bullies out of a sense of superiority. They will be condescending and have an entitled attitude. You will also recognize them by their “correcting comments” often spoken where others can hear. Next, we have nurses who bully because they have been offended by something said or done. They bully with an ax to grind. They may hold on to the grudge for a long time. Creating drama with the victim at the center will be their course of action; they will try to pull in other nurses to help ostracize their victim. Other nurse bullies will use rumors and gossip to bully their victim (3)
These bullies love to dish out the put-downs but can’t take any back. They will become offended at the slightest criticism. There are others who will be very friendly at first. Bringing the victim in close to learn details of their lives and then using that information against them. They will weaponize all obtained information to lift themselves up. Another characteristic is envy. There are those bullies who are envious of others. The envy could stem from something totally unrelated to nursing or the workplace. The victim, however, will most likely possess the item or characteristic that the bully is envious of. This bully is very bitter. Finally, there is the bully who plays favorites. They will favor their clique and ignore or exclude the victim (3).

Self Quiz
Ask yourself...
- Do you recognize these characteristics in the nurses you work with?
- Do you see any of these characteristics in you? How will you change?
What Can You Do?
There are many actions that you can take when you are either the witness or victim of nurse bullying. Though some bullies may be intentionally trying to intimidate a fellow nurse, there are those who are oblivious to the fact that they are bullies. They behave like a bully without knowing that they are perceived as such.
The first action that you may want to take is to talk with the bully about the behavior. The bullying may end there. Once it has been brought to the bully’s attention that the behavior is being taken as bullying, change can occur. Communication may be all that is needed (5). Prior to speaking with the bully, try using empathy. Put yourself in the bully’s shoes to figure out what the motive for the behaviors may be. This may aid you in both the tone and direction of the conversation.
Identifying a mentor in the workplace can also help you through a bullying situation. Having someone that you can talk to about the issue and seek their advice about how to handle the situation. Look for those nurses who can’t be bullied. Why do the bullies not prey on them? Why are they not intimidated? Often, these nurses are focused on the patient’s needs above all else and refuse to allow any situation to be about them or the bully (3).
Talking with your manager or director is another prudent course of action. It is possible that these nurse leaders have the best vantage point to deal with and prevent nurse bullying. They work closely with the front-line staff nurses and should have the pulse of the unit. In their position of authority, they are also able to investigate and, if needed, conduct disciplinary actions.
Unless your manager or director is the bully, a meeting with them to discuss any instances of bullying is needed. Contacting the Human Resources department is another step that can be taken. No matter the situation, it is always important to follow your facility’s policies and procedures and chain of command (3).

Self Quiz
Ask yourself...
- What can you do to prevent/stop nurse bullying in your organization?
- What organizational resource should you use to guide your actions?
Solutions to Nurse Bullying
Nurse bullying has repercussions throughout the entire facility. According to a study from 2012, the cost for each individual who is bullied can be from thirty thousand to one hundred thousand dollars (3). This includes the cost of absenteeism, lower work performance, any therapies needed for physical and psychological issues, and increased turnover due to ongoing bullying.
Nurse bullying can also play a big part in the overall feeling of “burnout” among nurses. Nurse bullying can lead to workplace errors which means it is crucial that organizations have strategies to combat any kind of bullying in the workplace. As nursing accounts for the majority of employees at most hospitals, curbing nurse bullying should be in the forefront. Here are some organizational strategies that should be considered:
Culture of Safety
Many organizations have adopted a “Culture of Safety”. The Culture of Safety promotes patient and colleague safety. It is the shared beliefs and values of the organization that influence behaviors and actions. Principles such as non-punitive reporting, communication of policies and expectations, recognition, and leadership modeling of behaviors all come into play in the Culture of Safety. All reports of bullying should be taken seriously (3).
Admit that there is a problem
Like any issue, the first step in fixing it is admitting that the problem exists in the first place. Bullying thrives in the darkness. Once it is brought to light and people are talking about it, it can be addressed. Even if there is no evidence of nurse bullying in your area, talking about and discouraging it may stop it from even starting (3).
Elimination
Try to eliminate factors that promote an environment of bullying.
Commitment
The organization should commit to a zero-tolerance policy when it comes to bullying. The policy on bullying should outline clear expectations along with the consequences that will be enforced if the policy is not followed. The policy should also include the organization’s social and online media sites (3).
Accountability
Nurses should be encouraged to hold each other accountable. You promote what you permit. As there are generally more bullying witnesses than actual bullies, nurses must be empowered to call out bullying. This can lead to a true change in the culture of an organization (3).

Self Quiz
Ask yourself...
- Is your facility currently using any of the above-mentioned strategies?
- How have these strategies mitigated the incidence of nurse bullying in your area?
- Can an organization eliminate nurse bullying?
Conclusion
Nurse bullying is a real problem that can affect any unit in any hospital. It creates a toxic work environment that we, as nurses, can no longer tolerate. In this post-COVID time, nursing shortages and nurse burnout are rapidly depleting the nursing ranks. It is time for nurses to call out bullying when they see it. It is time for nurse leaders to enforce the organizational consequences of nurse bullying.
We must create safe environments for our new nurses (all nurses) to thrive. It is the only way that our profession will survive. Know the signs of nurse bullying and become the change within your organization. Empower your colleagues to do the same. Together, we can see an end to nurse bullying.
Quality Improvement for Nurses
Introduction
Welcome to the world of Quality Improvement (QI) in healthcare, a dedicated field committed to continually enhancing patient care and outcomes. Quality Improvement involves a systematic approach to identify, analyze, and address areas for improvement within healthcare processes, ultimately resulting in improved patient safety, satisfaction, and overall healthcare excellence (13). In this course, we will embark on a journey to explore the fundamental principles and practical applications of QI, explicitly tailored for nurses who aspire to make a positive impact in their healthcare settings.
As a nurse, you know the significance of providing high-quality patient care. However, you may wonder how you can actively contribute to improving the systems and processes in your workplace.
Imagine this scenario: You observe a recurring issue with medication administration, where doses are occasionally missed due to workflow inefficiencies. Through this course, you will acquire the knowledge and skills to apply QI methodologies like Plan-Do-Study-Act (PDSA) cycles to investigate such issues, implement changes, and monitor the impact of your interventions. By understanding QI principles and tools, you will be better equipped to collaborate with your colleagues, drive meaningful improvements, and ensure that your patients receive the best care possible.

Self Quiz
Ask yourself...
- How can nurses leverage their unique position at the bedside to identify opportunities for quality improvement in healthcare settings?
- Can you provide an example from your own experience or knowledge where a quality improvement project led to tangible improvements in patient care?
- What potential challenges could a nurse encounter when attempting to implement quality improvement projects?
What is Quality Improvement?
Quality Improvement (QI) in healthcare represents an ongoing, systematic effort to elevate the quality of patient care and healthcare services that involves identifying areas needing improvement, implementing changes, and evaluating the effects of those changes to ensure better patient outcomes (12).
Let’s envision a scenario where a hospital's surgical department grapples with a higher-than-average rate of post-operative infections. Through a QI initiative, the healthcare team can meticulously scrutinize the surgical processes, pinpoint potential sources of infection, and introduce evidence-based practices such as enhanced sterilization techniques or more rigorous antibiotic prophylaxis protocols. Over time, they can gauge the effectiveness of these changes by monitoring infection rates for a reduction.
Commonly used QI methodologies in healthcare include the DMAIC (Define, Measure, Analyze, Improve, Control) process and the Plan-Do-Study-Act (PDSA) cycle. These approaches provide structured frameworks for healthcare professionals to tackle issues systematically and iteratively. For example, imagine a bustling primary care clinic with extended patient wait times.
Here, the PDSA cycle can come into play using the systematic iterative steps below:
- The team defines the problem (lengthy wait times)
- The team proceeds to test a change (for example, adjusting appointment scheduling)
- The team then scrutinizes the results and acts accordingly to refine the process.


Self Quiz
Ask yourself...
- How does the concept of Quality Improvement (QI) align with the goal to provide the best possible care for patients?
- Can you think of a specific healthcare scenario where QI methodologies like DMAIC or PDSA could significantly improve patient care?
- What are the advantages of using structured frameworks like DMAIC and PDSA in QI initiatives?
- How do DMAIC or PDSA contribute to the success of improvement projects?
History and Background of Quality Improvement
The history and background of Quality Improvement (QI) in healthcare have a rich and evolving timeline, dating back to the early 20th Century, with significant developments occurring over the years. One pivotal moment in this journey was the introduction of statistical quality control by Dr. Walter A. Shewhart in the 1920s (24). Dr. Shewhart's pioneering work laid the foundation for using statistical methods to monitor and enhance processes, a concept that would become integral to QI initiatives (24).
In the mid-20th Century, the contributions of Dr. W. Edwards Deming further propelled QI principles forward (7). Dr. Deming emphasized the significance of continuous improvement, active employee engagement, and process variability reduction. His ideas found fertile ground in post-World War II Japan, playing a crucial role in the nation's economic recovery and the emergence of renowned companies like Toyota, famous for its Toyota Production System (TPS), incorporating QI concepts (7).
Until today, QI has become indispensable to healthcare systems worldwide (16). To illustrate, envision a scenario where a hospital grapples with a high readmission rate among heart failure patients. By scrutinizing historical data and implementing evidence-based protocols for post-discharge care, hospitals can effectively lower readmissions, enhance patient outcomes, and potentially evade financial penalties under value-based reimbursement models (16).

Self Quiz
Ask yourself...
- How did the work of Dr. Walter A. Shewhart in the early 20th Century contribute to the foundation of QI, and how do statistical methods continue to play a role in healthcare improvement today?
- What fundamental principles were introduced by Dr. W. Edwards Deming, and how did they influence QI practices in healthcare and other industries?
- Can you provide an example of how QI methodologies, inspired by Deming's principles, have been successfully applied in modern healthcare settings to address specific challenges or improve patient care?
- How has continuous improvement evolved, and why is it considered a cornerstone of QI in healthcare?
Models
At the heart of ongoing transformations in healthcare lies various Quality Improvement (QI) models. These models provide structured frameworks for identifying and addressing areas of improvement within healthcare systems (14). These models offer healthcare professionals a systematic approach to instigate meaningful process changes, ultimately resulting in elevated care quality. See some models below.
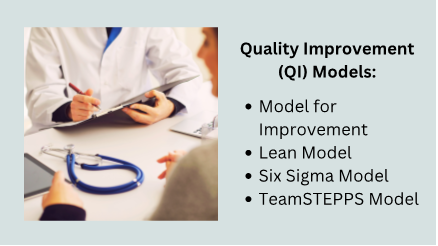
Model for Improvement
The Model for Improvement is a widely recognized and highly effective framework for Quality Improvement (QI) in healthcare. This is because it empowers healthcare professionals to systematically test and fine-tune their ideas for process improvement, ensuring that changes are grounded in evidence and proven effective (17).
The Model for Improvement offers a structured and systematic approach to identifying, testing, and implementing changes to enhance healthcare processes and ultimately elevate patient outcomes.
Developed by Associates in Process Improvement (API), this model revolves around the iterative "Plan-Do-Study-Act" (PDSA) cycle, which forms the foundational structure of QI initiatives (17). The Plan-Do-Study-Act (PDSA) cycle is a systematic approach that guides healthcare teams through quality improvement, and it comprises the four key phases below, each contributing to developing and implementing meaningful changes in healthcare practices (12).
- Plan: In this initial phase, healthcare teams define the specific problem they aim to address, set clear and measurable goals, and craft a comprehensive plan for implementing the proposed change. For instance, if a hospital seeks to reduce patient wait times in the emergency department, the plan may involve adjustments to triage protocols or streamlining documentation processes.
- Do: Once the plan is established, the proposed change is implemented, typically on a small scale or within a controlled or pilot environment. This enables healthcare professionals to assess the feasibility and potential impact of the change without making widespread adjustments.
- Study: The study phase involves rigorous data collection and analysis to evaluate the effects of the change. In our example, the hospital would measure the impact of the new triage protocols on wait times, closely examining whether they have decreased as expected.
- Act: Based on the findings from the study phase, the healthcare team makes informed decisions about the change. They may adopt the change if it has successfully reduced wait times, adapt it further for enhanced effectiveness, or, if necessary, abandon it.
The PDSA cycle's iterative nature means adjustments can be made, and the cycle repeats until the desired improvement is achieved (12).
Lean Model
The Lean model, initially conceived in the manufacturing sector, has found considerable success and applicability in healthcare as a potent tool for process enhancement and waste reduction (22). At its core, Lean thinking revolves around the principles of efficiency and value optimization because it focuses on refining processes to eliminate wasteful elements while simultaneously delivering care of the highest quality (22).
Healthcare organizations have adopted Lean methodologies to tackle many challenges, from reducing patient wait times to improving inventory management and elevating overall patient satisfaction (22). For instance, when a hospital is challenged with prolonged wait times in its outpatient clinic, it can apply Lean principles to systematically analyze the patient flow, pinpoint bottlenecks, and streamline processes.
This might involve reconfiguring furniture to enhance flow, adjusting appointment scheduling, or implementing standardized work procedures. The ultimate objective is to cultivate a patient-centric, efficient environment that ensures timely access to care while meticulously conserving time and resources.
Another integral aspect of Lean thinking is the unwavering commitment to continuous improvement and the pursuit of perfection through the systematic identification and eradication of various forms of waste (19). The forms of waste are often categorized into seven types: overproduction, waiting, unnecessary transportation, overprocessing, excess inventory, motion, and defects (19). By keenly identifying and addressing these forms of waste, healthcare organizations not only enhance the utilization of resources but also curtail costs and elevate the overall quality of care delivery.
Six Sigma model
The Six Sigma model is a robust and widely adopted healthcare method for improving processes and reducing mistakes (9). It was first used in manufacturing but is now used in healthcare to make processes more consistent and improved by finding and fixing mistakes and inefficiencies (9).
An example is when a hospital is concerned about the accuracy of medication dosing for pediatric patients, a Six Sigma team might include: indicating the problem, gathering data on mistakes regarding dosing, and finding out why the mistakes happened. The strategy may encompass the implementation of standardized dosing protocols, refining staff training programs, and closely monitoring the medication administration process to ensure that mistakes are eliminated.
Six Sigma uses a framework called DMAIC (Define, Measure, Analyze, Improve, Control) to make improvements. This framework utilizes data-driven tools to discern problems, quantify their origins, develop practical solutions, and institute control mechanisms to sustain improvements (11). Through this systematic journey, healthcare organizations position themselves to deliver care of elevated quality, curtail costs, and bolster patient safety.
TeamSTEPPS model
TeamSTEPPS, which stands for Team Strategies and Tools to Enhance Performance and Patient Safety, is a teamwork and communication model designed explicitly for healthcare settings (4). Developed by the U.S. Department of Defense and the Agency for Healthcare Research and Quality (AHRQ), TeamSTEPPS focuses on improving patient safety by enhancing team collaboration, communication, and decision-making among healthcare professionals (4).
One key element of TeamSTEPPS is using structured communication techniques to prevent errors and misunderstandings. For instance, during patient handoffs from one healthcare provider to another, TeamSTEPPS emphasizes using a structured tool like SBAR (Situation, Background, Assessment, Recommendation) to convey critical information succinctly and accurately. This ensures that essential patient details are noticed, reducing the risk of adverse events (18).
In a surgical team scenario, TeamSTEPPS principles can be applied to improve teamwork and communication among surgeons, nurses, and anesthesiologists. The model encourages briefings before procedures to set clear objectives, huddles during surgery to address emerging issues, and debriefings afterward to reflect on the process and identify areas for improvement. By fostering a culture of open communication and mutual respect, TeamSTEPPS contributes to safer, more efficient healthcare delivery (4).


Self Quiz
Ask yourself...
- How can healthcare organizations determine which QI model suits their specific challenges or improvement goals?
- How do QI models emphasize data collection and analysis, and why is this critical in healthcare?
- Can you imagine a real-world scenario where the Lean Six Sigma framework can successfully improve healthcare processes and outcomes?
- What are some emerging trends or innovations in QI models and methodologies, and how might they shape the future of healthcare quality improvement?
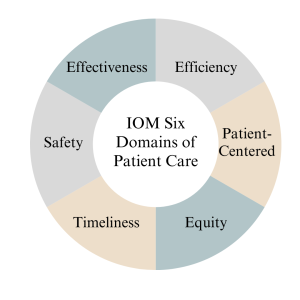
IOM Six Domains of Patient Care
The Institute of Medicine (IOM), now known as the National Academy of Medicine, introduced the Six Domains of Quality in Healthcare as a framework to assess and improve the quality of patient care (14). These domains, introduced in 2001, encompass various aspects of care delivery and patient experience, helping healthcare organizations and providers identify areas for improvement (14). The domains serve as pillars for assessing the different dimensions of care delivery, ensuring that healthcare organizations and providers address the holistic needs of patients (14).
Definitions
The Six Domains of Patient Care are essential for providing high-quality healthcare. See definitions of each of the IOM's six domains of patient care below.
- Safe: Safety is the foundational domain, emphasizing the importance of reducing the risk of patient harm. This includes preventing medical errors, preventing infections, and ensuring the safe administration of medications. Healthcare organizations implement safety protocols and engage in continuous monitoring to minimize risks (14).
- Effective: Effective care ensures that patients receive evidence-based treatments and interventions that result in the desired outcomes. It involves using the best available scientific knowledge to make informed decisions about patient care avoiding unnecessary or ineffective treatments (14).
- Patient-Centered: Patient-centered care focuses on individualizing healthcare to meet each patient's unique needs and preferences. It involves respecting patients' values and preferences, engaging them in shared decision-making, and delivering care with empathy and compassion (14).
- Timely: Timely care emphasizes reducing delays in healthcare delivery. It includes providing care promptly and avoiding unnecessary waiting times for appointments, tests, and treatments. Timely care is especially critical in emergencies (14).
- Efficient: Efficiency in healthcare means maximizing resource utilization and minimizing waste while providing high-quality care. This domain emphasizes streamlining processes, reducing unnecessary costs, and optimizing healthcare resources (14).
- Equitable: Equitable care underscores the importance of providing healthcare that is fair and just, regardless of a patient's background, socioeconomic status, or other factors. It aims to eliminate healthcare access and outcomes disparities among different patient populations (14).
Measures
Measures in the context of the Institute of Medicine (IOM) six domains of patient care refer to the metrics and indicators used to assess and evaluate the quality of care provided in each domain. According to (14), the measures below are essential for monitoring and improving healthcare services. See details below.
- The "Safe" domain measures focus on tracking and reducing adverse events and medical errors. Key indicators include rates of medication errors, hospital-acquired infections, falls, and complications from procedures. Safety measures also assess the implementation of safety protocols, such as hand hygiene compliance and patient identification bracelets.
- Measures in the "Effective" domain assess how evidence-based practices and treatments are utilized. These measures include adherence to clinical guidelines, appropriate use of medications, and the success rates of medical interventions. Additionally, outcomes such as patient recovery, remission, or improvement are indicators of the effectiveness of care.
- The "Patient-Centered" domain focuses on assessing the patient’s experience and satisfaction with care. Patient surveys and feedback are standard measures, evaluating aspects like communication with healthcare providers, involvement in decision-making, and overall satisfaction with the care received. Healthcare organizations also measure shared decision-making and respect for patient preferences.
- Measures related to the "Timely" domain evaluate the efficiency of healthcare delivery. Key metrics include waiting times for appointments, diagnostic tests, and procedures. Additionally, measures track the timely delivery of urgent care and the avoidance of unnecessary delays in treatment.
- Efficiency measures aim to quantify resource utilization and the reduction of waste in healthcare. Metrics may include the cost of care per patient, length of hospital stays, and resource allocation efficiency. Improvement in resource utilization and cost-effectiveness are vital indicators of efficiency.
- Measures within the "Equitable" domain assess disparities in healthcare access and outcomes among different patient populations. Healthcare utilization and outcomes data are stratified by demographics, socioeconomic status, race, and ethnicity to identify and address inequities. Key indicators include access to preventive care, healthcare utilization rates, and health outcomes across various demographic groups.

Self Quiz
Ask yourself...
- How can healthcare providers ensure their care aligns with patients' values, preferences, and cultural backgrounds?
- What challenges might patients face in accessing healthcare services, and how can healthcare organizations improve access for all patients?
- What are the potential consequences of poor care coordination among healthcare providers, and how can interdisciplinary teams work together to enhance coordination?
- Why must healthcare organizations continually assess and improve the quality of care they provide, and what mechanisms can be implemented to support ongoing improvement efforts?
Nursing Quality Indicators
According to (5), nursing quality indicators are essential metrics used to evaluate and improve the quality of nursing care in healthcare settings. These indicators provide valuable insights into nursing practice and patient outcomes, helping healthcare organizations and nursing staff deliver safe, effective, patient-centered care. Let's delve into some key nursing quality indicators and their significance below.
Patient Falls
Patient falls are a critical quality indicator in nursing care since they can result in severe injuries and complications for patients (5). As a result, healthcare organizations measure and monitor the rate of patient falls to identify trends and implement preventive measures.
For example, when a hospital notices an increase in the rate of falls among elderly patients in a particular unit, they may introduce interventions such as nonslip flooring, improved lighting, and patient education as fall prevention strategies to reduce the incidence of falls.

Medication Administration Errors
Ensuring accurate medication administration is crucial in nursing practice because medication errors can lead to adverse events, including patient harm or death (5). Nursing quality indicators related to medication administration errors include the rate of medication errors and adherence to medication reconciliation processes (5). For instance, nurses are encouraged to verify patient allergies and cross-check medication orders to prevent errors. If there is an increase in medication errors in a healthcare facility, it may prompt a review of medication administration protocols and additional staff training.

Pressure Ulcers (Bedsores)
Pressure ulcers are a quality indicator of patient skin integrity since they develop when patients remain immobile for extended periods (5). As a result, healthcare organizations measure the incidence and prevalence of pressure ulcers as an indicator of the quality of nursing care (5).
Patient Satisfaction
Patient satisfaction is a patient-centered nursing quality indicator since it reflects the overall patient experience and perception of care (5). Surveys and feedback mechanisms are used to measure patient satisfaction. For example, a scenario might involve patients receiving post-discharge surveys that assess various aspects of their hospital experience, including nurse responsiveness, communication, and pain management. Healthcare organizations can use this feedback to identify areas for improvement and enhance patient-centered care.
In summary, nursing quality indicators encompass a range of metrics that evaluate nursing care quality, patient safety, and patient experiences. By monitoring and responding to these indicators, healthcare organizations and nursing staff can continuously improve their quality of care, leading to better outcomes and increased patient satisfaction (5).

