Course
Women’s Health: Uterine Fibroids
Course Highlights
- In this Women’s Health: Uterine Fibroids course, we will learn about the signs and symptoms of uterine fibroids.
- You’ll also learn of the complications that can occur if uterine fibroids are left untreated.
- You’ll leave this course with a broader understanding of pharmacological and non-pharmacological interventions for uterine fibroid management.
About
Contact Hours Awarded: 2
Course By:
Sadia Arshad
MPH, MSN, WHNP-BC
Begin Now
Read Course | Complete Survey | Claim Credit
➀ Read and Learn
The following course content
Introduction
When hearing the phrase uterine fibroids, what comes to mind? Have you even heard of uterine fibroids prior to this course? Truthfully, most health care settings and nursing schools do not educate clinicians or patients on the complexities of uterine fibroids since fibroids are still quite the mystery in women’s health. In fact, uterine fibroids can vary in clinical presentation significantly from person to person, making their diagnosis and management complex and often time-consuming for patients (1). The information in this course will serve as a valuable resource for nurses of all specialties, education levels, and backgrounds to learn more about uterine fibroids.
Uterine Fibroids: The Basics
What Is a Uterine Fibroid?
Simply put, a uterine fibroid, also known as a myoma or leiomyoma, is a non-cancerous growth that occurs in the uterus. The uterus, also known as the womb, is an internal organ that plays a major role in pelvic health, the menstrual cycle, and pregnancy. For reference, the uterus is often comparable to the size of someone’s heart or fist. Uterine fibroids are interesting because they can occur anywhere in the uterus and sometimes protrude outside of the uterine cavity as well. For instance, someone can have a uterine fibroid in the upper part of the uterus or the lower part of the uterus (or both!).
Fibroids that can grow within the walls of the uterus are known as intramural fibroids. Fibroids that can grow and bulge into the uterine cavity are known as submucosal fibroids. In addition, a fibroid that can grow outside of the uterus is known as a subserosal fibroid. Fibroids are complex since someone can have only one fibroid or multiple fibroids [see Figure 2] (2).
Uterine fibroids can also be found in multiple parts of the uterus or in one part of the uterus. Fibroids can also vary in size, such as one fibroid the size of a pea to one fibroid the size of a grapefruit. Because of the varying locations, sizes, and amounts of fibroids, clinical presentation and management can vary from person to person. Fibroids can also resolve on their own in some cases, causing some patients to opt for a “wait and see” approach in terms of management (3).
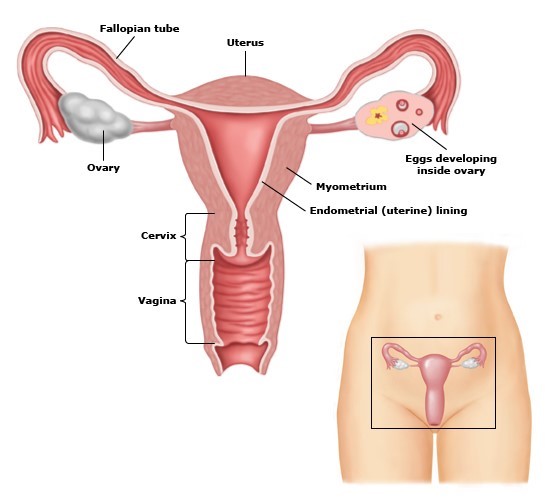
Figure 1. Female Reproductive System (2)
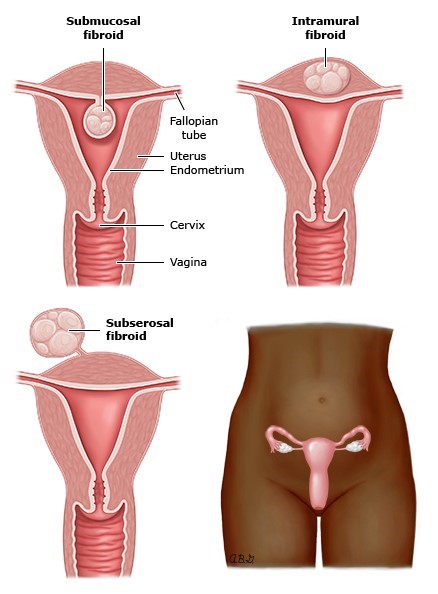
Figure 2. Types of Uterine Fibroids (2)
What Causes Uterine Fibroids to Develop?