Self Quiz
Ask yourself...
- Why is data collection critical in nursing quality improvement efforts?
- What types of data should nurses prioritize collecting to assess patient safety?
- How can nurses ensure the accuracy and reliability of the data they collect for quality improvement purposes?
- What challenges might nurse face when collecting patient-related data, and how can these challenges be overcome?
Data Collection
Quality improvement data collection is a critical component of healthcare quality initiatives, providing the necessary information to assess the current state of care, identify areas for improvement, and monitor progress over time (2). Accurate and meaningful data collection enables healthcare organizations to make informed decisions, implement evidence-based interventions, and ultimately enhance patient outcomes. Let's explore the methods of data collection below.
- Clinical Outcome Collection: Clinical outcome data collection is essential for assessing the effectiveness of healthcare interventions (2). For example, consider a scenario where a hospital is implementing a quality improvement project to reduce surgical site infections (SSIs) following orthopedic surgeries. Data collection would involve tracking the number of SSIs occurring over a specific period and collecting information on patient characteristics, surgical techniques, and post-operative care protocols. By analyzing this data, the healthcare team can identify trends, risk factors, and areas for improvement, ultimately leading to targeted interventions to reduce SSIs.
- Patient Satisfaction Survey Data Collection: Patient satisfaction surveys are valuable tools for collecting data on patient experience (2). A primary care clinic that aims to improve patient satisfaction may administer surveys to patients after each visit, asking about aspects of care such as communication with healthcare providers, wait times, and overall experience. The collected data can reveal areas of strength and areas requiring improvement. For instance, if survey results consistently indicate longer-than-desired wait times, the clinic can adjust scheduling practices or implement strategies to reduce wait times and enhance patient satisfaction.
- Process Measures Data Collection: Process measure data collection focuses on evaluating the efficiency and effectiveness of healthcare processes (2). For instance, in a medication reconciliation scenario, a healthcare organization might collect data on the accuracy and completeness of medication lists during care transitions. By tracking the frequency of medication reconciliation discrepancies, they can identify process inefficiencies and implement standardized protocols for reconciliation, leading to safer care transitions and reduced medication errors.
- Adverse Event Reporting Data Collection: Adverse event reporting is a crucial mechanism for collecting data on incidents that result in patient harm or near misses (2). For example, consider a scenario where a nurse administers the wrong medication dose to a patient but catches the error before any harm occurs. Reporting this near-miss event allows the healthcare organization to investigate the root causes, implement preventive measures, and share lessons learned with the care team to prevent similar incidents in the future.
Types of Data
Data types play a crucial role in understanding the current state of care, identifying areas for improvement, and implementing evidence-based interventions (2). Let’s explore the different types of data used in quality improvement below.
- Quantitative Data: Quantitative data involves numerical measurements and is particularly useful for assessing the frequency and extent of specific events or outcomes (2). For instance, in a hospital's quality improvement project focused on reducing hospital-acquired infections, the team collects quantitative data on the number of infections over time, allowing them to track trends and measure the impact of interventions, such as hand hygiene protocols or disinfection practices.
- Qualitative Data: Qualitative data provides insights into the "why" and "how" behind healthcare processes and patient experiences (2). This data type is collected through interviews, focus groups, and open-ended surveys. For example, in a primary care setting aiming to improve patient satisfaction, qualitative data may be collected through patient interviews to gather in-depth information about their perceptions of care. Qualitative data can uncover nuances and provide valuable context to complement quantitative findings (2).
- Patient-Reported Data: Patient-reported data includes information directly provided by patients about their health, symptoms, experiences, and preferences. Patient-reported outcome measures (PROMs) and patient-reported experience measures (PREMs) are standard data collection tools. In a scenario involving chronic disease management, patients with diabetes may be asked to complete a PROM assessing their quality of life and symptom management. This data helps healthcare providers tailor care plans to individual patient needs and preferences (2).
- Process Data: Process data track the steps and activities involved in healthcare delivery to help assess the efficiency and effectiveness of care processes. For example, in a surgical quality improvement initiative, process data may include the time from patient admission to surgery, surgical team checklist completion, and adherence to anesthesia protocols. By collecting and analyzing process data, healthcare organizations can identify bottlenecks and areas for improvement in care delivery processes.
In summary, quality improvement data collection relies on various data types, including quantitative, qualitative, patient-reported, and processed data. Each data type contributes to a comprehensive understanding of healthcare quality and supports evidence-based decision-making to enhance patient care and outcomes.

Identification Stage
The identification stage for quality improvement data collection is a critical initial phase where healthcare organizations and teams define what data to collect, why it is relevant, and how it aligns with their quality improvement goals (23). This stage is essential for ensuring meaningful data collection efforts will lead to actionable insights. Let's explore the identification stage in more detail.
- Defining Objectives and Goals: During this stage, healthcare organizations must clearly define the objectives and goals of their quality improvement initiative (23). For instance, a hospital aiming to reduce readmission rates for heart failure patients may set a specific goal of reducing readmissions by 20% within the following year.
- Selecting Relevant Metrics: Identifying the right metrics and data points is crucial, and organizations should choose metrics that directly relate to their quality improvement goals (23). Continuing with the example of reducing heart failure readmissions, relevant metrics might include the number of heart failure patients readmitted within 30 days, the reasons for readmission, and patient characteristics. By selecting these metrics, the organization ensures that data collection efforts are aligned with their specific improvement goal.
- Determining Data Sources: Healthcare organizations must identify where the necessary data will be sourced (23). This may involve looking at electronic health records, claims data, patient surveys, or other sources. For instance, to collect data on heart failure readmissions, the hospital may extract relevant information from electronic health records, including admission and discharge dates, diagnosis codes, and patient demographics.
- Creating Data Collection Protocols: Establishing clear data collection protocols is essential for consistency and reliability (23). Healthcare teams should define how data will be collected, who will be responsible for data collection, and the frequency of data collection. For example, in a hospital project aiming to improve hand hygiene compliance, data collection protocols might specify that trained observers will monitor hand hygiene practices at random intervals and record their findings on standardized forms.
By carefully navigating the identification stage, healthcare organizations ensure that their quality improvement data collection efforts are purposeful and aligned with their goals. This sets the stage for collecting meaningful data to drive evidence-based decisions and interventions to enhance healthcare quality.
Gathering Stage
The gathering stage of quality improvement data collection is crucial for healthcare organizations to collect the identified data based on their quality improvement objectives and goals (23). This stage involves systematically collecting data from various sources and often requires careful planning and coordination to ensure data accuracy and completeness. Let's delve into the gathering stage in detail below.
- Data Collection Methods: To gather data, healthcare organizations must determine the most suitable methods for collecting the identified data, which may involve a combination of electronic health records, patient surveys, direct observations, and administrative databases (23). For example, in a quality improvement project aimed at reducing hospital readmissions, data may be collected by reviewing electronic health records to track patient outcomes, conducting patient surveys to gather feedback on discharge instructions, and analyzing administrative data to identify trends in readmission rates.
- Ensuring Data Accuracy and Consistency: Data accuracy is critical in the gathering stage, and organizations must implement procedures to collect data consistently and without errors (23). For instance, if a healthcare facility is collecting data on medication administration, nurses may use standardized protocols to accurately record medication administration times and doses. Regular training and quality checks may also be implemented to maintain data accuracy.
- Timely Data Collection: Timeliness is another important aspect of the gathering stage, and data should be collected promptly to ensure it is current and relevant for analysis and decision-making (23). In a scenario involving tracking patient outcomes, healthcare teams may set specific intervals for data collection, such as collecting post-surgical complication data daily or weekly, depending on the project's requirements.
- Data Security and Privacy: Protecting patient data is a paramount concern in healthcare. As a result, healthcare organizations must adhere to strict privacy and security protocols during the gathering stage to ensure that patient information is handled confidentially and complies with applicable laws and regulations, such as the Health Insurance Portability and Accountability Act (HIPAA) (23). For example, when collecting patient-reported data, organizations may anonymize responses to protect patient identities and comply with privacy regulations.
By effectively managing the gathering stage, healthcare organizations can ensure that they collect accurate, timely, and secure data that will serve as the foundation for subsequent analysis and quality improvement efforts.
Analysis stage
The analysis stage for quality improvement data collection is a critical phase where collected data is processed, examined, and transformed into actionable insights. This stage involves various analytical techniques and tools to identify patterns, trends, and areas for improvement (2). Let's explore the analysis stage in detail below.
- Descriptive Analysis: Descriptive analysis is the initial step in data analysis, focusing on summarizing and presenting data meaningfully (2). For example, in a quality improvement project aimed at reducing patient wait times in an emergency department, an analysis may involve calculating and displaying key statistics, such as average wait times, 95th percentile wait times, and the distribution of wait times (2). These descriptive statistics provide an overview of the current situation and help identify areas that need attention.
- Root Cause Analysis (RCA): Root cause analysis is a critical aspect of the analysis stage, as it helps pinpoint the underlying causes of issues or problems (2). In our scenario, if the analysis reveals prolonged wait times in the emergency department, RCA may involve a thorough investigation into the factors contributing to the delays. Potential root causes include staffing shortages, inefficient triage processes, or bottlenecks in diagnostic testing. Identifying these root causes is essential for developing effective interventions.
- Statistical Analysis: Statistical analysis plays a vital role in quality improvement by examining the relationships between variables and testing hypotheses (2). In reducing hospital readmissions, statistical analysis may be used to identify factors associated with readmission risk. For example, healthcare teams can use logistic regression to analyze patient data to determine which variables, such as comorbidities or medication adherence, are statistically significant predictors of readmission risk. This information can guide the development of targeted interventions for at-risk patients.
- Benchmarking: Benchmarking involves comparing an organization's performance data with industry standards or best practices to identify performance gaps (2). When a hospital is looking to improve patient satisfaction, benchmarking may involve comparing its patient satisfaction scores to those of similar hospitals or national averages. Identifying areas where the hospital falls behind benchmarks can inform strategies for improvement, such as implementing best practices from higher-performing institutions.
The analysis stage is critical for transforming raw data into actionable insights and understanding healthcare quality factors (2). Through descriptive analysis, root cause analysis, statistical techniques, and benchmarking, healthcare organizations can gain valuable insights that drive evidence-based decisions and interventions to improve care quality (6).
Benchmarking
The benchmarking stage in quality improvement data collection is a crucial phase where healthcare organizations compare their performance against established benchmarks or best practices (1). This gives healthcare organizations a clear understanding of their position relative to recognized standards and allows them to effectively identify areas for improvement, prioritize, and focus their improvement efforts (5). Let's delve into the benchmarking stage in detail below.
- Defining Benchmarks: In the benchmarking stage, healthcare organizations must define the benchmarks or standards against which they will measure their performance. These benchmarks can be internal (comparing current performance to historical data) or external (comparing to industry standards, best practices, or similar organizations) (1). For example, a primary care clinic seeking to improve appointment scheduling efficiency may choose to benchmark its appointment wait times against industry benchmarks for acceptable wait times.
- Collecting Comparative Data: Gathering data that allows for a meaningful comparison is critical in benchmarking, so healthcare organizations must collect data from relevant sources to measure their performance against the chosen benchmarks (1). Continuing with the appointment scheduling example, the clinic may collect data on the time it takes to schedule an appointment, the number of scheduling errors, and patient feedback. This data is then compared to industry benchmarks or best practices.
- Identifying Performance Gaps: The benchmarking process reveals gaps or disparities between an organization's performance and the benchmarks to highlight improvement areas (1). For instance, if the clinic discovers that its appointment wait times are significantly longer than industry benchmarks, this identifies a performance gap that needs to be addressed to enhance patient access and satisfaction.
- Developing Improvement Strategies: Healthcare organizations can develop targeted improvement strategies once performance gaps are identified. These strategies are based on evidence from the benchmarking process and aim to align performance with or exceed established benchmarks (1). In our scenario, the clinic may implement strategies such as optimizing appointment scheduling processes, enhancing staff training, or using technology to improve scheduling efficiency.


Self Quiz
Ask yourself...
- Why is data collection a crucial step in the quality improvement process?
- What types of data are typically collected during the data collection stage of quality improvement?
- How do you determine which data points are relevant to your quality improvement project?
- What methods and tools can be used to collect data accurately and efficiently?
Change Models in Healthcare
Change models are essential frameworks used in healthcare, including nursing, to guide and manage the effective implementation of quality improvement initiatives (15). These models offer structured approaches to initiate, plan, execute, and sustain changes in healthcare practice (15). Let’s discuss some prominent change models used in nursing quality improvement below.
- Kotter's 8-Step Change Model: Developed by Dr. John Kotter, this model emphasizes the importance of creating a sense of urgency, building a guiding coalition, and sustaining the change (15). For instance, in a nursing scenario focused on reducing hospital-acquired infections, the 8-step model would involve creating urgency by highlighting the impact of infections on patient safety, assembling a coalition of nurses and infection control specialists, and sustaining change by monitoring infection rates over time and continually reinforcing hygiene protocols.
- Lewin's Change Management Model: Lewin's model consists of three stages: unfreezing, changing, and refreezing (15). Let's consider implementing a new electronic health record (EHR) system in nursing. Nurses first "unfreeze" by acknowledging the need for a new system and undergoing training. Then, they "change" by adopting the EHR and adjusting workflows. Finally, they "refreeze" by becoming proficient and maintaining the new system's use as a standard practice.
- PDSA Cycle (Plan-Do-Study-Act): This model emphasizes iterative cycles of planning, implementing, observing, and adjusting (15). For instance, if a nursing unit aims to improve patient handoffs, they might "plan" by identifying handoff best practices, "do" by implementing changes, "study" by assessing the impact on patient outcomes, and "act" by making further refinements based on their findings. This continuous cycle allows for gradual, data-driven improvements.
- ADKAR Model: The ADKAR model focuses on individual change management, and this could apply to a scenario where nurses are adopting new pain management protocols (15). Nurses would first need awareness of the change (A), followed by desire (D) to participate, knowledge (K) of how to implement the new protocols, ability (A) to do so, and reinforcement (R) to sustain the change over time.
In summary, change models provide structured approaches to drive quality improvement initiatives in nursing, and by applying these models, nurses and healthcare organizations can systematically plan, implement, and evaluate changes to enhance patient care, safety, and outcomes (15).

Self Quiz
Ask yourself...
- Why are change models essential in nursing quality improvement initiatives?
- What is the primary purpose of creating a sense of urgency in change models like Kotter's 8-Step model?
- How does Lewin's Change Management Model address the need to "unfreeze" existing practices in nursing before implementing change?
- Why is individual change management crucial in nursing practice, as the ADKAR model emphasizes?
Implementing Change
Implementing changes for quality improvement in nursing is a multifaceted process that requires careful planning, effective communication, and the engagement of healthcare professionals at all levels. According to (15), successful implementation ensures that desired changes are integrated into daily nursing practice, improving patient outcomes. Let’s explore key strategies and considerations for implementing changes in nursing quality improvement below.
- Engage Interdisciplinary Teams: According to (15), collaborative engagement is crucial when implementing changes in nursing practice, and healthcare organizations should assemble interdisciplinary teams that include nurses, physicians, administrators, and other stakeholders. For example, in a scenario involving the adoption of a new pain management protocol, nurses can collaborate with physicians to ensure the consistent application of evidence-based pain management practices. This team approach facilitates a shared understanding of the change and fosters buy-in from all parties.
- Effective Communication: Clear and consistent communication is essential during the implementation phase, so nurses should communicate the rationale behind the change, its expected benefits, and the specific steps involved (15). For example, suppose a hospital is transitioning to a new electronic health record system. In that case, nurses can attend training sessions to understand its features and communicate effectively with patients about how it will enhance their care. This ensures that all stakeholders are informed and can adapt to the change seamlessly.
- Training and Education: Providing adequate training and education is critical to equip nursing staff with the knowledge and skills to implement the change effectively (15). In the case of introducing a new wound care protocol, nurses would require training on the updated practices, wound assessment techniques, and the use of new wound care products. In addition to initial training, ongoing education would ensure that nursing staff stay current with best practices to provide quality care confidently.
- Continuous Monitoring and Feedback: According to (15), implementing change is an ongoing process that requires constant monitoring and feedback since feedback mechanisms allow for adjustments and refinements to the change process. As a result, nursing quality improvement initiatives benefit from the regular collection and analysis of data to assess the impact of the change. For example, suppose a hospital introduces a sepsis screening tool. In that case, nurses can track the number of patients screened, identify missed cases, and evaluate whether early interventions have reduced sepsis-related mortality rates. By engaging interdisciplinary teams, fostering effective communication, providing training and education, and implementing continuous monitoring and feedback mechanisms, nurses can successfully implement changes that improve the quality of patient care and enhance overall healthcare outcomes (8).

Self Quiz
Ask yourself...
- Why is it crucial for nursing teams to engage in interdisciplinary collaboration when implementing changes for quality improvement?
- How can effective communication strategies help nursing staff understand the purpose and benefits of a proposed change in healthcare practice?
- What role does ongoing training and education play in ensuring that nursing staff are well-prepared to implement and sustain changes in their practice?
- What methods can be employed to gather feedback from nursing staff while implementing a new practice or protocol?
Evaluating Change
Evaluating change for quality improvement in nursing is a critical phase that involves assessing the impact and effectiveness of implemented changes on patient care outcomes, safety, and the overall quality of healthcare services. According to (15), rigorous evaluation ensures that improvements are sustained, and necessary adjustments are made. Let’s explore key strategies and considerations for evaluating changes in nursing quality improvement below.
- Establishing Clear Evaluation Metrics: To evaluate change effectively, it is essential to define clear and measurable evaluation metrics, and according to (15), these metrics should align with the specific objectives of the change initiative. For example, suppose a nursing unit has introduced a new hand hygiene protocol to reduce hospital-acquired infections. In that case, evaluation metrics may include the number of infections before and after the change, adherence to hand hygiene guidelines, and patient satisfaction scores related to cleanliness and infection prevention.
- Data Collection and Analysis: Data collection is a fundamental component of the evaluation process, and nursing teams should collect relevant data using standardized methods and tools (15). In our scenario, data on infection rates can be collected regularly, and statistical analysis can be performed to determine whether the change has had a statistically significant impact. Nurses can then use run charts or control charts to visualize trends in infection rates over time, allowing for early detection of any potential issues.
- Patient and Staff Feedback: Patient and nursing staff feedback is invaluable in evaluating change since patients' perspectives on the quality of care and their experiences following the change can provide insights into the initiative's effectiveness (15). Additionally, nursing staff can provide feedback on the practicality and feasibility of the new practices. For instance, nursing staff may suggest further improvements in infection control procedures.
- Sustainability and Continuous Improvement: Evaluating change is not solely about assessing immediate outcomes but also ensuring sustainability and continuous improvement. According to (15), nursing teams should determine whether the positive effects of the change are maintained over time and whether there is room for further refinement. For example, when a nursing unit has reduced infection rates, regular audits and monitoring should continue to ensure sustained compliance with hygiene protocols.

Self Quiz
Ask yourself...
- Why must nursing teams establish clear and measurable evaluation metrics when assessing the impact of change in healthcare practice?
- How can nurses effectively collect and analyze data to evaluate the success of a change in their nursing practice?
- What role does patient feedback play in evaluating the impact of a change on the quality of nursing care, and how can this feedback be gathered and utilized?
- How can nursing staff engage in ongoing self-assessment to determine their practice changes' effectiveness and identify improvement areas?

Self Quiz
Ask yourself...
- What specific infection prevention measures should nurses prioritize in their daily practice to reduce hospital-acquired infections, and why are these measures effective?
- What are the primary goals of a quality improvement project to reduce hospital-acquired infections, and how can nursing staff contribute to achieving these goals?
- Why is continuous monitoring and evaluation crucial in quality improvement projects, and how can nursing staff use data to drive ongoing improvements in patient care quality?
- Enhancing Medication Safety: Medication errors can have severe consequences for patients (6). A quality improvement project may target medication safety by introducing barcode scanning systems for medication administration, implementing double-check procedures for high-risk medications, and providing ongoing training to nursing staff. The project's effectiveness can be assessed by monitoring the number of medication errors reported and verifying that the new safety measures reduce the occurrence of such errors. For example, a nursing team could reduce the incidence of wrong-patient medication administration by implementing barcode scanning during medication administration.

Self Quiz
Ask yourself...
- How can nurses ensure that barcode scanning systems and double-check procedures are effectively integrated into their daily workflow in medication safety improvement projects?
- What potential challenges and barriers can nurse units encounter when implementing medication safety improvements, and how can these challenges be addressed?
- Improving Nurse-to-Patient Ratios: Adequate nurse staffing levels are crucial for patient safety and quality of care (6). A quality improvement project may involve adjusting nurse-to-patient ratios based on patient acuity levels, introducing workload management tools, and conducting regular staffing needs assessments. In this case, the project's success can be measured by tracking patient outcomes, nurse workload, and patient satisfaction scores. For example, a nursing unit could reduce nurse burnout and improve patient care by optimizing staffing ratios during peak hours.

Self Quiz
Ask yourself...
- Why is it important to regularly assess and adjust nurse-to-patient ratios in a healthcare setting, and what strategies can nurse leaders employ to optimize staffing levels?
- In a quality improvement project focused on nurse-to-patient ratios, what key factors should nurse leaders consider when determining staffing needs during different shifts and patient acuity levels?
- Enhancing Discharge Planning and Care Transitions: Effective care transitions from the hospital to home or other healthcare settings are essential to preventing readmissions and ensuring continuity of care (6). A quality improvement project may focus on improving the discharge planning process, including patient education, medication reconciliation, and post-discharge follow-up. Success can be assessed by monitoring readmission rates and patient-reported experiences. For example, a nursing team could work on reducing hospital readmissions by ensuring that patients receive thorough discharge instructions and have access to follow-up care.

Self Quiz
Ask yourself...
- What steps can nurse teams take to enhance the discharge planning process and ensure seamless care transitions for patients moving from the hospital to home care?
- What strategies can nurse teams employ to ensure that patient education during discharge planning is effective and leads to better patient outcomes and satisfaction?
The above examples illustrate the diverse range of quality improvement projects in nursing, each addressing specific challenges to enhance patient safety and care quality.

Self Quiz
Ask yourself...
- Why is continuous monitoring and evaluation crucial in quality improvement projects, and how can nursing staff use data to drive ongoing improvements in patient care quality?
- What are the primary goals and objectives of QI models, and how do they contribute to the overall quality of healthcare?
Conclusion
In conclusion, this course provides essential knowledge and skills valuable for nurses aiming to deliver high-quality, safe, patient-centered care. Quality improvement in nursing is not merely a theoretical concept but a practical approach that can be applied to various aspects of healthcare, and one critical aspect to remember is the importance of interdisciplinary collaboration. As frontline caregivers, nurses must collaborate with physicians, administrators, pharmacists, and other healthcare professionals to drive improvements in healthcare delivery.
As nurses continue to play a pivotal role in healthcare delivery, the knowledge and skills gained from this course will empower them to lead and actively participate in quality improvement initiatives. By applying quality improvement principles, nurses can contribute to better patient experiences, patient outcomes, and overall healthcare quality.
Final Reflection Questions
- What have you learned from this course?
- Why is interdisciplinary collaboration essential for nurses to effectively implement quality improvement initiatives in healthcare settings, and how can nurses foster collaboration among healthcare professionals?
- How does the concept of continuous learning and adaptation align with the dynamic nature of healthcare, and what strategies can nurses employ to stay current with evolving best practices and guidelines?
- In what ways does Quality Improvement benefit both healthcare providers and patients?
- What are the potential challenges in implementing QI initiatives in a healthcare organization?
- In what ways has QI in healthcare become intertwined with the broader goals of healthcare reform, such as improving patient outcomes and reducing healthcare costs?
- What role does leadership play in the effective implementation of QI models?
- How can leaders promote a culture of continuous improvement within healthcare organizations?
- How do QI models facilitate interdisciplinary collaboration among healthcare professionals to drive improvements in patient care?
- What challenges might healthcare organizations face when attempting to adopt and sustain QI models, and how can these challenges be overcome?
- How does the "testing and learning" concept in the PDSA cycle align with the principles of evidence-based practice in healthcare?
- In what ways do QI models promote patient-centered care and patient safety, and can you provide examples of tangible improvements in these areas achieved through QI initiatives?
- How can the Six Sigma model contribute to the reliability and consistency of healthcare processes?
- Safe: What steps can healthcare organizations take to minimize the risk of medical errors and adverse events?
- Practical: How do healthcare providers ensure that evidence-based treatments and interventions lead to positive patient outcomes?
- Patient-centered: Why is it important to involve patients in their care decisions, and how can healthcare professionals effectively engage patients in the decision-making process?
- Timely: What are some key factors contributing to delays in healthcare delivery, and how can these delays be reduced to improve timeliness?
- Efficient: How can healthcare processes and workflows be streamlined to enhance efficiency and reduce waste?
- Equitable: What are some barriers to achieving healthcare equity, and how can healthcare organizations address these disparities?
- How can nurses actively involve patients in data collection to enhance patient-centered care?
- What tools or technologies are available to streamline data collection processes in nursing practice?
- How can nurses effectively collaborate with interdisciplinary teams to gather comprehensive data for quality improvement initiatives?
- What strategies can nurses employ to maintain patient privacy and confidentiality while collecting sensitive healthcare data?
- What methods can nurse use to analyze and interpret the data they collect to identify areas for improvement?
- Why must nurses regularly review and assess the data they collect to drive continuous quality improvement in healthcare settings?
- Regarding patient falls, what strategies can healthcare organizations implement to reduce the incidence of patient falls, and how can nursing staff actively contribute to fall prevention efforts?
- How can nurses ensure the accurate and safe administration of medications, and what measures can be taken to minimize medication errors?
- What are the key nursing practices and interventions that can prevent the development of pressure ulcers in hospitalized patients, and how can nursing staff collaborate to achieve this goal?
- Why is patient satisfaction an important nursing quality indicator, and what actions can nurses take to enhance the overall patient experience?
- What impact do nurse-to-patient staffing ratios have on the quality of nursing care, and how can healthcare organizations ensure safe nurse staffing levels?
- How can nurses enhance patient education to promote better understanding and self-management of their health conditions?
- How can you ensure that the data collected is reliable and valid?
- What role does standardization play in data collection for quality improvement?
- How can you establish baseline data for comparison in your quality improvement project?
- What challenges or obstacles might you encounter when collecting data for quality improvement?
- How frequently should data be collected to monitor progress in a quality improvement project?
- How can you involve frontline staff in the data collection to ensure accuracy?
- What measures can be taken to protect patient privacy and confidentiality during data collection?
- How can you analyze the data collected to identify trends or patterns?
- What actions should be taken if the data collected indicates a problem or deviation from the desired outcome?
- What strategies can ensure that data collection remains an ongoing and sustainable practice in healthcare quality improvement efforts?
- What are the potential challenges or resistance nurses might encounter when implementing changes using these models?
- How can a guiding coalition or interdisciplinary team be effectively assembled to support nursing quality improvement efforts?
- What strategies can nurses employ to sustain changes and prevent reverting to previous practices once implemented?
- How can nursing leaders ensure that staff have the necessary knowledge and skills to embrace the changes outlined in these models?
- How can nurses use these change models to promote a culture of continuous improvement in healthcare settings?
- How can nurses ensure their implementation changes align with evidence-based best practices and clinical guidelines?
- What potential challenges or barriers might nurse teams encounter when trying to implement changes for quality improvement?
- What strategies can address resistance to change among nursing staff and promote their active participation in the implementation process?
- How can nursing leaders effectively communicate the expected outcomes and benefits of the change to gain support and commitment from their teams?
- What are the advantages of using data and performance metrics to monitor the progress and impact of change implementation in nursing practice?
- How can nursing staff ensure that changes are sustained and become integral to their daily practice rather than temporary modifications?
- Why is it crucial to consider the sustainability of change when evaluating its long-term impact on nursing quality improvement?
- What challenges or obstacles might nurse teams encounter when collecting and analyzing data for change evaluation, and how can these challenges be addressed?
- How can nursing leaders encourage a culture of continuous improvement among their teams as part of the change evaluation process?
- What strategies can be employed to ensure that the feedback and insights gathered during the evaluation phase are actively used to refine and optimize nursing practices?
- What are the potential consequences of not conducting thorough and systematic evaluations of changes in nursing practice for quality improvement?
- How can nursing staff and healthcare organizations ensure that the lessons learned from change evaluations are applied to future improvement initiatives to enhance patient care outcomes?
Workplace Violence Against Nurses
Introduction
The role of the registered nurse, while fundamentally dedicated to the care and wellbeing of patients, has long been fraught with challenges that extend beyond the complexities of medical care. One such pressing concern is workplace violence, an issue that nurses confront with alarming frequency. Recent statistics show that healthcare workers, particularly nurses, are at a higher risk for workplace violence compared to other professions.
Given the vital role nurses play in patient care and the broader healthcare system, it is imperative to understand the scope, sources, and solutions to this pressing issue. This continuing education course is dedicated to arming nurses with the knowledge, tools, and strategies to recognize, respond to, and prevent incidents of workplace violence, thereby ensuring their safety and the uninterrupted provision of quality care.
Workplace Violence
Definitions
The Occupational and Safety Health Administration (OSHA) (3) defines workplace violence (WPV for the purpose of this course) as any act or threat of physical violence, harassment, intimidation, or other threatening, disruptive behavior that occurs at the work site. This can also include verbal, written, or acts of sabotage against an individual while they are at work.
Workplace violence crosses all demographic barriers and is indiscriminate in who it can and does affect. Even seeing workplace violence influences morale, attendance, and the overall well-being of employees and their co-workers.
Types of Violence
Currently, there are four categories of workplace violence according to the American Nurses Association (5).
1: Criminal Intent - normally involves theft from the business or employees.
Example: Carol is working on documentation and notices a person lingering in the hallway. Carol doesn’t really think anything of it, assuming they are family members of one of the patients. Several minutes later, the person exits quickly from the supply room and down the stairs. Carol calls security to let them know, but they can’t locate the individual. After looking through the supply room, they find that several containers of wound dressing supplies are missing.
2: Customer/client/patient - the individual becomes violent with employees while receiving services.
Example: David was updating a family on their father’s critical condition. David could tell the family was upset, but the patient’s son seemed more frustrated than the others. During David’s explanation, the son grabbed David’s clipboard and yelled, “You’re not doing anything! You’re just letting him die!” The son then threw the clipboard at David’s head. David blocked the clipboard with his arm, receiving a rather deep cut as a result. Security became involved, and David had to go to the ER for treatment.
3: Worker on worker - an employee bullies, attacks, or threatens another employee.
Example: Emily was rounding when Dr. G. came onto the floor. This doctor was well known for being difficult to work with, and he always required the nurses to stand behind him in the room while he talked with his patients. Emily had one of Dr. G.’s patients today and was in the room, he asked her if the patient had ambulated. Emily told him they had not, but they planned to before and after lunch. The doctor made an audible sigh and while shaking his head at the patient said, “See…this is what I deal with every day. These nurses can’t get anything right. They’re all useless.”
4: Personal relationship - involves a person who has an interpersonal relationship with the nurse, but no association with the nurse’s employer or the business.
Example: Rebecca was walking to her car after work. Halfway to her car, she noticed an individual leaning against the trunk of her vehicle. Rebecca recognized this person as the someone her friend was currently dating. This person approached Rebecca aggressively and began yelling about gossiping and trying to break their relationship. Rebecca started back toward the building, hoping security was nearby, and was pursued by the female. Eventually, Rebecca made it to the building and got inside. Luckily, the door only opened with an employee badge, and Rebecca was safe. She went ahead to security.
Currently, the customer/client type of workplace violence is the most prominent, especially in healthcare and toward nurses. The American Nurses Association (ANA) reports that OSHA does not require employers to implement workplace violence prevention programs, but it supplies voluntary guidelines and may cite employers for not supplying a workplace free from recognized serious hazards.
Some states have legislated that employers develop a program while most states have advanced laws that amend existing statute for assaults of first responders by adding health care providers / nurses and/or increasing the penalty associated with such behavior. (3)
It is worth noting that since there are, in most cases, no actual requirements for employers to provide safe work environments for nurses, preventing and dealing with WPV proves problematic. It falls on nurses to understand what constitutes WPV, how to manage it, how to cope with it, how to report it, and how to ensure action is taken and a resolution is reached when WPV occurs.

Self Quiz
Ask yourself...
- In the scenarios above, should the employees report these incidents to administration at once?
- How would you describe the earlier scenarios on workplace violence?
- Why is it important to ask how you would find and describe workplace violence?
- Can you provide any examples of workplace violence you have experienced or seen?
Epidemiology
Workplace violence can take many forms, and the possible varieties and scenarios are endless. Regardless of how it manifests, the effects of workplace violence are clear and widespread. It can affect productivity of employees, morale, attendance, turnover rates, quality of work, patient outcomes, and much more.
Workplace violence can affect and involve workers, clients, customers, and visitors. WPV ranges from threats and verbal abuse to physical assaults and even homicide. In 2010, the Bureau of Labor Statistics (BLS) data reported healthcare and social aid workers were the victims of approximately 11,370 assaults by persons; a greater than 13% increase over the number of such assaults reported in 2009 (10). Almost 19% of these assaults occurred in nursing and residential care facilities alone. Unfortunately, many more incidents probably go unreported (5).

Impact on Nurses Well-Being
Workplace violence can take a heavy toll on nurses. These tolls can be emotional, mental, and physical as well as short-term or long-term. The seriousness of these injuries can vary widely ranging from minor upset to permanent injury and in worst cases, even death. (13)
This harm doesn’t stop with the nurse. The effects of workplace violence may also include effects spanning the unit the nurse works on or even the entire facility. Low morale, reduced productivity, lack of trust in employers, and fear of going to work can be results of violent events occurring to even a single co-worker.
Workplace violence can also have a financial effect on nurses and their employers related to lost time at work from injury or callouts, costs of care for treatment related to the incident (physical and/or psychological), or even legal fees. (13)
Given that incidents of workplace violence are rapidly increasing, these impacts are expected to increase as well. It is easy to see how this harm is widespread and can potentially ripple outward into the nurse’s professional and personal life. The stress and harm do not stay at work, and can spread to the nurse’s family, social interactions, and more.

Self Quiz
Ask yourself...
- How far reaching do you think workplace violence is?
- Can you give some examples of how workplace violence has affected you or your co-workers?
- What are some examples of how workplace violence against someone else can affect you or the patients on your unit?
Barriers to Reporting
One way to combat workplace violence is knowledge of its existence, its nature, and its frequency. Unfortunately, there are many factors that either prevent or discourage nurses from coming forward with reports when they are the victims of WPV.
A study presented in a Chinese nursing journal surveyed 325 nurses. Of these nurses, 266 were spread across 165 hospitals, and these hospitals were in 72 cities.
A total of 172 nurses (64.7%) experienced violent incidents during the past year. Of these incidents, 45.5% were reported; and the reporting rate of physical assaults (69.0%) was higher than those of verbal abuse (36.9%), threatening behavior (51.7%), and sexual harassment (60.0%). Formal reporting accounted for 25.4% (15.4% in written form and 10.0% through a computer-assisted reporting system.
Almost half of the nurses (49.6%) said that the hospital had no reporting system, or they were uncertain about the reporting system. For reasons of not reporting, 51.9% of the nurses were unaware of how and what types of violence to report, and 50.6% of the nurses believed that the hospital paid greater attention to patients rather than staff. (7)
Interestingly, almost fifty percent of the nurses surveyed had limited knowledge, if any, of a reporting system available to them, while fifty percent felt the hospital favored the patients over their own employees. Combined with an actual or perceived lack of supervisory support, this encourages an environment where nurses feel powerless to protect themselves or to take proper action when threatened or harmed.
The Minnesota Nurses Association, in August of 2022, published a press release with the results of a nursing survey on the topic of workplace violence. In this survey, ninety-seven percent of the nurses surveyed observed WPV or harassment over the previous two years.
The top reasons cited by nurses who did not report workplace violence were lack of time due to overwork and under-staffing, cited by fifty-eight percent of respondents, and lack of action by hospital management, cited by fifty-three percent of nurses in the survey. (4)
It would appear from these studies that many nurses feel it is futile to report incidents of workplace violence they encounter, and even if they realized an incident was reportable, they may not be aware of a way to report it or have time to do it. This perceived powerlessness and sense of futility in the face of abuse and violence will only continue to worsen unless action is taken to remove barriers to reporting and for nurses to have access to aid and support for supervisory staff.

Self Quiz
Ask yourself...
- Can you think of any examples of when you or a co-worker tried to report an incident of workplace violence and were unable to?
- If so, what was the barrier that prevented you from reporting?
- Can you name three alternative ways to report workplace violence at your organization?
Culture of Safety
A commonly used phrase is “Culture of Safety”, but is there a standardized definition of what it is or could be? Many resources point to the safety of patients about medical errors, patient rights, and protecting the patient’s information, but few address the issue facing caregivers and especially nurses. However, there is no agreed-upon or standard definition of what exactly a “culture of safety” is or what it should look like.
The American Nurses Association approaches the concept by saying, “Establishing a culture of safety in health care is essential to the security and well-being of your patients, staff, and organization. Effective nurse leaders embrace safety protocols that ensure their organization delivers a secure, protective environment that prioritizes patients and caregivers.” (12)
Currently, there is only a single federal legislation in place about the issue.
The only federal regulation currently in place is the General Duty Clause of the Occupational Safety and Health Act of 1970. This clause requires employers to supply a work environment free from recognized hazards that are causing or likely to cause death or serious physical harm. However, the general duty clause offers no specific recommendations about management of workplace violence.
The Occupational Safety and Health Administration (OSHA) issued guidelines for workplace violence prevention for health care and social service workers. First issued in 1996 and later updated, the guidelines are only advisory. (1)
It is paramount that nurses and other direct care providers accept the responsibility of creating policies and procedures within their organizations to define and enforce a work environment where violence is not tolerated and dealt with accordingly.
There is currently a small body of research and work of the effects workplace violence has on nurses as human beings. Most of the evidence focuses on how workplace violence increases the risk nurses present to patients in the form of medical errors, staffing issues due to missed work, poor documentation, etc.
The main body of evidence discussing how workplace violence affects nurses is noted in research around nurse burnout. A 2020 study published by the National Health Institute (10) states, “Workplace aggression is a source of extreme socio-emotional stress, which may lead to the experience of psychological strain.
A large body of research shows that exposure to workplace aggression and violence may severely impair healthcare workers’ mental health, including symptoms of post-traumatic stress disorder, depression, and burnout.”
This study also shows an important association with workplace aggression and violence targeting nurses and drastically increased levels of emotional exhaustion, depersonalization, and deep feelings of poor personal accomplishment. Over time, these feelings lead to complete burnout, and even worse, possibly psychological and/or physical conditions in the nurse affected.
Even with this preliminary information and research, we still have a long way to go to show the full and far-reaching effects of workplace violence on nurses. Again, by being proactive and acting now, we as nurses can foster this research and bring to light the issues so they can be addressed.

Self Quiz
Ask yourself...
- How does your organization define a “culture of safety”?
- Do you agree with the definition?
- How would you define a “culture of safety” from your own perspective given your experiences and challenges?
ANA Zero Tolerance Policy
In 2019 the American Nurses Association (ANA) (2) release a brief titled “Reporting Incidents of Workplace Violence”. In it, they discussed several issues surrounding workplace violence, barriers to its reporting, and made recommendations to healthcare organizations on strategies relating to the issues of workplace violence.
They also set forth a “Zero Tolerance Policy on Workplace Violence”, which provided some definitions and several recommendations on how to deal with WPV.
The introduction to the “Culture of Safety” part of this brief is as follows:
By prioritizing, developing, and sustaining an organizational culture focused on safety, we can drive the future of healthcare to a place where patients and those who care for them are free from harm. It is not only one of many priorities but is the overriding ethical imperatives for all leaders. (9)
The ANA also suggested a three-level prevention strategy, each with a part for the employer and the employee. Essentially, the role of the employer is gathering data, providing a “safe” work environment, non-punitive reporting, and development of programs to provide a safe work environment for nurses. The employee’s role is to take part in the implementation and evaluation of said programs.
Unfortunately, these are only suggestions and employers do not have to implement any programs or services to protect employees against workplace violence. Also, healthcare employers do not have to report any incidents to JCAHO who consider events of workplace violence to be “sentinel events”.
In the end, it falls on the nurses and employees directly affected by WPV to assume the charge against workplace violence, hold employers accountable, communicate with local and state legislators, and effect change to protect themselves.

Self Quiz
Ask yourself...
- Considering the recommendations and guidelines set forth by these entities, do you think they are adequate or effective? Why nor why not?
- How has this information changed your perception of the overall reporting process on workplace violence against nurses?
- What generalizations can you make from this information on the reporting process from an employer perspective?
Strategies to Prevent Workplace Violence
To end nurse abuse for good, Boston-Leary says it takes every nurse speaking up and reporting abuse within an organizational culture that has an established process for allowing nurses to report abuse without fear of recrimination and then follows up with a resolution. (8)
There are some suggested actions to help prevent and combat workplace violence in your practice setting. These actions include:
Know the definition of abuse.
The National Institute for Occupational Safety and Health (NIOSH) defines workplace violence as “the act or threat of violence, ranging from verbal abuse to physical assaults directed toward persons at work or on duty.”
Agreeing on this definition is an important first step to achieving widespread acknowledgement of the distinct types of nurse abuse, particularly non-physical abuse, Boston-Leary explains. (8)
Report Abuse
Ask about how your workplace manages abuse reporting, whether it is in your current workplace or when you are applying for a position, Boston-Leary suggests. “Ask about how reporting abuse happens during any shift because there should be a reporting mechanism in place for everyone, even if it’s on a weekend or evening shift with no manager easily accessible to report to.”
If (when) you do experience abuse, it’s essential that you speak up immediately and note any witnesses who could corroborate your description of the incident, she says.
Even after you experience abuse and even if you didn’t report it, it’s important to share your past abuse with others to empower them to report abuse they experience. (8)
Change Your Culture
Join or meet a committee to build or strengthen zero-tolerance abuse policies. Based on ANA’s Zero Tolerance Policy on Workplace Violence, Boston-Leary suggests these crucial elements of a zero-tolerance abuse program:
Stop violence before it starts through education to find risks and reduce vulnerabilities for workplace violence.
Create an effective response to violence immediately after it occurs, including emergency care.
Establish long-term responses that reduce the long-term negative effects of workplace abuse. (8)
Communicate with your Legislator!
Congress was considering legislation to #End Nurse Abuse by passing The Workplace Violence Prevention for Health Care and Social Service Workers Act (H.R 1195). If approved, this law would have required health care and social service industry employers to develop and implement a comprehensive workplace violence prevention plan that protects nurses and other healthcare professionals from on-the-job abuse.
Boston-Leary believes legislators are very attuned to the trusted voice of nurses to share about what is happening in health care today (8).