Studies have shown that an estimated 70-80% of people with a uterus can have at least one uterine fibroid in their lifetime (2, 3). Unfortunately, there is no known specific cause for uterine fibroids. More research is showing that possible increased oxidative stress on the cellular level can possibly influence fibroid development. Oxidative stress is when there is an imbalance between antioxidants and prooxidants in the body. Smoking, dietary habits, and chronic stress can play a role in oxidative stress; however, more research needs to be done to determine the long-term implications of oxidative stress on fibroid growth and development (1).
What are Risk Factors for Developing Uterine Fibroids?
Since the exact cause for uterine fibroid development is not known yet, many studies have looked at possible risk factors for uterine fibroid development (1, 2, 3). Some studies have discussed that chronic stress, such as exposure to repeated instances of racism and sexism, and genetics play a role in fibroid development (4). Multiple studies have also suggested that Black women in America are far more likely to develop fibroids possibly because of the complex chronic trauma and stress Black women experience (3, 4). Further research suggests that Asian women are at increased risk of uterine fibroid development as well (5). Globally, women of color compose the majority of cases of uterine fibroids (6). Researchers speculate the role of chronic stress and lack of access to gynecological care as risk factors for uterine fibroid development (3, 5). Estrogen, progesterone, and obesity are thought to play roles in fibroid development as well (3).
What are Signs and Symptoms of Uterine Fibroids?
Because of their varied presentation in (and even around) the uterus, signs and symptoms of uterine fibroids can also significantly vary person to person (1, 2, 3, 6). Some signs and symptoms of uterine fibroids include:
- Heavy menstrual bleeding, sometimes soaking through more than one pad or tampon an hour and with visible chunks of bloody tissue
- Prolonged menstrual bleeding, sometimes lasting longer than a week
- Pelvic pain or pressure (or both) in varying parts of the pelvis
- Constipation
- Intestinal pain
- Abdominal pain
- Urinary pain
- Urinary urgency
- Bladder pain
- Back pain
- Pain during sex (dyspareunia)
- Fertility complications, such as trouble getting pregnant
- Pregnancy complications, such as recurrent pregnancy loss and placental complications

Self Quiz
Ask yourself...
- What is the possible connection between oxidative stress and uterine fibroid development?
- What is the difference between a submucosal fibroid and intramural fibroid?
- What are some reasons why women of color in the U.S. and globally are at increased risk for uterine fibroid development?
Epidemiology
How Common are Uterine Fibroids in the USA? Globally?
Uterine fibroids are estimated to affect 70-80% of people with a uterus in the U.S. (2, 3). Uterine fibroids are estimated to affect 20-80% of people with a uterus globally (6). Due to the lack of access to reproductive health care, stigma around uterine health, social shame around women’s health, and lack of education on uterine fibroids among patients and health care professionals, the true prevalence of uterine fibroids in the U.S. and globally is not known (6).

Self Quiz
Ask yourself...
- What are possible contributing factors that influence uterine fibroid prevalence in the U.S. and globally?
- What are some factors that may contribute to the high costs of uterine fibroids in someone’s life?
- What are some health issues that can possibly emerge as a result of having uterine fibroids?
Pathophysiology
How Do Uterine Fibroids Grow?
Several factors can influence uterine fibroid growth; however, there is not a known singular cause for uterine fibroid growth. Several research studies are assessing the possible causes for uterine fibroid growth and proliferation. First, someone needs to have a uterus. Second, uterine fibroid growth is a result of complex etiology involving epigenetics, cellular hypoxia, pelvic inflammation, chronic stress, diet, environmental exposures, and fibrogenesis (1, 3, 5, 6). Whole-genome sequencing has shown that a mutation in mediator complex subunit 12 (MED12) occurs in approximately up to 70% of uterine fibroid cases, showing a possible association between the rate of MED12 mutations and tumor number (1).
In addition, hypoxia is a condition in which there is inadequate oxidation. Hypoxia is thought to have a role in increasing the expression of prooxidant enzymes, like myeloperoxidase (MPO) and inducible nitric oxide synthase (iNOS) in human uterine fibroid cells. Research suggests that fibroid cells have higher levels of oxidative stress markers MPO and iNOS, which are further increased under hypoxic conditions. Increased oxidative stress markers can lead to decreased apoptosis of uterine fibroid cells, leading to the possible buildup of uterine fibroid cells (1).
What Happens if Uterine Fibroids are Left Untreated?
For some people, if uterine fibroids are left untreated, uterine fibroids can resolve on their own (2). For other people, uterine fibroids may have no signs or symptoms that affect their daily lives, as fibroids can vary in their size and location. Yet, for many others, having fibroids is a chronic, life-altering health condition that is among the top leading causes of morbidity among reproductive-age women in the U.S. (3). Many people with fibroids experience decreased quality of life, such as increased pain with sex, missed days of school or work, and prolonged heavy vaginal bleeding. These experiences can also further lead to hemorrhage, anemia, chronic pelvic pain, increased hospitalizations, increased medical complications, and more (1, 3, 4, 5, 6, 7).
Research shows that people with uterine fibroids tend to have increased rates of anxiety, depression, and self-harm, which can further influence their quality of life and overall health (7). In addition, fibroids can influence someone’s fertility and pregnancy outcomes, leading to possible fertility and pregnancy complications (3). Most people with fibroids do not have fibroids in the menopausal or postmenopausal phase; however, there are still instances of uterine fibroids in menopausal and postmenopausal women (2). Many social and cultural norms also influence the lives of people with fibroids, as menstrual health and pelvic health is stigmatized in many cultures. As a result, there is possible social stigma and shame prevalent among people with fibroids, which can further influence quality of life, mental health, and overall physical health (6).

Self Quiz
Ask yourself...
- How can genetics influence uterine fibroid growth and development?
- What are some psychosocial and physical implications for someone with uterine fibroids that are left untreated?
- What role do social norms and culture play in the development of uterine fibroid complications?
Diagnosis and Management
Uterine fibroids are often diagnosed via pelvic examination and ultrasound (2). Sometimes, uterine fibroids are also found in instances of uterine surgery, such as during a cesarean section (C-section) or tubal ligation procedure. There is no blood test to determine if someone has uterine fibroids. After diagnosis, management options for uterine fibroids is often a conversation between health care professionals and patients, as several management decisions are influenced by cost, time, personal choice, and extent of fibroids.
Medications
Presently, there is no medication approved by the Food and Drug Administration (FDA) to reduce or eliminate the growth of uterine fibroids. Myfembree and Oriahnn are both GnRH antagonist drugs that are FDA approved to help with bleeding associated with uterine fibroids (8, 9). Tranexamic acid is an antifibrinolytic medication that can possibly help with bleeding associated with uterine fibroids (10).
It is important to educate patients that Myfembree, Oriahnn, and tranexamic acid will not decrease the size of uterine fibroids or eliminate uterine fibroids. Due to the nature of these types of medications, a detailed health history should be taken along with an explanation of side effects (2, 11).
Treatment for Bleeding
If someone is experiencing extensive bleeding because of fibroids, iron supplementation and blood transfusions can be considered (11). Pain management for fibroids is often with NSAIDs, such as ibuprofen (2, 11). Depending on someone’s health history and clinical presentation, hormonal contraception can be considered for help with bleeding and pelvic pain (11). The Mirena intrauterine device (IUD) is FDA approved for heavy menstrual bleeding management and may help with bleeding from fibroids (11, 12). Oral contraception, the vaginal ring, and other forms of hormonal contraception can be considered as well (11).
As with Myfembree, Oriahnn, and tranexamic acid, hormonal contraception will not decrease the size of or eliminate uterine fibroids. Obtaining a health history and educating on side effects should be initiated as well (2, 11).