Self Quiz
Ask yourself...
- What is your organization’s primary method of reporting abuse or violence against employees?
- Do you know who your local and state legislators are and how to contact them?
- Are you aware of any committees or groups within your organization that actively address the issue of workplace violence?
Nurse-led Strategies
You can join these committees or work with your employer to create them. Collaborating with your supervisory staff and HR, you can create workflows, policies, reporting methods, and provide education on prevention of workplace violence and make a difference in your overall work environment.
Regarding Your Legislators
As mentioned before, 2021 Congress was considering federal legislation to end nurse abuse by passing The Workplace Violence Prevention for Health Care and Social Service Workers Act (H.R. 1195). The bill was passed by the House on April 16, 2021, but was never passed by the Senate.
You can find your local and state legislator contact information very easily on the internet. A simple search for “how to find state legislator contact information” is a wonderful place to start. As a voting citizen, you have every right to contact them, and demand laws be created to protect you while you work.
Below are some links to help you find elected officials:
- https://www.usa.gov/elected-officials
- https://www.usa.gov/state-governor
- https://www.senate.gov/senators/senators-contact.htm
- https://www.house.gov/representatives/find-your-representative
Advocate for your own safety the same way you would for your patients!
As nurses we aren’t afraid of stepping up to bat for our patients when they need something, but we are notorious for taking a hit and letting it slide, sometimes even to our own detriment.
We owe it to ourselves to offer that same level of advocacy to ourselves and our co-workers.
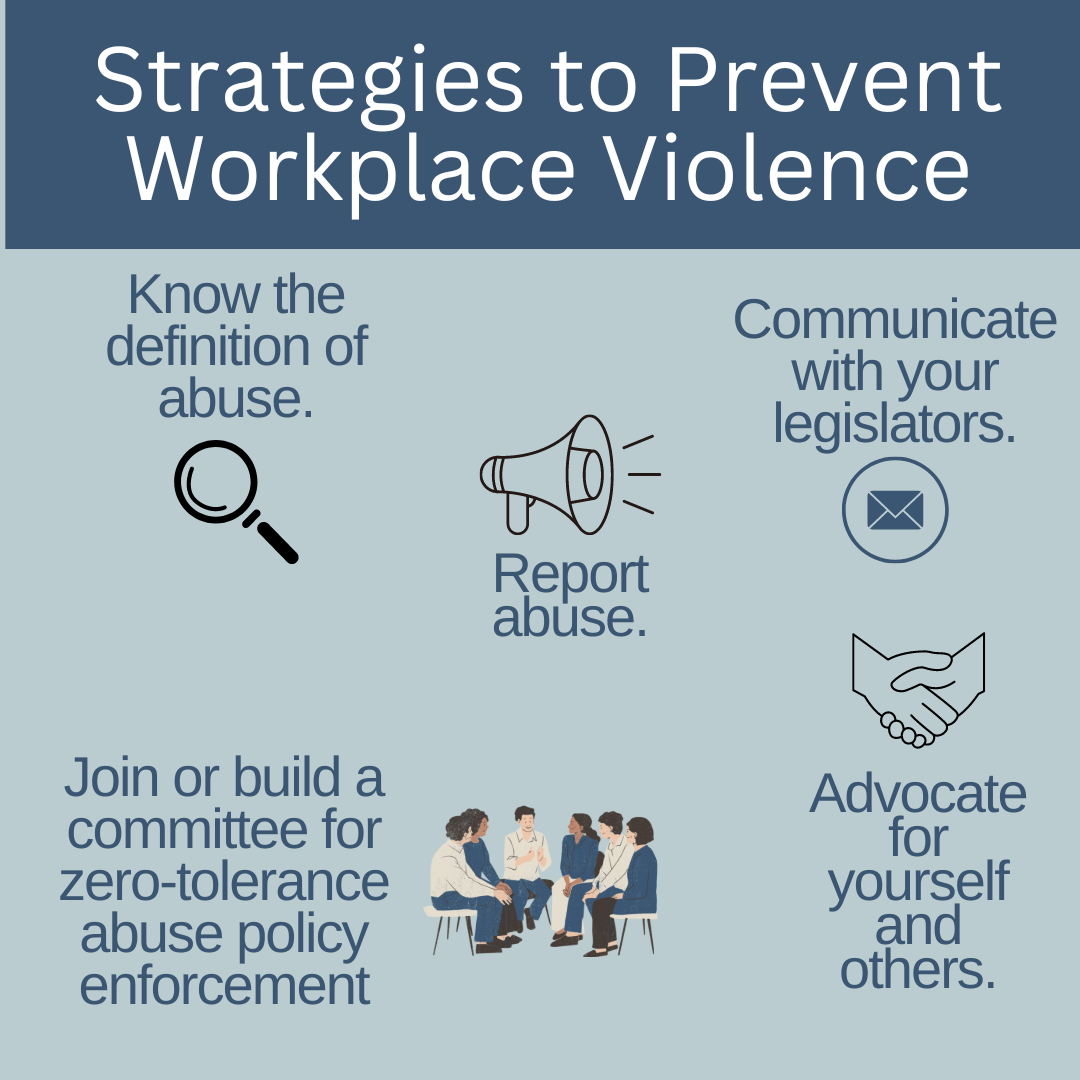

Self Quiz
Ask yourself...
- How can you become an advocate for yourself or your co-workers when it comes to workplace violence?
- Who is the contact in your organization for instances of workplace violence?
Resources
The Joint Commission supplies resources available to report and learn about how to report workplace violence. The links included are for federal, state, professional, and other resources. The direct link to this page is:
The Joint Commission: Workplace Violence Prevention Resources
Local law enforcement
As a private citizen, you are protected by laws about assault, battery, and other attacks on your person. You are within your rights to call the police on events of workplace violence, especially if your life or health are threatened, or you are physically attacked. It is likely your employer will not support you in this situation due to legal implications. It is best to ask your HR department and supervisory staff how these situations should be managed if they occur.
Legal Counsel
Consult with a lawyer about your legal rights in situations on workplace violence and how to best manage them. Be sure to bring scenarios, information on how your employer suggests dealing with these situations, and examples of violence you have seen or have experienced.
Educate and Train Yourself
Learn as much as you can about recognizing and managing workplace violence. Your employer may supply these courses, and if they don’t, it may be prudent to request them. Also, you can seek outside education and training on these topics including self-defense classes and crisis management courses.
Practice Self-Awareness
We all have inherent beliefs, perspectives, and feelings that can prevent us from acting in certain situations. Knowing yourself and understanding possible nuances within yourself that could be a detriment to you appropriately handling a situation of workplace violence could mean the difference between prevention and becoming a victim.

Self Quiz
Ask yourself...
- What training opportunities does your organization provide on management and follow-up for workplace violence?
- What information would you ask local law enforcement or a legal counsel for on workplace violence?
- What might someone who believes abuse against nurses is “just part of the job” do when they find themselves a victim of workplace violence?
- What can you do to help individuals that may simply allow workplace violence to affect their well-being?
Conclusion
Being an agent of change can be intimidating, terrifying, and even force us to deal with feelings and beliefs we didn’t even realize were in our way. Incidents of WPV have been rising sharply over the past several years, and there is no sign of slowing. It’s up to us as front-line workers, nurses, and co-workers to take responsibility for our own safety and work environment.
Through cooperation and consistency, we can create and bring solutions to the workplace and hopefully one day, aid in the creation of laws that make our jobs safer for us to supply the care and support our patients need. We owe it to ourselves to take the necessary steps to show our employers it’s time to address this issue. “Be the change you wish to see in the world.” ~Mahatma Gandhi –
West Virginia Drug Diversion
In 2018, West Virginia had not only the highest opioid-related death rate in the nation, but also the highest synthetic opioid-related death rate (46). In 2019, West Virginia ranked in the top 10 for opioid dispensing rates, with a rate of 59.4 per 100 persons being prescribed an opioid (10), which is well above the national average of 46.7 per 100 (9). While this number has consistently decreased since 2006, the numbers of individuals in West Virginia affected by addiction and overdose remains high (30).
Introduction
The opioid crisis in the United States continues to affect millions of individuals. The American Psychiatric Association (APA) estimates nearly one in three Americans know someone who either is or has been addicted (1). The Centers for Disease Control (CDC) identified that in 2017, there were 70,237 overdose deaths, and in 2018, there were 67,367 (46). In both 2017 and 2018, nearly two-thirds of these involved an opioid (46). Currently, it is estimated 128 people die per day from an opioid overdose (8). The National Institute on Drug Abuse (NIDA) identifies misunderstandings and misconceptions about addiction of prescription opioids, held by pharmaceutical companies and health care providers in the 1990s, led to an increase in their use and subsequent rise in misuse and addiction (8, 31). Following this in 2010, deaths related to heroin began to rise quickly, and in 2013, deaths associated with synthetic opioids, like illicitly manufactured fentanyl, began to increase (8).
The impact of opioid misuse and addiction is devastating to families. It can lead to job loss, relationship difficulties, inability to care for children, and death. Families who have a loved one struggling with opioid addiction may feel at a loss regarding handling or supporting their loved one, putting additional stress on the family unit. Arrest, conviction, hospitalization, and even death of a parent from opioid addiction, often place children in the care of the child welfare, further straining the system. Not only does the use of opioids impact individuals and families, but it puts additional strain on both state and national economies. It is estimated that misuse of prescription opioids costs the United States $7.5 billion per year (31).
In 2018, the West Virginia Department of Health and Human Resources introduced an opioid response plan, which addressed prevention, early identification, treatment, overdose reversal, family support, and recovery (43). Recommendations of the plan include expanded treatment for neonatal abstinence syndrome (NAS), improved access to treatment, improved overdose reporting, improved access to naloxone, addressing issues with pain management and prescribing practices, expanded licensing for medication-assisted treatment programs, and it created the Opioid Reduction Act (43). It is important to discuss The Opioid Reduction Act of 2018 in this West Virginia Drug Diversion course as it requires health care providers to prescribe the lowest effective dose and limits opioid prescriptions to a four-day supply for an emergent or urgent care, a three-day supply for minor surgery or procedure, a three-day supply for dentist or optometrist, and a seven-day supply for patients seen by their primary physician or at discharge from a hospital (34).
While West Virginia has taken steps to address the opioid crisis, more work is needed to meet the need of patients, families, and health care workers. Health care providers who are not specifically trained to treat substance use disorders may struggle when working with patients who suffer from addiction, as there are often knowledge gaps related to these patients’ care. Gaps exist related to fully understanding the broad spectrum of a substance use disorder and in the identification of at-risk populations. Additionally, stereotypes about addicts still exist, which can inhibit health care providers from properly identifying and developing treatment plans for these patients.
Many patients with substance use disorders are often able to hide their addiction from loved ones and providers for a period of time, which further complicates timely identification and intervention. Health care providers prescribing opioids and other medications that are high-risk for abuse should perform not only regular screening of at-risk patients, but also explore alternative methods for treating chronic pain. In an effort to address these concerns, the West Virginia Board of Nursing requires annual education for nurses who prescribe, administer, or dispense controlled substances (45). This course will address issues concerning the opioid crisis, including best practices for prescribing controlled substances, managing patients who divert, behaviors associated with drug seeking and substance use disorders, providing patient education on opioid use, storage, disposal, and reversal agents, as well as use of the West Virginia Controlled Substance Automated Prescription Program (CSAPP).
Epidemiology of Pain and Substance Use Disorder
Pain
Pain is a complex problem. Because of the personal nature and the varying pain experiences of the patient, it is often difficult to adequately treat. When pain goes unrelieved, the potential of it impacting the patient’s life negatively increases. Untreated pain can result in increased stress on the body, increased healing time after injury or surgery, decreased immune response, feelings of anxiety or depression, and alterations in performing activities of daily living. The effect of this can also be long-reaching as untreated pain can result in a decrease in work performance and job loss for some patients.
Acute or Chronic
For this West Virginia Drug Diversion course, it is necessary to outline that pain can be classified as either acute or chronic. Acute pain is often associated with injury, inflammation, ischemia, or surgery and typically only lasts for a short while. Patients experiencing acute pain are often able to easily localize the pain. Acute pain that is not adequately treated can progress to chronic pain. One example of this is seen in musculoskeletal injuries, such as back strain, where repeated injury and inadequate pain management progress to a state of chronic pain.
Chronic pain usually lasts more than three months. Unlike acute pain, chronic pain often is not as well defined, the onset is typically gradual and characteristics of the pain can change over time. While some chronic pain can be tied to a specific cause or disease state, such as arthritis or cancer, other times, the exact cause is not as easy to determine.
Nociceptive and Neuropathic
Pain can be further categorized into nociceptive and neuropathic pain. Nociceptive pain is a result of normal stimuli, and it is further identified as either somatic or visceral pain. Somatic pain is superficial and involves skin, muscles, bone, blood vessels, and connective tissues. An example of acute somatic pain would be a sprained ankle and an example of chronic somatic pain would be arthritis. Visceral pain refers specifically to pain in the organs. An example of acute visceral pain is seen in cardiac ischemia, which is often described as chest pain or left arm and jaw pain in patients experiencing a myocardial infarction (MI). An example of chronic visceral pain would be abdominal pain secondary to stomach cancer.
Neuropathic pain results from damage to either the central or peripheral nervous system. While most cases of neuropathic pain are chronic, acute neuropathic pain can be seen in injuries or infections affecting the nerves. In some cases, acute neuropathic pain, such as what is seen in amputations, may come and go with the severity of the pain differing greatly from patient to patient. Acute neuropathic pain may progress to chronic neuropathic pain if not treated effectively. Additionally, other disease states may cause chronic neuropathic pain, such as what is seen in diabetic neuropathy. Chronic neuropathic pain is often difficult to treat, and patients may be prescribed several medications before finding something that provides some pain relief.
Pain Assessment
There are various factors affecting how pain is perceived and managed. These factors include the type of pain, how long the pain has been occurring, patient age, cognitive level of the patient, the patient’s personality or temperament, previous experiences with pain, and even cultural beliefs. Understanding how these factors influence the patient’s response can help to inform the assessment and may be helpful in determining appropriate treatments for the pain.
A comprehensive assessment of the pain is also important in determining the type of pain. A thorough assessment at the start of treatment will also serve as a baseline and help to determine if interventions have been effective. Additionally, patients who are not adequately assessed for pain are at a higher-risk of their pain not being effectively managed. It is important to remember not all patients are capable of describing their pain, and as such completing a pain assessment can help these patients to provide the information necessary for informed diagnosis and treatment. How a pain assessment is obtained may also vary. While traditionally, a pain assessment is completed as part of the general assessment, use of a paper or electronic form completed by the patient prior to evaluation may also be used. For this West Virginia Drug Diversion course, it is vital to thoroughly read through the “Pain Assessment Components” table below.
|
Pain Assessment Components |
||
| Location |
|
Identify if it is superficial (near the skin) or deep (visceral) pain. This assessment may also include the use of a diagram or pictures. |
| Intensity |
|
A valid pain assessment tool should be used. For most adults a numerical rating scale (0-10) is often used. Health care providers should also explore the use of alternate scales if the patient is not able to understand or provide a number. Use of the Wong-Baker Faces scale, verbal descriptor scales, or visual descriptor scales are acceptable alternatives. |
| Quality |
|
Use of descriptors, such as stabbing, sharp, or burning will help the patient to describe what they are feeling. Presence of radiating pain may also help in diagnosing underlying conditions that may be contributing to the pain. |
| Onset and Duration |
|
Identify if it is an acute or chronic problem. Chronic pain may be constant, as is seen in some cancers, or it may be episodic, as is seen in migraines. Understanding this can better inform treatment options |
| Aggravating and Alleviating Factors |
|
Identify what medications and non-pharmacological approaches the patient has already tried. If certain positions or activities affect the pain this may also help in diagnosis and treatment. |
| Effect on Function and Quality of Life |
|
This information will be helpful in determining if interventions have been effective. As depression is also impacted by chronic pain, patient reports of isolation or inability to be with friends and family may also indicate the need for a behavioral health referral. |

Self Quiz
Ask yourself...
-
Why is the type of pain important to consider, prior to a patient being prescribed opioid therapy?
-
Why is obtaining a comprehensive pain assessment important?
Substance Use Disorder
The National Survey on Drug Use and Health found in 2017, 19.7 million Americans over the age of 12 suffered from a substance use disorder, and 11.4 million people had misused opioids (6). This same study found 62.6% of participants identified the initial reason they misused a prescription pain reliever was to relieve pain (6). Addiction costs related to productivity, health care, and legal care totaled over $7 billion annually by 2017 (6). These statistics are staggering and show why early intervention to identify at risk individuals and to prevent severe substance use disorders is necessary.
There is a drastic difference between substance use and addiction, which is more accurately called substance use disorder. Not every patient who uses a controlled substance develops a substance use disorder. However, risk factors may predispose some patients to develop one. There is an increased risk for the development of a substance use disorder in patients who have family members who also suffer from a substance use disorder or a mental health disorder (41). Additionally, how the drug acts within the body and brain and stress will increase the risk of developing a substance use disorder, even when the medication is taken as prescribed (41).
The NIDA defines misuse (abuse) as the action of taking medication other than prescribed, either for purpose or dose, taking another person’s prescription, or taking a medication to get high (27). Misuse, by itself, may not necessarily indicate an addiction as other factors need to be considered. Patients may misuse a wide variety of prescription medications without incident; however, when misuse of medication is common, the risk of it occurring with medications that are addictive or controlled is higher. In patients who make a choice to misuse medications regularly, the ability to control their own behavior decreases (29). NIDA defines addiction as a chronic condition, where patients may have periods of relapse, will compulsively seek out drugs, and continue to use, despite the harmful effects and long-lasting changes it may have on the brain; it is considered both a complex brain disorder and a mental illness (29).
Diagnosis of Substance Use Disorders
The process of developing a substance use disorder occurs on a continuum. The majority of patients who take a couple of doses of an opioid to treat acute pain, such as seen in post-surgical patients, will not become addicted. The risk for addiction increases when the patient is at higher risk due to genetics or psychological factors (41). Exposure to a substance changes how the brain responds, leading to intoxication (2). When a patient repeatedly uses the substance, they build up a tolerance, which then requires the patient to use more of the substance to achieve the same feeling. Over time, even patients who use a substance as prescribed can develop a tolerance. This is often seen in patients who suffer from chronic pain and use opioid medications for pain management. While increased tolerance can be an indicator of addiction, this alone does not equate to a diagnosis of addiction or a substance use disorder.
The Diagnostic and Statistical Manual of Mental Disorders: Version 5 (DSM-5) categorizes substance use disorder symptoms into four categories, impaired control, social problems, risky use, and physical dependence (20). Understanding the DSM-5 categorizations will further help you not only in this West Virginia Drug Diversion course, but also in identifying signs and symptoms of substance use disorders in patients.
Impaired Control
- Cannot control the use of the substance
- Unable to cut down or stop using
- Spends time obtaining, using, or withdrawing from substance
- Reports craving the substance (20)
Social Problems
- Unable to meet obligations of work, home, or school
- Continues use of a substance even though it causes social or interpersonal problems
- Is no longer as active in social, work, or recreational activities (20)
Risky Use
- The substance is used in dangerous situations, such as when driving
- Continues using the substance even though it is making a medical or psychological problem worse (20)
Physical Symptoms
- Displays evidence of tolerance
- Has symptoms of withdrawal when the substance is stopped or counteracted (20)
If a patient has more than two positive symptoms in a 12-month period, they should be diagnosed with a substance use disorder (20). The severity of the disorder is further determined by the number of criteria or symptoms present, with mild being two-to-three, moderate four-to-five, and severe addiction being greater than six (20).

Self Quiz
Ask yourself...
-
How prevalent is substance abuse, in the U.S.?
-
How does abuse differ from addiction?
-
What risk factors predispose a patient to developing a substance use disorder?
Opioids
Indications and Action
Opioid analgesics can be used to manage pain, used as anesthesia adjuncts in surgery, and as a cough suppressant. Opioid analgesics work by binding to specific opiate receptors (mu, delta, and kappa). Opiate receptors can be found in the central nervous system, peripheral tissues, and in the gastrointestinal (GI) tract. Opiate receptors also help to control blood pressure, pupil dilation, GI secretions, respiration, and pain response (19). When opioids are used to manage pain, they act upon these same opiate receptors, resulting in a decrease in pain and affecting the control these receptors have on other systems, resulting in some of the effects experienced by patients when taking opioids.
The most prescribed opioids include hydrocodone, oxycodone, oxymorphone, morphine, codeine, fentanyl, hydromorphone, tapentadol, and methadone (7). Administration routes vary based upon the type of opioid prescribed.
In determining which route should be used, consideration should be given to the type of medication, what type of pain is being treated, as well as the age and cognitive level of the patient. Common routes for home use include oral (both tablet and liquid), buccal, sublingual, intranasal, topical, and transdermal. Rectal routes may be used for pediatric patients or for those who are unable to tolerate oral ingestion. Opioid treatment in hospitals or clinics may also include intravenous (IV) injection, subcutaneous injection, and intrathecal. Patients prescribed opioid medications should receive medication education that includes administration and adverse effects and general education about safety, storage, and disposal.
The Controlled Substances Act identifies scheduled medications based upon their current acceptable medical use, abuse potential, and risk of dependence (38).
Examples of scheduled substances:
Schedule I: Heroin
Schedule I substances have a high abuse potential and are not currently considered to be acceptable for medical use (38)
Schedule II: Hydromorphone, oxycodone, morphine, methadone, and fentanyl
Schedule II substances can be prescribed but are high risk for abuse (38).
Schedule III: acetaminophen with codeine, as these products contain less than 90mg of codeine per dose
Schedule IV: Tramadol
Schedule V: Antidiarrheal diphenoxylate/atropine and cough suppressants containing less than 200 mg/100 ml of codeine
They have the lowest potential for abuse.
Contraindications and Precautions
Use of opioid analgesics should be used cautiously in patients with conditions resulting in respiratory insufficiency, morbid obesity, and pregnancy. Additional assessment and risk analysis should be performed prior to prescribing or administering opioid analgesics to patients with a diagnosed substance abuse disorder, concurrent psychiatric illness, and those taking benzodiazepines. Concurrent use of opioids and benzodiazepines should only occur if no other treatment options are available due to the increased risk of respiratory depression. Patients taking tramadol, meperidine, or fentanyl are at an increased risk for the development of serotonin syndrome when these drugs are taken with other medications that affect serotonin, and care should be taken when these medications are prescribed concurrently (36).
Adverse Effects
Adverse effects of opioids range from mild to severe, and most patients who are prescribed opioids will experience one or more effects. Common adverse effects include:
- nausea
- vomiting
- constipation
- urinary retention
- urticaria
- lightheadedness
- sedation (19)
With the exception of constipation, which can be an ongoing effect, many of the common adverse effects such as nausea, vomiting, and urticaria often lessen in severity with continued use. More serious adverse effects, which may occur even with continued use, include hypotension, bradycardia, and respiratory depression. Patients should be prescribed the shortest-acting, lowest effective dose to minimize severe adverse effects (14).
Toxicity
Opioid toxicity can occur regardless of the route of administration. Patients presenting with opioid toxicity often have CNS depression, ranging from confusion and drowsiness to unresponsiveness. Other symptoms of toxicity include respiratory depression and pupil constriction. Patients may initially present with hypotension, but as CNS and respiratory depression worsen, hypertension may be seen as the body attempts to compensate. Patients should be monitored for seizure activity if the overdose is a result of meperidine.
It is important to note in this West Virginia Drug Diversion course that treatment of opioid toxicity should begin immediately with the administration of naloxone. Repeat dosing may need to be administered as naloxone has a half-life of 30-60 minutes. Pre-hospital treatment with nasal or injectable naloxone should be administered, even if unsure of overdose or toxicity. In-hospital treatment should consider not only the patient’s condition but also the half-life of the opioid (if known), and the naloxone dose should be titrated based upon these factors to limit the potential adverse effects of naloxone (22). One option for treatment is continuous IV infusion as opposed to repeated larger bolus doses. The use of a continuous IV infusion has been shown to decrease the symptoms of opioid withdrawal better than bolus dosing (22).