Lifestyle Considerations
In addition to medication management, there are also possible lifestyle considerations to keep in mind. Stress management, diet, exercise, mental health therapy, and pelvic floor physical therapy are possible options to help manage uterine fibroids (1, 13).
Holistic Therapies
Acupuncture, massage therapy, and herbal medications per some cultural traditions are also possible methods of chronic pain management as a result of fibroids, though limited evidence exists showing the effectiveness of these methods on fibroid pain and bleeding management (1, 13).
Surgeries and Procedures
Furthermore, there are surgical options for uterine fibroid management. A myomectomy is a surgical procedure to remove uterine fibroids. Depending on the location and extent of fibroids, people can maintain their fertility after a myomectomy (2, 11). However, many people will need to have a C-section after a myomectomy given the health of the uterus. A myomectomy can remove existing fibroids, but it will not stop fibroids from re-emerging, as there are people who have experienced several myomectomy procedures.
Another surgical option is uterine artery embolization, a procedure in which medicine is introduced into the uterine arteries to reduce blood supply to the uterine fibroids and uterus directly [see Figure 3]. Like a myomectomy, people can maintain their fertility after uterine fibroid embolization, and they might also need a C-section as well depending on the extent of their uterine health (2, 11).
Finally, one of the most recommended routes for uterine fibroid management is hysterectomy – the surgical removal of the uterus. Hysterectomy is often recommended for patients who do not desire to get pregnant and who exhausted several options with fibroid management. For many people, fibroid management is extremely personal because of the possible medication side effects, surgical interventions, medication costs, work-life balance, personal goals, access to health care, and desire for future fertility (3).
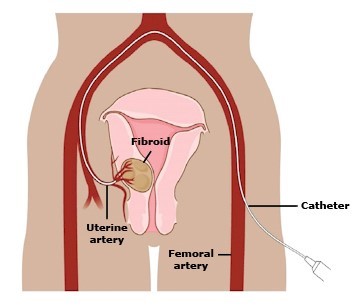
Figure 3. Uterine Artery Embolization (2)

Self Quiz
Ask yourself...
- What are some methods that can be used to help with bleeding associated with uterine fibroids?
- How might a myomectomy influence someone’s uterine health and possible future fertility?
- In what situation would a patient consider a hysterectomy?
The Nurse’s Role
Nurses remain the most trusted profession for a reason. Patients turn to nurses for guidance, education, and support. Unfortunately, it is not possible to look at someone with the naked eye and determine if they have uterine fibroids. Nurses can assist in identifying if someone has uterine fibroids by taking a complete health history, listening to patients’ concerns, and communicating any concerns to other health care professionals. The following are nursing roles in uterine fibroid care.
Providing Quality Uterine Fibroid Care
While there is no specific guideline for the nurse’s role in uterine fibroid care, here are some suggestions to provide quality care for patients with or suspected of having uterine fibroids.
- Take a detailed health history. Often, women’s pain associated with conditions like heavy bleeding or constipation, are often dismissed in health care settings (even in women’s health settings) (1, 3, 4, 5, 6). If a patient is complaining of heavy bleeding, pelvic pain, or anything that causes the patient or you concern, inquire more about that complaint. Ask about how long the symptoms have lasted, what treatments have been tried, if these symptoms interfere with their quality of life. Ask if anything alleviates any of these symptoms. If you feel like a patient’s complaint is not being taken seriously by other health care professionals, advocate for that patient to the best of your abilities.
- Ask about family history. If someone is complaining of symptoms that could be related to uterine fibroids, ask if anyone in their immediate family, such as their mother or sister, experiences heavy bleeding or has a history of fibroids.
- Be willing to answer questions about uterine fibroids and pelvic anatomy. Society often stigmatizes open discussions of reproductive and pelvic health. Fibroids are no exception. There are many people who do not know the location of the uterus, the existence of uterine fibroids, or the ways the menstrual cycle works. Be willing to be honest with yourself about your comfort level discussing topics and providing education on uterine fibroids and pelvic anatomy.