Self Quiz
Ask yourself...
-
What underlying health conditions should the patient be evaluated for, prior to being prescribed opioid therapy?
-
What education should be provided to patients regarding the adverse effects of opioids?
-
What information should be communicated to patients and their family members so early intervention for opioid toxicity can be initiated?
Pain Management Using Opioids
Assessment
Patient assessment is an important factor in determining the need for opioid therapy. Assessment of all patients should start with a full history and physical, including a complete pain assessment as well as any previous episodes of pain and treatments used (15). A thorough social and psychological assessment should also be completed. A social assessment should explore how the patient functions at home, work, and socially while including a discussion of how the current pain impacts their ability to function (15). A psychological assessment should include a previous history of substance use disorder and substance use as well as any underlying mental health disorders and medications currently being used to treat these (4).
For patients with a history of substance abuse disorders, the initial assessment should further explore the substance use disorder. The history should include the type and number of opioids used recently, routes of administration, date of last use, any treatment the patient received, and physical, social, or psychological problems experienced as a result of the disorder (4).
Patients should be screened for infectious diseases such as hepatitis B and C, human immunodeficiency virus (HIV), and tuberculosis (TB) (4). If the patient has a history of IV drug use, follow-up should include infections related to IV use, such as infective endocarditis, osteomyelitis, and abscesses (4). As opioid misuse and alcohol abuse often occur concurrently, questions related to alcohol use, frequency, and the amount should be addressed (47).
During the physical assessment, the health care provider should also look specifically for signs and symptoms of opioid intoxication or withdrawal, as well as any physical symptoms related to long term substance abuse. Patients with a history of opioid use may have alterations in hematology, and in patients with chronic use, diet changes may result in anemia. In patients with a history of substance abuse, a baseline laboratory analysis of a complete blood count (CBC) and liver function test are recommended, as well as testing to determine the presence of TB, hepatitis B and C, HIV, and other sexually transmitted diseases (4).
| Intoxication | Withdrawal | Symptoms of Chronic Use |
|
|
|
Addiction Risk Assessment
In addition to the history and physical exam, the use of an addiction risk assessment tool can be helpful in determining the risk of misuse or addiction in patients prescribed opioids for chronic pain (15). There are several addiction risk assessment tools available, but these tools vary in complexity as well as the specific criteria being measured.
It is important when using a screening tool to determine the risk of misuse or addiction that healthcare providers recognize a “one size fits all” approach does not work. The type of assessment used may need to vary based upon the patient and their history. For patients with a complex history of a substance use disorder, a more complex and complete assessment should be used, whereas a patient without risk factors may only need a basic risk assessment. Availability, ease of access, and target patient age may also play a part in the type of tool chosen. Several tools are readily available through the NIDA website and can be downloaded by health care providers. Having two or three tools available that health care providers have been trained to use and are comfortable using allows for improved assessment and ability to better identify at risk individuals.
Finding a patient is high-risk can be scary for both the healthcare provider and the patient as the goal of treatment is not to create an additional problem. However, the risk assessment does not mean the patient’s pain should not be treated. Evaluating alternative treatment methods is important, and opioids or other controlled substances should not be a first line option. Additional support will need to be provided to this patient through referrals to both a pain and behavioral health specialist to ensure the needs of the patient are being met and their pain is being adequately treated.

Self Quiz
Ask yourself...
-
What assessments need to be completed prior to prescribing opioids to a patient?
-
Why is performing a risk assessment on all patients necessary?
-
What steps should be taken if the risk assessment indicates a patient has a high risk of developing a substance abuse?
Treatment Options and Goals
While acute pain can be treated with opioid medications, considerations should be made regarding the severity of the pain, diagnosis, and the effect of the pain on the ability of the patient to function (14). If the patient can tolerate the pain and there is minimal impact on their ability to function, non-pharmacological and non-opioid medications should be used before determining an opioid is necessary. Additionally, steps should be taken to evaluate and treat underlying causes of pain. In cases where the acute pain is severe and impairs patient function, steps should be taken to ensure the patient is prescribed the lowest possible dose of an immediate-release opioid, ideally with only a three-to-five-day supply (14).
Non-pharmacological Pain Management
Options for non-pharmacological pain management and their effectiveness will vary based on the patient and the nature of their pain. When determining which methods will work for the patient, healthcare providers should discuss options with the patient and provide education about how it can be used, as well as the benefits for using a particular therapy. Healthcare providers after reading this West Virginia Drug Diversion course should also evaluate potential costs and the barriers to using these therapies. Follow-up is necessary in determining the effectiveness of the therapy and if further treatment is necessary.
|
Sample of Non-Pharmacological Pain Management Modalities |
|
|
Modality |
Barriers to Use |
|
Heat/cold therapy |
Education – patient should be provided instruction on proper use to avoid injury |
|
Relaxation (music, imagery, meditation) |
Education |
|
Low impact exercise (yoga, tai chi) |
Ability to perform, potential costs associated with gym membership or training center |
|
Acupuncture |
Access to licensed acupuncturist, cost if not covered by insurance |
|
Massage therapy |
Cost may be prohibitive, not covered by all insurances, may require a prescription if the service is able to be covered |
|
Chiropractic services |
Cost if not covered by insurance, access may be limited in some areas |
|
Physical or Occupational Therapy |
Access if the patient lives in a rural area, cost |
|
*This list is only a representative sample of some non-pharmacological modalities for pain management. Other options exist and may also be considered when developing a treatment plan. |
|
Non-opioid Pain Management
The use of non-opioid medications for pain management should be carefully considered prior to implementation. These medications should be evaluated based upon the need for short-term or long-term therapy. For some medications, the risk of complications when taken concurrently with opioids is high, so patient evaluation and screening are key in determining the current use of opioids. The patient should be monitored for therapeutic effectiveness as well as potential side effects. Additionally, some non-opioid options carry their own risk of addiction and patients should be monitored for substance use disorders related to these.
|
Sample of Non-opioid Options for Pain Management |
||
|
Classification |
Examples |
Considerations |
| Nonsteroidal anti-inflammatory drugs (NSAIDs) | Ibuprofen, diclofenac, naproxen, celecoxib, aspirin (often found in combination medications) |
|
| Acetaminophen |
|
|
| Muscle Relaxants | Cyclobenzaprine, carisoprodol, tizanidine |
|
| Antidepressants |
Tricyclics – amitriptyline, nortriptyline SNRIs** – duloxetine, venlafaxine SSRIs*** – paroxetine, fluoxetine |
|
| Anticonvulsants | Carbamepazine, pregabalin, gabapentin, lamotrigine |
|
| Cannabis |
|
|
|
*This list only identifies a select number of non-opioid medications used when managing pain. Other available medications, patient history, etiology of pain, and patient function should be considered prior to prescribing. **SNRIs are serotonin and norepinephrine reuptake inhibitors ***SSRIs are selective serotonin reuptake inhibitors |
||
Evaluation of the type and nature of the pain is important in determining which options would best fit the patient’s needs. Healthcare providers will need to discuss with the patient the possibility of having to try different modalities and medications to find a fit that is right for them. Patient tracking of symptoms, use of relief methods and medications, the effect on the ability to function, and effectiveness of interventions is key in determining which modalities and medications are working. Various mobile apps for tracking and managing pain are available and may be an option for helping some patients to record and track this data.
In the event the patient and healthcare provider determine non-pharmacological and non-opioid medications are not effectively managing the pain, opioids may be added to the treatment plan (14).
If opioid therapy is needed and tramadol is prescribed, consideration should be given to tapering patients off antidepressants being used for pain relief to decrease the risk of serotonin syndrome. Opioids should be prescribed at the lowest effective dose, and it is recommended that immediate-acting opioids be prescribed before long-acting opioids, although long-acting or sustained-release formulations remain an option for treating neoplastic-related pain (14). Prior to prescribing opioid therapy and at every visit, the risk versus benefits of opioids should be evaluated and discussed with the patient (14). If benefits do not outweigh risks of continued therapy, steps should be taken to taper the dose down or taper to discontinue the opioid (14).
Therapy Goals
Another important step in therapy is the determination of therapy goals. Goal setting should occur early in the treatment process and should be a collaboration between the patient and the health care provider. When setting goals, they should be realistic to what can be achieved medically and within the base functioning of the patient, they should be specific as to what the patient wants to achieve, and include a realistic time frame for achieving these goals (14). Goals should be included in the patients plan of care within the electronic health record (EHR) and be reviewed at each visit. Evaluation of goals should also incorporate data tracked by the patient.
Compliance with use and appointments should also be encouraged. Patient education about the proper use of opioids and follow-up appointments is key. Other steps include requiring a follow-up visit before the first refill, with the understanding no additional scripts will be written until after the follow-up, and scheduling future appointments before the patient leaves the office (14). Health care providers should also work with the patient’s other providers to ensure the patient is not receiving multiple prescriptions and to ensure there are not any concurrent prescriptions for benzodiazepines (14). A thorough check the EHR for previously written prescriptions should be completed. For outside health care providers, the patient should be asked to sign a release of information, to allow these records to be obtained. For health care providers living in states with prescription drug monitoring programs, the database should be checked prior to prescribing and information regarding prescriptions written should be submitted following the regulations set forth by individual states (14).

Self Quiz
Ask yourself...
-
Why should non-pharmacological and non-opioid options be considered before treating pain with opioids?
-
Looking at what resources are readily available in your current practice area, what non-pharmacological would be available for your patients?
-
What barriers might your patients have to accessing these resources?
Ongoing Monitoring
The CDC identifies urine drug screens should not be used solely to determine risk; however, when they are used in combination with other risk assessment strategies, the use of urine screens may be helpful to identify those patients at high risk of overdose, and as a method to identify which patients may need additional monitoring or support (14). Urine screens should be used at the start of opioid therapy for chronic pain and can be used throughout therapy to validate what the patient has reported and to identify the use of multiple substances (4, 15). The frequency of testing should be determined by how stable the patient is, the type of treatment, and the setting in which the treatment is taking place (4). The CDC’s basic recommendations are that urine screening occurs annually for patients on long-term opioid therapy (14). However, in some cases, more frequent screening may be mandated for patients undergoing treatment for substance use disorders (4).
Not all urine screens are the same. As such, the healthcare provider, nurses, and staff performing the screen should obtain additional training and education beyond this West Virginia Drug Diversion course regarding the specific screen being used and following manufacturer recommendations for performing. Because some substances may only be present in the urine for up to 3 days, a negative result may not rule out the use of a substance (4). Instead, health care providers should use this information in conjunction with assessment findings and subjective patient reporting to determine if further action or monitoring is necessary.
Pill counts are also sometimes used as a method for ongoing monitoring of a patient’s compliance with therapy and as a method for preventing drug diversion. The idea behind pill counts is if the patient presents to the visit with the correct number of pills then misuse and diversion are not occurring. When used alone, pill counts are not effective in preventing addiction, and the evidence does not support using this as a sole method for preventing misuse (14). However, use of pill counts are still sometimes used as part of opioid therapy and are still sometimes included as part of the treatment agreements. When used with other methods, they can provide insight into patient use of the medication and provide an opportunity for ongoing education about safe use and storage of opioid medications. Healthcare practitioners choosing to use pill counting as a method of deterring misuse and diversion should recognize pill counts may be “padded” by borrowing, renting, or purchasing additional pills illegally. Care should be taken not just to count the pills remaining in the prescription but to also verify the pills all have the same appearance.

Self Quiz
Ask yourself...
-
Why are urine drug screens and pill counting only a small part of ongoing monitoring and why should these not be used alone for determining compliance?
-
What should be taught to the patient about use of urine drug screens and pill counting as methods of monitoring opioid use?
Referrals
Referrals are an important part of managing a patient with pain, especially in cases of chronic pain. Healthcare providers should be willing to provide referrals to outside providers and specialists to address specific pain concerns. For example, if a patient is identified to have chronic pain in their lower back or hips, a referral to an orthopedic specialist for evaluation is warranted. If a patient has used multiple modalities, including opioids, without success a referral to an interventionalist may be needed to determine if the patient is a candidate for a nerve block, neuromodulation, or implantation of an intrathecal medication delivery device (12).
For patients with a history of substance use disorder or other underlying mental health concerns, a referral to a psychologist, psychiatrist, or mental health therapist should be provided, and the healthcare provider should work in conjunction with this specialist to manage the patient. Behavioral health services should also be considered for patients without a personal or family history of addiction or mental health disorders, as chronic pain can cause depression and anxiety. When opioids are used, long-term chemical changes in the brain occur, increasing the risk of not only substance use disorder but depression, anxiety, paranoia, and hallucinations (25). This West Virginia Drug Diversion course highlights the importance of not only identifying patients who may be suffering from a mental health disorder as a result of opioid use but ensuring that proper treatment is provided.
For some patients with chronic pain, referral to a pain specialist may be necessary. While not every patient needs this, there are some reasons when a referral becomes necessary:
- the patient requires higher dosages of morphine or another opioid
- concurrent use of other CNS depressants (benzodiazepines, muscle relaxers, or anticonvulsants)
- requests more opioids, asks for early refills, or has pain-related visits to the emergency department or urgent care
- reports use of illicit drugs or urine drug screen is positive for non-prescribed drugs
- the patient is unable to follow the pre-agreed upon treatment plan
- refuses to use non-pharmacological or non-opioid pain management strategies
- refuses to taper dosage when risk outweighs benefits (12)
Primary healthcare providers should work with pain specialists to determine if the patient should be referred for medication management or if a transfer of care is necessary (12).
Referrals may also be needed for services such as physical therapy or occupational therapy. In some states, patients may seek out therapy services on their own, and in some states, a referral or prescription is required. Health care providers should determine if a prescription or referral is necessary for insurance purposes before sending the patient for evaluation by a physical or occupational therapist or other specialty healthcare providers. When determining which referrals are needed, the healthcare provider should explore what resources are available locally as well as any barriers the patient may have to attend those appointments.

Self Quiz
Ask yourself...
-
Consider patients currently under your care. What additional referrals might benefit these patients?
-
When should patients be referred to a pain specialist?
Treatment Agreements and Informed Consent
The use of patient-provider agreements has a long history in opioid treatment. Initially, these were used to set standards or requirements for patient behavior and often included dismissal as a punishment for not adhering to the agreed-upon treatment regimen (12). When used in this manner, the effect on patients was not always positive. Patients often felt a sense of distrust and stigma related to the use of these agreements, which only served to undermine the therapeutic relationship and threatened the treatment plan (12, 33). Yet, the use of patient-provider agreements continues to be included as part of treatment recommendations, because when used correctly they can help support both the patient and healthcare provider (14).
Because of these recommendations, treatment agreements continue to be used. Healthcare providers should take steps to ensure the treatment agreements are being implemented in a way that is patient-centered and are not punitive in nature, but instead act to provide information about risks and benefits as well as steps to ensure compliance (12, 33). Perhaps a better way of looking at treatment agreements is to see them as a method of informed consent, wherein the patient is provided need-to-know information including risks, benefits, and consequences of noncompliance, and is then allowed to determine if undergoing treatment is what they desire (12, 33).
While patient treatment agreements historically may not have always been effective, they become one part of a patient-centered treatment plan when used correctly. Not only can these agreements serve as a way to document the patient’s informed consent of the treatment, but they can be used to identify clear goals and expectations for patients receiving opioid therapy. Treatment forms may vary from clinic to clinic, but common components include:
- treatment goals
- responsibilities for safe medication use
- storage and disposal of opioid medications
- requirement for the patient to obtain prescriptions from only one clinician or practice
- requirement to only fill prescriptions at one pharmacy
- agreement for periodic drug testing
- clinician agreement to be available or have coverage (16)
In addition to the use of treatment agreements, healthcare providers should implement the use of informed consent forms (16). In some cases, these are combined with the treatment agreements, and in other cases the informed consent may be a separate document. Components of the informed consent should include:
- the limited benefit of opioid in chronic pain
- risks and benefits of opioids
- potential side effects, including sedation and impaired motor skills
- risk of tolerance, physical dependence, development of a substance use disorder, overdose, and death
- prescribing policies and expectations
- reasons why therapy may be changed or discontinued
- education that the patient should not expect to be pain free (16)

Self Quiz
Ask yourself...
-
What consequences might be incurred by the patient or provider who fails to uphold or follow the treatment agreement?
-
Should treatment plans be used every time an opioid is prescribed?
Discontinuing Opioid Therapy
Discontinuing opioid therapy may be considered for various reasons; risk outweighs the benefit, effective use of non-pharmacological therapies and non-opioid medications, patient desire to stop use, and noncompliance. Understanding why the therapy is being discontinued and communicating with the patient is important to ensure that pain management goals are met. Recommendations for discontinuing opioid therapy are to initially taper just the dose, then extend the time between doses (14). Once a patient has reached the point where they are taking an opioid less than once a day, the opioid can be stopped (14).
Emergency discontinuation of therapy or rapid tapering of opioid dosing may occur when a patient overdoses on their current dose (14). In these cases, patients should be closely monitored in a controlled setting, and supportive therapy to manage withdrawal symptoms should be employed. Urine drug screens should be completed to rule out the presence of other drugs and baseline CBC, metabolic panel, and liver enzymes should be obtained. The clinical opiate withdrawal scale (COWS) should be utilized to monitor for signs and symptoms of withdrawal.
The COWS is an 11-criterion scale that looks at physical symptoms of withdrawal. Each criterion is scored based upon what is being evaluated or observed in the patient. A score of 5-12 indicates mild withdrawal, 13-24 is moderate, 25-36 is moderately severe, and patients scoring above 36 are in severe withdrawal. The criterion evaluated includes:
- resting pulse rate
- sweating
- restlessness
- pupil size
- joint pain
- runny nose or tearing of the eyes
- GI upset
- tremors
- yawning
- reported anxiety or irritability
- piloerection
Proper use of the scale is important, and the nursing staff who will be using the scale to evaluate patients should be properly training in its use. Treatment of acute withdrawal symptoms should be based on the patient’s COWs score and the symptoms they are presenting. In addition to the symptoms evaluated using the COWs, blood pressure should be monitored and hypertension should be managed. Medications used to manage symptoms of acute withdrawal include anti-emetics, non-opioid antidiarrheals, and clonidine or lofexidine. Care should also be taken to provide a low stimuli environment, such as dimmed lights, limiting excess noise, and keeping the room at a comfortable temperature.
Managed withdrawal can also occur more slowly and is commonly seen in patients who are heroin-dependent or if the patient and healthcare provider identify a detoxification program is needed. In some cases, methadone or buprenorphine may be used to lessen the symptoms of withdrawal. Patients prescribed methadone should also be provided referral to a methadone clinic for monitoring and medication distribution. Patients undergoing methadone or buprenorphine treatment should also be referred for behavioral therapy to help manage psychological effects, and for ongoing treatment and support of a substance use disorder (14).

Self Quiz
Ask yourself...
-
What are the dangers related to discontinuing opioid medications?
-
Why should patients undergoing acute withdrawal be in a monitored setting, such as a clinic or hospital?
-
What type of situations might lead a health care practitioner to identify the need for managed withdrawal with the use of buprenorphine or methadone?
Patient Education
Education of patients at the point of prescribing and at every visit thereafter is important to ensuring patients are actively involved in their own care and are taking steps to manage their care at home. However, educational practices can be inconsistent between clinics and facilities, between health care practitioners, and, in some cases, education is missing (18). For patients who are prescribed opioids, education is a key component towards ensuring patient safety.
Both patients and family members should be taught the risks and benefits of opioid use, the effectiveness of opioids, and the appropriate use of opioid medications. Patients and families should be taught the signs and symptoms of an overdose and how to appropriately intervene in the case of an overdose. Additionally, patients should be taught about diversion’s risk and steps to prevent it (18).
Prior to engaging in patient education about opioids or addiction, the nurse should first self-evaluate or reflect on their own feelings related to these topics. Efforts should be made to approach each patient as an individual and to avoid stereotyping patients based upon their type of pain, use of opioids, or history of a substance use disorder. Patients should be approached in a nonjudgmental manner, and nurses should employ therapeutic communication techniques, allowing the patient to express their concerns and to encourage questions.
When starting an educational session, it is important to identify the specific learning needs of the patient. This may range from identifying the type of learner the patient is, the level of education or reading level, and even includes identifying specific questions or concerns the patient has related to using an opioid.
Time should also be committed to evaluating what the patient’s current knowledge about opioid use is and to dispel misconceptions the patient may have about opioids. Misconceptions that may be held by patients about opioids, addiction, or the prescribing process might include:
- Opioids are the only thing that will help the pain.
- When taken as prescribed, addiction will not occur.
- Not being prescribed an opioid means the health care provider thinks the patient is an addict
- Addiction only happens to certain types of people.
Nurses should take care to provide facts and evidence (at the patient’s level) to dispel misconceptions. When addressing misconceptions, it is also important to be aware of tone and forms of non-verbal communication to not inadvertently pass judgment on what the patient believes.
While teaching should be specific to meet the patient’s individual needs and prescribed opioid, information about safe use, storage and disposal, and use of opioid antagonist medications should be provided to every patient. The information provided in this West Virginia Drug Diversion course offers great opportunities and points to share with patients. Standardized educational materials should be around a 6th grade reading level to ensure that most patients easily understand the material. The use of videos through a patient education platform, like those available through Krames or X-Plain, can be useful for educating patients who are unable to read the material or are auditory learners. If these are not available, clinic-made videos or videos available online may be used.

Self Quiz
Ask yourself...
-
Why is it important for the nurse to explore their own biases about opioid use and substance use disorders?
-
What teaching might be provided to a patient who had misconceptions? Why is this teaching important?
Safe Use of Opioids
One aspect of patient education that is essential to highlight in this West Virginia Drug Diversion course is the safe use of opioids. Because opioids are used in both acute and chronic pain management, education about safe use is an important step in helping patients take an active role in their treatment plan and ensuring their safety outside the clinical setting. In the case of a patient being treated for acute pain, instructions should include guidelines for how the opioid should be taken and for how long it should be taken. Nurses’ common education for a patient with acute pain is to take their opioid pain medication to “stay ahead” of the pain. This instruction does not go far enough to address safe use. Patients should be instructed to take their opioid medication as prescribed and not increase the frequency or dosage if the pain worsens, but instead to notify their health care provider. Patients may believe that if it is prescribed, they must take the medication, so the nurse should also educate that opioids are an as-needed medication and should not be taken if not needed; in most cases of acute pain, opioids may only be needed for the first few days. Teaching patients to self-evaluate their pain is important in determining if the opioid is necessary or if an alternative medication, such as a NSAID, would be more appropriate.
In the case of a patient being treated for chronic pain, instructions should still include guidelines for how it should be taken, but additional guidance should be provided about safety related to toxicity and withdrawal. Opioids for chronic pain management may be either immediate-acting or long-acting, and education differs based on what is prescribed. Patients prescribed immediate-acting medications should be instructed not to change the frequency or dosage prescribed due to the risk of toxicity.
If the patient finds their pain is not being managed, further evaluation is necessary, and they should be instructed to notify their healthcare provider. These patients should also be aware of how many doses have been prescribed and be taught to manage their use of the medications. Patients who are unable to manage this effectively may find they have finished the supply and are not able to refill the prescription for several days, leading to withdrawal. For patients prescribed long-acting opioids, they should be provided education on how these medications differ from immediate-acting and to not take extra for breakthrough pain. Taking long-acting opioids as prescribed is important to prevent withdrawal. Because these medications stay in the system longer, there is also a risk of toxicity if the patient takes an extra dose or additionally medicates with a short-acting opioid.
With any patient-prescribed opioids, additional education related to misuse and diversion should be provided. Most people who reported misusing prescription opioids identified they got the drugs from a friend or family member (21). Patients should be taught to count their medications and to keep track of their use. If they identify pills are missing, patients should be informed to notify authorities and their healthcare provider. Education should include that the prescriptions are only for personal use and should not be shared with a relative or friend. Education about safe use also needs to include concurrent use of opioids with other medications or alcohol. The patient should be instructed to avoid alcohol because of the additive CNS depressant effects, which increase the risks associated with respiratory depression. A thorough review of all patient medications, prescribed, over-the-counter, and herbal, should be completed. Education regarding potential reactions should be provided.

Self Quiz
Ask yourself...
- A patient is given a new prescription for a fentanyl transdermal patch. What should the nurse teach the patient about safe use?
Proper Storage and Disposal
Proper storage of opioids can deter theft, loss, and misuse of medications. Patients should be taught to keep opioids in the original packaging and not to store them in pillboxes. Many patients often keep medications in the kitchen or bathroom near the sink or on a shelf. Patients should be taught to keep opioids in a locked drawer or cabinet that is not easily visible or accessible to others. Additional patient education should include the dangers of accidental ingestion by children or pets. Patients should also be cautious with whom they tell about their opioid prescription and should be educated that this information should only be shared with direct caregivers.
Patients also need to be taught about the proper disposal of opioids. Many patients will often save leftover prescription medications, “just in case,” and many patients may have multiple old prescriptions in their home, increasing the likelihood they are unaware of what is there or if it may have gone missing. It is estimated less than 20% of patients properly dispose of opioid medications (18). Educating patients on proper disposal can help to prevent problems related to the diversion of opioids by people the patient knows (18). The Food and Drug Administration (FDA) identifies the preferred method of opioid or other controlled substance disposal is to take the medication to a disposal location (39). Many pharmacies offer take-back services that will allow patients to dispose of old or unused prescriptions. Locations for take-back services can also be found by completing a search through the Department of Justice.
In some cases, a patient may not be able get to a drop off location. In these cases, the FDA has also identified both a flush and no-flush list for medications that can either be disposed of by flushing down the toilet or by discarding into the trash (39). Most medications containing opioids can be flushed to prevent misuse or diversion (39).
For other controlled substances that cannot be flushed, it is recommended patients be taught to mix the medications in something most people wouldn’t dig through or ingest, such as cat litter, to place the mixture in a sealed plastic bag, and to throw it in with regular household trash (39). Patients should also be taught to blacken with a permanent marker or to scratch out any personal information on the prescription bottles before putting them in the trash (39). Education on disposal should include where a local drop-off site is located, which prescribed medications can be flushed, and which ones need to be put in the trash. Patients concerned about the environmental impact of flushing medications should be informed that the FDA has found the flushable medications “present negligible risk to the environment” (39).

Self Quiz
Ask yourself...
-
The patient with the new prescription for the fentanyl transdermal patch wants to know what she does with the used patch. What instructions should be provided?
-
What additional resources to patients have for disposing of unused prescriptions?
Opioid Antagonists
There are two commonly used opioid antagonists in use in the U.S., naloxone and naltrexone; both medications bind to opiate receptor sites, blocking the ability of the opioid to bind to the site. Patient education should include why a specific opioid antagonist is being used, appropriate administration, and potential side effects.
Naloxone
Naloxone (otherwise known as Narcan) is used as a reversal agent for acute overdose or accidental ingestion. Patients taking opioids or who have family members who take opioids can either obtain naloxone either by prescription or directly from their pharmacist without a prescription. It can be used by patients or their loved ones in the home to prevent death or permanent disability as the result of opioid use. Family members should be taught to call for emergency assistance (911) if they administer naloxone to a loved one. Additionally, they should be taught to look for signs and symptoms of respiratory depression in the event a second dose needs to be administered. Patients and families should also be taught naloxone is only effective for the treatment of opioid overdose and will not treat overdose related to other substances. The FDA recommends healthcare providers discuss and consider prescribing naloxone for patients who meet the following criteria:
- high risk for overdose
- take other central nervous system (CNS) depressants
- history of substance abuse
- history of overdose
- have children who may accidentally ingest opioids (40)
Currently, naloxone has been approved for administration via three methods (28).
- Injectable naloxone – This is available in a 2mg/2ml syringe and is mostly used by healthcare workers in hospitals and by paramedics. For patients who receive this type of naloxone, training should be provided on the appropriate use of a syringe, dosing, and administration.
- Autoinjectable Naloxone – Teach patients each autoinjector only contains one dose. If an additional dose is necessary, a second autoinjector will need to be used. If using an auto-injectable form, patients should be taught specifically how to open and activate the device and inject into the outer thigh.
- Nasal Spray – A prepackaged nasal spray is often easiest for patients to use and can be obtained without a prescription from a pharmacy. With the nasal spray, patients and families should be instructed to ensure the patient is on their back, place the device’s tip into one nostril, and press firmly on the activator. Each package of spray contains one dose. Additional doses can be administered but a new device will be needed. Patients and families should be instructed to alternate nostrils if repeat doses are necessary.
Naloxone adverse effects are often related to the reversal of the opioid and may include nausea, vomiting, diaphoresis, tachycardia, blood pressure irregularities, and tremors (28). When administered to a patient who regularly takes opioids or in an overdose, withdrawal symptoms may become present with minutes. Severe adverse effects include seizures, dysrhythmias, pulmonary edema, and cardiac arrest (35).
Nalxtexone
Naltrexone is an opioid antagonist used for longer-term treatment and management of opioid addiction. It requires a prescription and can be taken as a daily oral medication or as a monthly injectable. It should not be prescribed to patients who currently take opioids or who have recently used opioids or alcohol, as withdrawal symptoms will occur (37). Patients prescribed naltrexone should be instructed to avoid any opioids (prescribed or non-prescribed), alcohol, and cough or cold medications containing alcohol (37). Prior to naltrexone being prescribed, patients should have a thorough medication review done to avoid potential interactions with other prescribed medications, specifically those used to treat depression (37). Education regarding adverse effects should also be provided. Common adverse effects include nausea, vomiting, decreased appetite, drowsiness, and problems sleeping (37). Instruct patients to notify their health care provider if they experience severe adverse effects such as difficulty breathing, injection site skin changes, right upper abdominal pain, or suicidal thoughts (37).

Self Quiz
Ask yourself...
-
When should naloxone or naltrexone be used?
-
What priority education should be provided to patients and families about opioid antagonists?
Drug Seeking and Diversion
Patients
The term ‘drug-seeking’ can have a negative connotation. It is often used by healthcare providers and nurses to refer to patients who behave in a certain way, seek out treatment for certain types of pain, or their explanation of events is viewed as unbelievable or untrustworthy. Unfortunately, because the term drug-seeking has come to be used as a kind of a catch-all, legitimate patients sometimes get identified as being “drug seekers,” and their pain goes untreated (13). The use of the term ‘drug-seeking behavior’ specifically refers to behaviors displayed by patients who are struggling with substance use disorders. In caring for patients who display drug-seeking behaviors, nurses need to be aware of their own feelings and biases as they relate to opioid use and addiction. They should approach each situation with a patient in a non-judgmental manner and objectively evaluate the patient so proper intervention can be given.
Patients who are misusing prescription opioids may not recognize they have a problem and may feel their pain is being ignored. They will often lie about symptoms or exaggerate the amount of pain they are experiencing. This can be especially difficult to assess as nurses are taught pain is whatever the patient says it is. Because each patients’ pain experience is different and their responses vary, making objective pain assessments can be difficult. Physical changes, such as elevated blood pressure, tachycardia, or diaphoresis, which might be seen in acute pain are often not present in chronic pain, further complicating the assessment.
Patients may visit multiple clinics, urgent care, and emergency departments, which is often called ‘doctor shopping,’ and this practice allows the patient to potentially receive multiple opioid prescriptions from different healthcare providers. Depending upon what is available in the area where the patient lives, the patient may also travel to other towns or neighboring states to obtain prescriptions. Often in these cases, the patient will only give a partial or vague history. Patients may deny a request to obtain recent health records or provide false information about either themselves or where they have been treated. In addition to ‘doctor shopping,’ patients may also use multiple pharmacies to have prescriptions filled. Following the completion of this West Virginia Drug Diversion course, it is vital for healthcare providers to pick up on these signs of ‘doctor shopping.’
Escalation of use is often seen and occurs when patients take a higher dose, takes a dose more frequently, or both, outside of how the opioid has been prescribed by their provider. Patients may also take measures to obtain additional prescriptions from their regular healthcare provider. Patients who call the office to ask for a prescription right before the weekend or a holiday may require further investigation, especially if this is a common occurrence. One occurrence of a patient doing this does not meet the criteria of drug-seeking behavior; however, when there are repeated incidents or a pattern of behavior, it should be addressed.
Patients may request a specific opioid or having a long list of allergies to other pain medications. Many of these patients may also report they are currently taking multiple opioids or other controlled substances. When asked about the use of opioids, other controlled substances, or even illicit drug use, patients may become angry. Aggression may also be seen when adjusting a plan of care, where the opioid medication will be changed, or the healthcare provider identifies it is time to start tapering the medication due to risks outweighing the benefits of treatment.
In urgent care, emergency department settings, and even with the general hospital setting, changes in behavior from the waiting room to the treatment room are sometimes observed. When this occurs, patients may be calm, at a distance appear to be comfortable, or may be seen doing other activities (talking on the phone, conversing with other people, walking around); however, once placed in a treatment room, the patient may hold the area that hurts, moan, or even begin crying. If receiving IV medications, they may ask the nurse to “push it fast” or may request oral medications be changed to IV.
Drug diversion is an illegal act occurring when a prescribed controlled substance is obtained illegally. In some cases, diversion is done as a method of obtaining prescription opioids in order to sell them. However, diversion also occurs when a patient obtains a prescription, under false pretenses, for their own use. Identifying the end goal allows the health care provider to take appropriate steps to help the patient. Healthcare providers have a duty to report opioid diversion to law enforcement; however, criminal action against a patient will vary based upon the state, intent of diversion, and if there is an intent to sell or distribute. When a patient is diverting drugs for their own use, treatment of the substance use disorder is a priority and, depending upon the situation; legal action may not be taken if the patient undergoes treatment.

Self Quiz
Ask yourself...
-
What actions might the nurse see in a patient with drug seeking behaviors?
-
How might have the term drug seeking become stigmatized?
-
What steps can the nurse take to prevent their own biases and feelings from interfering with their care of these patients?
Drug Diversion in Nursing
It is estimated that 10% of practicing nurses are abusing one or more substances (32). Nurses with substance use disorders often go unidentified and it can be easy for co-workers to ignore the signs and symptoms or to dismiss them as the being stress related (24). Yet, failing to identify nurses who are struggling with substance use puts not only patients, but co-workers at risk. It is necessary to address this prevalence in this West Viriginia Drug Diversion course.
Because nurses often have readily available access to controlled substances, their methods of diversion differ from those of patients and often are not as easily detected until a pattern is identified.
Nurses may remove a full dose but only give a partial dose to the patient, may substitute the patient’s injectable opioid for saline, or may “forget” to waste excess opioids. Additionally, the nurse may be overly helpful; coming in early or staying late, offering to give medications for another nurse, or picking up extra shift as it gives them greater access. If not unidentified, the nurse may divert for a period of time undetected, in some cases, years. For some nurses, it is not until their behavior or physical appearance starts to change for co-workers and managers to identify a problem. Physical changes may include changes in appearance, hygiene, disheveled clothing, and in their cognitive ability (memory or concentration). Behaviors commonly seen include changes in their schedule (coming in early, leaving late, or frequent sick days), multiple breaks off the unit, and frequent bathroom breaks. As the drug starts to have a greater impact on the nurse, there may be an increase in the documentation or medication errors, or narcotic counts will consistently be off when that nurse works.
When a nurse is suspected of diversion, reporting the incident helps the individual and helps to keep patients safe; depending upon the environment and area where the nurse works may determine to whom or where the suspicions should be reported.
Many facilities have policies related to what should be reported, who it should be reported to, and what documentation will be required. In most cases, the incident would be reported to the direct supervisor or employer. Once it has been reported, the employer is responsible for investigating the incident, which included looking at pharmacy logs, reviewing documentation, and interviewing involved parties. If controlled substances are missing, the employer has 24 hours to report the Drug Enforcement Agency (DEA) discrepancy. In some cases, law enforcement may also be contacted if the amount missing may indicate theft. The nurse will also be reported to their state board of nursing. In some cases, the nurse may be given the opportunity to self-report the incident. It is also important to note best practice supports the nurse not being terminated when impairment or diversion is confirmed, as this often prevents the nurse from accessing treatment (5).
The act of drug diversion by a nurse does not immediately mean their license will be revoked. An investigation by the licensing board will occur and depending upon the circumstances, the nurse’s license may be suspended, and they may be required to undergo substance abuse treatment, or, in some states, may enter an alternative-to-discipline program. This program entails evaluation, treatment, and ongoing monitoring as a condition of being allowed to return to work (5, 24). The nurse who has had their license suspended may request their license be reinstated if they meet the requirements by the board of nursing disciplinary board. In some cases, restrictions may be placed limiting the administration of controlled substances to patients.
Once the nurse returns to the workforce, employers should take steps to support the nurse and their recovery. Best practice supports the use of employer-employee contracts that outline conditions (23). Suggested components of the contract include:
- providing the nurse with a mentor who has been successful in recovery
- assigning to a day shift
- information regarding facility liability insurance and relevant guidelines and policy from the state board of nursing
- practice restrictions placed by either the board of nursing or the facility
- accommodations made to support in recovery (time off to attend meetings)
- facility policies on random drug testing
- evaluation criteria and timeline for evaluations
- expectations related to ongoing treatment
- consequences if the nurse relapses
- length of time the contract will be valid (23)
Nurses who are undergoing treatment and returning to work should be encouraged to ask questions to ensure expectations are clear. There remains a lot of stigma related to substance use disorders in nurses and employers should take steps to ensure the unit where the nurse is placed will be a supportive environment (5). Steps should also be taken to protect the nurse’s right to privacy from co-workers as it relates to ongoing treatment (5).

Self Quiz
Ask yourself...
-
What signs and symptoms might indicate a nurse has a substance use disorder?
-
What steps should be taken if nurse diversion is suspected?
-
Why is it important to place a nurse, returning to work after treatment, in a supportive environment?
Prescription Drug Monitoring Programs
While tracking and monitoring controlled substances ultimately falls under the DEA purview, in reality, the DEA’s ability to accurately track this data on a state or local level is difficult. In response to the need for improved data collection and access to data, multiple states have started statewide prescription drug monitoring programs (PDMP).
These programs are used to track prescribers and pharmacies, and patients who receive these prescriptions as well. PDMPs improve patient safety by allowing practitioners and pharmacists to quickly identify patients who have obtained prescriptions from multiple providers, identify the total number of prescribed opioids, and identify high-risk patients who have been prescribed other controlled substances (11). Through careful tracking and data collection, states can also use the data to determine if other statewide measures to combat opioid addiction and overdose are having any impact. The biggest drawback to these programs is the interoperability of systems between states, which limits data sharing and integration with electronic health records (3).
In 1995, West Virginia introduced their first controlled substance monitoring program. Since its initial introduction, the program has evolved to an internet-based program capable of exchanging information with several other states (17). Work is also being done to integrate the Controlled Substances Monitoring Program (CSMP) into the electronic health record using the NarxCare program (42). Once fully integrated, providers can search for patients through the system without logging into the CSMP separately and help providers identify patient risk scores, prescription data, and patient safety alerts (42).
Use of CSAPP
Practioners in West Virginia, who prescribe schedule II, III, IV, and V controlled substances, products containing gabapentin, and opioid antagonists, are required to report to the CSAPP (44). Reports should be submitted every 24 hours.
The information to be reported includes:
- name, address, pharmacy, and DEA number of the pharmacy
- full legal name, address, and date of birth for the patient
- name, address and DEA number of the prescriber
- name and national drug code number of the substance being prescribed
- quantity and dosage of substance being prescribed
- date prescription was written and filled
- number of refills authorized by the prescriber
- government-issued ID of the individual picking up the prescription if not done so by the patient
- payment source (44)
Additionally, in the event a provider treats a patient for an overdose, the provider should report the full legal name, address, and date of birth of the patient being treated as well as any data collected as evidence of the overdose (44).