- Communicate the care plan to other staff involved for continuity of care. For many patients, uterine fibroid management often involves a team of obstetricians/gynecologists (OB/GYNs), nurses, pelvic floor physical therapists, pharmacies, and more. Ensure that patients’ records are up to date for ease in record sharing and continuity of care.
- Stay up to date on continuing education related to uterine fibroids and gynecological conditions, as evidence-based information is always evolving and changing. You can then present your new knowledge and findings to other health care professionals, and educate your patients with the latest information. You can learn more about the latest research on uterine fibroids and gynecological health by following updates from the American College of Obstetrics and Gynecology (ACOG) and other national women’s health evidence-based organizations (14).
Teaching Patients About Uterine Fibroids
Patients should know that anyone with a uterus has the possibility of developing uterine fibroids. Patients should be aware that if they notice any changes in their bleeding patterns, experience any continuous pelvic pain, or feel like something is a concern, they should seek medical care. Due to the social stigma associated with women’s health, pelvic health, and reproductive health, people may be hesitant to seek medical care because of society’s normalization of women’s pain and bleeding. However, as more research and social movements discuss women’s health and uterine fibroids more openly, there can be a heightened awareness of uterine fibroids and uterine health (1, 2, 3).
Nurses should also teach patients to advocate for their own health in order to avoid progression of uterine fibroids and possible chronic health complications from uterine fibroids. Here are important tips for patient education in the inpatient or outpatient setting.
- Tell the nurse or health care provider of any existing medical conditions or concerns (needed to identify risk factors)
- Tell the nurse or health care provider if you notice any changes in your menstrual flow, duration, or intensity (possible changes that could hint at the development or existence of uterine fibroids)
- Tell the nurse or health care provider if you have any changes in urinary or bowel habits, such as increased or decreased urination or defecation (potential risk for chronic pelvic complications)
- Tell the nurse or health care provider if you experience any pain that increasingly becomes more severe or interferes with your quality of life
- Keep track of your menstrual cycle, bleeding, pain, and any pelvic health concerns via an app, diary, or journal (self-monitoring for any changes)
- Tell the nurse or health care provider if you start to have trouble using the restroom by yourself or bleed through your clothes (possible changes that can indicate hemorrhage, pelvic pain progression, or other health emergencies)
- Tell the nurse or health care provider right away if you are bleeding vaginally and having trouble breathing, trouble walking, or trouble maintaining consciousness (increased blood loss due to bleeding from fibroids can lead to hemorrhage and other health emergencies)
- Take all prescribed medications as indicated and ask questions about medications and possible other treatment options, such as non-pharmacological options or surgeries
- Tell the nurse or provider if you notice any changes while taking medications or undergoing other treatments to manage your uterine fibroids (potential worsening or improving uterine fibroid situation)

Self Quiz
Ask yourself...
- What are some problems that can occur if uterine fibroids are managed adequately?
- What is one reason a health care provider would order a pelvic ultrasound?
- What are some possible ways you can obtain a detailed, patient-centric health history?
- What are some possible ways nurses can educate patients on uterine fibroids?
Research Findings
There are several studies on uterine fibroids, especially on the influence of uterine fibroid development and chronic stress. More research is being done to determine the exact cause of uterine fibroids and possible methods to reduce fibroid growth or size (1, 2, 3).
Many major cities in the U.S. have opportunities for people with uterine fibroids to be involved in uterine fibroid research through major universities or health care systems. In addition, the Eunice Kennedy Shriver National Institute of Child Health and Human Development (NICHD) conducts research on uterine fibroids and can serve as a resource when searching for existing research opportunities (15).

Self Quiz
Ask yourself...
- What are some ways you can educate patients on uterine fibroid clinical trials?
- What are some reasons someone might would want to enroll in uterine fibroid clinical trials?