Self Quiz
Ask yourself...
-
Why are PDMPs an important tool in battling the opioid epidemic?
-
What drawback still exist with these programs?
-
What responsibility do health care practioners have related to use of the CSAPP?
Case Study
S. is a 40-year-old male. He denies any chronic illnesses. He is being evaluated at a local urgent care for lower back pain. He reports the pain started after helping a friend move some heavy boxes. C. S. denies any other injuries to his back and states, “other than what is going on right now, I am healthy.”
After evaluation by the health care provider, no acute injuries were identified, and he was diagnosed with back strain. He received instructions to ice his back, was provided exercises to strengthen his back muscles, was prescribed hydrocodone/APAP 5/500mg for the pain, and instructed to follow up with his primary health care provider.
Based upon what has been learned, what should have been done differently at this urgent care visit regarding prescriptions provided to C. S.?
It has now been one year since C. S.’s initial diagnosis of back strain. Since then, he has had repeated visits for back pain and has progressed to needing daily opioid medication to manage the pain. He reports the pain got to the point where he struggled to complete tasks at his job, and frequently had to call in sick. Recently, he lost his job as a construction worker, a job he had for 17 years. C. S. is being evaluated at his primary health care provider’s office due to his reports of chronic back pain.
What priority assessments should be obtained regarding C. S.’s pain and current opioid use?
What diagnostic tests should be performed and why are these tests important?
After meeting with his health care provider, C. S. has agreed to the use of non-pharmacological and non-opioid therapy for his chronic back pain. He reports he is willing to try anything that will make him feel better and get back to work.
What non-pharmacological modalities or non-opioid medications might he benefit from receiving?
As part of the treatment plan for C. S. what referrals might need to be made?
What considerations need to be taken into account when prescribing treatments and making referrals?
During the visit with the health care provider, C. S.’s frequent visits to the urgent care and emergency department are addressed. C. S. admits to often taking more of the hydrocodone than he should have because the pain was so bad.
Based upon what is known about C. S., what type of ongoing monitoring should be used?
Why is this monitoring the best choice for C. S.?
S. has agreed to the proposed treatment plan but he also expresses he is worried his family and friends will only see him a drug addict. He expresses concern that because of his opioid use he won’t be able to go back to work.
What should the nurse include in the teaching plan for C. S?
Summary
Pain is a complex process that differs for each patient and is not always easily treated. A thorough assessment is necessary to determine the type of pain present. This assessment also serves to aid in diagnosis and as a baseline for determining the effectiveness of prescribed interventions. For patients with pain, who are using opioids, there is a risk of developing tolerance and dependence upon the drug, resulting in the development of a substance use disorder—previously known as an addiction, substance use disorders are now recognized by the APA and are further categorized in the DMS-5. This important step has helped to further awareness of the problem among health care providers and provides clear guidelines for the diagnosis of the disorder.
The CDC has identified best practice guidelines to prescribing opioid therapy:
- Implement non-pharmacological and non-opioid medications before using opioids for pain
- Identify realistic goals addressing both pain and level of function
- Educate patients on both the risks and benefits of opioid therapy
- Prescribe immediate-release and the lowest effective dose for patients who need opioid therapy
- When prescribing opioids for acute pain, only prescribe what the patient will need for three days
- Regularly evaluate risk versus benefit and taper dosage or discontinue if benefits do not outweigh the risks
- Evaluate risk factors for misuse and addiction
- Use PDMP data to inform decision-making and identify patients at high risk for overdose.
- Implement urine drug screening at initiation of therapy and annually
- Avoid prescribing both opioids and benzodiazepines
- Offer treatment for patients with substance use disorder (14)
When non-pharmacological and non-opioid options have been attempted without success, opioid therapy remains an option for pain management. Patient education related to opioid use should focus on the medication being prescribed and address both administration and adverse effects. Additional education related to the safe use of opioids, storage and disposal, and the use of opioid antagonists should also be provided.
The incidence of substance use disorder is the U.S. remains high, even in light of steps taken by federal and states governments to address the problem. The cost of addressing opioid misuse takes a heavy toll on the healthcare system and both state and federal budgets, but these pale in comparison to the impact on patients and families who are suffering under the heavy burden of substance use disorders. Everyday patients and their families are affected by opioids and feel the impacts of joblessness, broken families, and death from overdose as result of the opioid epidemic. Measures taken by the state of West Virginia have raised awareness of the problem and have helped address concerns related to prescribing and access, but the work is not done; this West Virginia Drug Diversion course is just one step in the right direction. Continuing education about prescribing, administering, and dispensing controlled substances is essential to help curb over-prescribing and to help identify patients at risk of substance use disorders, so early intervention can be provided. Likewise, patient education is needed to ensure patients are taught the skills to safely use opioids to manage their pain and to be prepared to take an active role in their treatment plans.
References + Disclaimer
- Centers for Disease Control and Prevention (2023). What is health Literacy? Retrieved on September 15, 2023 from https://www.cdc.gov/healthliteracy/learn/index.html
- MedlinePlus [Internet] National Library of Medicine. Choosing effective patient education materials; Reviewed 2021 October 17] Retrieved on September 15, 2023, from https://medlineplus.gov/ency/patientinstructions/000455.htm
- Goodman, C., Lambert., (2022). Scoping review of the preferences of older adults for patient education materials. Patient Education and Counseling, Volume 108, March 2023, 107591. Retrieved on September 15, 2023, from https://doi.org/10.1016/j.pec.2022.107591
- Zajacova, A., & Lawrence, , (2018). The relationship between education and health: reducing disparities through a contextual approach. Annual Review of Public Health. 2018 April 1; Vol 39: pp 273-289. Retrieved on September 15, 2023 from https://www.ncbi.nlm.nih.gov/pmc/articles/PMC5880718/
- Betancourt, , Green, A., & Carrillo, E., (2021). The patient’s culture and effective communication. UpToDate. Retrieved on September 14th, 2023 from https://www.uptodate.com/contents/the-patients-culture-and-effective-communication/print
- Centers for Disease Control and Prevention (2021). Importance of Health Literacy. Retrieved on September 13, 2023 ,from https://www.cdc.gov/healthliteracy/developmaterials/audiences/olderadults/importance.html#:~:text=The%20National%20Assessment%20of%20Adult,interpreting%20numbers%20and%20doing%20calculations
- S. Department of Health and Human Services. (2019). Health Literacy Reports and Publications. Retrieved on September 15, 2023 from https://www.hhs.gov/surgeongeneral/reports-and-publications/health-literacy/index.html#:~:text=Health%20literacy%20is%20key%20to,have%20proficient%20health%20literacy%20skills
- Health Care Education Association. (2021). Patient Education Guidelines for Health Care Professionals. Retrieved on September 14, 2023, from https://www.hcea-info.org/assets/hcea%20guidelines%20color%201-25-2021.pdf
- Chick, N (2010). Learning Styles. Vanderbilt University Center for Teaching. Retrieved September 15, 2023, from https://cft.vanderbilt.edu/guides-sub-pages/learning-styles-preferences/
- Merriam-Webster. (d). Education. In Merriam-Webster.com dictionary. Retrieved September 15, 2023, from https://www.merriam-webster.com/dictionary/education
- Use the Teach-back Method: Tool #5. Content last reviewed September 2020. Agency for Healthcare Research and Quality, Rockville, MD. Retrieved on September 15, 2023, from https://www.ahrq.gov/health-literacy/improve/precautions/tool5.html
- Medline Plus. [Internet]. National Library of Medicine. (2021). Communicating with patients. Retrieved on September 17, 2023 from https://medlineplus.gov/ency/patientinstructions/000456.htm
- Marcum, J., Ridenour, M., Shaff, G., Hammons, M., & Taylor,M. (2021). A Study of Professional Nurses’ Perceptions of Patient Education. The Journal of Continuing Education in 2013;33(3): pp 112-118. Retrieved on September 18, 2023 from https://doi.org/10.3928/0022-0124-20020501-05
- Nurses are Still Stressed, Frustrated, and Overwhelmed Almost 2 Years into COVID-19. (2021, October 26). ANA. https://www.nursingworld.org/news/news-releases/2021/new-survey-data-thousands-of-nurses-are-still-stressed-frustrated-and-overwhelmed-almost-2-years-into-the-pandemic/
- General, O. O. T. S. (2022, May 23). New Surgeon General Advisory sounds alarm on health worker burnout and resignation. gov. https://www.hhs.gov/about/news/2022/05/23/new-surgeon-general-advisory-sounds-alarm-on-health-worker-burnout-and-resignation.html
- Harvey, B. (2022) 98 Best self-care quotes to remind you what matters. Retrieved from https://www.goodgoodgood.co/articles/self-care-quotes
- Writers, S. (2023, March 23). What is nurse burnout? | nursejournal.org. NurseJournal. https://nursejournal.org/resources/nurse-burnout/
- Wolotira, E. A. (2023). Trauma, compassion fatigue, and burnout in nurses. Nurse Leader, 21(2), 202–206. https://doi.org/10.1016/j.mnl.2022.04.009
- Vaughn, N. (2023). Nursing Compassion Fatigue and Burnout vs. Moral Injury. com Blog. https://www.nurse.com/blog/nursing-compassion-fatigue-and-burnout-vs-moral-injury/
- Shah, M., Gandrakota, N., Cimiotti, J. P., Ghose, N., Moore, M., & Ali, M. K. (2021). Prevalence of and factors associated with nurse burnout in the US. JAMA Network Open, 4(2), e2036469. https://doi.org/10.1001/jamanetworkopen.2020.36469
- National Academies Press (US). (2019, October 23). Introduction. Taking Action Against Clinician Burnout – NCBI Bookshelf. https://www.ncbi.nlm.nih.gov/books/NBK552613/#:~:text=Extensive%20research%20has%20found%20that,and%2060%20percent%20for%20medical
- Nurse burnout: What is it & how to prevent it | ANA. (2023, February 17). ANA. https://www.nursingworld.org/practice-policy/work-environment/health-safety/nurse-burnout-and-how-to-prevent-it/
- Burnout. (2022, September 27). PSNet. https://psnet.ahrq.gov/primer/burnout#:~:text=The%20emotional%20exhaustion%20and%20depersonalization,compromises%20the%20quality%20of%20care
- (2021, June 22). On the Verge of Burnout? Three Proactive Steps You Can Take Today – SHIFT. SHIFT. https://www.shiftnursing.com/articles/on-the-verge-of-burnout-three-proactive-steps-you-can-take-today
- Caring for your mental health. (n.d.). National Institute of Mental Health (NIMH). https://www.nimh.nih.gov/health/topics/caring-for-your-mental-health
- Tribe-Scott, BSN, RN, RAC-MT, RAC-MTA, QCP, M. (2022). Burnout: How can nurse leadership help? AAPACN. https://www.aapacn.org/blog/burnout-how-can-nurse-leadership-help
- Anusiewicz, C. V., Ivankova, N. V., Swiger, P. A., Gillespie, G. L., Li, P., & Patrician, P. A. (2020). How does workplace bullying influence nurses’ abilities to provide patient care? a nurse perspective. Journal of Clinical Nursing, 29(21-22), 4148–4160. https://doi.org/10.1111/jocn.15443
- Collins, B. (2022). Mobbing and workplace bullying among registered nurses in Mississippi. ABNFF Journal, 1(2), 20–28.
- Edmonson, C., & Zelonka, C. (2019). Our own worst enemies. Nursing Administration Quarterly, 43(3), 274–279. https://doi.org/10.1097/naq.0000000000000353
- Harassment definition & meaning. (n.d.). Dictionary.com. https://www.dictionary.com/browse/harassment
- Meires, J. (2018). Workplace incivility – the essentials: Here’s what you need to know about bullying in nursing. Urologic Nursing, 38(2), 95. https://doi.org/10.7257/1053-816x.2018.38.2.95
- Thompson, R. (Feb 2022). Getting Clear on Bullying Versus Incivility. Florida Nurse, 70(1), 19–19.
- Agency for Healthcare Research and Quality (AHRQ). (2021). Benchmarking for Quality Improvement. https://digital.ahrq.gov/health-it-tools-and-resources/evaluation-resources/workflow-assessment-health-it-toolkit/all-workflow-tools/benchmarking
- Agency for Healthcare Research and Quality (AHRQ). (2021). Data Collection and Management. https://www.ahrq.gov/talkingquality/measures/data-collection.html
- Agency for Healthcare Research and Quality (AHRQ). (2021). Nursing-sensitive indicators: AHRQ quality indicators. https://www.qualityindicators.ahrq.gov/Modules/nursing-sensitive_indicators.aspx
- Agency for Healthcare Research and Quality (AHRQ). (2019). TeamSTEPPS 2.0: Strategies and Tools to Enhance Performance and Patient Safety. https://www.ahrq.gov/teamstepps/index.html
- Agency for Healthcare Research and Quality (AHRQ). (2021). Types of Measures. https://www.ahrq.gov/talkingquality/measures/types.html
- Centers for Medicare & Medicaid Services (CMS). (2021). Quality Improvement and Evaluation System (QIES). https://www.cms.gov/medicare/health-safety-standards/quality-safety-oversight-general-information/iqies
- Deming, W. E. (1986). Out of the Crisis. MIT Press.
- Dowding, D., Randell, R., Gardner, P., Fitzpatrick, G., Dykes, P., & Favela, J. (2019). Dashboards for improving patient care: Review of the literature. International Journal of Medical Informatics, 124, 87-97. https://doi.org/10.1016/j.ijmedinf.2019.01.008
- Feldstein, A. C., Glasgow, R. E., Smith, D. H., & Aickin, M. (2019). Six-Sigma: A case study in a community health center. The Joint Commission Journal on Quality and Patient Safety, 45(2), 96-104. doi:10.1016/j.jcjq.2018.05.002
- George, M. L. (2020). Lean Six Sigma for Service: How to Use Lean Speed and Six Sigma Quality to Improve Services and Transactions (2nd ed.). McGraw-Hill Education.
- George, M. L., Rowlands, D., & Price, M. (2015). The Lean Six Sigma Pocket Tool book: A Quick Reference Guide to 100 Tools for Improving Quality and Speed. McGraw-Hill Education.
- Institute for Healthcare Improvement (IHI). (2020). Introduction to Quality Improvement. https://www.ihi.org/education/IHIOpenSchool/Courses/Pages/QualityImprovement.aspx
- Institute for Healthcare Improvement. (2019). What is Quality Improvement? https://www.ihi.org/education/IHIOpenSchool/Courses/Pages/QualityImprovement.aspx
- Institute of Medicine (IOM). (2001). Crossing the Quality Chasm: A New Health System for the 21st Century. National Academies Press.
- Johnson, J. K., & Jolivet, R. R. (2018). Applying Kotter’s 8-Step Change Model in Nursing. Nurse Leader, 16(2), 117-119. https://doi.org/10.1016/j.mnl.2017.09.005
- Joynt Maddox, K. E., Orav, E. J., Zheng, J., Epstein, A. M. (2018). Evaluation of Medicare’s Bundled Payments Initiative for Medical Conditions. New England Journal of Medicine, 379(3), 260-269. doi:10.1056/NEJMsa1801569
- Langley, G. J., Moen, R. D., Nolan, K. M., Nolan, T. W., Norman, C. L., & Provost, L. P. (2009). The Improvement Guide: A Practical Approach to Enhancing Organizational Performance. Jossey-Bass.
- Leonard, M., Graham, S., & Bonacum, D. (2004). The human factor: Effective teamwork and communication is critical in providing safe care. Quality and Safety in Health Care, 13(Suppl 1), i85-i90. doi:10.1136/qshc.2004.010033
- Mazzocato, P., Savage, C., Brommels, M., Aronsson, H., & Thor, J. (2010). Lean thinking in healthcare: A realist review of the literature. Quality & Safety in Health Care, 19(5), 376-382. doi:10.1136/qshc.2009.037986
- National Academies of Sciences, Engineering, and Medicine. (2018). Crossing the Global Quality Chasm: Improving Health Care Worldwide. National Academies Press.
- National Quality Forum (NQF). (2021). Safe Practices for Better Healthcare – 2021-2022. https://www.qualityforum.org/News_And_Resources/Press_Kits/Safe_Practices_for_Better_Healthcare.aspx
- Radnor, Z. J., & Holweg, M. (2012). Lean in healthcare: The unfilled promise? Social Science & Medicine, 74(3), 364-371. doi:10.1016/j.socscimed.2011.02.011
- Schweickert, P., Keller, M., & Reber, A. (2019). Using data to drive quality improvement in nursing: A guide. Journal of Nursing Management, 27(7), 1404-1408. https://doi.org/10.1111/jonm.12829
- Wheeler, D. J. (2003). Deming’s Profound Changes: When Will the Sleeping Giant Awaken? SPC Press.
- Womack, J. P., Jones, D. T., & Roos, D. (2019). The Machine That Changed the World: The Story of Lean Production–Toyota’s Secret Weapon in the Global Car Wars That Is Now Revolutionizing World Industry. Free Press.
- Arnetz, J. E. (2022, April). The Joint Commission’s new and revised Workplace violence prevention standards for hospitals: A major step forward toward improved quality and safety. Joint Commission journal on quality and patient safety. https://www.ncbi.nlm.nih.gov/pmc/articles/PMC8816837/
- American Nurses Association. (2019, January). Reporting incidents of Workplace Violence – Ana Enterprise. Reporting Incidents of Workplace Violence. https://www.nursingworld.org/~495349/globalassets/docs/ana/ethics/endabuse-issue-brief-final.pdf
- Occupational Safety and Health Administration. (n.d.). Healthcare – workplace violence. https://www.osha.gov/healthcare/workplace-violence/
- Minnesota Nurses Association. (2022, August 10). Hennepin Healthcare Nurses report rising violence against nurses and patients, cite under-staffing, unresponsive management as barriers in new survey. Minnesota Nurses Association. https://mnnurses.org/hennepin-healthcare-nurses-report-rising-violence-against-nurses-and-patients-cite-under-staffing-unresponsive-management-as-barriers-in-new-survey/
- ANA) Workplace violence. (2017). https://www.nursingworld.org/practice-policy/advocacy/state/workplace-violence2/
- Sahebi, A., Golitaleb, M., Moayedi, S., Torres, M., & Sheikhbardsiri, H. (2022, August 8). Prevalence of workplace violence against health care workers in hospital and pre-hospital settings: An umbrella review of meta-analyses. Frontiers in public health. https://www.ncbi.nlm.nih.gov/pmc/articles/PMC9393420/#:~:text=The%20overall%20prevalence%20of%20WPV,%2C%20and%2010.5%25%20(95%25
- Song, C., Wang, G., & Wu, H. (2020, December 3). Frequency and barriers of reporting workplace violence in nurses: An online survey in China. International Journal of Nursing Sciences. https://www.ncbi.nlm.nih.gov/pmc/articles/PMC7859538/
- Staff, A. (2022, November 4). End Nurse Abuse: 4 Actions You Can Take Today. Aorn.org. https://www.aorn.org/article/2021-12-03-End-Nurse-Abuse
- Fountain, D., Zankowski, D., & Arriola, J. (n.d.). Reporting incidents of Workplace Violence – Ana Enterprise. Reporting incidents of Workplace Violence. https://www.nursingworld.org/~495349/globalassets/docs/ana/ethics/endabuse-issue-brief-final.pdf
- S. Bureau of Labor Statistics. (n.d.). Workplace violence in healthcare, 2018. U.S. Bureau of Labor Statistics. https://www.bls.gov/iif/factsheets/workplace-violence-healthcare-2018.htm
- Vincent-Höper, S., Stein, M., Nienhaus, A., & Schablon, A. (2020, May 1). Workplace aggression and burnout in nursing-the moderating role of follow-up counseling. International journal of environmental research and public health. https://www.ncbi.nlm.nih.gov/pmc/articles/PMC7246829/
- Creating a culture of safety in nursing. ANA. (2023, September 12). https://www.nursingworld.org/resources/individual/nurse-managers/safety-in-nursing/
- AlGhatrif, M., & Lindsay, J. (2012). A brief review: History to understand fundamentals of electrocardiography. Journal of Community Hospital Internal Medicine Perspectives, 2(1), 14383. https://doi.org/10.3402/jchimp.v2i1.14383
- Alila Medical Media. (2017). Cardiac action potential, animation. [YouTube Video]. In YouTube. https://www.youtube.com/watch?v=v7Q9BrNfIpQ
- American Heart Association. (2016). Ventricular fibrillation. Www.heart.org. https://www.heart.org/en/health-topics/arrhythmia/about-arrhythmia/ventricular-fibrillation
- Atkielski, A. (2023). PQRST segment. In StatPearls. https://www.ncbi.nlm.nih.gov/books/NBK551635/figure/article-20939.image.f1/?report=objectonly
- Benzoni, T., & Cascella, M. (2021). Procedural sedation. PubMed; StatPearls Publishing. https://www.ncbi.nlm.nih.gov/books/NBK551685/
- Bern Dibner. (2018). Luigi Galvani | Italian physician and physicist. In Encyclopædia Britannica. https://www.britannica.com/biography/Luigi-Galvani
- Birnbaum, Y., Ye, Y., Smith, S. W., & Jneid, H. (2021). Rapid diagnosis of STEMI equivalent in patients with left bundle‐branch block: Is it feasible? Journal of the American Heart Association, 10(18). https://doi.org/10.1161/jaha.121.023275
- Bracey, A. (2023). Posterior MI. In nlm.nih.gov. https://www.ncbi.nlm.nih.gov/books/NBK553168/figure/article-698.image.f1/?report=objectonly
- Burns, E., & Buttner, R. (2021). PVCs. In com. https://litfl.com/premature-ventricular-complex-pvc-ecg-library/
- Burns, E., & Buttner, R. (2023a). Anterior MI. In com. https://litfl.com/anterior-myocardial-infarction-ecg-library/)
- Burns, E., & Buttner, R. (2023b). Monomorphic vtach. In com. https://litfl.com/ventricular-tachycardia-monomorphic-ecg-library/
- Burns, E., & Buttner, R. (2023c). Torsades de Pointes. In com. https://litfl.com/polymorphic-vt-and-torsades-de-pointes-tdp/
- Cadogan, M. (2018, August 1). Delta wave. Life in the Fast Lane. https://litfl.com/delta-wave-ecg-library/
- Cadogan, M. (2022). Lead positioning. In com. https://litfl.com/ecg-lead-positioning/
- Cardiac Science. (2021). ECG graph paper. In ca. https://cardiacsciencesmb.ca/ecg-graph-paper/
- Cardogan, M., & Buttner, R. (2021). Sgarbossa criteria. In com. https://litfl.com/sgarbossa-criteria-ecg-library
- Cascino, T., & Shea, M. (2022, September). Electrocardiography – cardiovascular disorders. MSD Manual Professional Edition. https://www.msdmanuals.com/professional/cardiovascular-disorders/cardiovascular-tests-and-procedures/electrocardiography
- Center for Advanced Cardiac and Vascular Interventions. (2023). Mobile cardiac telemetry (MCT). Center for Advanced Cardiac and Vascular Interventions. https://cacvi.org/services/diagnostic-procedures/mobile-cardiac-telemetry/
- Center for Drug Evaluation and Research. (2021, January 8). FDA drug safety communication: New information regarding QT prolongation with ondansetron (zofran). https://www.fda.gov/drugs/drug-safety-and-availability/fda-drug-safety-communication-new-information-regarding-qt-prolongation-ondansetron-zofran
- Chruścik, A., Kauter, K., Windus, L., & Whiteside, E. (2021). 6.2 cardiac muscle and electrical activity. In pressbooks.pub. University of Southern Queensland. https://usq.pressbooks.pub/anatomy/chapter/6-2-cardiac-muscle-and-electrical-activity/
- Cleveland Clinic. (2022a). Asystole. In clevelandclinic.org. https://my.clevelandclinic.org/health/symptoms/22920-asystole
- Cleveland Clinic. (2022b, June 3). Pulseless electrical activity (PEA): Causes and treatment. Cleveland Clinic. https://my.clevelandclinic.org/health/symptoms/23213-pulseless-electrical-activity
- Cleveland Clinic. (2022c, June 11). Cardiac event monitor: Types and uses. Cleveland Clinic. https://my.clevelandclinic.org/health/diagnostics/23272-cardiac-event-monitor
- Clip Art Library. (2023). EKG machine. In https://clipart-library.com/clipart/2049261.htm.
- Cohagan, B., & Dov Brandis. (2019, February 17). Torsade de Pointes. Nih.gov; StatPearls Publishing. https://www.ncbi.nlm.nih.gov/books/NBK459388/
- Costa, C. (2016). Figure 2.1: A) basic cardiac anatomy and blood circulation through the… In ResearchGate. ResearchGate. https://www.researchgate.net/figure/A-Basic-cardiac-anatomy-and-blood-circulation-through-the-hearts-cavities-and-valves_fig20_320411039
- de Jong, J. (2007a). 2nd AV block. In org. https://en.ecgpedia.org/index.php?title=File:Wenckebach2.png
- de Jong, J. (2007b). A fib. In org. https://en.ecgpedia.org/index.php?title=File:Afib_ecg.jpg
- de Jong, J. (2007c). Normal sinus rhythm. In org. https://en.ecgpedia.org/index.php?title=File:Nsr.jpg
- de Jong, J. (2008). SVT. In org. https://en.ecgpedia.org/index.php?title=File:Avrt_small.svg
- de Jong, J. (2009). A flutter. In org. https://en.ecgpedia.org/index.php?title=File:ECG000011.jpg
- de Jong, J. (2010a). 1st AV block. In org. https://en.ecgpedia.org/index.php?title=File:Rhythm_1stAVblock.png
- de Jong, J. (2010b). 3rd AV block. In org. https://en.ecgpedia.org/index.php?title=File:Rhythm_3rdAVblock.png
- de Jong, J. (2010c). A fib RVR. In org. https://en.ecgpedia.org/index.php?title=File:Afib_f_VR_ecg.jpg
- de Jong, J. (2010d). Bigeminy PVC. In org. https://en.ecgpedia.org/index.php?title=File:Rhythm_bigemini.png
- de Jong, J. (2010e). Idioventricular rhythm. In org. https://en.ecgpedia.org/index.php?title=File:Rhythm_idioventricular.png
- de Jong, J. (2010f). PAC. In org. https://en.ecgpedia.org/index.php?title=File:Rhythm_premature.png
- de Jong, J. (2010g). PVCs. In org. https://en.ecgpedia.org/index.php?title=File:Rhythm_ventricular_premature.png
- de Jong, J. (2010h). Ventricular fibrillation. In org. https://en.ecgpedia.org/index.php?title=File:Rhythm_ventricular_fibrillation.png
- de Jong, J. (2011a). Mobitz. In org. https://en.ecgpedia.org/index.php?title=File:Rhythm_Mobitz.png
- de Jong, J. (2011b, December 13). Normal tracing. En.ecgpedia.org. https://en.ecgpedia.org/index.php?title=Normal_Tracing
- de Jong, J. (2011c). Sinus tachycardia. In org. https://en.ecgpedia.org/index.php?title=File:Rhythm_tachycardia.png
- Dmitriy Scherbak, & Hicks, G. J. (2019, April 7). Left bundle branch block (LBBB). Nih.gov; StatPearls Publishing. https://www.ncbi.nlm.nih.gov/books/NBK482167/
- Douedi, S., & Douedi, H. (2020). P wave. PubMed; StatPearls Publishing. https://www.ncbi.nlm.nih.gov/books/NBK551635/
- Foth, C., Manesh Kumar Gangwani, & Alvey, H. (2020, January 13). Ventricular Tachycardia (VT, V Tach). Nih.gov; StatPearls Publishing. https://www.ncbi.nlm.nih.gov/books/NBK532954/
- Foth, C., & Mountfort, S. (2022). Acute myocardial infarction ST elevation (STEMI). National Library of Medicine; StatPearls Publishing. https://www.ncbi.nlm.nih.gov/books/NBK532281/
- Gangwani, M. K., & Nagalli, S. (2020). Idioventricular rhythm. PubMed; StatPearls Publishing. https://www.ncbi.nlm.nih.gov/books/NBK554520/
- GE HealthCare. (2023a). Apexpro ch telemetry system patient monitors. Www.gehealthcare.com. https://www.gehealthcare.com/products/patient-monitoring/patient-monitors/apexpro-ch-telemetry-system
- GE HealthCare. (2023b). Cardiac beside monitor. In com. https://www.gehealthcare.com/products/patient-monitoring/patient-monitors/carescape-monitor-b650
- Glenlarson . (2023). Inferior MI. In nlm.nih.gov. https://www.ncbi.nlm.nih.gov/books/NBK470572/figure/article-23500.image.f1/?report=objectonly
- Gray, D. (2016). How to read an electrocardiogram (EKG/ECG) (K. Gaines , Ed.). Nurse.org. https://nurse.org/articles/how-to-read-an-ECG-or-EKG-electrocardiogram/
- Hafeez, Y., & Grossman, S. A. (2020). Junctional rhythm. PubMed; StatPearls Publishing. https://www.ncbi.nlm.nih.gov/books/NBK507715/
- Harkness, W. T., & Hicks, M. (2019, June 3). Right bundle branch block (RBBB). Nih.gov; StatPearls Publishing. https://www.ncbi.nlm.nih.gov/books/NBK507872/
- Heaton, J., & Yandrapalli, S. (2021). Premature atrial contractions. PubMed; StatPearls Publishing. https://www.ncbi.nlm.nih.gov/books/NBK559204/
- Henning, A., & Krawiec, C. (2022, August 8). Sinus tachycardia. PubMed; StatPearls Publishing. https://www.ncbi.nlm.nih.gov/books/NBK553128/
- Ibrahim, H. (2022a, May 19). ECG tip 20. what about “orthodromic” SVT?youtube.com. https://www.youtube.com/watch?v=XcnU7mGKdis
- Ibrahim, H. (2022b, May 24). ECG tip 21. what about “antidromic” SVT?youtube.com. https://www.youtube.com/watch?v=qTaNeoGEKJc
- Johns Hopkins Medicine. (2019). Holter monitor. John Hopkins Medicine. https://www.hopkinsmedicine.org/health/treatment-tests-and-therapies/holter-monitor
- Jordan, M. R., Lopez, R. A., & Morrisonponce, D. (2020). Asystole. PubMed; StatPearls Publishing. https://www.ncbi.nlm.nih.gov/books/NBK430866/
- Mangi, M. A., Jones, W. M., & Napier, L. (2019, November 6). Atrioventricular block second-degree. Nih.gov; StatPearls Publishing. https://www.ncbi.nlm.nih.gov/books/NBK482359/
- Mayo Clinic. (2017). Implantable cardioverter-defibrillators (ICDs). Mayoclinic.org. https://www.mayoclinic.org/tests-procedures/implantable-cardioverter-defibrillators/about/pac-20384692
- Mayo Clinic. (2019). Acute coronary syndrome – symptoms and causes. Mayo Clinic. https://www.mayoclinic.org/diseases-conditions/acute-coronary-syndrome/symptoms-causes/syc-20352136
- Mayo Clinic. (2023, July 26). Atrial fibrillation – symptoms and causes. Mayo Clinic. https://www.mayoclinic.org/diseases-conditions/atrial-fibrillation/symptoms-causes/syc-20350624
- McMurray, P. (2018). PVCs multiform. In com. https://bossrn.com/pvc
- Miner, B., Grigg, W. S., & Hart, E. H. (2020a). Wellens syndrome. PubMed; StatPearls Publishing. https://www.ncbi.nlm.nih.gov/books/NBK482490/
- Mountfort, S. (2023). Lateral MI. In nlm.nih.gov. https://www.ncbi.nlm.nih.gov/books/NBK537228/figure/article-24110.image.f2/?report=objectonly
- National Heart, Lung, and Blood Institute. (2022). Atherosclerosis . In nih.gov. https://www.nhlbi.nih.gov/health/atherosclerosis
- Oldroyd, S. H., & Makaryus, A. N. (2020). First degree heart block. PubMed; StatPearls Publishing. https://www.ncbi.nlm.nih.gov/books/NBK448164/
- Osmosis by Elsevier. (2023). Cardiac electrophysiology notes: Diagrams & illustrations. Www.osmosis.org. https://www.osmosis.org/notes/Cardiac_Electrophysiology#page-1
- Oxford Medical Education. (n.d.). ECG (EKG) – bundle branch block. Oxford Medical Education. https://oxfordmedicaleducation.com/ecgs/bundle-branch-block/
- Parker, S. (n.d.). Telemetry – MeSH – NCBI. Www.ncbi.nlm.nih.gov. Retrieved September 8, 2023, from https://www.ncbi.nlm.nih.gov/mesh/?term=telemetry
- Patti, L., & Ashurst, J. V. (2019, June 4). Supraventricular tachycardia (SVT). Nih.gov; StatPearls Publishing. https://www.ncbi.nlm.nih.gov/books/NBK441972/
- Rodriguez Ziccardi, M., Goyal, A., & Maani, C. V. (2020). Atrial flutter. PubMed; StatPearls Publishing. https://www.ncbi.nlm.nih.gov/books/NBK540985/
- RWJ Barnabas Health. (2023). Telemetry monitor technician. In org. https://www.rwjbh.org/community-medical-center/treatment-care/heart-and-vascular-care/programs-and-specialties/centralized-cardiac-telemetry-monitoring-program/
- Sandau, K. E., Funk, M., Auerbach, A., Barsness, G. W., Blum, K., Cvach, M., Lampert, R., May, J. L., McDaniel, G. M., Perez, M. V., Sendelbach, S., Sommargren, C. E., & Wang, P. J. (2017). Update to practice standards for electrocardiographic monitoring in hospital settings: A scientific statement from the American Heart Association. Circulation, 136(19). https://doi.org/10.1161/cir.0000000000000527
- Sattar, Y. (2023). Lead placement. In StatPearls. https://www.ncbi.nlm.nih.gov/books/NBK549803/figure/article-20969.image.f1/?report=objectonly
- Sklavos, T. (2020, November 3). ECG interpretation: Myocardial ischaemia and infarction. LITFL. https://litfl.com/ecg-interpretation-myocardial-ischaemia-and-infarction/
- Slane, M., Knabben, V., & Chhabra, L. (2019). Third-Degree atrioventricular block. Nih.gov; StatPearls Publishing. https://www.ncbi.nlm.nih.gov/books/NBK545199/
- Smith, S. (2014). Wide complex SVT. In hqmeded-ecg.blogspot.com. https://hqmeded-ecg.blogspot.com/2014/12/wide-complex-tachycardia-lewis-leads-do.html
- Vincent’s Hospital. (n.d.). Holter monitor. In svhhearthealth.com.au. https://www.svhhearthealth.com.au/Images/UserUploadedImages/976/10_HolterMonitor.jpg
- Thanassoulis, G., & Aziz, H. (2018). Atherosclerosis. Merck Manuals Professional Edition; Merck Manuals. https://www.merckmanuals.com/professional/cardiovascular-disorders/arteriosclerosis/atherosclerosis
- The Univeristy of Nottingham. (n.d.-a). Bipolar Leads. Www.nottingham.ac.uk. https://www.nottingham.ac.uk/nursing/practice/resources/cardiology/function/bipolar_leads.php
- The University of Nottingham. (n.d.-b). Limb leads. Www.nottingham.ac.uk. https://www.nottingham.ac.uk/nursing/practice/resources/cardiology/function/limb_leads.php
- University of Utah Health. (n.d.). ECG learning center – an introduction to clinical electrocardiography. Utah.edu. https://ecg.utah.edu/lesson/9
- Wisconsin Technical College System. (2021). 3 cardiovascular assessment. Wtcs.pressbooks.pub. https://wtcs.pressbooks.pub/nursingskills/chapter/9-3-cardiovascular-assessment/
- Wong, E. (2013). Action potential of cardiac muscles. In org. http://www.pathophys.org/physiology-of-cardiac-conduction-and-contractility/actionpotential/
- Yamama Hafeez, & Grossman, S. A. (2019, November 18). Sinus bradycardia. Nih.gov; StatPearls Publishing. https://www.ncbi.nlm.nih.gov/books/NBK493201/
- Yasar Sattar, & Hashmi, M. F. (2019, December 3). Ventricular premature complexes. Nih.gov; StatPearls Publishing. https://www.ncbi.nlm.nih.gov/books/NBK547713/
- Zeid Nesheiwat, Amandeep Goyal, & Mandar Jagtap. (2022). Atrial fibrillation . Nih.gov; StatPearls Publishing. https://www.ncbi.nlm.nih.gov/books/NBK526072/
- Zimmermann, P., & Hammond, B. (2023). Sheehy’s manual of emergency care. (8th ed.). Elsevier Health Sciences.
- ZOLL Medical Corporation. (2023). X series cardiac monitor/defibrillator for EMS – ZOLL medical. Www.zoll.com. https://www.zoll.com/products/defibrillators/x-series-for-ems
- American Psychiatric Association. (2018, May 7). Nearly one in three people know someone addicted to opioids; More than half of millennials believe it is easy to get illegal opioids. https://www.psychiatry.org/newsroom/news-releases/nearly-one-in-three-people-know-someone-addicted-to-opioids-more-than-half-of-millennials-believe-it-is-easy-to-get-illegal-opioids#:~:text=An%20estimated%202%20million%20people,more%20than%2042%2C000%20in%202016.
- American Psychiatric Association. (2020). Addiction and substance use disorders. https://www.psychiatry.org/patients-families/addiction/what-is-addiction
- American Society of Addiction Medicine. (2018, April 11). Public policy statement on prescription drug monitoring programs (PDMPs) [Policy Brief]. American Society of Addiction Medicine. https://www.asam.org/docs/default-source/public-policy-statements/2018-statement-on-pdmpsf406229472bc604ca5b7ff000030b21a.pdf?sfvrsn=63ba42c2_0
- American Society of Addiction Medicine. (2020). The ASAM National Practice Guideline for the treatment of opioid use disorder: 2020 focused update. https://www.asam.org/docs/default-source/quality-science/npg-jam-supplement.pdf?sfvrsn=a00a52c2_2
- Bettinardi-Angres, K. (2020). Nurses with substance use disorder: Promoting successful treatment and reentry, 10 years later. Journal of Nursing Regulation, 11(1), 5-11. https://doi.org/10.1016/S2155-8256(20)30054-5
- Bose, J., Hedden, S. L., Lipari, R. N., & Park-Lee, E. (2018). Key substance use and mental health indicators in the United States: Results from the 2017 National Survey on Drug Use and Health. Substance Abuse and Mental Health Services Administration. https://www.samhsa.gov/data/sites/default/files/cbhsq-reports/NSDUHFFR2017/NSDUHFFR2017.pdf
- Centers for Disease Control and Prevention (CDC). (2020a). Prescription opioids: The basics. https://www.cdc.gov/rxawareness/information/index.html
- Centers for Disease Control and Prevention (CDC). (2020b). Understanding the epidemic. https://www.cdc.gov/drugoverdose/epidemic/index.html
- Centers for Disease Control and Prevention (CDC). (2020c). U.S. opioid dispensing rate maps. https://www.cdc.gov/drugoverdose/maps/rxrate-maps.html
- Centers for Disease Control and Prevention (CDC). (2020d). U.S. state opioid dispensing rates, 2019. https://www.cdc.gov/drugoverdose/maps/rxstate2019.html
- Centers for Disease Control and Prevention (CDC). (2021). Prescription drug monitoring programs (PDMPs). https://www.cdc.gov/drugoverdose/pdmp/providers.html
- Christo, P., Fudin, J., Gudin, J. & Peeples, L. (Eds.) (2019). Opioid prescribing and monitoring: How to combat opioid abuse and misuse responsibly. https://www.practicalpainmanagement.com/resource-centers/opioid-prescribing-monitoring/cover
- Copeland, D. (2019). Drug-seeking: A literature review (and an exemplar of stigmatization in nursing). Nursing Inquiry, 27, e12329. https://doi.org/10.1111/nin.12329
- Dowell, D., Haegerich, T. M., & Chou, R. (2016, March 18). CDC guidelines for prescribing opioids for chronic pain – United States, 2016. MMWR, 65(1), 1-49. http://dx.doi.org/10.15585/mmwr.rr6501e1
- Ducharme, J. & Moore, S. (2019). Opioid use disorder assessment tools and drug screening. Missouri Medicine, 116(4), 318-324. https://www.ncbi.nlm.nih.gov/pmc/articles/PMC6699803/
- Federation of State Medical Boards. (2017, April). Guidelines for the chronic use of opioid analgesics. https://www.fsmb.org/siteassets/advocacy/policies/opioid_guidelines_as_adopted_april-2017_final.pdf
- Goff, M. (2016). WV Board of Pharmacy; Controlled substance monitoring program (CSMP). https://www.deadiversion.usdoj.gov/mtgs/pharm_awareness/conf_2016/feb_2016/goff.pdf
- Gregorian, R., Marrett, E., Sivathanu, V., Torgal, M., Shah, S., Kwong, W. J. & Gudin, J. (2020). Safe opioid storage and disposal: A survey of patient beliefs and practices. Journal of Pain Research, 13, 987-995. http://doi.org/10.2147/JPR.S242825
- Karch, A. M. (2017). Focus on nursing pharmacology (7th ed.). Wolters Kluwer.
- Khan, M. (2020). Substance use disorders. https://www.merckmanuals.com/home/mental-health-disorders/substance-related-disorders/substance-use-disorders
- Lipari, R. N. & Hughes, A. (2017). How people obtain the prescription pain relievers they misuse. SAMHSA Short Report. https://www.samhsa.gov/data/sites/default/files/report_2686/ShortReport-2686.html
- Lynn, R. R., & Galinkin, J. L. (2018). Naloxone dosage for opioid reversal: Current evidence and clinical implications. Therapeutic Advances in Drug Safety, 9(1), 63-68. https://doi.org/10.1177/2042098617744161
- Mennella, H. & Uribe, L. M. (2018). Personnel management: Impaired health professionals – Return to work. CINAHL Nursing Guide.
- National Council of State Boards of Nursing (NCSBN). (2018). A nurse’s guide to substance use disorder in nursing. https://www.ncsbn.org/SUD_Brochure_2014.pdf
- National Institute on Drug Abuse (NIDA). (2020a). Health consequences of drug misuse. https://www.drugabuse.gov/drug-topics/health-consequences-drug-misuse/introduction
- National Institute on Drug Abuse (NIDA). (2020b). Marijuana research report. https://www.drugabuse.gov/publications/research-reports/marijuana/letter-director
- National Institute on Drug Abuse (NIDA). (2020c). Misuse of prescription drugs research report. https://www.drugabuse.gov/publications/research-reports/misuse-prescription-drugs/overview
- National Institute on Drug Abuse (NIDA). (2020d). Opioid overdose reversal with naloxone (narcan, evzio). https://www.drugabuse.gov/drug-topics/opioids/opioid-overdose-reversal-naloxone-narcan-evzio
- National Institute on Drug Abuse (NIDA). (2020e). The science of drug use and addiction: The basics. https://www.drugabuse.gov/publications/media-guide/science-drug-use-addiction-basics
- National Institute on Drug Abuse (NIDA). (2020f). West Virginia: Opioid-involved deaths and related harm. https://www.drugabuse.gov/drug-topics/opioids/opioid-summaries-by-state/west-virginia-opioid-involved-deaths-related-harms
- National Institute on Drug Abuse (NIDA). (2021). Opioid overdose crisis. https://www.drugabuse.gov/drug-topics/opioids/opioid-overdose-crisis
- Perry, J. & Vandenhouten, C. L. (2019). Drug diversion detection. Nursing Management, 50(2), 16-21. https://doi.org/10.1097/01.NUMA.0000552735.56577.4b
- Rager, J. B. & Schwartz, P. H. (2017). Defending opioid treatment agreements: Disclosure, not promises. Hastings Center Report, 47(3), 24-33. https://doi.org/10.1002/hast.702
- Sedney, C. L., Khodaverdi, M., Pollini, R., Dekeseredy, P., Wood, N, & Haggerty, T. (2021). Assessing the impact of a restrictive opioid prescribing law in West Virginia. Substance Abuse Treatment, Prevention, and Policy, 16(14). https://doi.org/10.1186/s13011-021-00349-y
- Sinha, S. (2020). Naloxone injection. https://www.drugs.com/naloxone.html
- Smischney, N., Pollard, E. M., Nookala, A. U., & Olatoye, O. O. (2018). Serotonin syndrome in the perioperative setting. American Journal of Case Reports, 19, 833-835. https://doi.org/10.12659/AJCR.909497
- Thornton, P. (2020). Naltrexone injection. https://www.drugs.com/naltrexone.html
- U.S. Department of Justice. (n.d). Controlled substance schedules. https://www.deadiversion.usdoj.gov/schedules/#define
- U.S. Food and Drug Administration. (2020a). Disposal of unused medicines: What you should know. https://www.fda.gov/drugs/safe-disposal-medicines/disposal-unused-medicines-what-you-should-know
- U.S. Food and Drug Administration. (2020b). New recommendations for naloxone. https://www.fda.gov/drugs/drug-safety-and-availability/new-recommendations-naloxone
- U.S. National Library of Medicine. (2020). Substance use disorder. https://medlineplus.gov/ency/article/001522.htm
- West Virginia Board of Pharmacy. (2018, July 6). West Virginia Board of Pharmacy announces statewide electronic health record integration of prescription data. https://www.wvbop.com/article.asp?id=24
- West Virginia Department of Health and Human Services. (2020, January 20). West Virginia 2020-2022 substance use response plan. https://dhhr.wv.gov/office-of-drug-control-policy/news/Documents/FINAL%20-%20West%20Virginia%202020_2022%20Council%20Substance%20Use%20Plan_January%2020,%202020%20(as%20filed).pdf
- West Virginia Legislature. (2021). Chapter 60A. Uniformed Controlled Substance Act: Article 9. Controlled substances monitoring. West Virginia Legislature’s Office of Reference and Information. http://www.wvlegislature.gov/wvcode/code.cfm?chap=60A&art=9#01
- West Virginia RN Board. (2021). Education information for nurses. https://wvrnboard.wv.gov/education/Pages/For-Nurses.aspx
- Wilson, N., Kariisa, M., Seth, P., Smith, H. IV., & Davis, N. L. (2020). Drug and opioid overdose deaths – United States, 2017-2018. MMWR, 69, 290-297. http://dx.doi.org/10.15585/mmwr.mm6911a4
- Witkiewitz, K. & Vowles, K. E. (2018). Alcohol and opioid use, co-use, and chronic pain in the context of the opioid epidemic: A critical review. Alcohol Clin Exp Res., 42(3), 478-488. https://doi.org/10.1111/acer.13594
Disclaimer:
Use of Course Content. The courses provided by NCC are based on industry knowledge and input from professional nurses, experts, practitioners, and other individuals and institutions. The information presented in this course is intended solely for the use of healthcare professionals taking this course, for credit, from NCC. The information is designed to assist healthcare professionals, including nurses, in addressing issues associated with healthcare. The information provided in this course is general in nature and is not designed to address any specific situation. This publication in no way absolves facilities of their responsibility for the appropriate orientation of healthcare professionals. Hospitals or other organizations using this publication as a part of their own orientation processes should review the contents of this publication to ensure accuracy and compliance before using this publication. Knowledge, procedures or insight gained from the Student in the course of taking classes provided by NCC may be used at the Student’s discretion during their course of work or otherwise in a professional capacity. The Student understands and agrees that NCC shall not be held liable for any acts, errors, advice or omissions provided by the Student based on knowledge or advice acquired by NCC. The Student is solely responsible for his/her own actions, even if information and/or education was acquired from a NCC course pertaining to that action or actions. By clicking “complete” you are agreeing to these terms of use.
➁ Complete Survey
Give us your thoughts and feedback
➂ Click the Green MARK COMPLETE Button Below
To receive your certificate