Case Studies
Case Study #1
Samantha is a 32-year-old Black woman working as a chef. She arrives to her annual well-women exam at the local OB/GYN clinic next to her place of work. She reports that she’s using condoms with her husband and would like to get pregnant within the next year. As she talks about her desire to become pregnant, she mentions that she had a miscarriage last year. Samantha also mentions that within the past year, she’s been having more heavy periods that last a long time and experiencing more trouble going to the bathroom regularly. She also mentions that she’s been having some trouble adjusting to her new job as a chef lately and even takes a few days off during her period because the bleeding is getting worse. She denies taking any medications, denies having a history of sexually transmitted infections (STIs), and denies any drug use. Her urine pregnancy test is negative.
- What are some specific questions you’d want to ask about her bleeding pattern?
- What are some family history questions you’d want to highlight?
- What lab work or imaging would you suggest to the health care provider to obtain?

Samantha agrees to complete an ultrasound and bloodwork later this week and thinks she might have a family history of uterine fibroids. She said that no one in her family talks about periods or “things down there,” but she heard about fibroids from her mother and grandmother a long time ago. She’s back in the office a few weeks later, and her ultrasound shows that she has four fibroids in different parts of the uterus. Her bloodwork also shows that she has low hemoglobin as well.
- How would you discuss fibroids and their locations to Samantha?
- How would you explain to Samantha the impact of fibroids and heavy bleeding on her hemoglobin levels?
Samantha still wants to try to get pregnant with fibroids and is not interested in hormonal contraception. She would also want to have at least two biological children and is willing to learn more about her management options.
- Knowing Samantha’s concerns, what are some possible uterine fibroid management options for her?
- How would you explain the role of fibroids in her ability to maintain a pregnancy or become pregnant?
Case Study #2
Kim is a 19-year-old Asian woman working as a tutor at her university as a full-time student. She arrives to her annual well-women exam at the local OB/GYN office in the student health building. She reports that she’s never been to a women’s health doctor before, but she wants to be checked out for her periods. Kim states that she’s had her period for a few years, and they’ve been getting heavier for the past year. She states that in high school, she used to bleed through her underwear sometimes, even with using a pad. Kim doesn’t want to repeat what happened in high school. She wants to know what can be causing this bleeding and what can be done to stop heavy periods. She states that sometimes her period pain is so bad, she can’t get out of bed.
Kim reports having some social support, but she states she cannot “deal with the stress of more heavy periods anymore.” She thinks she wants kids in the future, but she’s not sure. She denies any concerns about being pregnant and denies engaging in sex recently. She reports taking 12 pills of ibuprofen during her period for the last six months for period pain, denies having a history of sexually transmitted infections (STIs), and denies any drug use. Her urine pregnancy test is negative.
- What are some specific questions you’d want to ask about her medication use?
- What are some family history questions you’d want to highlight?
- What lab work or imaging would you suggest to the health care provider to perform?
- What are some questions around pregnancy prevention you could ask?
Kim agrees to complete an ultrasound and bloodwork later in the week and thinks she might have a family history of uterine fibroids. She said that no one in her family talks about periods or “stuff down there,” but she heard about fibroids from her mother and some aunts a long time ago. She’s back in the office a few weeks later, and her ultrasound shows that she has six fibroids in different parts of the uterus. Her bloodwork returns and shows no abnormalities. When you tell her about the six fibroids, she starts crying because she thinks she is being punished for having sex before marriage and for going to college so far away from her family. She asks if she can get pregnant in the future with fibroids.
- How would you discuss fibroids and their locations to Kim? What educational tools would you use?
- How do culture, social norms, and social stigma influence the public perception of uterine fibroids?
Kim is crying less now after you answered her concerns, and she texted her mom while she was crying in the office. Her mom said that she also had uterine fibroids before she entered menopause. Kim still wants to get pregnant after completing her college studies, but she states she “definitely doesn’t want to get pregnant now” with her busy school and work schedule. Kim reports feeling stressed, sleep deprived, and worried about her health, but is interested in learning any options to help with her uterine fibroid situation.
- Knowing Kim’s concerns and health history, what are some possible uterine fibroid management options for her?
- How would you explain the role of uterine fibroids in her ability to maintain a pregnancy or become pregnant?
- How would you explain the role of uterine fibroids in someone’s body throughout their lifespan?
- How would her uterine fibroids influence her possible pelvic pain and mental health?
- What are some non-pharmacological options you can discuss with Kim regarding her uterine fibroids?
Case Study #3
Barabara is a 45-year-old white woman working as a lawyer. She arrives to her annual well-women exam at the local OB/GYN clinic next to her office. She reports that she’s been having really heavy periods in the past year. She states that her periods have been heavy most of her life, but in the past year, the pain and flow is “becoming a literal living nightmare.” Barbara reports that her husband had a vasectomy, so she’s not worried about being pregnant and has no desire to be pregnant again. Barbara mentions that she’s having increased back pain and pelvic pain with the last few periods, and she wants to know what can be done about this pain and bleeding.
She reports smoking a pack of cigarettes a day, denies having a history of sexually transmitted infections (STIs), and reports taking an unknown contraceptive pill in the past for heavy periods “which did nothing.” Her urine pregnancy test is negative.
- What are some specific questions you’d want to ask about her bleeding pattern?
- What are some family history questions you’d want to highlight?
- What lab work or imaging would you suggest to the health care provider to obtain?
Barbara agrees to complete an ultrasound and bloodwork later this week and thinks she might have a family history of uterine fibroids. She’s back in the office a few weeks later, and her ultrasound shows that she has eight fibroids in different parts of the uterus. Her bloodwork shows no abnormalities. In this visit, she mentions that her mom had “her tubes tied to fix things down there,” so she thinks her mom had uterine fibroids. Barbara’s sister was diagnosed with uterine fibroids yesterday, and Barbara is concerned about fibroids. Barbara asks if smoking can cause uterine fibroids.
- How would you discuss uterine fibroids and their locations to Barbara?
- How would you explain to Barbara the impact of fibroids and chronic pain?
- How would you explain that uterine fibroids might have an environmental component?
Barbara has no interest in taking another pill for any reason and still does not want to be pregnant in the future. Barbara does not want to stop smoking, as she states, “it’s the only stress reliever I have in my busy life.” She reports having a good social support system and the financial means to explore all uterine fibroid treatment and management options. She is willing to learn more about possible surgery options because “I can’t keep on living like this. It’s a living nightmare, and I’m willing to do anything to end it.”
- Knowing Barbara’s concerns, what are some possible uterine fibroid surgical options for her?
- What are some possible considerations for surgery to keep in mind?
- What are non-pharmacological ways Barbara can reduce her discomfort with uterine fibroids prior to surgery?
Conclusion
Uterine fibroids are a complex chronic health condition that affects millions of people with a uterus nationwide. Due to their varying sizes, shapes, and locations, uterine fibroids can present clinically in several ways. Some people with uterine fibroids will state that they bleed for two weeks every month through a pad an hour, have constipation, and pain with sex. Others will state they bleed for a few days heavily, have trouble urinating, and have chronic back pain. Some people will present to the emergency room with severe anemia and pain requesting for a hysterectomy immediately. Education and awareness of this chronic health condition can influence the lives of many people.
References + Disclaimer
- AlAshqar, A., Lulseged, B., Mason-Otey, A., Liang, J., Begum, U.A.M., Afrin, S., & Borahay, M.A. (2023). Oxidative Stress and Antioxidants in Uterine Fibroids: Pathophysiology and Clinical Implications. Antioxidants, 12, 807. https://doi.org/10.3390/antiox12040807
- Stewart, E. A. & Laughlin-Tommaso, S. K. (2023). Patient Education: Uterine Fibroids (Beyond the Basics). UptoDate. Retrieved 19 December 2023 from https://www.uptodate.com/contents/uterine-fibroids-beyond-the-basics/
- Katon, J. G., Plowden, T. C., & Marsh, E. E. (2023). Racial disparities in uterine fibroids and endometriosis: A systemic review and application of social, structural, and political context. Fertility and Sterility, 119(3), 355-365. https://doi.org/10.1016/j.fertnstert.2023.01.022
- Qin, H., Lin, Z., Vasquez, E., & Xu, L. (2019). The association between chronic psychological stress and uterine fibroids risk: A meta-analysis of observational studies. Stress and Health, 35(5), 585-594. https://doi.org/10.1002/smi.2895
- Huang, D., Magaoay, B., & Rosen, M. (2023). Presence of fibroids on transvaginal ultrasonography in a community-based diverse cohort of 996 reproductive-age female participants. JAMA Network Open, 6(5), 1-3. https://doi:10.1001/jamanetworkopen.2023.12701
- Cheng, L-C., Li, H-Y., Gong, Q-Q., Huang, C-Y., Zhang, C., & Yan J-Z. (2022). Global, regional, and national burden of uterine fibroids in the last 30 years: Estimates from the 1990 to 2019 Global Burden of Disease Study. Frontiers in Medicine, 9, 1-9. https://doi.org/10.3389/fmed.2022.1003605
- Chiuve, S.E., Huisingh, C., Petruski-Iveleva, N., Owens, C., Kuohung, W. &Wise, L. A. (2021). Uterine fibroids and incidence of depression, anxiety and self-directed violence: a cohort study. Journal of Epidemiology and Community Health, 76, 92-99. https://doi:10.1136/jech-2020-214565
- Pfizer – Myfembree. (2023). Meet Myfembree. Retrieved 19 December 2023 from https://www.myfembree.com
- Abbvie – Oriahnn. (2022). Oriahnn. Retrieved 22 December 2023 from https://www.oriahnn.com
- Lysteda (Tranexamic Acid). Federal Drug Administration (FDA) (2009). Full Prescribing Information – Lysteda (Tranexamic Acid). Retrieved 22 December 2023 from https://www.accessdata.fda.gov/drugsatfda_docs/label/2009/022430lbl.pdf
- De la Cruz, M. S. D. & Buchanan, E.M. (2017). Uterine Fibroids: Management and Treatment. American Family Physician, 95(2), 100-107. Retrieved 19 December 2023 from https://www.aafp.org/pubs/afp/issues/2017/0115/p100.html
- Bayer – Mirena. (2023). Mirena. Retrieved 19 December 2023 from https://www.mirena-us.com
- Tu, F. F. & As-Sanie, S. (2022). Patient Education: Chronic pelvic pain in females (Beyond the Basics). UptoDate. Retrieved 19 December 2023 from https://www.uptodate.com/contents/chronic-pelvic-pain-in-females-beyond-the-basics
- The American College of Obstetrics and Gynecology (ACOG). (2023). Uterine Fibroids: Frequently Asked Questions. ACOG. Retrieved 19 December 2023 from https://www.acog.org/womens-health/faqs/uterine-fibroids
- National Institute of Child Health and Human Development (NICHD). (2018). NICHD Uterine Fibroids Research Information. NICHD. Retrieved 19 December 2023 from https://www.nichd.nih.gov/health/topics/uterine/researchinfo
Disclaimer:
Use of Course Content. The courses provided by NCC are based on industry knowledge and input from professional nurses, experts, practitioners, and other individuals and institutions. The information presented in this course is intended solely for the use of healthcare professionals taking this course, for credit, from NCC. The information is designed to assist healthcare professionals, including nurses, in addressing issues associated with healthcare. The information provided in this course is general in nature and is not designed to address any specific situation. This publication in no way absolves facilities of their responsibility for the appropriate orientation of healthcare professionals. Hospitals or other organizations using this publication as a part of their own orientation processes should review the contents of this publication to ensure accuracy and compliance before using this publication. Knowledge, procedures or insight gained from the Student in the course of taking classes provided by NCC may be used at the Student’s discretion during their course of work or otherwise in a professional capacity. The Student understands and agrees that NCC shall not be held liable for any acts, errors, advice or omissions provided by the Student based on knowledge or advice acquired by NCC. The Student is solely responsible for his/her own actions, even if information and/or education was acquired from a NCC course pertaining to that action or actions. By clicking “complete” you are agreeing to these terms of use.
➁ Complete Survey
Give us your thoughts and feedback
➂ Click the Green MARK COMPLETE Button Below
To receive your certificate
